Abstract
Purpose
The influence of physiologic femoral bowing on range of motion (ROM) after total hip arthroplasty (THA) remains unknown. The purpose of this study was to investigate the morphology of the femur in patients who underwent THA, and to analyze the influence of femoral bowing on ROM due to implant impingement after THA.
Methods
The ROM was calculated from 100 hips in 90 patients who underwent THA using computed tomography data with a 3D dynamic analysis software. Lateral and anterior bowing angles of the femur were measured. A modular implant (Modulus system, Lima Corporate, Villanova di San Daniele del Friuli, Italy) was used for simulation. In all subjects, cup inclination, anteversion, and stem anteversion were set to 40°, 15°, and 30°, respectively. Multiple linear regression analyses were performed to assess the relationship between the morphology of the femur and ROM.
Results
Lateral bowing of the femur was demonstrated to be significantly correlated with age (r = 0.361, p < 0.001) and female sex (r = 0.315, p = 0.001). Lateral bowing of the femur was significantly positively correlated with flexion and internal rotation (Int-R) with 90° flexion. Anterior bowing was significantly associated with decreasing flexion, decreasing Int-R with 90° flexion and increasing Int-R with 45° flexion and 15° adduction.
Conclusions
A ROM-optimized cup position cannot be calculated from femoral stem anteversion values alone; therefore, when surgeons position the cup in relation to the femoral stem anteversion, the influence of femoral bowing may also require consideration.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Proper positioning of both the acetabular and femoral components during total hip arthroplasty (THA) minimizes the risk of implant impingement, which can lead to post-operative complications such as dislocation, cup loosening and breakage or accelerated wear of the cup liner [1,2,3]. Studies have indicated that several options can be utilized to acquire a satisfactory range of motion (ROM) [4, 5]. Widmar et al. reported a combined anteversion theory for implant impingement after THA when the cervico-diaphyseal angle (CDA) of the femoral component was set to 130° [4]. Similarly, the CDA of the femoral component has been demonstrated to influence the ROM after THA [5].
Asian patients undergoing total knee arthroplasty for medial osteoarthritis commonly were reported to exhibit more severe lateral femoral bowing, compared with healthy Western subjects [6]. Notably, lateral bowing of the femoral shaft was recently reported to increase with aging in a Japanese population [7, 8]. The femoral component of THA could follow the physiologic anterior bowing of the proximal femur during insertion into the medullary canal, which creates a deviation between the femoral shaft and the cranial-caudal axis of the femoral coordinate system. Previous studies have suggested that femoral component anteversion may be influenced by femoral anterior bowing [9, 10]. However, the influence of physiologic femoral bowing on the ROM after THA has generally been overlooked. To the best of our knowledge, no authors have quantitatively evaluated the physiologic bowing of the femur from the perspective of THA.
The aims of this study were to investigate the morphology of the femur in patients who underwent THA, and to analyze the influence of femoral bowing on ROM due to implant impingement after THA.
Materials and methods
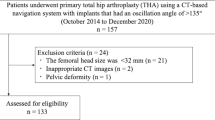
Patients and study design
All study protocols were approved by our institutional review board. All patients gave their consent for the use of their data prior to surgery.
A total of 106 consecutive primary THAs, which were undertaken between January 2015 and May 2016 in 96 patients, were assessed in this study. Three hips with a history of femoral surgery and three hips diagnosed with femoral neck fracture were excluded. Following exclusions, the present study included 100 hips in 90 patients (Table 1). In all patients, computed tomography (CT) images from the pelvis to the knee for CT-based navigation were pre-operatively captured at a voxel size of 0.70-0.78 mm in the planar view, and in 1.25 mm sections using a 64-slice scanner (Optima CT660, GE Medical Systems, Inc., Little Chalfont, UK).
Data were saved in a standard digital imaging and communications in medicine format and imported into CT-based simulation software (ZedHip; Lexi Co., Ltd., Tokyo, Japan) on a SONY VAIO workstation (SONY, Inc., Tokyo, Japan). ZedHip software was used to create virtual 3D bone models and perform virtual simulations of the component settings, using the pre-operative THA planning mode [5, 11]. The system was run under Windows 7 Professional on an Intel Core i7 computer (1.87 GHz, 8.0 GB RAM).
Coordinate system
As a patient specific coordinate system, practically, only the femoral coordinate system was used in the present study (Fig. 1). The femoral coordinate system was based on the retrocondylar plane, including the most posterior points of both femoral condyles and the most posterior points of the greater trochanter of the femur. The Y-axis was perpendicular to the retrocondylar plane, whereas the Z-axis was parallel to the line between the trochanteric fossa and the centre of the knee projected on the retrocondylar plane. The centre of the knee was defined as the tip of the intercondylar fossa. The X-axis was perpendicular to the Y- and Z-axes. The X-, Y-, and Z-axes pointed to the right, anterior, and superior direction, respectively (Fig. 1).
Definitions of the coordinate system. An inferred pelvic coronal plane (solid red arrow) was used to describe the acetabular cup orientation (a). The X-, Y-, and Z-axes point to the right, anterior, and superior direction, respectively. The femoral coordinate system is based on the retrocondylar plane (solid white arrow), including the most posterior points of both femoral condyles and the most posterior points of the greater trochanter of the femur (b, c). The Y-axis is perpendicular to the retrocondylar plane (c), whereas the Z-axis is parallel to the line between the trochanteric fossa and the centre of the knee (yellow line) projected on the retrocondylar plane (b, c). The X-axis is perpendicular to the Y- and Z-axes (b)
Simulation of implantation
Simulated implantation was performed in a multiplanar reconstructed view of the ZedHip software (Fig. 2). A Trident® hemispherical cup (Stryker Orthopedics, Mahwah, NJ, USA) with an outer diameter arbitrarily set to 50 mm, with a highly cross-linked polyethylene liner (X3™) without marginal lips (Stryker Orthopedics, Mahwah, NJ, USA), was used to simulate the implantation of a cup. Radiographic definition of an inferred pelvic coronal plane was used to describe the acetabular cup orientation [12] (Fig. 1). The X-axis was the medial-lateral axis, the Y-axis pointed to the anterior direction, and the Z-axis pointed in the cranial direction in the inferred pelvic coordinate system. In all cases, the radiographic inclination and anteversion were set to 40° and 15°, respectively.
The Modulus system (Lima Corporate, Villanova di San Daniele del Friuli, Italy) was used to simulate the implantation of a stem. This system consists of a cementless conical tapered stem, coupled axially with a modular neck that rotates 360° around the stem axis, regardless of the type of rotational deformity of the proximal femur. Femoral stem size was chosen to maximize the fit and fill in the medulla of the proximal femoral shaft along with the axis of the original proximal femoral diaphysis, by aligning the cranial-caudal position of the prosthetic femoral head with that of the original femoral head (Fig. 2). There are two neck-stem connection tapers to choose from, A (for stem size 13-15 mm) and B (for stem size 16-26 mm). As the minimum size of the femoral stems used in the present study was 16 mm, the type B neck-stem connection taper was used in each case. There are four different models in the modular necks: two CDAs (125° and 135°) and two lengths along the cervical axis (short and long). In this study, for simplification, both the 125° and 135° necks used were short. The angle between the femoral component neck axis projected to the XY plane of the femur and the posterior intercondylar line projected to the XY plane of the femur was defined as the anteversion of the femoral component (Fig. 1). Anteversion of the femoral component was set to 30° in all cases. A 32-mm-diameter femoral head was used with a modular head of standard length in all subjects. This combination of cup and stem orientation was based on a simplified version of the combined anteversion theory [13].
Simulation of ROM
The centre of the femoral head coincided with that of the articulating prosthetic cup. In this study, neutral hip position was defined as the position in which all corresponding axes in the femoral and the inferred pelvic coordinate systems were parallel (Fig. 1).
ZedHip software was used to analyze implant impingement, with the maximum ROM defined as the degrees of movement prior to the occurrence of implant impingement. Degrees of movement were calculated to the nearest 0.5°.
The maximum ROM was measured during flexion, extension, abduction, adduction, and the directions that are important for dislocation: internal rotation (Int-R) with 90° flexion and 0° adduction, Int-R with 45° flexion and 15° adduction, and external rotation (Ext-R) with 0° extension and 0° adduction.
Morphology of the femur
Based on the femoral coordinate system, digitally reconstructed radiographs (DRR) of the femur were constructed on the coronal, sagittal, and axial planes from the pre-operative CT images using the ZedHip software, to measure lateral bowing, anterior bowing, and anteversion of the femur, respectively.
Lateral bowing of the femur was measured on the coronal plane of the DRR [6]. Lateral bowing of the femur was defined as the angle between the line connecting the points bisecting the femur at 0 cm and 5 cm below the lowest portion of the lesser trochanter, and the line connecting the points bisecting the femur at 5 cm and 10 cm above the lowest portion of the lateral femoral condyle (Fig. 3).
Measurements of lateral bowing of the femur. On the coronal plane of the digitally reconstructed radiographs of the femur, lateral bowing of the femur was defined as the angle between the line connecting the points bisecting the femur at 0 and 5 cm below the lowest portion of the lesser trochanter, and the line connecting the points bisecting the femur at 5 and 10 cm above the lowest portion of the lateral femoral condyle
Anterior bowing of the femur was measured on the sagittal plane of the DRR [14]. Anterior bowing of the femur was assessed using the angle between the medullary lines of the proximal and distal femur. Proximal medullary lines were drawn as the line connecting the two points 10 and 15 cm distal to the proximal end of femoral head, and distal medullary lines as the line connecting the two points 5 and 10 cm proximal to the distal end of the medial femoral condyle (Fig. 4).
Measurements of anterior bowing of the femur. On the sagittal plane of the digitally reconstructed radiographs of the femur, anterior bowing of the femur was assessed using the angle between the medullary lines of the proximal and distal femur. Proximal medullary lines were drawn as the line connecting the two points 10 and 15 cm distal to the proximal end of the femoral head, whereas distal medullary lines were drawn as the lines connecting the two points 5 and 10 cm proximal to the distal end of the medial femoral condyle
Femoral anteversion was measured on the axial plane of the DRR just proximal to the lesser trochanter and on the axial slice where the femoral condyles were the largest [15]. The axis of the femoral neck was calculated as the line-of-best-fit connecting slices taken through a central segment of the neck. Femoral anteversion was defined as the angle between the axis of the neck and a line connecting the posterior femoral condyles (Fig. 5).
Measurements of anteversion of the femur. Femoral anteversion was measured a on the axial plane of digitally reconstructed radiographs just proximal to the lesser trochanter and b on the axial slice where the femoral condyles were largest. The axis of the femoral neck was calculated as the best-fit line connecting slices taken through a central segment of the neck. Femoral anteversion was defined as the angle between the axis of the neck and a line connecting the posterior femoral condyles
Statistical analysis
Mann-Whitney U tests were performed to compare data between men and women. To compare the 125° and 135° necks for implant impingement after THA, Wilcoxon signed-rank tests were performed.
Simple linear regression analyses were performed using Spearman’s rank correlation coefficient for the following anthropometric parameters: age, sex, body mass index (BMI), lateral bowing, anterior bowing, and anteversion of the femur.
Multiple linear regression models were used to analyze the influence of lateral and anterior bowing and anteversion of the femur (independent variables) on each ROM (dependent variable). The variables were included in a forward stepwise manner, with an entrance criterion of p < 0.05 and an exit criterion of p > 0.10. The variables in the final model were centralized to adjust for possible multi-collinearity.
Statistical analyses were conducted using SPSS for Windows (version 23.0; IBM, Armonk, NY, USA) and P values of <0.05 were considered to indicate statistical significance.
Results
The study participants were diagnosed with the following: osteoarthritis (89 hips), idiopathic osteonecrosis of the femoral head (six hips), osteonecrosis of the femoral head following a fracture of the femoral neck (three hips), rapidly destructive coxarthropathy (one hip), and rheumatoid arthritis (one hip). Demographic parameters are listed in Table 1. Lateral bowing of the femur was significantly more common in women compared with men (p = 0.002). The prosthetic ROM after THA when using the 125° and 135° necks is shown in Table 2. There were significant differences between ROM in the 125° neck and that in the 135° neck in each position (p < 0.001).
The correlation matrix for the anthropometric data is shown in Table 3. Lateral bowing of the femur was demonstrated to be significantly correlated with age (r = 0.361, p < 0.001), female sex (r = 0.315, p = 0.001), BMI (r = 0.204, p = 0.042), and anteversion (r = 0.273, p = 0.006).
Multiple linear regression analyses indicated that in both the 125° and 135° necks, lateral and anterior bowing of the femur tended to be independently correlated with each ROM, and lateral bowing tended to have an opposite effect on each ROM compared to anterior bowing (Tables 4 and 5). The anatomical femoral anteversion did not explain the variation of each ROM.
Discussion
This study investigated the morphology of the femur in patients who underwent primary THA, and the influence of physiologic bowing of the femur on prosthetic impingement after THA was analyzed. Due to individual variations in anatomy, the femoral component is positioned with a certain degree of anatomy [16]. The femoral component used in this study was a cone-type stem aligning regardless of the type of rotational deformity of the proximal femur. Therefore, this study analyzed the influence of the morphology of the femur on the ROM of implant impingement after THA.
In this study, using the 125° neck induced a greater ROM during flexion, adduction, and Int-R with 90° flexion and 0° adduction compared with the 135° neck; however, using the 125° neck lead to less ROM during extension, abduction, Int-R with 45° flexion and 15° adduction, and Ext-R with 0° extension and 0° adduction. Using a changeable neck system with the combined anteversion fixed, Shoji et al. reported that the decreasing CDA of the femoral component achieved a greater ROM between components in flexion and Int-R with 90° flexion and 0° adduction, whereas the decreasing CDA lead to less ROM between components in Ext-R with 0° extension and 0° adduction [5], which was consistent with the present results. Although they argued that implants with high CDA had a negative effect on the ROM during flexion and Int-R with 90° flexion and 0° adduction [5], this study demonstrated that Int-R with 45° flexion and 15° adduction was smaller in the 125° neck, compared with the 135° neck. Notably, high CDA had a positive effect on ROM in Int-R in the middle range of flexion (45° flexion). In this study, high CDA resulted in greater abduction and smaller adduction angles, respectively. Higher CDA can induce a larger lateral arc from the neck of the femoral component to the lateral inner edge of the liner. It is reasonable, therefore, that the femoral component with the higher CDA was able to achieve the largest abduction ROM of implant impingement.
In this study, lateral bowing of the femur significantly increased in women compared with men (P = 0.002), whereas no significant differences between men and women were detected in the anterior bowing of the femur. Nakano et al. reported that lateral femoral bowing gradually increased with aging in the general Japanese population without knee-related symptoms, and they also demonstrated greater lateral bowing of the femur in females, compared with males, particularly in young and middle-aged individuals [8]. These findings were consistent with the results of the present study. Harma et al. found no significant difference between male and female patients when measuring femoral medullary bowing on lateral radiography [17], which was also consistent with the present findings. These previous studies all investigated surgery, such as TKA, which aim to achieve neutral mechanical alignment. To the best of our knowledge, this study was the first to consider femoral bowing when assessing ROM after THA.
In this study, with both the 125° and 135° necks, lateral bowing of the femur tended to be significantly positively correlated with flexion, adduction, and Int-R with 90° flexion and 0° adduction. On the other hand, lateral bowing negatively correlated with extension, abduction, Int-R with 45° flexion and 15° adduction, and Ext-R with 0° extension and 0° adduction. Notably, if lateral bowing increases, the functional CDA decreases (Fig. 6). Therefore, reduction of the functional CDA leads to increases in flexion, adduction, and Int-R with 45° flexion and 15° adduction; however, smaller functional CDA causes decreasing extension, abduction, Int-R with 45° flexion and 15° adduction, and Ext-R with 0° extension and 0° adduction, which is in good agreement with the present results of comparison between ROM in the 125° and 135° necks.
Schematic of the concept of functional cervico-diaphyseal angle (CDA) of the femoral component of total hip arthroplasty. a Representative medial bowing of the femur. A Modulus stem with a 125° neck was implanted. Since the femur bowed medially, the functional CDA of the femoral component indicated 125.8°. b Representative lateral bowing of the femur. A Modulus stem with a 125° neck was implanted. Since the femur bowed laterally, the functional CDA of the femoral component indicated 118.5°
Increasing anterior bowing of the femur was demonstrated to be significantly associated with decreasing flexion, decreasing Int-R with 90° flexion and 0° adduction, and increasing Int-R with 45° flexion and 15° adduction. If anterior bowing of the femur increases, the femoral component may flex more at the neutral position. Therefore, it is reasonable that the extent of anterior bowing of the femur was negatively correlated with Int-R with 90° flexion and 0° adduction. However, it is paradoxical that anterior femoral bowing was positively correlated with Int-R with 45° flexion and 15° adduction. Although the mechanism underlying how anterior bowing of the femur is able to influence the Int-R ROM in a different manner between 45° and 90° flexion remains unclear, Renkawitz et al. reported that the flexion ROM decreased and the Int-R ROM at 45° flexion increased with the proximal part of the stem tilted toward the posterior, even when the same anteversion of the femoral component with 30–40° of cup inclination was applied [9]. These findings are in good agreement with this study.
This study has some potential limitations. Firstly, the present results may not be versatile, as only one prosthetic design was evaluated. However, the present femoral component was a cone type that was implanted with the stem axis parallel to the medulla of the proximal femoral shaft. Therefore, if the femoral component is aligned with the proximal shaft of the femur in a parallel manner, the present findings may be applicable to other designs. Secondly, the position of the acetabular and femoral component in this study was fixed by a pattern of alignment (cup inclination, 40°; cup anteversion, 15°; stem anteversion, 30°) based on the combined anteversion theory [4, 13]. Another alignment of the components may indicate different findings in relation to ROM. Thirdly, the present method was not able to evaluate bone-to-bone or bone-to-implant impingement as a pelvic bone model was not created, and the present pelvic coordinate system was inferred instead of being patient-specific. Further studies should take bone-to-bone or bone-to-implant impingement into consideration when evaluating the influence of femoral bowing on ROM after THA.
In conclusion, this study demonstrated that lateral and anterior bowing of the femur were independently correlated with each ROM after THA, and lateral bowing tended to have an opposite effect on each ROM compared to anterior bowing even though the implant alignment was consistent with avoiding the impingement based on the combined anteversion concept. Clinically, these findings are very important, particularly for surgeons following the concept of “combined anteversion” in THA. A ROM-optimized cup position cannot be calculated from anteversion values alone; therefore, when surgeons position the cup in relation to the femoral stem anteversion, particularly when using a cone-type stem, the influence of femoral bowing may also require consideration.
References
Shon WY, Baldini T, Peterson MG et al (2005) Impingement in total hip arthroplasty a study of retrieved acetabular components. J Arthroplast 20:427–435
Bader R, Steinhauser E, Zimmermann S et al (2004) Differences between the wear couples metal-on-polyethylene and ceramic-on-ceramic in the stability against dislocation of total hip replacement. J Mater Sci Mater Med 15:711–718
Barrack RL (2003) Dislocation after total hip arthroplasty: implant design and orientation. J Am Acad Orthop Surg 11:89–99
Widmer KH, Zurfluh B (2004) Compliant positioning of total hip components for optimal range of motion. J Orthop Res 22:815–821
Shoji T, Yamasaki T, Izumi S et al (2016) The influence of stem offset and neck shaft angles on the range of motion in total hip arthroplasty. Int Orthop 40:245–253
Lasam MP, Lee KJ, Chang CB et al (2013) Femoral lateral bowing and varus condylar orientation are prevalent and affect axial alignment of TKA in Koreans. Clin Orthop Relat Res 471:1472–1483
Matsumoto T, Hashimura M, Takayama K et al (2015) A radiographic analysis of alignment of the lower extremities — initiation and progression of varus-type knee osteoarthritis. Osteoarthr Cartil 23:217–223
Nakano N, Matsumoto T, Hashimura M et al (2016) Coronal lower alignment in normal knees- a radiographic analysis of 797 normal knee subjects. Knee 23:209–213
Renkawitz T, Haimerl M, Dohmen L et al (2012) The association between Femoral Tilt and impingement-free range-of-motion in total hip arthroplasty. BMC Musculoskelet Disord 13:65
Müller M, Abdel MP, Wassilew GI et al (2015) Do post-operative changes of neck-shaft angle and femoral component anteversion have an effect on clinical outcome following uncemented total hip arthroplasty? Bone Joint J 97-B:1615–1622
Imai N, Ito T, Suda K et al (2013) Pelvic flexion measurement from lateral projection radiographs is clinically reliable. Clin Orthop Relat Res 471:1271–1276
Murray DW (1993) The definition and measurement of acetabular orientation. J Bone Joint Surg Br 75:228–232
Sugano N, Tsuda K, Miki H et al (2012) Dynamic measurements of hip movement in deep bending activities after total hip arthroplasty using a 4-dimensional motion analysis system. J Arthroplast 27:1562–1568
Chung BJ, Kang YG, Chang CB et al (2009) Differences between sagittal femoral mechanical and distal reference axes should be considered in navigated TKA. Clin Orthop Relat Res 467:2403–2413
Sugano N, Noble PC, Kamaric E (1998) A comparison of alternative methods of measuring femoral anteversion. J Comput Assist Tomogr 22:610–614
Maruyama M, Feinberg JR, Capello WN, D’Antonio JA (2001) The frank Stinchfield award: morphologic features of the acetabulum and femur: anteversion angle and implant positioning. Clin Orthop Relat Res 393:52–65
Harma A, Germen B, Karakas HM et al (2005) The comparison of femoral curves and curves of contemporary intramedullary nails. Surg Radiol Anat 27:502–506
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All authors certify that our institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Akiyama, K., Shibuya, T. Influence of femoral bowing on range of motion after total hip arthroplasty. International Orthopaedics (SICOT) 42, 1795–1802 (2018). https://doi.org/10.1007/s00264-017-3732-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3732-7