Abstract
Purpose
The aim of this investigation was to study patient-reported long-term clinical outcome, instrumental stablitity and prevalence of radiological osteoarthritis (OA) a minimum of ten years after isolated anterior cruciate ligament (ACL) reconstruction.
Methods
An average of 13.5 years after ACL reconstruction with bone–patellar tendon–bone (BTB) autograft, 73 patients were evaluated. Inclusion criteria consisted of an isolated ACL rupture and reconstruction with BPTB graft with no associated intra-articular lesions, in particular, cartilage alterations or meniscal lesions. Clinical assessment was performed using the International Knee Documentation Committee (IKDC) and Tegner and Lysholm scores. Instrumental anterior laxity testing was carried out with the KT–1000™ arthrometer. Degree of degenerative changes and prevalence of OA were determined using the Kellgren- Lawrence scale.
Results
Mean follow-up was 13.5 years. Mean age was 43.8 years. About 75% of patients were graded A or B according to the IKDC score. The Lysholm score was 90.2 ± 4.8. Radiological assessment reported degenerative changes of grade II OA in 54.2% of patients. Prevalence of grades III or IV OA was found in 20%. The incidence of OA was significantly correlated with stability and function at long-term follow-up.
Conclusion
Arthroscopic ACL reconstruction using BPTB autograft resulted in a high degree of patient satisfaction and good clinical results on long-term follow-up. A higher degree of OA developed in 20% of patients and was significantly correlated with increased anterior laxity at long-term follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) reconstruction surgery and techniques have changed over recent decades. The need for operative re-stabilisation is generally accepted. Restoration of long-term knee-joint stability and function remain the basic principles of any treatment strategy to avoid serious sequelae such as meniscus and cartilage damage and, in particular, progression of degenerative changes. [3, 6, 29]. The need for arthrometric graft positioning adapted to the individual factors of the knee has been proven in several studies and remains a cardinal assumption for achieving stability and free range of motion (ROM) of the operated knee joint [10, 19]. Furthermore postoperative individualised rehabilitation programmes represent basic requirements for overall therapeutic success. Modern arthroscopic management and reconstruction provide a high degree of patient satisfaction and good clinical results at short- and mid-term intervals [9]. However, progressive degenerative changes may develop over time. Important factors in osteoarthritis (OA) onset are concomitant meniscectomy or the time elapsed from injury to reconstruction [3, 10, 16]. On reviewing the literature, we found that many authors report successful results after ACL reconstruction [2, 5, 8, 22]. However, many studies focus on short- and mid-term results. Reports with follow-up periods over ten years or more remain rare [5, 20, 23]. Further limitations are the delay between primary injury and definitive operative treatment or major associated intra-articular injuries, particularly meniscal and cartilage lesions at reconstruction [3, 15, 29]. The primary objective of this study was to evaluate long-term functional and clinical outcomes and the incidence of potential OA based on a large study cohort after isolated ACL rupture and operative restoration.
Material and methods
Between January 1994 and December 1995 166 isolated ACL reconstructions were performed at our institution. Only patients with an isolated ACL rupture confirmed by arthroscopy in the course of treatment were included. All other patients with significant articular surface damage, meniscus lesions or osteoarthritic lesions of grade I or greater according to the Kellgren–Lawrence classification (17 patients) or concomitant medial collateral ligament repair (13 patients) at the time of reconstruction were excluded. Operative treatment was performed within two to three weeks from injury. Within the framework of the entire follow-up period of ten to 15 years, 11 patients (6.6%) suffered a graft rupture due to new trauma; four of them underwent an ACL revision procedure. Graft failure occurred on average 38 months after ACL reconstruction (range 12–120 months). Secondary partial or total medial meniscectomy was performed in 24 patients and lateral meniscectomy in 12. Five further revisions were for infected postoperative intra-articular haematomas. During the follow-up period, 14 patients (8.4%) suffered a contralateral ACL rupture and were excluded. At two year follow-up, the study group consitsed of 126 patients. On long-term follow-up, there were 78 patients, with 73 having a complete data record, which accounts for an overall follow-up rate of 44% [46 men, 27 women; median age 43 (range 24–63) years] 13 years after ACL reconstruction. Additional reasons for the high rate of loss on final follow-up were geographical limitations to attending the follow-up examination. In 53 cases the right knee and in 20 the left knee was affected.
Operative technique and postoperative rehabilitation
Operative technique was standardised in all patients: ACL reconstruction was performed with an autogenous bone–patellar tendon–bone (BTB) graft from the middle third of the patellar tendon. The central third (ten mm in width) was harvested through a single longitudinal incision. The graft was removed with a rectangular bone plug (20–25 mm in length). The tendon portion was freed from fat, and bone blocks were trimmed to fit a ten-mm-diameter bone tunnel. An arthroscopic-assisted reconstruction was used. The ruptured ACL was debrided and the anatomical tibial and femoral footprints were identified and left intact. The tibial tunnel was drilled using a drill guide under arthroscopic view through the posterior part of the middle of the tibial ACL footprint. To create the femoral tunnel a five-mm offset guide system was placed transtibially at the posterior margin of the intercondylar notch. The patellar tendon autograft was passed through the tibial tunnel using an Ethibond pull-through suture. Bone blocks were positioned in the tunnel, and the autograft was placed with its cortical edge oriented posteriorly within the femoral tunnel. The position of the femoral tunnel was determined with the knee in 120º of flexion using the five-mm offset instrument. Femoral-graft fixation was performed by press-fit positioning in the tunnels and by additional remote mini-plate fixation via a lateral incision. Exact intra-articular graft position of the tibial tunnel was performed with the knee in 90° of flexion, positioned in the footprint of its anatomical insertion. Afterwards, tibial-graft fixation was performed by press-fit fixation and additional joint-distant staple fixation. After femoral fixation, the affected knee was cycled several times to assess graft fixation and isometry. For the final tibial fixation, staples were used to fix the threads outside the tunnel. Postoperatively, patients were immobilised in a full-extension orthesis for the two days. Our concept of rehabilitation allows a free knee ROM. Isometric muscle exercises were then started with no limitations, and full weight bearing was allowed according to the patient’s pain level. During the entire rehabilitation period of six weeks, there was no additional external protection. High-demand pivoting sports activities were allowed after six to nine months.
Assessments
Clinical and functional follow-up assessment was based on the International Knee Documentation Committee (IKDC) score [1]. Further clinical evaluation criteria consisted of Tegener and Lysholm score [16, 26]. Patients who scored >92 points were considered to have excellent results; scores between 91 and 76 points were good; scores <76 points were fair/poor according to the Lysholm score [18]. Clinical evaluation using both IKDC and Lysholm scores was performed 24 months after surgery and at the ten to 15-year follow-up. Pretrauma status was documented. Anterior laxity was assessed using the KT 1000™ arthrometer (MEDmetric Cooperation, San Diego, CA, USA) according to IKDC graduation (degree of differential instrumental laxity in side comparison) [27]. The degree of degenerative changes was determined according to the Kellgren and Lawrence score. Conventional radiographs in three planes were used to evaluate the incidence of radiographic tibiofemoral and patellofemoral knee OA. Radiographic evaluation of the pretrauma status supplemented the overall radiographic assessment. Radiographs were evaluated according to the Kellgren and Lawrence classification: grade 0, no changes; grade 1, doubtful narrowing of the joint space and possible osteophytic lipping; grade 2, definite osteophytes and possible narrowing of the joint space; grade 3, moderate multiple osteophytes, definite joint-space narrowing, some sclerosis and possible deformity of the bone ends; and grade 4, large osteophytes, marked joint-space narrowing, definite sclerosis and definite deformity of the bone ends. Evidence of degenerative changes of grade II OA or greater according to the Kellgren–Lawrence classification were used to define OA whereas grade III and grade IV degenerative changes should account for symptomatic OA [11, 23].
Statistical analyses
Statistical analysis was performed by using the software SPSS 17.0. version for windows. Correlations were regarded as significant at p < 0.05 using the Pearson and chi-square tests and the Kruskal–Wallis test.
Results
IKDC evaluation
Clinical evaluation according to IKDC scores showed deterioration of the patient’s clinical constitution over the long term in comparison with results of the two year follow-up (Fig. 1).
Two years after the ACL reconstruction, functional assessment according to the IKDC score revealed 47 patients (37.3%) with an IKDC grade A, 60 (48.4%) with grade B, 18 patients (14.3%) with a grade C and one ( 0,8%) with grade D. On long-term follow-up, 17 (23.3%) patients with physiological clinical condition (IKDC A), 35 ( 47.9%) with a nearby physiological condition (IKDC B), 17 (23.3%) with an abnormal condition (IKDC C) and four (5.5%) with a severe abnormal clinical condition (IKDC D) were recorded. However, 75% of patients were graded A or B. Mean subjective IKDC score was 78.4 points on long-term follow-up. Reasons for abnormal clinical discoveries according to the IKDC score accounted for pain and progressive swelling of the knee joint during substantial load in the subjective IKDC questionnaire. Furthermore, an evident extension deficit, intermittent intra-articular effusion formation or a striking differential laxity on assessment with the Lachman test accounted for worse results within the objective IKDC evaluation.
Lysholm knee scoring scale
Clinical assessment according to the Lysholm score showed deterioration in average values over the long term (Table 1). On long-term follow-up—13 years after ACL reconstruction—13 (17.8%) patients scored <76 points; 41 (56.1%) patients scored >91 (excellent) and 29 (39.7%) scored between 77 and 91 (good).
Tegener activity scale
During the entire follow-up, there was a decrease in activity level according to the Tegener score (Table 1). On final follow-up, 12 patients (16.4%) had stopped or never returned to sports, whereas 75.6% were participating in sports and their follow-up remained excellent (55 of 73). However, pivoting and contact sports decreased from 77.8% to 45.2%. Furthermore, competitive involvement decreased from 65.3% to 18.5%. Forty-five patients (61.8%) stated that their level of performance had decreased. Only 19 (26.3%) patients indicated that these changes were related to the reconstruction. Socioprofessional factors were the main reason cited for the change in sports participation.
Assessment of anterior laxity (Lachman test)
Assessment of anterior translation with the KT-1000 arthrometer showed a slight deterioration on long-term follow-up in comparison with results at the 2-year follow-up. However, overall long-term knee-joint stability remained satisfactory to excellent after 13 years (Table 2).
Incidence of osteoarthritis
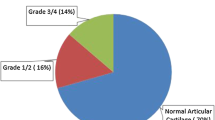
Radiographic assessment according to Kellgren and Lawrence revealed no signs of degenerative changes on pretrauma assessment. On two year and long-term follow-ups, a marked increase of degenerative changes was detected (Fig. 2).
Discussion
This retrospective clinical study evaluated clinical and radiological long-term outcomes after isolated ACL reconstruction with BTB graft. There was a high rate of loss on final follow-up (55.6%). Reasons for the lack of return visits represented the strict exclusion criteria, such as intermittent operative procedures due to partial or total menisectomy and geographical limitations. Various studies reviewing the literature have reported mid- and long-term results after ACL reconstruction [4, 5, 7–9, 13, 18, 21, 22]. Limitations of the majority of these studies were variable intervals between injury to ACL reconstruction, concomitant meniscectomy procedures or variable rehabilitation programmes. This study intended to identify factors associated with our long-term outcomes, focussing in particular on long-term knee-joint stability and prevalence of knee OA. It was also based on a homogenous sample, a standardised operative procedure and postoperative rehabilitation, and a short interval from injury to ACL reconstruction of only two to three weeks [3, 4, 13, 20]. Furthermore, it only focussed on isolated ACL injuries. All other patients—in contrast to other studies that included patients with concomitant intra-articular injuries such as significant articular surface damage, meniscal tears or concomitant medial collateral ligament repair at the time of reconstruction—were excluded. Results of clinical and functional evaluation, according to subjective and objective questionnaires of IKDC score on long-term follow-up, showed a decrease in comparison to mid-term results. Reasons for abnormal clinical findings according to IKDC score were pain and swelling on strenuous activity in the subjective IKDC questionnaire. Furthermore, obvious extension deficit, intra-articular effusion formation or a striking differential laxity on assessment with the Lachman test, accounted for worse results within the objective IKDC evaluation. The mean subjective IKDC score was 78.4 points on long-term follow-up. However, 75% of all patients could be evaluated as IKDC A or IKDC B grade; 85% subjectively judged the outcome of their ACL reconstruction at ten years as satisfactory. This judgment was based on a questionnaire provided in addition to IKDC evaluation. This questionnaire consisted of a four-step graduation from excellent to very poor for the subjective perceived overall therapeutic success. Therefore, 95% of the study population would have ACL reconstruction performed again. These results were comparable with those found in the literature. In a review of studies, Fox et al. and Lebel et al. reported that 91–98% of patients were satisfied with their ACL reconstruction at follow-up [7, 13]. Lebel et al. and Möller et al. reported high satisfaction rates and good to excellent clinical outcomes according to IKDC score (80–92 points on average) based on a population of similar age and overall constitution (13,189). In addition, Hertel et al. reported that at an average of 11 years after ACL reconstruction, 96% of re-evaluated patients would undergo ACL reconstruction surgery again. Furthermore, the reported mean IKDC subjective score was >90 points [8]. These results emphasise the fact that ten years after ACL reconstruction, most patients had nearly normal knee function. In a prospective study on 63 patients, Wu et al. reported similar results from patients with ACL rupture and reconstruction surgery [29]. They also reported a significant deterioration in clinical condition with associated meniscectomy or imperfect control of laxity and increasing incidence of OA. On the other hand, the authors could not show a significant correlation of IKDC score deterioration and OA increase based only on isolated ACL reconstruction. In contrast; Salmon et al. found that even though evidence of degeneration was present on radiographs, it was not yet reflected in patients’ self-reported results [23]. Mihelic et al. and Streich et al. published a report comparing operative versus conservative treatment. They found significant differences in mean IKDC score of the two groups and reported significant differences in the rate of OA in both groups, with a significantly higher rate of OA in conservative treatment [17, 25].
Lysholm and Tegener scores showed deterioration of patents’ clinical constitution in comparison with results two years after ACL reconstruction. The median Tegener score of 5 at final follow-up to that in studies with more than ten years of follow-up, which reported Tegener scores between 4 and 6 [13–15, 19]. Mean Lysholm score >90 points at long-term follow-up was similar to other studies with over ten years of follow-up, which reported scores between 82 and 94 points [19, 21, 22, 29]. Reasons for worse clinical scores are in relation to pain and progressive swelling on very strenuous activity. However, a satisfactory rate of 75.6% of patients still participated in sports at final follow-up. Socioprofessional factors were the main reason cited for the change in sports participation [19].
Assessment of long-term anterior laxity via the KT-1000 arthrometer showed deterioration in average values. On the other hand, overall results for the entire follow-up remained excellent: 79% of all patients showed a differential laxity less than three mm on long-term evaluation. Overall performance concerning the anterior translation measured on KT 1000 arthrometer was comparable with those found by Fox et al. and other study groups at mid- to long-term follow-up, with 70–90% of patients having a KT–1000 arthrometer result less than three mm [7]. Milhelic et al. published a report comparing operative versus conservative treatment and reported significant differences in OA rate between groups, with a significantly higher rate of OA with increased laxity. Furthermore, they reported the highest OA rate with concomitant menisectomy [18]. In this report, radiographic evaluation of OA revealed no signs of degenerative changes in 86.7% of patients on pretrauma assessment. On mid- and long-term follow-up, a marked increase in degenerative changes was detected upon radiographic evaluation.
In our study, radiological assessment revealed mild to moderate degenerative changes in 73.8% of patients regarding grade I or II OA according to Kellgren and Lawrence. Symptomatic OA grades III and IV was found in 17% and 6% on long-term follow-up, respectively. The study demonstrated a significant correlation for the incidence of OA and performance on instrumental anterior translation assessment on long-term follow-up. The study also showed a significant increase in degenerative changes and OA progression in patients with increased anterior laxity (p < 0.05) (Fig. 3). Our investigation showed that even maintenance of excellent scores concerning long-term anterior translation were not able to prevent the onset of degenerative changes and OA progression. A great advantage of this study is its strict inclusion criteria, because only patients with isolated ACL injuries were evaluated. Various studies have reported on long-term results after ACL reconstruction. However, few of these studies focusing in particular on the incidence of OA [5, 12, 13, 21, 22]. Limitations of those studies were an unselected patient group and, in particular, a high prevalence of accompanying intra-articular injuries such as meniscal lesions and significant cartilage damage [3–5, 12, 13, 21, 22]. For example, Lohmander et al. and von Porat et al., evaluating soccer players, reported a high prevalence of knee OA (69% and 59%, respectively) in individuals with ACL injuries combined with meniscal injuries [14, 15, 28]. Furthermore, Lebel et al. retrospectively examined 98 individuals after ACL injury reconstruction with BTB autograft [13] and reported a 13.6% prevalence of knee OA in individuals with isolated injuries and 21.5% in individuals with combined injuries. Additionally, a detailed review of the study shows a rate of concomitant intra-articular lesions and meniscectomies and graft ruptures over the entire assessment period. These patients were not excluded. Other prospective studies found a lower prevalences of radiographic knee OA (1–11%) in individuals who have undergone ACL reconstruction surgery [22]. Other investigations could demonstrate that partial meniscal resection induces less radiographic OA over time than does total meniscectomy [4, 16]. Wu et al. reported a strong correlation between the magnitude of the meniscectomy and the incidence of OA [29]. Øiestad et al. evaluated 181 individuals at ten to 15-year follow-up [21] and reported no significant differences in knee function and clinical constitution over time between isolated- and combined-injury groups. Individuals with combined injury had a significantly higher prevalence of radiographic knee OA compared with those with isolated injury (80% and 62%, respectively), but no significant differences were shown between groups for symptomatic radiographic knee OA (42% and 36%, respectively) [20]. In another review of different study populations and reconstruction techniques, the authors concluded that variation in the reported prevalence of degenerative changes may be explained by different study designs, different ACL populations or different surgical procedures. Another reason for the wide variation of reported radiographic knee OA may be explained by the use of different radiological classification systems [24]. For instance, Kellgren and Lawrence grade 2 involves osteophytes and possible joint-space narrowing, whereas the IKDC classification and the Ahlback classification involve mainly joint-space narrowing for defining knee OA. In the study reported here, radiological changes were observed in >80% of patients. On the other hand, the majority of these changes were graded I and II OA according to the Kellgren-Lawrence classification. The rate of severe OA (grades III and IV) was 22.1%, which is comparable with other published long-term studies after ACL reconstruction [8, 12, 13, 21].
The striking variation in the literature for the prevalence and significance of degenerative changes after ACL reconstruction emphasises the need for studies on selected patient samples, which was the primary objective of our study. We showed that even maintenance of excellent scores concerning long-term anterior translation were not able to prevent the onset of degenerative changes and progression of OA. Therefore, OA after ACL reconstruction remains of multifactorial genesis, and further research is needed.
Conclusion
The primary goal of ACL reconstruction is to restore and maintain knee-joint stability and function. ACL reconstruction with the BTB autograft resulted in a high degree of patient satisfaction levels and good clinical results after 13 years. Prevalence of symptomatic OA developed in about 20% and significantly correlated with increased anterior laxity. On the other hand, despite excellent long-term scores and good knee-joint stability, degenerative changes progressed over time, and obviously OA development is not preventable.
References
Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ (2006) International Knee Documentation Committee. The International Knee Documentation Committee Subjective Knee Evaluation Form: normative data. Am J Sports Med 34:128–135
Biau DJ, Katsahian S, Kartus J et al (2009) Patellar tendon versus hamstring tendon autografts for reconstructing the anterior cruciate ligament: a meta-analysis based on individual patient data. Am J Sports Med 37(12):2470–2478
Church S, Keating JF (2005) Reconstruction of the anterior cruciate ligament: timing of surgery and the incidence of meniscal tears and degenerative change. J Bone Joint Surg Br 87:1639–1642
Cohen M, Amaro JT, Ejnisman B et al (2007) Anterior cruciate ligament reconstruction after 10 to 15 years: association between meniscectomy and osteoarthrosis. Arthroscopy 23(6):629–634
Drogset JO, Grontvedt T, Robak OR et al (2006) A sixteen-year follow-up of three operative techniques for the treatment of acute ruptures of the anterior cruciate ligament. J Bone Joint Surg Am 88:944–952
Fithian DC, Paxton LW, Goltz DH (2002) Fate of the anterior cruciate ligament- injured knee. Orthop Clin North Am 33:621–636
Fox JA, Nedeff DD, Bach BR Jr, Spindler KP (2002) Anterior cruciate ligament reconstruction with patellar autograft tendon. Clin Orthop Relat Res 402:53–63
Hertel P, Behrend H, Cierpinski TS, Musahl V, Widjaja G (2005) ACL reconstruction using bone-patellar tendon-bone press-fit fixation: 10-year clinical results. Knee Surg Sports Traumatol Arthrosc 13:248–255
Jarvela T, Kannus P, Jarvinen M (2001) Anterior cruciate ligament reconstruction in patients with or without accompanying injuries: a re-examination of subjects 5 to 9 years after reconstruction. Arthroscopy 17:818–825
Keays SL, Newcombe PA, Bullock-Saxton JE, Bullock MI, Keays AC (2010) Factors involved in the development of osteoarthritis following anterior cruciate ligament surgery. Am J Sports Med 38(3):455–463
Kellgren JH, Lawrence JS, Bier F (1963) Genetic factors in generalized Osteoarthritis. Ann Rheum Dis 22:237–255
Laxdal G, Kartus J, Ejerhed L et al (2005) Outcome and risk factors after anterior cruciate ligament reconstruction: a follow-up study of 948 patients. Arthroscopy 21:958–964
Lebel B, Hulet C, Galaud B, Burdin G, Locker B, Vielpeau C (2008) Arthroscopic reconstruction of the anterior cruciate ligament using bonepatellar tendon-bone autograft: a minimum 10-year follow-up. Am J Sports Med 36(7):1275–1282
Lohmander LS, Englund PM, Dahl LL, Roos EM (2007) The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med 35(10):1756–1769
Lohmander LS, Ostenberg A, Englund M, Roos H (2004) High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum 50(10):3145–3152
Louboutin H, Debarge R, Richou J et al (2008) Osteoarthritis in patients with anterior cruciate ligament rupture: a review of risk factors. Knee 16(4):239–244
Lysholm J, Gillquist J (1982) Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 10:150–154
Mihelic R, Jurdana H, Jotanovic Z, Madjarevic T, Tudor A (2011) Long-term results of anterior cruciate reconstruction: a comparison with non-operative treatment with a follow-up of 17–20 years. Int Orthop 35(7):1093–1097
Möller E, Weidenhielm L, Werner S (2009) Outcome and knee-related quality of life after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 17:786–794
Øiestad BE, Engebretsen L, Storheim K, Risberg MA (2009) Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med 37(7):1434–1443
Øiestad BE, Holm I, Gunderson R, Myklebust G, Risberg A (2010) Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med 38(11):2201–2210
Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J (2007) A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med 35(4):564–574
Salmon LJ, Russell VJ, Refshauge K et al (2006) Long-term outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft: minimum 13-year review. Am J Sports Med 34:721–732
Schiphof D, Boers M, Bierma-Zeinstra SM (2008) Differences in descriptions of Kellgren and Lawrence grades of knee osteoarthritis. Ann Rheum Dis 67(7):1034–1036
Streich NA, Zimmermann D, Bode G et al (2011) Reconstructive versus non-reconstructive treatment of anterior cruciate ligament insufficiency. A retrospective matched-pair long-term follow-up. Int Orthop 35(4):607–613
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Tyler TF, McHugh MP, Glim GW et al (1999) Association of KT-1000 measurements with clinical tests of knee stability 1 year following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 29(9):540–545
Von Porat A, Roos EM, Roos H (2004) High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis 63:269–273
Wu WH, Hackett T, Richmond JC (2002) Effects of meniscal and articular surface status on knee stability, function, and symptoms after anterior cruciate ligament reconstruction: a long-term prospective study. Am J Sports Med 30:845–850
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Struewer, J., Frangen, T.M., Ishaque, B. et al. Knee function and prevalence of osteoarthritis after isolated anterior cruciate ligament reconstruction using bone-patellar tendon-bone graft: long-term follow-up. International Orthopaedics (SICOT) 36, 171–177 (2012). https://doi.org/10.1007/s00264-011-1345-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-011-1345-0