Purpose
To evaluate the influence of stem offset and neck shaft angles on the range of motion before component impingement (ROMCI) and bony impingement (ROMBI), and the types of impingement in total hip arthroplasty (THA).
Methods
Using the computed tomography data of 101 patients who underwent THA, three-dimensional dynamic motion analysis was performed using a modular implant (Kinectiv® stem) that enabled adjustment of offset and leg length independently. We defined offset as horizontal offset (HO) and leg length as vertical offset (VO), and measured the ROMCI and ROMBI in flexion (Flex), internal rotation (Int-R) and external rotation (Ext-R) with the configuration of each horizontal/vertical offset.
Results
We found that HO lengthening increased the ROMCI and ROMBI in Flex and Int-R by delaying bony impingement, although excessive lengthening had minimal effect. On the contrary, VO lengthening decreased the ROMCI and ROMBI in Flex and ROMCI in Int-R. As for Ext-R, VO lengthening had positive effects on the ROMCI and ROMBI, whereas lengthening of HO had negative effects on the ROMCI and ROMBI.
Conclusions
We demonstrated that the appropriate long offset with a low shaft angle increased the ROM in Flex and Int-R, and a high neck shaft angle increased the ROM in Ext-R. We should use implants properly in accordance with the types of impingement for avoiding dislocations in THA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total hip arthroplasty (THA) has been the most popular treatment procedure for patients with severe osteoarthritis of the hip joint. However, there are several complications in THA, and dislocation is one of the most serious complications for patients. It has continued to be a frequent complication over the past several years and the incidence after primary THA is reported as between 1.7 and 4% [1–3]. Bartz et al. [4] reported three different mechanisms of dislocation: (1) impingement of the prosthetic femoral neck on the cup liner (implant impingement), (2) impingement of the osseous femur on the osseous pelvis (bony impingement), and (3) spontaneous dislocation. Many authors have reported that dislocation occurs mainly by implant impingement and bony impingement [4–6].
The factors that are associated with increased risk of dislocation include surgical approach, status of the soft tissues, and implant orientation and alignment. Other factors which influence dislocation include the implant design, the choice of neck shaft angle and stem offset [7–9]. Recently, a lot of implants have become available from several manufacturers, thus allowing surgeons the choice of a greater variety of femoral implants with different neck-shaft angles and offsets so that an adequate range of motion (ROM) and soft-tissue tension can be achieved. Several previous clinical reports have shown that increasing the femoral offset has the benefits of an increased ROM, better mechanical advantage for the abductor and decreased instability [10, 11]. Therefore, surgeons should be familiar with the effects of increasing or decreasing the offset and neck shaft angles on hip ROM, although the magnitudes of the contributions of these factors to implant/bony impingement, both singly and in combination, are not fully known.
Nowadays, preoperative planning is often performed for THA and computed simulation analysis is often used by many investigators to predict optimal implant orientations and to analyze the ROM in THA [12–15]. The purpose of this study is to evaluate the influence of the stem offset and neck shaft angles on the types of impingement and ROM before bony/implant impingement after THA using computed tomography (CT)-based three-dimensional (3D) dynamic motion analysis.
The modular femoral stem system
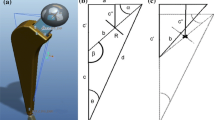
To evaluate the influences of the stem offset and neck shaft angles on hip ROM after THA, we used the Zimmer M/L Taper Hip Prosthesis with Kinectiv® Technology (Zimmer, Warsaw, IN, USA) that would allow us to manipulate the femoral offset and leg length independently (Fig. 1a). This modular system consists of three components: a femoral head, femoral neck, and femoral stem. We used two definitions: horizontal offset (HO) and vertical offset (VO) (Fig. 1b). There are three neck variables that can be adjusted independently: HO, leg length (VO) and version. There are up to five HO and VO options in 4-mm increments, and the system has 20 neck options in horizontal/vertical offset combinations in total. Each neck option can be coupled with a different head option (e.g., a 28-mm, a 32-mm, and a 36-mm diameter head). To evaluate the influences of increased HO and VO on hip ROM, five necks were used in this study; standard offset, +4 mm and +8 mm in vertical and horizontal offset with standard neck version, respectively (Fig. 1b). The neck-shaft angle is altered; increasing HO while maintaining the same VO decreases the neck-shaft angle, and increasing VO while maintaining the same HO increases the neck-shaft angle (Fig. 1c).
a Kinectiv® femoral stem. b We evaluated ROM using five necks: standard offset (0 mm); a +4 mm HO (point a means neck length is horizontally extended by 4 mm while maintaining the same VO), b +8 mm HO; c +4 mm VO (point c means neck length is vertically extended by 4 mm while maintaining the same HO); d +8 mm VO. c The red arrow indicates the neck-shaft angle increases from 128 to 138° by decreasing HO and increasing VO
Materials and methods
Patients
This study comprised a total of 101 Japanese patients (101 hips) who underwent THA, including 30 men and 71 women with the mean age of 63.5 years (range, 54–87 years). The hip diagnoses were osteoarthritis in 79 joints and osteonecrosis of the femoral head in 22 joints. We excluded patients who had a severely dislocated hip, or who had undergone previous surgery or a post-osteotomy from the present study. A subset of patients with complete implant data was reviewed for sizing. All patients had a preoperative CT scan of their hip joint, from the anterior superior iliac spine (ASIS) to the knee joint through the distal femoral condyles using a 320-row multidetector helical CT scanner (Aquilion ONE; Toshiba Medical Healthcare, Tochigi, Japan) (detector configuration, 80 × 0.5; beam collimation, 40 mm) with a reconstructed slice width of 1.00 mm and a slice interval of 1.00 mm. The CT data were transferred to the planning module. Ethics approval was granted by the Institutional Review Board.
Three-dimensional motion analysis
CT-based simulation software (ZedHip Lexi, Tokyo, Japan) [15] was used to create virtual 3D bone models and perform virtual simulations of the femoral cut and component setting, using the preoperative THA planning mode. This software allows for the generation and separation of independent femoral and acetabular 3D models.
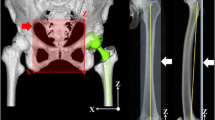
Based on CT scans of pelvis and femur, the reference points were firstly digitized, then a 3D reconstruction of the bone model was made semi-automatically. If there was noise, they were revised manually (Fig. 2). Next, the size of the components and their 3D orientation relative to the host bones were planned and implantation was performed in a multiplanar reconstructed (MPR) view. This software allows the simulation and calculation of the ROM until contact occurs between bones and components. It also visualizes the site of impingement in 3D axial/sagittal/coronal views of MPR images. The pelvic coordinate system was the functional pelvic plane and the femoral coordinate system was defined by the center of the femoral head, the knee center, and both femoral condyles.
The simulated implant was the Kinectiv® femoral stem with a 32-mm-diameter alumina head in all cases. The appropriate size of femoral stem was selected for each femur to maximize both fit and fill in the femoral metaphysis under the consideration of stem size used in the actual procedure. The center of the femoral component was placed in the center of the native femoral diaphysis. The acetabular side had a Trilogy® Acetabular Hip System with a PE liner without marginal lips in all cases. The acetabular component size was also selected to maximize fit in the acetabulum under the consideration of component size used in the actual procedure. The acetabular component position was determined to place the implant at the site of the normal acetabulum. The anteversion of the femoral implant was set at 25°, cup anteversion 20° (total anteversion was fixed) and cup abduction 45° in a radiographic manner.
Calculation of the ROM and impingement location
The center of the femoral head is located by fitting a sphere to the articular surface of the femoral head. The pelvis was fixed in space, while the femur was free to translate in all directions but constrained to rotate around the center of rotation of the hip. The computer software was capable of detecting bone to bone, bone to implant and implant impingement, which allowed the maximum ROM to be defined as the degrees of movement before impingement of either bone or implant occurred. We defined the ROM before component impingement as ROMCI and the ROM before bony impingement as ROMBI, and measured ROMCI and ROMBI in each horizontal/vertical offset. The location of this impingement on both the femoral and acetabular side, as well as the position of the femur in space relative to the fixed pelvis, can be also defined in the model. Based on this computerized analysis, the ROM was measured in those directions that are important for dislocation and activities of daily living (ADL): flexion with 0° of adduction (Flex), internal rotation in 90° of flexion with 0° of adduction (Int-R) and external rotation in 0° of flexion with 0° of adduction (Ext-R).
Evaluation design
To evaluate the influences of the stem offset and neck shaft angles on the ROMCI and ROMBI, the ROMCI and ROMBI were compared in each horizontal/vertical offset.
Statistical analysis
All data were expressed as mean ± standard deviation (SD) and statistical analysis was performed using Stat-View-J version 5.0 software (Hulinks, Tokyo, Japan). The correlations were evaluated using Pearson’s chi-squared test. A P value of less than 0.001 was considered statistically significant.
Results
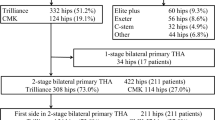
In this section, we summarized the data of types of impingement and each ROM in Table 1.
Flex
In Flex, impingement occurred in three ways: bone to bone impingement (bony impingement) (the anterior great trochanteric region of the femur or femoral bony neck impinges on the anteroinferior edge of anterior inferior iliac spine [AIIS]); stem neck impinges on the edge of acetabular component (implant impingement); the femoral shaft impinges on the anterior aspect of anterior superior iliac spine (ASIS). In standard offset, bony impingement often preceded implant impingement in many cases. However implant impingement preceded bony impingement as VO increased (Table 1).
Overall, the mean total ROM of Flex was 111 ± 11.1° in standard offset, 119 ± 11.6° in +4 mm HO, 126 ± 11.4° in +8 mm HO, 108 ± 8.2° in +4 mm VO, and 104 ± 11.3° in +8 mm VO. The hip ROM of flex increased statistically significantly as the HO increased (Fig. 3a). Furthermore, the ROM of Flex increased by 8.4 ± 3.8° with +4 mm HO and increased by 6.8 ± 3.3° with +8 mm HO, with significant differences between them (Fig. 3b). On the other hand, the mean ROM of Flex decreased inversely proportional to the VO length with statistical significance (Fig. 3a). However, the decreased angle was 2.8 ± 5.2° between standard and +4 mm VO, and 2.9 ± 4.4° between +4 mm VO and +8 mm VO, with no significant differences (Fig. 3b). As for the ROMBI and ROMCI, the former was smaller than the latter in all cases, which indicates that bony impingement caused a more limited ROM than implant impingement in Flex. Both the ROMCI and ROMBI increased with statistical differences as the HO length increased, whereas the ROMCI and ROMBI decreased with statistical differences as the VO length increased. There were significant differences between the ROMCI and ROMBI in each length of HO and VO (Fig. 3c).
a The average ROM of Flex in each horizontal/vertical offset. The black line indicates the ROM of Flex in each length of HO. The gray line indicates the ROM of Flex in each length of VO. b. The increased angle of Flex from standard neck to +4 mm length and from +4 mm length to +8 mm in each horizontal/vertical offset; +4 mm means the each offset was lengthen by 4 mm from standard neck, and +8 mm means the each offset was lengthen from +4 mm neck to +8 mm neck. c. The ROMCI and ROMBI in Flex with each horizontal/vertical offset. The black line indicates the ROMCI in each length of HO. The gray line indicates the ROMCI in each length of VO. The black dotted line indicates the ROMBI in each length of HO and the gray dotted line indicates the ROMBI in each length of VO (*P < 0.0001)
Int-R
In Int-R, impingement occurred in two ways: bony impingement (the anterior great trochanteric region of the femur or femoral bony neck impinges on the anteroinferior edge of AIIS) and implant impingement. In standard offset, bony impingement preceded implant impingement in many cases. However, implant impingement increased as the length of VO and HO increased, and implant impingement occurred more frequently as the VO increased compared with HO (Table 1).
Overall, the mean total ROM in Int-R was 27.1 ± 14.2° in standard offset, 32.7 ± 13.3° in +4 mm HO, 36.8 ± 12.4° in +8 mm HO, 27.4 ± 12.5° in +4 mm VO and 26.9 ± 11.4° in +8 mm VO (Table 1). The ROM significantly increased as the HO increased (Fig. 4a). Furthermore, the increased angle was 5.6 ± 2.5° between standard and +4 mm HO, and 4.0 ± 2.7° between +4 mm HO and +8 mm HO, with significant differences between them (Fig. 4b). On the other hand, the mean ROM hardly changed, as the length of VO increased. There were no significant differences between the ROM in standard, +4 mm VO and +8 mm VO, respectively (Fig. 4a). As for the ROMCI and ROMBI, both ROMCI and ROMBI significantly increased as the length of HO increased, and the ROMBI also increased as the length of VO increased, although ROMBI improved more by increasing HO in comparison with increasing VO. Furthermore, the increasing HO had a positive effect on the ROMBI more greatly compared with ROMCI. However, the ROMCI decreased with statistical differences as the VO increased. There were significant differences between ROMCI and ROMBI of Int-R in each length of HO and VO (Fig. 4c).
a The average ROM of Int-R in each horizontal/vertical offset. The black line indicates the ROM of Int-R in each length of HO. The gray line indicates the ROM of Int-R in each length of VO. b The increased angle in Int-R from standard neck to +4 mm length and from +4 mm length to +8 mm in each horizontal/vertical offset. c The ROMCI and ROMBI in Int-R with each horizontal/vertical offset. The black line indicates the ROMCI in each length of HO. The gray line indicates the ROMCI in each length of VO. The black dotted line indicates the ROMBI in each length of HO and the gray dotted line indicates the ROMBI in each length of VO (*P < 0.0001)
Ext-R
In Ext-R, impingement occurred in two ways: bony impingement (the lesser trochanter or femoral bony neck impinges on ischial bone) and implant impingement. In standard offset, bony impingement preceded implant impingement in many cases. The number of bony impingement cases increased as the length of HO increased, whereas the number of implant impingement cases increased as the length of VO increased (Table 1).
Overall, the mean total ROM in Ext-R was 57.1 ± 8.0° in standard, 50.5 ± 6.5° in +4 mm HO, 45.1 ± 6.0° in +8 mm HO, 63.1 ± 9.8° in +4 mm VO and 68.1 ± 11.0° in +8 mm VO. The total ROM decreased as the length of HO increased with statistical significance (Fig. 5a). The decreased angle was 5.6 ± 2.5° between standard and +4 mm HO, and 4.0 ± 2.7° between +4 mm HO and +8 mm HO, with significant differences between them (Fig. 5b). On the contrary, the mean ROM significantly increased, as the length of VO increased (Fig. 5a). The increased angle was 5.9 ± 6.8° between standard and +4 mm VO, and 4.9 ± 4.9° between +4 mm HO and +8 mm HO, with significant differences between them (Fig. 5b). As for ROMBI and ROMCI, both of them decreased with statistical differences as the length of HO increased, whereas the ROMCI increased with statistical differences as the length of VO increased (Fig. 5c). Furthermore, ROMBI was improved more in comparison with ROMCI by increasing VO.
a The average ROM in Ext-R with each horizontal/vertical offset. The black line indicates the ROM of Ext-R in each length of HO. The gray line indicates the ROM of Ext-R in each length of VO. b The increased angle in Ext-R from standard neck to +4 mm length and from +4 mm length to +8 mm in each horizontal/vertical offset. c The ROMCI and ROMBI of Ext-R in each horizontal/vertical offset. The black line indicates the ROMCI in each length of HO. The gray line indicates the ROMCI in each length of VO. The black dotted line indicates the ROMBI in each length of HO and the gray dotted line indicates the ROMBI in each length of VO (*P < 0.0001)
Discussion
Impingement is often the main etiology for post-THA instability. If a force is transmitted to push the femoral head out of the cup, it would be inevitable to prevent the dislocation. Even without dislocation, the patient may complain of clicking in various daily of life, leading to anxiety and dissatisfaction. Recent studies have shown several options to acquire a satisfactory ROM. Widmar et al. [12] reported that a cup inclination between 40° and 42°, combined with a cup anteversion between 23°and 28°, and the stem antetorsion determined according to the formula, cup anteversion + 0.7 × stem antetorsion = 37°, fulfilled the severe ROM conditions. Alternative bearings with femoral heads of larger diameter have been also used with the aim of reducing both wear and implant impingement [16, 17]. Crowinshield et al. [18] demonstrated an almost linear increase in the prosthetic impingement free ROM with an increase in femoral head diameter from 22 to 40 mm. However, once bony impingement becomes a main cause of impingement and restriction of hip motion in THA, dislocation can occur even with optimally positioned implants and large femoral head [6, 19, 20].
The characteristics of a prosthesis, such as implant design, neck shaft angle and stem offset are also important factors for joint stability after THA [7, 8, 21, 22]. An appropriate offset and leg-length restoration are reported to be important factors for improving the physical function and minimizing the risk of dislocation [19, 23]. Several clinical reports have shown that an increased femoral offset correlates with increased ROM by delaying the effects of bony impingement [10, 22]. However, the magnitudes of the contributions of the stem offset and neck shaft angle on implant/bony impingement, both singly and in combination is not yet fully understood, and less has been detailed the effect of lengthening of HO and VO on ROMCI, ROMBI and the types of impingement.
Nowadays, preoperative planning can be executed with a high degree of accuracy for THA and the optimal implant orientation and impingement have been evaluated by many investigators using computerized simulation analysis [12–15]. It offers a template of information regarding the location of the impingement region, providing feedback on the anticipated improvement in motion in vivo.
In our study, the implant positions were set to be the same in all cases for avoiding the impingement based on the ‘combined anteversion concept’. Our results showed that the longer the HO length, the more the ROMCI and ROMBI in Flex and Int-R increased. Greater ROM was achieved with an 8-mm femoral offset, although the effect of HO lengthening decreased especially in ROMCI of Int-R. With respect to Int-R, the increasing HO had a positive effect on the ROMBI more greatly compared with ROMCI. In a standard neck, the location of initial contact in Flex and Int-R was at the greater trochanteric region or femoral bony neck on the anteroinferior aspect of AIIS in most of the cases, and the number of bony impingement cases decreased as the length of HO became longer. On the other hand, the longer the length of VO, the more the ROMCI and ROMBI of Flex and the ROMCI of Int-R decreased. These results indicate that an implant with low neck shaft angle and high offset is effective for improving the ROM in Flex and Int-R by delaying the bony impingement, although excessive HO lengthening had minimal positive effects. However, implant with high neck shaft angle has a negative effect on ROM in Flex and Int-R. As for Ext-R, lengthening of the HO had a negative effect on the ROMCI and ROMBI, and the effect of HO lengthening also became small. On the contrary, lengthening of VO had a positive effect on the ROMCI and ROMBI of Ext-R, and the effect of lengthening of VO from +4 to +8 mm was the same as that from standard neck to +4 mm.
With respect to the location of initial contact in Ext-R, the number of bony impingement cases decreased as the length of VO became longer. These results indicate that implant with high neck shaft angle and low offset is effective for improving the ROM by delaying bony impingement in Ext-R.
From the point of view for avoiding the anterior impingement, when implant impingement became the restricting factor of hip ROM, selection of the implant with a lower neck shaft angle and high offset, increasing head diameter and/or decreasing femoral anteversion may decrease the incidence of dislocation by allowing increased ROMCI of Flex and Int-R. On the other hand, when bony impingement became the restricting factor of ROM, increasing head diameter had no further effect on ROM, so the selection of the lower neck shaft implant with high offset, increasing femoral anteversion [24] and/or trimming of impingement site may increase the ROMBI of Flex and Int-R.
However, some reports claim that a substantial number of patients with a high offset femoral stem experienced either trochanteric or gluteal pain [25], and bearing in mind that the effect on ROM attenuates with excessive HO lengthening, the latter should be avoided. On the other hand, when posterior impingement became the restricting factor, using an implant with a higher neck shaft angle and low offset and/or decreasing femoral neck version may decrease the incidence of dislocation by allowing increased ROMCI and ROMBI of Ext-R. Whether implant or bony impingement can restrict ROM after THA can be assumed to some extent by CT date or simulation [24], we have to take these facts into consideration and select the proper implant and offset before THA for the case with easily impingement.
There were several limitations in our study. Firstly, in our study the influence of the surrounding soft tissue was not taken into account, which may have affected the actual hip ROM. Appropriate soft-tissue tensioning is critical to achieving stability; however, such analysis is difficult to perform experimentally. Secondly, only one prosthetic design was tested, the absolute ROM values may not be applicable to other designs, although the relative changes in ROM due to neck-shaft angle and HO should be generally valid for other implant geometries. Thirdly, we only analyzed the ROM until impingement. Hip dislocation involves levering of the head out of the socket after impingement, and a larger head size may improve resistance to dislocation, even if the ROM until impingement remains the same.
In summary, we demonstrated that the HO lengthening has positive effects on the ROMCI and ROMBI of Flex and Int-R, whereas the implant with high neck shaft angle is effective for improving the ROM of Ext-R. Therefore, we should use the proper implant and offset options in accordance with the types of impingement in THA.
References
Caton J, Prudhon JL (2011) Over 25 years survival after Charnley’s total hip arthroplasty. Int Orthop 35(2):185–188
Gordon M, Greene M, Frumento P, Rolfson O, Garellick G, Stark A (2014) Age- and health-related quality of life after total hip replacement: decreasing gains in patients above 70 years of age. Acta Orthop 85(3):244–249
Bozic KJ, Lau EC, Ong KL, Vail TP, Rubash HE, Berry DJ (2012) Comparative effectiveness of metal-on-metal and metal-on-polyethylene bearings in medicare total hip. J Arthroplasty 27(8 Suppl):37–40
Bartz RL, Nobel PC, Kadakia NR, Tullos HS (2000) The effect of femoral component head size on posterior dislocation of the artificial hip joint. J Bone Joint Surg Am 82:1300–1307
Jolles BM, Zangger P, Leyvraz PF (2002) Factors predisposing to dislocation after primary total hip arthroplasty a multivariate analysis. J Arthroplasty 17:282–288
Kessler O, Patil S, Stefan W, Mayr E, Colwell CW, D’Lima DD (2008) Bony impingement affects range of motion after total hip arthroplasty: a subject-specific approach. J Orthop Res 26(4):443–452
Charnley J (1979) Low friction principle. In: Charnley J (ed) Low friction arthroplasty of the hip. Springer, New York, pp 3–15
McGrory BJ, Morrey BF, Cahalan TD, Cabanela ME (1995) Effect of femoral offset on range of motion and abductor muscle strength after total hip arthroplasty. J Bone Joint Surg (Br) 77:865
Wallner O, Stark A, Muren O, Eisler T, Sköldenberg O (2015) Unstable hip arthroplasties. A prospective cohort study on seventy dislocating hips followed up for four years. Int Orthop 39(6):1037-1044
Matsushita A, Nakashima Y, Jingushi S, Yamamoto T, Kuraoka A, Iwamoto Y (2009) Effects of the femoral offset and the head size on the safe range of motion in total hip arthroplasty. J Arthroplasty 24(4):646–651
Sariali E, Klouche S, Mouttet A, Pascal-Moussellard H (2014) The effect of femoral offset modification on gait after total hip arthroplasty. Acta Orthop 85(2):123–127
Widmer KH, Zurfluh B (2004) Compliant positioning of total hip components for optimal range of motion. J Orthop Res 22:815–821
Kessler O, Patil S, Stefan W, Mayr E, Colwell CW, D’Lima DD (2008) Bony impingement affects range of motion after total Hip arthroplasty: a subject-specific approach. J Orthop Res 26(4):443–452
Incavo SJ, Thompson MT, Gold JE, Patel RV, Icenogle KD, Noble PC (2011) Which procedure better restores intact hip range of motion: total hip arthroplasty or resurfacing? a combined cadaveric and computer simulation study. J Arthroplasty 26(3):391–397
Shoji T, Yasunaga Y, Yamasaki T, Mori R, Hamanishi M, Ochi M (2013) Bony impingement depends on the bone morphology of the hip after total hip arthroplasty. Int Orthop 37:1897–1903
Lachiewicz PF, Soileau ES (2013) Low early and late dislocation rates with 36- and 40-mm heads in patients at high risk for dislocation. Clin Orthop Relat Res 471(2):439–443
Garbuz DS, Masri BA, Duncan CP, Greidanus NV, Bohm ER, Petrak MJ, Della Valle CJ, Gross AE (2012) Dislocation in revision THA: do large heads (36 and 40 mm) result in reduced dislocation rates in a randomized clinical trial? Clin Orthop Relat Res 470(2):351–356
Crowninshield RD, Maloney WJ, Wentz DH, Humphrey SM, Blanchard CR (2004) Biomechanics of large femoral heads: what they do and don’t do. Clin Orthop Relat Res 429:102–107
Bourne RB, Rorabeck CH (2002) Soft tissue balancing the hip. J Arthroplasty 17(Suppl 1):17–22
Caton JH, Prudhon JL, Ferreira A, Aslanian T, Verdier R (2014) A comparative and retrospective study of three hundred and twenty primary charnley type hip replacements with a minimum follow up of ten years to assess whether a dual mobility cup has a decreased dislocation risk. Int Orthop 38(6):1125–1129
Puchner SE, Funovics PT, Hipfl C, Dominkus M, Windhager R, Hofstaetter JG (2014) Incidence and management of hip dislocation in tumour patients with a modular prosthesis of the proximal femur. Int Orthop 38(8):1677–1684
Chandler DR, Glousman R, Hull D, McGuire PJ, Kim IS, Clarke IC, Sarmiento A (1982) Prosthetic hip range of motion and impingement the effects of head and neck geometry. Clin Orthop Relat Res 166:284–291
Iorio R, Healy WL, Warren PD, Appleby D (2006) Lateral trochanteric pain following primary total hip arthroplasty. J Arthroplasty 21:233–236
Shoji T, Yasunaga Y, Yamasaki T, Izumi S, Hachisuka S, Ochi M (2015) Low femoral antetorsion and total hip arthroplasty: a risk factor. Int Orthop 39(1):7–12
Incavo SJ, Havener T, Benson E, McGrory BJ, Coughlin KM, Beynnon BD (2004) Efforts to improve cementless femoral stems in THR: 2- to 5-year follow-up of a high-offset femoral stem with distal stem modification (Secur-Fit Plus). J Arthroplasty 19(1):61–67
Conflict of interests
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this work. No competing interests are disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shoji, T., Yamasaki, T., Izumi, S. et al. The influence of stem offset and neck shaft angles on the range of motion in total hip arthroplasty. International Orthopaedics (SICOT) 40, 245–253 (2016). https://doi.org/10.1007/s00264-015-2826-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2826-3