Abstract
Purpose
The aim of this study was to evaluate patient-reported clinical outcome, instrumental stability and prevalence of radiological osteoarthritis (OA) based on a homogeneous patient sample after two years and on average ten years after isolated anterior cruciate ligament (ACL) reconstruction.
Methods
Primarily we performed ACL reconstruction using a four-strand semitendinosus tendon (ST) autograft in 112 patients. Two years after reconstruction 98 patients could be re-evaluated. Long-term clinical and functional follow-up assessment was then performed on 52 patients on average 10.2 years after operative treatment. Inclusion criteria consisted of an isolated ACL rupture, reconstruction with ST graft and no associated cartilage alterations and meniscal lesions. Clinical and functional follow-up assessment included the International Knee Documentation Committee (IKDC) score and the scores of Tegner and Lysholm. Instrumental stability testing was carried out with the KT1000™ arthrometer. The degree of degenerative changes and prevalence of OA was based on the Jäger-Wirth score.
Results
The mean long-term follow-up was 10.2 years (eight–13 years), and the mean age was 40.4 years (24–62 years). About 72 % of patients were graded A or B according to the IKDC score. Activity levels according to the scores of Tegner and Lysholm were 4.8 and 88.2 on long-term follow-up. Radiological assessment revealed degenerative changes in the sense of a grade I OA in 21.2 % of patients. Prevalence of a grade II OA was found in 53.8 % of patients. A grade III OA and a grade IV OA were found in 19.2 and 5.7 %. Correlation analysis showed significant relationships between the long-term stability and prevalence of OA (p < 0.05).
Conclusions
Arthroscopic ACL reconstruction using four-strand ST autograft resulted in high patient satisfaction and good clinical results at two years and long-term follow-up. The prevalence of higher degree OA that developed in about 25 % of patients is significantly correlated with long-term knee joint stability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rupture of the anterior cruciate ligament (ACL) represents a common injury, both in amateur and professional sports. Patients with a lesion of the ACL are characterised by difficulty with athletic performance and/or giving way symptoms in daily activities [1, 2]. The necessity of operative re-stabilisation is generally accepted [1–6]. ACL reconstruction surgery and techniques have changed over the past decades [7, 8]. Reconstruction using a bone-patellar tendon-bone graft (BPTB) and hamstring grafts (semitendinosus and gracilis graft) are the most commonly used procedures for ACL surgery [7, 8]. Anterior knee pain, decreased sensitivity of the knee and kneeling pain have been reported as donor-site morbidity after harvesting of BPTB grafts [9, 10]. With regard to reconstruction using hamstring grafts (HT) less donor-site complications have been reported. On the other hand increased femoral tunnel widening and weakness of the hamstring muscles postoperatively have been described as potential adverse events after HT reconstruction [11–13].
Restoration of long-term stability and free knee joint function remain basic treatment principles in order to avoid serious sequelae like meniscus and cartilage alterations and in particular progression of degenerative changes [3, 6, 14–17].
Meniscectomy, cartilage lesions or a prolonged interval from injury to reconstruction illustrate important factors for the onset of osteoarthritis (OA) [17–20]. With regard to the current literature many authors report successful short- and midterm results after ACL reconstruction [9, 21–27]. However, reports with follow-up periods of ten years or longer remain rare. The priority objective of this study was to evaluate long-term functional and clinical outcomes as well as the incidence of potentially pending OA based on a large study sample after isolated ACL rupture and operative restoration using four-strand semitendinosus tendon graft.
Material and methods
In the years 1999–2002, a total of 112 patients with an isolated ACL rupture were treated via four-strand semitendinosus tendon graft reconstruction at our institution. Only patients with an isolated ACL rupture confirmed during the arthroscopic reconstruction were included in this investigation. All other patients with significant intra- articular cartilage damage, concomitant meniscus lesions or higher degree osteoarthritic lesions (> grade I according to the Jäger-Wirth classification) were excluded. At the scheduled two year follow-up 98 patients could be re-evaluated according to functional and radiological scores. Of this patient sample a total of 52 (46.4 %) patients could be re-assessed on long-term follow-up an average of 10.2 years after primary reconstruction. Reasons for patient dropout from the long-term evaluation included intermittent partial or total medial meniscectomy, graft rupture due to new trauma and finally geographical limitations and reluctance to attend the follow-up examination. Based on these criteria long-term follow-up was performed on 52 patients (30 male/22 female). The average age was 40.4 years (24–62 years). In 39 cases the right knee joint was affected and in 13 the left knee. Long-term follow-up examination occurred on average 10.2 years (eight–13 years) after reconstruction
Operative technique and rehabilitation
ACL reconstruction was performed with the anatomical single-bundle technique with the patient under general anaesthesia with an interval from injury to surgery of about two to three weeks. The semitendinosus tendon was harvested (min. 26 cm long) through a 2.5-cm long incision centred 1 cm medial and 1 cm distal to the medial margin of the tibial tubercle. ACL reconstruction was then performed via so-called transtibial conventional single-bundle reconstruction, which represented the standard operative technique at our institution till 2004. The tibial tunnel was drilled using a drill guide under arthroscopic visualisation through the posterior part of the middle of the tibial ACL footprint. A tibial tunnel was created with a cannulated drill with a diameter matched to the width of the prepared graft. To create the femoral tunnel a 5-mm offset guide system was placed transtibially at the posterior margin of the intercondylar notch. A Kirschner wire was then drilled into the lateral femoral condyle at the 1:30 o’clock (or 10:30 o’clock) position. Then the drill system for EndoButton™ fixation (Smith & Nephew Endoscopy, Andover, MA. USA) was used to create a femoral tunnel. The graft was then passed and the EndoButton™ was flipped in the standard fashion for femoral fixation. Afterwards the knee was cycled from 0 to 120° approximately 25 times for preconditioning of the graft. Afterwards, tibial graft fixation was performed by Suture Disc™ fixation (Smith & Nephew Endoscopy, Andover, MA, USA) with the knee at full extension with a forced posterior drawer. Postoperatively, patients were immobilised in a full-extension orthesis for two days.
Full weight-bearing was allowed according to the patient’s pain level directly after the operation. Afterwards according to our concept of rehabilitation patients were treated with a flexion-limiting orthesis (ext./flex. 0°/0°/90°) for six weeks. After six weeks of rehabilitation there was no additional limitation of the range of motion of the operated knee. High-demand pivoting sports activities were allowed after six to nine months.
Assessments
The clinical and functional follow-up assessment was carried out according to the International Knee Documentation Committee (IKDC) score [28]. Further criteria of clinical evaluation were based on the scores of Tegner and Lysholm [29, 30]. Patients who scored more than 92 points were considered as excellent. Patients with Lysholm scores between 91 and 76 points were rated as good and scores less than 76 points were rated as fair/poor. Clinical evaluation using the IKDC score and the scores of Tegner and Lysholm was performed at 24 months after surgery and at final follow-up. Furthermore, the pre-trauma status was documented. Assessment of the anterior laxity was carried out with the KT1000™ arthrometer (MEDmetric® Corporation, San Diego, CA, USA) according to a modified IKDC grading system (degree of differential instrumental laxity in side comparison) [31]. Radiographic evaluation was performed using conventional radiographs in three planes to evaluate the incidence of radiographic tibiofemoral and patellofemoral knee OA. Radiographic evaluation of the pre-trauma status supplemented the overall radiographic assessment. The degree of OA was evaluated according to the Jäger-Wirth classification, a radiographic grading system accepted and commonly used in Europe, staging OA from grade I to grade IV [32]. Grades I and II of this classification were defined as minor osteoarthritic changes, and grades III and IV were defined as major osteoarthritic changes.
Statistical analyses
Statistical analysis was performed using the software SPSS version 17.0 for Windows. Correlations were regarded as significant at p < 0.05 concerning the Pearson chi-square test and the Kruskal-Wallis test.
Results
IKDC evaluation
Clinical evaluation according to the IKDC score showed a decline of the clinical results in the long-term course in comparison to the results at two year follow-up (Fig. 1).
Two years after ACL reconstruction, functional assessment according to the IKDC score revealed 27 patients (27.6 %) with an IKDC A score, 52 patients (53.1 %) with an IKDC B score, 16 patients (16.3 %) with a grade C score and 3 patients (3.1 %) were graded D according to the IKDC criteria.
On long-term follow up nine patients (17.3 %) with an IKDC grade A, 28 patients (53.8 %) with an IKDC grade B, seven patients (23.1 %) with an IKDC grade C and three patients (5.7 %) with a “severely abnormal clinical condition” (IKDC grade D) could be detected.
However, in total 72 % of all patients could be graded A or B according to the IKDC score. Reasons for worse clinical results according to the IKDC grading system included pain and progressive swelling of the knee joint with increasing load on the subjective IKDC questionnaire. Furthermore, an evident extension deficit, intermittent intra-articular effusion formation or a striking differential laxity on assessment with the Lachman test accounted for worse results in the objective IKDC evaluation.
Lysholm knee scoring scale/Tegner activity scale
Clinical assessment according to the Lysholm knee scoring scale and the Tegner activity scale showed a deterioration of the overall clinical constitution on long-term follow-up and is presented as mean value and range in Table 1.
Assessment of anterior laxity (Lachman test)
Instrumental assessment of anterior translation with the KT1000™ arthrometer showed a deterioration of the results on long-term follow-up in comparison with the two year results. However, overall long-term knee joint stability was satisfactory to excellent on average ten years after reconstruction (Table 2).
Prevalence of osteoarthritis
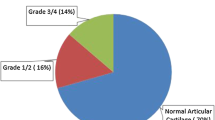
Radiographic assessment according to the Jäger-Wirth classification revealed no signs of degenerative changes in 101 patients (90.2 %) on pre-trauma assessment. In 9.8 % of the cases (11 patients) degenerative changes according to grade I OA were detected on radiographic assessment. Prevalence of grade II–IV OA was not detected on radiological pre-trauma assessment. At the two year follow-up and long-term follow-up a marked increase of degenerative changes was detected on radiological evaluation (Fig. 2).
Correlation analysis
Instrumental stability vs prevalence of osteoarthritis
Correlation analysis of the instrumental anterior laxity with the KT1000™ arthrometer and radiological evaluation of OA showed a significant correlation with p < 0.05. The analysis pointed out a significant increase of degenerative changes and progression of OA with concomitant decrease in long-term stability (Fig. 3).
Discussion
This retrospective clinical study evaluated clinical and radiological long-term outcomes after isolated ACL reconstruction using four-strand semitendinosus tendon autograft. The results from our study confirmed the hypothesis that long-term clinical outcome and prevalence of OA are correlated with restoration and conservation of stability after isolated ACL rupture. With regard to the current literature various studies have reported midterm and long-term results after ACL reconstruction with satisfactory to excellent clinical outcomes [6, 9, 22, 23, 25, 33, 34].
Limitations of the majority of these studies include variable intervals between injury and ACL reconstruction, concomitant meniscectomy procedures or variable rehabilitation programmes [2, 9, 15, 17, 18]. This study intended to identify factors associated with our long-term outcomes in particular focussing on long-term knee joint stability and prevalence of knee OA based on a homogeneous study sample with a standardised operative procedure and postoperative rehabilitation. Furthermore, the study only focussed on isolated ACL injuries. In contrast to other studies, all other patients with additional intra-articular injuries like cartilage alterations or concomitant meniscectomy procedures at the time of reconstruction or during the follow-up period were excluded.
Based on our results we found a decrease of the clinical condition and subjective functional outcome according to the IKDC score on long-term follow-up in comparison to the two year results. However, 72 % of all patients could be graded A or B according to the IKDC classification and 81 % judged the outcome as satisfactory according to the subjective criteria of the IKDC score on average ten years after reconstruction. These results were comparable to those found in the current literature [3, 6, 9, 23, 24, 35].
In a review of studies, Leys et al. and Mascarenhas et al. compared long-term clinical and radiographic results after ACL reconstruction with either BPTB graft or hamstring grafts reported that 85–92 % of patients were satisfied with their ACL reconstruction at long-term follow-up [34, 36]. Leys et al. and Mascarenhas et al. also reported high satisfaction rates and good to excellent clinical outcomes according to the IKDC classification (85–94 points on average) based on a population with similar age and overall constitution [34, 36].
Fox et al. and Lebel et al. focussing on ACL reconstruction using BPTB grafts reported that 91–98 % of patients were satisfied with their ACL reconstruction at follow-up [10, 22]. Lebel et al. and Möller et al. reported high satisfaction rates and excellent clinical outcomes according to the IKDC score (80–92 points on average) [22, 23]. Furthermore, Hoffelner et al. reporting on long-term clinical outcome and prevalence of OA after ACL reconstruction with hamstring grafts showed an excellent long-term IKDC score of 89.2 ± 9.3 points. The median pre-injury Tegner score was 8 ± 2, corresponding to 7 ± 2 at follow-up. In 68 % of patients, the Tegner score was unchanged from pre-injury to follow-up [21]. These results emphasise the fact that 10 years after ACL reconstruction, most of the patients had a nearly normal knee function.
Based on the emphasis of this study of isolated ACL injury and reconstruction, Wu et al. in a prospective study reported on 63 patients with isolated ACL rupture and reconstruction with BPTB graft. They reported a significant deterioration of the clinical condition with concomitant provision of meniscectomy or imperfect control of laxity and with increasing incidence of OA [20]. Hoffelner et al. focussing on athletes support these results comparing the incidence of OA after ACL reconstruction with the uninjured contralateral knee [21]. They reported ongoing signs of radiographic OA in 14 % of uninjured knees according to Kellgren and Lawrence, in comparison with 21 % of injured knees. The functional outcomes between the injured knee and uninjured knee did not show any statistical differences with regard to the criteria of the IKDC score or the scores of Tegner and Lysholm. The total Knee Injury and Osteoarthritis Outcome Score was 92.7 ± 7.8. The median pre-injury Tegner score was 8 ± 2, corresponding to 7 ± 2 at follow-up. In 68 % of patients, the Tegner score was unchanged from pre-injury to follow-up [21]. Mihelic et al. published a report comparing operative versus conservative treatment. They found significant differences in the mean IKDC score of the two groups and reported significant differences in the rate of OA in both groups with a significantly higher rate of OA in the conservative treatment group. Furthermore, they report the highest rate of OA with concomitant meniscectomy [4].
Our clinical long-term evaluation of functional and activity levels according to the scores of Lysholm and Tegner showed a deterioration of the patients’ overall clinical constitution in comparison to the results two years after reconstruction. The median Tegner score of 4.8 at final follow-up is similar in comparison to studies with more than ten years of follow-up which have reported Tegner scores between 4 and 6 [21, 23, 25, 34, 35]. The mean Lysholm score of nearly 90 points was similar to other studies with similar follow-up periods that have reported scores of 82–94 [3, 9, 21, 24, 25, 35]. Reasons for worse clinical results according to the scores of Tegner and Lysholm included pain and progressive swelling of the knee joint with increasing load. Furthermore, an evident extension deficit, intermittent intra-articular effusion formation or a striking differential laxity on assessment with the KT1000™ arthrometer accounted for worse results.
Evaluation of long-term anterior laxity showed deterioration in the long-term course but conservation of overall stability remained excellent; 84 % of all patients showed a differential laxity <3 mm on long-term evaluation. Overall instrumental stability performance is comparable with those found by Fox et al. and other study groups at midterm to long-term follow-up with 70–90 % of patients having a KT1000™ arthrometer result of less than 3 mm [5, 12, 24, 34].
In our study radiographic evaluation of OA revealed no signs of degenerative changes in 90.2 % of patients on pre-trauma assessment. At long-term follow-up a marked increase of the degenerative changes was detected in comparison to the midterm results. Radiographic evaluation showed mild to moderate degenerative changes (grade I or grade II) according to the Jäger-Wirth classification in about 75 % of all patients. Detection of a symptomatic OA in the sense of a grade III and grade IV OA was found in 19.2 and 5.7 % at final follow-up. The study could demonstrate a significant correlation for the prevalence of OA and performance on instrumental stability assessment on long-term follow-up (p < 0.05). We could show that deterioration of long-term stability is significantly correlated with progression of OA based on a study sample after isolated ACL reconstruction. On the other hand conservation of good long-term stability was not able to stop the onset of degenerative changes at all. With regard to the current literature there are various long-term investigations focussing on the prevalence of OA and potentially associated risk factors [5, 6, 15, 16, 24, 27, 33].
Holm et al. comparing hamstring and BPTB grafts showed no significant difference with regard to the prevalence of OA at ten years after reconstruction but on the other hand an increased rate compared with the contralateral knee [35]. Lidén et al. after seven years of follow-up found similar results and in particular an increased risk of developing OA if an associated meniscal injury was present at primary surgery [12].
Øiestad et al. performed a systematic review and found variable rates of OA after ACL reconstruction at ten to 15-year follow-up [24]. They found no significant differences in knee function and clinical condition between the isolated and combined injury groups. Subjects with combined injury had a significantly higher prevalence of radiographic knee OA compared to those with isolated injury (80 and 62 %), but no significant group differences were shown for symptomatic radiographic knee OA (42 and 36 %) [24]. Louboutin et al. reviewed risk factors for developing OA 20 years after injury and again reported a higher rate of osteoarthritic changes if meniscal injury was present. The same study also compared reconstructed knees to knees with cruciate ruptures managed non-operatively and found the reconstructed knees to have a significantly lower rate of arthritis [5]. Leys et al. support these findings furthermore focussing on isolated injuries [34].
Another reason for the wide variation of reported radiographic knee OA may be explained by the use of different radiological classification systems with no universal method of radiological classification, making it difficult to draw conclusions, other than that combined injuries had a higher rate of osteoarthritic changes than isolated ACL injury [37].
In this study, radiological changes were observed in more than 75 % of patients. On the other hand the majority of these changes was graded I and II OA according to the Jäger-Wirth classification. The rate of severe OA (grade III and IV OA) was 24.9 %, which is comparable to published long-term studies after ACL reconstruction.
On the other hand this investigation has limitations. First of all, our study does not give a randomised report of clinical and radiological results comparing the incidence of OA after ACL reconstruction with the uninjured contralateral knee. Additionally there was a high rate of loss to final follow-up (46.4 %). Reasons for the lack of return visits included the strict exclusion criteria like intermittent operative procedures due to partial or total meniscectomy and geographical limitations. In contrast we intended in particular to focus on long-term knee joint stability and prevalence of knee OA based on a homogeneous study sample with a standardised operative procedure and postoperative rehabilitation.
The striking variation for the prevalence and significance of degenerative changes after ACL reconstruction in the literature emphasises the need for studies on selected patient samples and was the priority objective of the study at hand. We could demonstrate that conservation of long-term stability is significantly correlated with development of OA, but even maintenance of long-term stability was not able to stop the onset of degenerative changes at all. OA after ACL reconstruction remains a condition of multifactorial genesis and further research is needed.
Conclusion
Arthroscopic ACL reconstruction using four-strand semitendinosus tendon autograft provided high patient satisfaction and satisfactory to excellent clinical results on long-term follow-up. The prevalence of symptomatic OA that developed in about 20 % is significantly correlated with conservation of long-term knee joint stability. Our findings support the evidence to perform ACL replacement. However, multiple factors may contribute to the development of knee OA.
References
Andersson D, Samuelsson K, Karlsson J (2009) Treatment of anterior cruciate ligament injuries with special reference to surgical technique and rehabilitation: an assessment of randomized controlled trials. Arthroscopy 25(6):653–685
Herrington L, Fowler E (2006) A systematic literature review to investigate if we identify those patients who can cope with anterior cruciate ligament deficiency. Knee 13(4):260–265
Gobbi A, Francisco R (2006) Factors affecting return to sports after anterior cruciate ligament reconstruction with patellar tendon and hamstring graft: a prospective clinical investigation. Knee Surg Sports Traumatol Arthrosc 14(10):1021–1028
Mihelic R, Jurdana H, Jotanovic Z, Madjarevic T, Tudor A (2011) Long-term results of anterior cruciate ligament reconstruction: a comparison with non-operative treatment with a follow-up of 17–20 years. Int Orthop 35(7):1093–1097
Louboutin H, Debarge R, Richou J, Selmi TA, Donell ST, Neyret P, Dubrana F (2009) Osteoarthritis in patients with anterior cruciate ligament rupture: a review of risk factors. Knee 16(4):239–244
Laxdal G, Kartus J, Ejerhed L, Sernert N, Magnusson L, Faxén E, Karlsson J (2005) Outcome and risk factors after anterior cruciate ligament reconstruction: a follow-up study of 948 patients. Arthroscopy 21(8):958–964
Poolman RW, Abouali JA, Conter HJ, Bhandari M (2007) Overlapping systematic reviews of anterior cruciate ligament reconstruction comparing hamstring autograft with bone-patellar tendon-bone autograft: why are they different? J Bone Joint Surg Am 89(7):1542–1552
van Eck CF, Schreiber VM, Mejia HA, Samuelsson K, van Dijk CN, Karlsson J, Fu FH (2010) “Anatomic” anterior cruciate ligament reconstruction: a systematic review of surgical techniques and reporting of surgical data. Arthroscopy 26(9 Suppl):S2–S12
Biau DJ, Katsahian S, Kartus J, Harilainen A, Feller JA, Sajovic M, Ejerhed L, Zaffagnini S, Röpke M, Nizard R (2009) Patellar tendon versus hamstring tendon autografts for reconstructing the anterior cruciate ligament: a meta-analysis based on individual patient data. Am J Sports Med 37(12):2470–2478
Fox JA, Nedeff DD, Bach BR Jr, Spindler KP (2002) Anterior cruciate ligament reconstruction with patellar autograft tendon. Clin Orthop Relat Res 402:53–63
Herrington L, Wrapson C, Matthews M, Matthews H (2005) Anterior cruciate ligament reconstruction, hamstring versus bone-patella tendon-bone grafts: a systematic literature review of outcome from surgery. Knee 12(1):41–50
Lidén M, Sernert N, Rostgård-Christensen L, Kartus C, Ejerhed L (2008) Osteoarthritic changes after anterior cruciate ligament reconstruction using bone-patellar tendon-bone or hamstring tendon autografts: a retrospective, 7-year radiographic and clinical follow-up study. Arthroscopy 24(8):899–908
Roe J, Pinczewski LA, Russell VJ, Salmon LJ, Kawamata T, Chew M (2005) A 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction: differences and similarities. Am J Sports Med 33(9):1337–1345
Fithian DC, Paxton LW, Goltz DH (2002) Fate of the anterior cruciate ligament-injured knee. Orthop Clin North Am 33(4):621–636
Keays SL, Newcombe PA, Bullock-Saxton JE, Bullock MI, Keays AC (2010) Factors involved in the development of osteoarthritis after anterior cruciate ligament surgery. Am J Sports Med 38(3):455–463
Levy AS, Meier SW (2003) Approach to cartilage injury in the anterior cruciate ligament-deficient knee. Orthop Clin North Am 34(1):149–167
Shelbourne KD, Benner RW (2009) Correlation of joint line tenderness and meniscus pathology in patients with subacute and chronic anterior cruciate ligament injuries. J Knee Surg 22(3):187–190
Lohmander LS, Englund PM, Dahl LL, Roos EM (2007) The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med 35(10):1756–1769
Stein T, Mehling AP, Welsch F, von Eisenhart-Rothe R, Jäger A (2010) Long-term outcome after arthroscopic meniscal repair versus arthroscopic partial meniscectomy for traumatic meniscal tears. Am J Sports Med 38(8):1542–1548
Wu WH, Hackett T, Richmond JC (2002) Effects of meniscal and articular surface status on knee stability, function, and symptoms after anterior cruciate ligament reconstruction: a long-term prospective study. Am J Sports Med 30(6):845–850
Hoffelner T, Resch H, Moroder P, Atzwanger J, Wiplinger M, Hitzl W, Tauber M (2012) No increased occurrence of osteoarthritis after anterior cruciate ligament reconstruction after isolated anterior cruciate ligament injury in athletes. Arthroscopy 28(4):517–525
Lebel B, Hulet C, Galaud B, Burdin G, Locker B, Vielpeau C (2008) Arthroscopic reconstruction of the anterior cruciate ligament using bone-patellar tendon-bone autograft: a minimum 10-year follow-up. Am J Sports Med 36(7):1275–1282
Möller E, Weidenhielm L, Werner S (2009) Outcome and knee-related quality of life after anterior cruciate ligament reconstruction: a long-term follow-up. Knee Surg Sports Traumatol Arthrosc 17(7):786–794
Øiestad BE, Engebretsen L, Storheim K, Risberg MA (2009) Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med 37(7):1434–1443
Øiestad BE, Holm I, Aune AK, Gunderson R, Myklebust G, Engebretsen L, Fosdahl MA, Risberg MA (2010) Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med 38(11):2201–2210
Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J (2007) A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med 35(4):564–574
Struewer J, Frangen TM, Ishaque B, Bliemel C, Efe T, Ruchholtz S, Ziring E (2012) Knee function and prevalence of osteoarthritis after isolated anterior cruciate ligament reconstruction using bone-patellar tendon-bone graft: long-term follow-up. Int Orthop 36(1):171–177
Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ, International Knee Documentation Committee (2006) The International Knee Documentation Committee Subjective Knee Evaluation Form: normative data. Am J Sports Med 34(1):128–135
Lysholm J, Gillquist J (1982) Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 10(3):150–154
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198(198):43–49
Tyler TF, McHugh MP, Gleim GW, Nicholas SJ (1999) Association of KT-1000 measurements with clinical tests of knee stability 1 year following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 29(9):540–545
Jäger M, Wirth C (1986) Praxis der Orthopaedie. Thieme, Stuttgart, p 980
Kessler MA, Behrend H, Henz S, Stutz G, Rukavina A, Kuster MS (2008) Function, osteoarthritis and activity after ACL-rupture: 11 years follow-up results of conservative versus reconstructive treatment. Knee Surg Sports Traumatol Arthrosc 16(5):442–448
Leys T, Salmon L, Waller A, Linklater J, Pinczewski L (2012) Clinical results and risk factors for reinjury 15 years after anterior cruciate ligament reconstruction: a prospective study of hamstring and patellar tendon grafts. Am J Sports Med 40(3):595–605
Holm I, Oiestad BE, Risberg MA, Aune AK (2010) No difference in knee function or prevalence of osteoarthritis after reconstruction of the anterior cruciate ligament with 4-strand hamstring autograft versus patellar tendon-bone autograft: a randomized study with 10-year follow-up. Am J Sports Med 38(3):448–454
Mascarenhas R, Tranovich MJ, Kropf EJ, Fu FH, Harner CD (2012) Bone-patellar tendon-bone autograft versus hamstring autograft anterior cruciate ligament reconstruction in the young athlete: a retrospective matched analysis with 2–10 year follow-up. Knee Surg Sports Traumatol Arthrosc 20(8):1520–1527
Schiphof D, Boers M, Bierma-Zeinstra SM (2008) Differences in descriptions of Kellgren and Lawrence grades of knee osteoarthritis. Ann Rheum Dis 67(7):1034–1036
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Struewer, J., Ziring, E., Frangen, T.M. et al. Clinical outcome and prevalence of osteoarthritis after isolated anterior cruciate ligament reconstruction using hamstring graft: follow-up after two and ten years. International Orthopaedics (SICOT) 37, 271–277 (2013). https://doi.org/10.1007/s00264-012-1653-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-012-1653-z