Abstract
Purpose
The purpose of this study was to evaluate whether femoral antetorsion affects the range of motion (ROM) following total hip arthroplasty (THA) using 3D dynamic analysis.
Methods
Using 3D computed tomography (CT) data of 71 patients (71 hips) who underwent THA, we calculated antetorsion of the femoral neck, flexion range of motion (Flex ROM), internal rotation (Int-R) and external rotation (Ext-R). Evaluation of the relationship between antetorsion, ROM and the impingement site was performed. As for implant position, anteversion of the femoral implant was set to be the same as natural antetorsion of the femoral neck, and the acetabular component was set 45° of total anteversion in all cases.
Results
We found a significant decrease in Flex ROM and Int-R inversely proportional to femoral antetorsion. In patients with lower antetorsion, Flex ROM and Int-R decreased due to bony impingement (the anterior great trochanteric region of the femur impinges on the anteroinferior edge of the anteroinferior iliac spine). However, in Ext-R, there was no relationship between ROM and femoral antetorsion.
Conclusions
We demonstrated that lower femoral antetorsion substantially affects Flex ROM and Int-R due to bony impingement. For these patients, consideration must be given to retaining femoral anterior offset in THA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total hip arthroplasty (THA) has been one of the most successful operative interventions for improving quality of life (QoL) in patients with severe degenerative osteoarthritis (OA). However, there are several complications with THA, and dislocation is one of the most serious complications for patients and surgeons. It has continued to be a frequent complication over the past several years, and the incidence of dislocation after primary THA is reported to be 1.7–4 % [1–3]. The factors that are associated with increased risk of dislocation include implant design, alignment, large femoral head, surgical approach and status of soft tissues [4, 5]. In addition, patient factors that influence dislocation are gender, advanced age and history of previous hip surgery [6, 7]. Many studies have analysed the variables that affect the range of motion (ROM) after THA. Bartz et al. noted three different mechanisms of dislocation: (1) implant impingement, (2) bony impingement and (3) spontaneous dislocation [8]. Previous clinical reports have shown the several procedures such as implant positioning in a “safe zone” described by Lewinnek [9], use of the combined anteversion concept [10] and using larger femoral heads to avoid implant impingement [11, 12]. However, once bony impingement becomes a main cause of impingement and restriction of hip motion following THA, dislocation can occur even with optimally positioned implants and large femoral head. With regard to the femoral component, high-offset and femoral-component antetorsion are important factors for proper hip stability. Antetorsion for the femoral component is generally recommended to be between 10° and 30° [13, 14]. However, these studies address the issue from the perspective of implant impingement, and there is no report detailing how femoral antetorsion can affect ROM after THA due to bony impingement.
Pre-operative planning is often performed for THA and computer simulation analysis to predict optimal implant settings and analyse ROM after THA [15–18]. In this study, we evaluated the influence of femoral antetorsion on ROM after THA using computed tomography (CT)-based 3D dynamic motion analysis.
Patients and methods
In this study, we retrospectively reviewed 71 patients (71 hips) comprising 11 men and 60 women who underwent THA with a titanium/molybdenum/zirconium/ferrous (AccoladeII TMZF) stem and Trident acetabular PSL and the hemispherical cup systems (Stryker Orthopedics/Howmedica, Mahwah, NJ, USA). Implant sizes were no. 3–5 stem and 48- to 52-mm-diameter cup for excluding the factor of bony anatomy, which is related to dislocation [19]. Mean patient age at surgery was 65.1 (45– 83) years. Hip diagnoses were osteoarthritis (OA) in 67 joints and osteonecrosis of the femoral head in four. We excluded patients who had had a previous operation or a severely dislocated hip. A subset of patients with complete implant data was reviewed for sizing. All patients had a pre-operative CT scan of their hip joint, from the anterior superior iliac spine (ASIS) to the knee joint through the distal femoral condyles using a 320-row multidetector helical CT scanner (Aquilion ONE, Toshiba Medical Healthcare, Tochigi, Japan) (detector configuration 80 × 0.5, beam collimation 40 mm) with a reconstructed slice width of 1 mm and a slice interval of 1 mm. CT data were transferred to the planning module. Ethics approval was granted by the Institutional Review Board.
Three-dimensional motion analysis
CT-based simulation software (ZedHip Lexi Co., Ltd., Tokyo, Japan) [19] was used to create virtual 3D bone models and perform virtual simulations of the femoral cut and component setting using pre-operative THA planning mode. This software allows generation and separation of independent femoral and acetabular 3D models. Based on a CT scan of pelvis and femur, reference points were digitised, then a 3D reconstruction of the bone model was made semiautomatically. If there was noise, they were revised manually. Next, component size and 3D orientation relative to host bones were planned, and implantation was performed in a multiplannar reconstructed (MPR) view. This software allows ROM simulation and calculation until contact occurs between bones and components. It also visualises the site of impingement in 3D axial/sagittal/coronal views of MPR images. The pelvic coordinate system was the functional pelvic plane, and the femoral coordinate system was defined by the centre of the femoral head, centre of the knee and both femoral condyles. Antetorsion angle of the femoral neck to the transepicondylar axis of the knee was measured as a parameter of antetorsion on the axial plane in the simulation.
Implant positioning and setting
The simulated implant was the Accolade II TMZF stem with a 36-mm-diameter alumina head, a neck of standard length and a Trident acetabular PSL cup with a PE insert without marginal lips in all cases. Femoral implant size was chosen to maximise both fit and fill in the femoral metaphysic and the acetabular component size to maximise fit and fill in the acetabulum, both under the consideration of implant size used in the operation. For implant position, the femoral shaft axis was placed in the centre of the original femoral diaphysis, whereas anteversion was set to be the same as the natural rotation of the femoral neck in all cases. Acetabular component position was at the site of the original acetabulum. Cup anteversion was set to 45° total anteversion and abduction in a radiographic manner in all cases [20]. Any acetabular osteophytes attached to the acetabular bony rim were removed.
ROM and impingement-site calculations
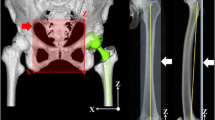
The centre of the femoral head is located by fitting a sphere to the articular surface of the femoral head. The pelvis was fixed in space, whereas the femur was free to translate in all directions but was constrained to rotate around the rotational centre of the hip. The computer software was capable of detecting both bone-to-bone, bone-to-implant and implant impingement, which allowed maximum ROM to be defined as the degrees of movement before impingement of either bone or implant occurred. The location of this impingement on both femoral and acetabular side and the position of the femur in space relative to the fixed pelvis can be also defined in the model (Fig. 1a–d). Based on this computerised analysis, ROM was measured in the directions that are important for dislocation and activities of daily living (ADL): flexion (Flex) with 0° adduction and internal rotation (Int-R), Int-R in 90° of flexion with 0° adduction, and external rotation (Ext-R) in 10° of extension with 0° adduction.
Evaluation design
To evaluate the relationship between femoral antetorsion, ROM after THA and impingement site, three evaluations were performed:
-
1.
Analysis of the relationship between ROM and femoral antetorsion
-
2.
Analysis of the relationship between impingement site and femoral antetorsion
-
3.
Comparison of ROM between patients with a low angle of femoral antetorsion (< 10°) (low antetorsion group) and a high angle of femoral antetorsion (> 25°) (high antetorsion group).
Statistical analysis
All data are expressed as mean ± standard deviation (SD) ,and statistical analysis was performed using Stat-View-J version 5.0 software (Hulinks, Tokyo, Japan). Correlations were evaluated using Pearson's chi-squared test. P value < 0.01 was considered statistically significant.
Results
Analysis of the relationship between ROM and femoral antetorsion
Mean femoral antetorsion was 22.4 ± 10.0°.; mean ROM in simulation was 114.2 ± 11.9° in Flex, 28.6 ± 13.7° in Int-R and 37.7 ± 5.2° in Ext-R. There was no significant correlation between stem size and Flex ROM (R 2 0.01; P > 0.01), Int-R (R 2 0.01; P > 0.01) and Ext-R (R 2 0.05; P > 0.01), which indicates no significant correlation between ROM and femoral size. There were positive correlations between antetorsion and Flex ROM (R 2 0.4; P < 0.0001) and strong positive correlation between antetorsion and Int-R ROM (R 2 0.6; P < 0.0001), respectively (Fig. 2a, b). However, there was no significant correlation between antetorsion and Ext-R ROM (R 2 0.08; P > 0.01) (Fig. 2c). Some cases produced result of a maximum of 10° in Int-R, especially in excessively low anteverted cases (Fig. 2b).
Analysis of the relationship between impingement site and femoral antetorsion
Impingement occurred in two ways: bone-to-bone and cup-to-neck impingement. Bony impingement preceded cup–neck impingement in many cases, especially in Flex and Int-R. In Flex, bony impingement was observed in 62 cases; the anterior great trochanteric region of the femur impinges on the anteroinferior edge of the anteroinferior iliac spine (AIIS) (Fig. 3a). There were nine cases of cup–neck impingement, primarily in patients with higher femoral antetorsion (Fig. 3c). In Int-R, there were 60 cases of bony impingement: the anterior great trochanteric region of the femur or femoral neck at the cutting point impinges on the anteroinferior edge of AIIS (Fig. 3b). Another 11 cases involved cup–neck impingement. In Flex and Int-R, only bony impingement was observed in patients with lower antetorsion, whereas cup–neck impingement was observed only in patients with higher antetorsion. In Ext-R, cup–neck impingement was observed in 54 cases and bony impingement–lesser trochanter impinged on ischial bone in 17 cases (Fig. 3d). When the site of impingement was plotted to the previous graph (Flex–antetorsion, Int-R–antetorsion and Ext-R–antetorsion), Flex ROM and Int-R decreased for bony impingement as femoral antetorsion became lower (Fig. 4a, b). Besides, Flex and Int-R ROM was restricted for implant impingement as femoral antetorsion increased. However, there was no tendency towards Ext-R (Fig. 4c).
Impingement site in relation to antetorsion of the femur. a Flexion, antetorsion: blue dots indicate bony impingement [anterior superior iliac spine (AIIS) on greater trochanter] and red dots indicate cup–neck impingement. b Internal rotation, antetorsion: blue dots indicate bony impingement (AIIS on femoral neck or great trochanter) and red dots indicate cup–neck impingement. c. External rotation, antetorsion: red dots indicate cup–neck impingement, blue dots indicate bony impingement. 448 × 288 mm (72 × 72 DPI)
Comparison of ROM between the patients with a low angle of natural antetorsion of the femur (< 10°) and a high angle of natural antetorsion (> 25°)
In the low-antetorsion group, 29 hips (two men and 27 women) and in the high antetorsion group, 11 hips (three men and eight women) were assessed. Mean antetorsion was 32.5 ± 4.1° in the low and 7.8 ± 2.2° in the high antetorsion group. In the latter group, mean ROM was 121.2 ± 8.3 in Flex, 39.0 ± 10.4° in Int-R and 39.1 ± 6.8° in Ext-R, whereas it was 99.7 ± 10.7 in Flex, 11.2 ± 9.0° in Int-R and 36.5 ± 3.6° in Ext-R in the former group. As for Flex ROM and Int-R, there were significant differences between groups (Flex P < 0.0001,;Int-R P < 0.0001). However, there was no significant difference between groups in Ext-R (P = 0.2)
Discussion
Impingement is often the main aetiology for post-THA instability. Dislocation can occur subsequent to impingement between the two components or between the acetabulum and the proximal femur. Widely recognised mechanisms to reduce the incidence of impingement include meticulous component positioning and the use of larger-diameter femoral heads or dual-mobility cup [5, 11, 12]. Implant malposition is a common contributor to impingement, and multifold models have been developed to determine the optimal combination of cup inclination, cup anteversion and stem antetorsion for maximising ROM and minimising the risk of impingement. Previous studies show detailed implant positions by which to acquire a satisfactory ROM. Widmar et al [15]. reported the formula for the theoretically optimal combination of cup and stem from a 3D computer model, and several studies support “the combined femoral and acetabular anteversion concept” and propose it should be from 25° to 50° to avoid impingement or dislocation [10].
These appropriate orientations of the implant and large femoral head are important factors for preventing implant impingement; however, once bony impingement becomes a main cause of impingement and restricts hip motion, dislocation can occur, even with optimally positioned implants and a large femoral head. Using a still CT frame, Suzuki et al. reported that bony impingement frequently limits hip motion after THA independent of ROM of prosthetic components [21]. As for femoral heads of larger diameter, likewise, several studies show that ROM after THA with a larger-diameter femoral head is not limited by implant impingement but by bony impingement [8, 16, 22]. Although there are several reports about bony impingement, the causative variables have largely remained unknown, and surgeons have traditionally relied on high-offset femoral stems, longer and larger modular heads, elevated liners and removal of the acetabular bony rim to avoid hip instability. With regard to femoral component, high offset and femoral component version are important factors for proper hip stability. Unequivocally, excessive anteversion or retroversion was thought to lead to component dislocation; however, less has been written about the importance of femoral antetorsion in the context of bony impingement. In this study, we took a subject-specific approach to analyse the effect of femoral antetorsion on restricting hip ROM after THA due to bony impingement.
Pre-operative planning can now be executed with high accuracy for THA, and optimal implant orientation in relation to impingement was evaluated by many investigators using CT simulation analysis [15–18, 23]. Such analysis offers a template of information regarding location of the impingement region and provides feedback on anticipated improvement in RON in vivo.
In our study, antetorsion of the femoral component was set to be the same as that of natural femoral anteversion; cup abduction was 45°, whereas cup anteversion was set to 45° of the combined anteversion to avoid prosthetic impingement based on the combined anteversion concept. Our results show that the lower the angles of femoral antetorsion, the more the Flex ROM and Int-R decreased. Moreover, the location of initial contact was not at the cup–neck region but consistently at the greater trochanteric or femoral neck regions on the anteroinferior aspect of AIIS in patients with lower femoral antetorsion and at the cup–neck region in patients with higher femoral antetorsion. These phenomena in bony impingement were also mentioned by several authors [24, 25]. Bartz et al., reported that osseous impingement was likely to occur between the greater trochanter and the iliac bone before implant impingement in a cadaver study [8] These results indicate that hip ROM after THA decreases due to bony impingement in patients with lower femoral antetorsion. However, excessive anteversion may lead to implant impingement. We define anterior offset as the distance between the line on the anterior aspect of the proximal femur and the centre of the stem head. Kessler et al. anticipated that the head–neck ratio of the native femur would correlate with overall hip ROM before bony impingement in THA [12]. Hence, it is important to retain anterior offset in order to avoid bony impingement and to improve ROM of Flex and Int-R, especially in patients with lower femoral antetorsion. From the viewpoint of bony impingement, cup positioning and increasing head diameter without retaining the femoral anterior offset has no further effect on improving ROM. Our results suggest that elongation of stem offset and/or use of a femoral implant and appropriate anteversion setting may increase hip ROM after THA. Furthermore, results showing that bony impingement often occurs at the anteroinferior aspect of AIIS also forewarn against excessive medialisation or superiolisation of the hip centre in cup positioning. If bony impingement is observed as a restricting factor in these conditions, resection of the bony impingement site (anterior aspect of the femoral neck and greater trochanter or anteroinferior aspect of the AIIS) may reduce the incidence of posterior dislocation by allowing increased ROM in Flex and Int-R until bony impingement. This would be a seriously consideration in patients with ow femoral antetorsion. These factors can be assumed preoperatively, so these phenomena must be taken into consideration during THA planning.
There are several limitations in our study. Firstly, the influence of surrounding soft tissue was not taken into account, which may have affected actual hip ROM. Secondly, we only analysed ROM until impingement. Hip dislocation involves levering the head out of the cup after impingement, so a larger head size may have the advantage of reducing dislocation by providing a jumping distance, even if the impingement-restricted ROM remains the same.
In summary, we demonstrated that natural femoral anteversion substantially affects Flex and Int-R ROM, especially in patients with a low degree of natural femoral antetorsion. For these patients, bony impingement of the proximal femur on AIIS may have a significant impact on dislocation. Therefore, we should consider retaining femoral anterior offset by using a femoral implant with increased anteversion, cemented implant, elongation of stem offset and/or resection of the bony impingement site in THA.
References
Caton J, Prudhon JL (2011) Over 25 years survival after Charnley's total hip arthroplasty. Int Orthop 35(2):185–188
D’Lima DD, Urquhart AG, Buehler KO, Walker RH, Colwell CW Jr (2000) The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head–neck ratios. J Bone Joint Surg Am 82:315–321
Bozic KJ, Lau EC, Ong KL, Vail TP, Rubash HE, Berry DJ (2012) Comparative effectiveness of metal-on-metal and metal-on-polyethylene bearings in Medicare total hip. J Arthroplasty 27(8):37–40
Caton JH, Prudhon JL, Ferreira A, Aslanian T, Verdier R (2014) A comparative and retrospective study of three hundred and twenty primary Charnley type hip replacements with a minimum follow up of ten years to assess wether a dual mobility cup has a decreased dislocation risk. Int Orthop 38(6):1125–1129
Nevelos J, Johnson A, Heffernan C, Macintyre J, Markel DC, Mont MA (2013) What factors affect posterior dislocation distance in THA? Clin Orthop Relat Res 471(2):519–526
Morrey BF (1997) Difficult complications after hip joint replacement. Dislocation. Clin Orthop Relat Res 344:179–187
Jolles BM, Zangger P, Leyvraz PF (2002) Factors predisposing to dislocation after primary total hip arthroplasty. A multivariate analysis. J Arthroplasty 17:282–288
Bartz RL, Nobel PC, Kadakia NR, Tullos HS (2000) The effect of femoral component head size on posterior dislocation of the artificial hip joint. J Bone Joint Surg Am 82:1300–1307
Lewinnek GE (1978) Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am 60:217–220
Dorr LD, Malik A, Dastane M, Wan Z (2009) Combined anteversion technique for total hip arthroplasty. Clin Orthop Relat Res 467(1):119
Lachiewicz PF, Soileau ES (2013) Low early and late dislocation rates with 36- and 40-mm heads in patients at high risk for dislocation. Clin Orthop Relat Res 471(2):439–443
Garbuz DS, Masri BA, Duncan CP, Greidanus NV, Bohm ER, Petrak MJ, Della Valle CJ, Gross AE (2012) Dislocation in revision THA: do large heads (36 and 40 mm) result in reduced dislocation rates in a randomized clinical trial? Clin Orthop Relat Res 470(2):351–356
Dorr LD, Wan Z, Malik A, Dastane M, Deshmane P (2009) A comparison of surgeon estimation and computed tomographic measurement of femoral component anteversion in cementless total hip arthroplasty. J Bone Joint Surg Am 91:2598–2604
D’Lima DD, Urguart AG, Buehler KO, Walker RH, Colwell CW (2000) The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head neck ratios. J Bone Joint Surg Am 82:315–321
Widmer KH, Zurfluh B (2004) Compliant positioning of total hip components for optimal range of motion. J Orthop Res 22:815–821
Kessler O, Patil S, Stefan W, Mayr E, Colwell CW, D’Lima DD (2008) Bony impingement affects range of motion after total Hip arthroplasty: a subject-specific approach. J Orthop Res 26(4):443–452
Rousseau MA, Lazennec JY, Boyer P, Mora N, Gorin M, Catonné Y (2009) Optimization of total hip arthroplasty implantation: is the anterior pelvic plane concept valid? J Arthroplasty 24(1):22–26
Incavo SJ, Thompson MT, Gold JE, Patel RV, Icenogle KD, Noble PC (2011) Which procedure better restores intact hip range of motion: total hip arthroplasty or resurfacing? A combined cadaveric and computer simulation study. J Arthroplasty 26(3):391–397
Shoji T, Yasunaga Y, Yamasaki T, Mori R, Hamanishi M, Ochi M (2013) Bony impingement depends on the bone morphology of the hip after total hip arthroplasty. Int Orthop 37:1897–1903
Ranawat CS, Rao RR, Rodriguez JA, Bhende HS (2001) Correction of limb length inequality during total hip arthroplasty. J Arthroplasty 16:715–720
Suzuki K, Matsubara M, Morita S, Muneta T, Shinomiya K (2002) CT image evaluation of the internal rotation limit prior to bony impingement after total hip arthroplasty. J Orthop Sci 7:433–438
Burroughs BR, Hallstrom B, Golladay GJ et al (2005) Range of motion and stability in total hip arthroplasty with 28-, 32-, 38-, and 44-mm femoral head sizes. J Arthroplasty 20(1):11–19
Schileo E, Taddei F, Cristofolini L, Viceconti M (2008) Subject-specific finite element models implementing a maximum principal strain criterion are able to estimate failure risk and fracture location on human femurs tested in vitro. J Biomech 41:356–367
Dorr LD, Wan Z (1998) Causes of and treatment protocol for instability of total hip replacement. Clin Orthop Relat Res 335:144–151
Dorr LD, Wolf AW, Chandler R et al (1983) Classification and treatment of dislocations of total hip arthroplasty. Clin Orthop 173:151–158
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shoji, T., Yasunaga, Y., Yamasaki, T. et al. Low femoral antetorsion and total hip arthroplasty: a risk factor. International Orthopaedics (SICOT) 39, 7–12 (2015). https://doi.org/10.1007/s00264-014-2452-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-014-2452-5