Abstract
ACL-reconstruction aims to restore joint stability and prevent osteoarthritis; however, malfunction and osteoarthritis are often the sequelae. Our study asks whether ACL-reconstruction or conservative treatment lead to better long-term results. In this retrospective cohort study, 136 patients with isolated ACL-rupture who had been treated by bone-ligament-bone transplant or conservatively were identified. Twenty-seven of these were excluded because of a revision operation in the 11.1 years follow-up period, leaving 109 patients (60 reconstructions and 49 conservatively treated) for evaluation based on clinical, radiological and internationally accepted knee-scores (Tegner, IKDC, Kellgren and Lawrence). An individual cohort study is classified as EBM level 2b according to the Oxford Centre of EBM. We observed significantly better knee-stability (P = 0.008) but more osteoarthritis (Grade II or higher) after ACL-reconstruction (42% vs. 25%). Physical activity levels were similar in both groups during the follow-up period (P = 0.16). Eleven years after ACL-rupture the physical activity levels are similar for both groups. After ACL-reconstruction, stability is higher as is osteoarthritis, whereby the result is not necessarily perceived as better subjectively. Specifically, this retrospective study yielded a 24% incidence of oseoarthrits 11 years after conservative management of ACL-rupture in patients not needing secondary surgery. The risk of secondary meniscal tears is reduced after ACL reconstruction, which reduces the negative effects of OA after surgery. The ultimate objective would be to achieve a good subjective outcome by conservative treatment followed by a rehabilitation program designed to keep secondary meniscus tears at a low level.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rupture of the anterior cruciate ligament (ACL) occurs frequently and leads to changes in the kinematics of the knee joint. Therefore, the main aims of ACL-reconstruction are to reconstruct the kinematics, prevent joint instability and thus preclude the development of osteoarthritis. Nevertheless, malfunction and osteoarthritis are frequently seen after ACL-reconstruction [17,25].
The indication for ACL-reconstruction cannot be regarded as absolute. Some authors are of the opinion that if physical activity is kept to a minimum and pivotal sports activities are avoided, then the situation may remain stable for many years [8]. Kostogiannis et al. observed 100 patients with an acute total ACL injury without reconstruction for 15 years and concluded that early modification of activity and neuromuscular rehabilitation resulted in good knee function and an acceptable activity level in the majority of patients [22]. On the other hand, Strehl and Eggli, in their investigation of conservative treatment for ACL rupture found that almost two-thirds of those patients selected for primary conservative treatment required surgical reconstruction in the long-term [37]. Furthermore, some authors conclude that patients with a high level of activity may suffer secondary damage. In this context, meniscectomies as a result of meniscal lesions have been described in 20–80% of cases after 5–10 years [4,16,34]. Cohen et al. report a statistically significant relationship between medial or lateral arthrosis of the knee and meniscal injury 10–15 years after arthroscopy-assisted ACL-reconstruction [9]. The loss of the meniscus as a secondary stabilizer promotes instability, which is associated with a high risk of osteoarthritis [11,2].
After ACL-rupture there seems to be a far greater risk of degenerative joint disease than in the unaffected population and this has been quantified by various authors, namely, McDaniel 40% [26], Indelicato 54% [18], Neyret 80% [31]. In addition to restoration of knee stability and functionality, ACL-reconstruction is also regarded as an important measure to prevent the risk of osteoarthritis. But, there are only a few studies that permit any valid statement as to whether surgical management is more advantageous than conservative management [24], and whether it can be justified on the basis of osteoarthritis prevention [3] and there are few reports on isolated ACL-ruptures whose status has been assessed after 11 years or more. Meunier et al. completed a follow-up of 15 years and found that, regardless of the treatment approach, the status of the menisci was the most important predictor of developing osteoarthritis. Their findings support the hypothesis that early stabilization of the knee after ACL injury is beneficial to the long-term outcome [28]. The aim of our study was to record and compare functionality, activity, and arthrotic manifestations after isolated ACL-ruptures for conservative treatment and ACL-reconstruction in the long-term.
Patients and methods
Patient sample
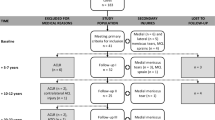
From January 1989 to September 1997 posttraumatic ACL-rupture was confirmed by arthroscopy in 194 patients. The choice of subsequent treatment was based on consensus between the treating surgeon and the patient independent of the sports activity level. We excluded 58 patients for the following reasons: concomitant ligamentous injuries (n = 3), meniscal and/or cartilaginous lesions (n = 38), fractures (n = 1), BMI > 30 and age (n = 1), non-attendance due to lack of symptoms (n = 5), no reply and non-attendance (n = 5), unknown address (n = 5). A further 27 patients with isolated ACL rupture (OP = 8 vs. NOP = 19) were excluded from the study because they had undergone a revision operation at some time during the 11-year follow-up period, leaving a total of 109 patients (60 reconstructions, 49 conservative treatment) as the definitive sample of patients available to follow-up (total 85 exclusions). The need for surgery in the follow-up period for patients with isolated ACL rupture is therefore eight out of 68 (12%) compared to 19 of 68 treated non-operatively (28%) (P < 0.035). These revision procedures were mainly due to meniscal lesions, namely, OP, six instabilities with ACL rerupture and/or seven meniscus lesions (total of eight patients), and NOP, 18 meniscus lesions with 12 concomitant instabilities (total of 19 patients). Overall, the requirement for meniscal surgery was seven out of 68 in the operatively treated group (10%) and 18 out of 68 in the non-operatively treated group (26%) (P < 0.03) and/or knee instabilities, six out of 68 in the operatively treated group (9%) and 12 out of 68 in the non-operatively treated group (18%). None of the patients included in this retrospective study had received revision surgery during the follow-up period.
The reasons for the injuries are summarized below:
NOP: Distortion sport
OP: Distortion sport
Overall total: 100% (109 patients)
The data indicate that more cases of direct contusion are recorded as the type of accident in the OP group. Whether this has any effect on the later development of osteoarthritis is speculative, partly because the effects of the force and distortion mechanisms cannot be quantified but are based on descriptions given by the patients, and partly because other intra-articular lesions or fractures were excluded.
The results recorded at the time of the final follow-up were based on the clinical and radiological findings and were quantified by means of the scores reported in the manuscript. MRI investigation was not performed at the time of the final follow-up.
Follow-up
In 2004 and 2005 the authors MAK and HB performed final follow-up evaluations, including consensus readings of the radiographs. The surgeons who had operated on these patients were not involved in the present study. The mean follow-up time was 11.1 years (min 7.5, max 16.3 years) and the mean age at the time of trauma was 30.7 years (12.5–54.0 years), whereby the gender distribution was 68 males versus 41 females. The evaluation was based on internationally recognized knee evaluation scores for function, namely, IKDC [19] incl. KT-1000 bilaterally, Tegner for sports ability [38], and Kellgren and Lawrence for radiological alterations (radiological views under full loading as described by Rosenberg, in 0° flexion a.p. and lateral, the patella axially in 45° flexion) [21]. Radiographs were not taken of the healthy knee to avoid unnecessary radiation exposure.
Matching
Matching criteria, such as gender, identical age ±5 years, BMI ±3, Tegner-Score ±1, follow-up period ±6 months, were applied to ensure that habitual knee loading in both groups was comparable.
Operative management
ACL-reconstruction had been performed by various senior registrars specialized in knee ligament surgery. The reconstruction was performed with bone-patellar tendon-bone graft with extra-articular screw fixation of tibia and femur in arthroscope-assisted and mini-arthrotomy technique.
Rehabilitation
Both groups followed the same rehabilitation program based on a standard physiotherapy protocol. This involved wearing an ACL brace for 6 weeks, training of hamstrings and quadriceps muscle, proprioception training, no flexion under load greater than 60° for 6 weeks, return to sports activities after 3 months, and return to contact/pivoting sports after 9 months. The patients attended their physiotherapist of choice. The criteria for return to sports were no pain, no swelling during or after loading, and no sense of instability. All patients were advised to participate in sports activities regardless of the treatment method.
Statistical analysis
Data are presented as means and standard deviations, percentages and rates, or odds-ratios and 95% confidence intervals. Categorical variables were univariately compared by Fisher’s exact test or Chi-square test for trend. Binary outcomes were multivariately analyzed by logistic regression. Continuous outcomes (including scores) were univariately compared by Student’s t-tests or Wilcoxon’s tests as appropriate according to normality assumptions, and multivariately by linear regression. Variables were included in the final models if they were significant predictors of the outcome variables in a stepwise elimination procedure or if they were considered clinically relevant (e.g. BMI, gender, and age) irrespective of their statistical significance.
Results
Function by IKDC_score
At follow-up the patients with ACL-reconstruction achieved a significantly better IKDC score (P = 0.008). The scores were distributed as follows: IKDC normal (A) for OP n = 32, this corresponds to 53% of all patients after ACL-reconstruction. In contrast, only seven NOP patients, corresponding to 14% of all NOP, were assessed as IKDC normal (A). IKDC nearly normal (B) for OP 11(18%) versus NOP 20 (41%), IKDC abnormal(C) for OP = 12 (20%) versus NOP = 15 (31%), IKDC severely abnormal (D) for OP = 5(8%) versus NOP = 7 (14%). The KT1000 difference between the healthy and the affected knee at the time of follow-up produced a mean for OP of 3.9 mm (min = 0; max = 12) versus a mean of 5.7 mm (min = 0, max = 16) for NOP. A statistically significant difference (P < 0.05) could be demonstrated (Fig. 1).
Radiological evaluation on the Kellgren and Lawrence score
About 52% (57 of 109) of all the cases evaluated had no osteoarthritis (Grade 0) at the time of follow-up, whereas 48% (52 of 109) were already doubtful (Grade I) or arthrotic changes were definitely present (Grades II–III). With reference to the specific therapeutic procedure, no osteoarthritis (Grade 0) was observed after ACL-reconstruction in 45% (27 of 60) or in 61% (30 of 49) after conservative treatment. A doubtful osteoarthritis with debatable or slight involvement of the intercondylar eminence or the patella (Grade I) was identified after OP in 10% (6 of 60) and after NOP in 14% (7 of 49). Distinct involvement of the tibia and joint space narrowing (Grade II) was recorded after OP in 42% (25 of 60) and after NOP in 20% (10 of 49). Moderate osteoarthritis (Grade III) was identified after OP in 3% (2 of 60) and after NOP in 4% (2 of 49). If the risk of osteoarthritis after ACL-rupture is calculated (cut-off between Grades I and II), it can be shown that the risk is 24% after a conservative procedure in contrast to 45% after ACL-reconstruction (Fig. 2). This difference can be shown to be statistically significant (P = 0.03).
The risk of radiologically evident osteoarthritic alterations in relation to the specific treatment procedure. The risk of mild or moderate arthrosis (Grades II and III) after ACL-reconstruction is 45%, whereas it is only 24% after conservative treatment. A 24% risk of arthrosis after 11.4 years can be regarded as the natural course
In a multivariate analysis other factors (age, BMI) were also identified as being associated with a significantly higher osteoarthritis rate (Table 1).
Sports ability on the Tegner score
Sports ability, expressed as a Tegner score, came to 5.4 (2.0–10) points for OP and 5.9 (2.0–10) for NOP before the trauma (P = n.s.). At the time of follow-up, the OP group scored 5.3 (2.0–10) points compared to the NOP group with 4.9 (2.0–10) points (P = n.s.). The loss of sports ability was expressed as the difference (delta-Tegner), i.e. of 0.48 (−1–4) points for OP and 0.55 (0–7) points for NOP (P = n.s.). Therefore, no difference between the two groups could be proven with regard to loss of sports ability (Fig. 3).
Discussion
The concept of reconstruction to prevent osteoarthritis, and maintain function and activity cannot be accepted unquestioningly. ACL-reconstruction is often indicated to treat concomitant injuries to the meniscus or lateral collateral ligament; however, in the case of an isolated ACL-lesion, many different considerations will play a role in deciding whether to proceed with a surgical or a conservative treatment.
In our study, comparison of the groups based on the IKDC criteria showed a clear advantage in favor of ACL-reconstruction (Fig. 1). Nevertheless, it must be remembered that the overall IKDC score is determined by the worst individual parameter. Therefore, it is not a surprise to find that patients without ACL have greater a.p. translation and achieve lower IKDC scores. Even though surgical procedures might be preferred on the basis of these results, a large proportion of the patients with distinct, objective a.p. instability (IKDC B,C,D) are subjectively almost symptom-free and have high level of activity (Fig. 3). After ACL-rupture some patients achieve a subjectively satisfactory result after special training, whereas some patients have residual persistent subjective instability [27]. In this context, reference should be made to R. Jakob’s theory of the ACL dominant knee, “apparently there are today unexplained and poorly understood factors that place the dominant onus for stability on the ACL in one knee (ACL dominant knee) while the other joint functions normally without the ACL”[20].
Progressive destruction of the joint structures is described after ACL-rupture and reconstruction is recommended [26]. This is partly justified by increased a.p. translation and rotational instability [7], leading to cartilaginous and meniscal damages. Vasara et al. were able to show a correlation between the time of ACL-rupture and the number of cartilaginous lesions in the context of symptomatic knee instability [39], whereby Daniel et al. in their investigations found this effect to be more distinct if the menisci were also injured [11]. Therefore, the prevention of osteoarthritis is often brought forward as a strong argument in favor of ACL-reconstruction. The theory that ACL-plasty is valuable as a means of preventing premature degeneration of the joint cannot be confirmed by the data obtained in this present study (Fig. 2). Not only was a significantly lower rate of osteoarthritis recorded in our patient group after conservative treatment (42% vs. 25%), but also comparison with the data obtained from other studies failed to reveal the clear superiority of ACL-reconstruction [17].
Fink et al. did not find any differences in osteoarthritis development in their comparison of the conservative and reconstructive treatment of patients over a period of 7 years, although it should be stated that their patient sample included 50% meniscal lesions [13]. Fithian [15] implemented a prospective investigation of 209 patients with 6.6 years follow-up and came to the conclusion that reconstruction cannot prevent the occurrence of degenerative alterations, whereby the study included a mixture of patients with and without meniscal lesions and evaluation was only by MRI and not arthroscopy. It should be emphasized that internal damage to the knee with ACL-rupture frequently consists of a combination injury with meniscal lesion (Feagin [12] at 19%, Mc Daniel [27] at 70%), whereas an isolated ACL-lesion rarely occurs [14].
In a study by Nebelung [30] involving 19 patients with a follow-up of 35 years following conservative treatment of ACL rupture, it was established that meniscectomies were necessary after 10 years in 79% and after 20 years in 95%. Ten patients required total knee replacement. In comparison with our study, the initial diagnosis of ACL rupture “was based on acute hemarthrosis, the history of the injury and the anterior drawer test”. Arthroscopy was not performed to confirm the diagnosis. Associated concomitant injuries such as meniscal or chondral lesions cannot be excluded so that these data cannot be compared with ours.
In our study we were able to investigate a patient sample with isolated ACL-lesions but without meniscal lesions. Results for the high number of patients and long follow-up time that we have been able to achieve in our study have not been published previously. A follow-up of 11.4 years is regarded as long-term follow-up; however, when one considers that the majority of injuries occur in the second and fourth decades of life, even more long-term investigations would be desirable.
Nevertheless, the issue of increased risk of osteoarthritis after surgery needs further discussion. This paper shows that operatively treated isolated ACL rupture is complicated by a higher rate of osteoarthritis in the follow-up period than non-operatively treated rupture not needing surgery in the follow-up period. Non-operatively treated rupture leads to a significantly higher rate of meniscal lesions requiring later surgery than operatively treated ACL rupture. However, it was not possible to determine the degree of oseoarthritis in these knees with secondary meniscal tears.
Abnormal mechanical relationships may arise due to suboptimal technique, whereby placement of the graft insertion in vertical or horizontal alignment is still under discussion [36], or they may be caused by the level of tension in hamstring tendon grafts [10]. According to Stergiou et al. [35] activities that are more demanding than walking can cause excessive anterior and rotational loading of the knee. This leads to abnormal loading of cartilage areas that are not usually loaded in the healthy knee. Alteration of the biomechanical situation caused by graft harvesting is another issue that has not yet been fully clarified; however, Pinczewski et al. [32,40] concluded that decreased harvest-site symptoms and radiographic osteoarthritis were observed after hamstring tendon compared with patellar tendon autograft. On the other hand, important antagonists to inner rotational stability are sacrificed during hamstring tendon harvesting, which may lead to an increased incidence of osteoarthritis in the long-term. In our study, we harvested the patellar tendon, which may have affected the elastic properties of the extensors and, consequently, altered the compression forces acting on the knee joint. This situation may also tend to induce osteoarthritis, but conclusive evidence is not available at this time and more research will have to be done in this area.
It has to be noted with regard to this investigation that it was not a prospective, blinded, randomized study. This means that bias in terms of making one particular treatment approach more attractive to the patient, either due to the influence of the treating physician or individual patient factors, cannot be excluded.
It is unclear what secondary damage may develop after conservative treatment. Renewed knee trauma may occur even after many years, sometimes perceived by the patient as a trivial sprain, and may take the form of meniscopathy or massive instability. This may require a secondary surgical procedure with ACL-plasty. On the other hand, persistent instability, meniscopathy or re-rupture of the transplant has been described in up to 10% of cases even after primary ligament reconstruction [1]. In our patient sample a slightly increased reconstruction rate after conservative treatment is apparent and might be considered an argument in favor of primary ACL-reconstruction. On the other hand, if a patient is expected to do well with primary conservative treatment, then this method should be preferred because of the apparent lower risk of osteoarthritis compared with surgical management.
The success of surgical treatment is partly a question of technique whereas, in the case of conservatively treated injuries, the surgeon has little influence on the healing process [23,6,29]. The data presented here, especially the osteoarthritis rate after conservative treatment, can therefore be understood as reference values. From a preventive point of view, the aim must be to lower these values by improvement of surgical procedures. Surgical methods have indeed been modified in various ways over the last 12 years—position of the reaming channel, anchoring techniques, choice of transplant, rotational stability—and the process is ongoing [5,33]. It is therefore to be hoped that an investigation of current procedures in the near future will demonstrate the superiority of a surgical approach and that the osteoarthritis rate can be diminished further.
References
Ahn JH, Yoo JC, Yang HS, Kim JH, Wang JH (2007) Second-look arthroscopic findings of 208 patients after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 15(3):242–248
Ait Si Selmi T, Fithian D, Neyret P (2006) The evolution of osteoarthritis in 103 patients with ACL reconstruction at 17 years follow-up. Knee 13:353–358
Andersson C, Odensten M, Gillquist J (1991) Knee function after surgical or nonsurgical treatment of acute rupture of the anterior cruciate ligament: a randomized study with a long-term follow-up period. Clin Orthop Relat Res:255–263
Andersson C, Odensten M, Good L, Gillquist J (1989) Surgical or non-surgical treatment of acute rupture of the anterior cruciate ligament. A randomized study with long-term follow-up. J Bone Joint Surg Am 71:965–974
Behrend H, Stutz G, Kessler MA, Rukavina A, Giesinger K, Kuster MS (2006) Tunnel placement in anterior cruciate ligament (ACL) reconstruction: quality control in a teaching hospital. Knee Surg Sports Traumatol Arthrosc 14(11):1159–1165
Beynnon BD, Ryder SH, Konradsen L, Johnson RJ, Johnson K, Renstrom PA (1999) The effect of anterior cruciate ligament trauma and bracing on knee proprioception. Am J Sports Med 27:150–155
Brophy RH, Selby RM, Altchek DW (2006) Anterior cruciate ligament revision: double-bundle augmentation of primary vertical graft. Arthroscopy 22:683 e681–e685
Casteleyn PP, Handelberg F (1996) Non-operative management of anterior cruciate ligament injuries in the general population. J Bone Joint Surg Br 78:446–451
Cohen M, Amaro JT, Ejnisman B, Carvalho RT, Nakano KK, Peccin MS, Teixeira R, Laurino CF, Abdalla RJ (2007) Anterior cruciate ligament reconstruction after 10 to 15 years: association between meniscectomy and osteoarthrosis. Arthroscopy 23:629–634
Cunningham R, West JR, Greis PE, Burks RT (2002) A survey of the tension applied to a doubled hamstring tendon graft for reconstruction of the anterior cruciate ligament. Arthroscopy 18:983–988
Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR (1994) Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med 22:632–644
Feagin JA Jr, Curl WW (1976) Isolated tear of the anterior cruciate ligament: 5-year follow-up study. Am J Sports Med 4:95–100
Fink C, Hoser C, Benedetto KP, Hackl W, Gabl M (1996) Long-term outcome of conservative or surgical therapy of anterior cruciate ligament rupture. Unfallchirurg 99:964–969
Finsterbush A, Frankl U, Matan Y, Mann G (1990) Secondary damage to the knee after isolated injury of the anterior cruciate ligament. Am J Sports Med 18:475–479
Fithian DC, Paxton EW, Stone ML, Luetzow WF, Csintalan RP, Phelan D, Daniel DM (2005) Prospective trial of a treatment algorithm for the management of the anterior cruciate ligament-injured knee. Am J Sports Med 33:335–346
Hawkins RJ, Misamore GW, Merritt TR (1986) Followup of the acute nonoperated isolated anterior cruciate ligament tear. Am J Sports Med 14:205–210
Hertel P, Behrend H, Cierpinski T, Musahl V, Widjaja G (2005) ACL reconstruction using bone-patellar tendon-bone press-fit fixation: 10-year clinical results. Knee Surg Sports Traumatol Arthrosc 13:248–255
Indelicato PA, Bittar ES (1985) A perspective of lesions associated with ACL insufficiency of the knee. A review of 100 cases. Clin Orthop Relat Res (198):77–80
Irrgang JJ, Ho H, Harner CD, Fu FH (1998) Use of the international knee documentation committee guidelines to assess outcome following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 6:107–114
Jakob RP (1990) Indikation zur Kreuzbandplastik: rekapitulation. Springer, Berlin, Heidelberg, New York
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Kostogiannis I, Ageberg E, Neuman P, Dahlberg L, Friden T, Roos H (2007) Activity level and subjective knee function 15 years after anterior cruciate ligament injury: a prospective, longitudinal study of nonreconstructed patients. Am J Sports Med 35:1135–1143
Kuster MS, Grob K, Kuster M, Wood GA, Gachter A (1999) The benefits of wearing a compression sleeve after ACL reconstruction. Med Sci Sports Exerc 31:368–371
Linko E, Harilainen A, Malmivaara A, Seitsalo S (2005) Surgical versus conservative interventions for anterior cruciate ligament ruptures in adults. Cochrane Database Syst Rev:CD001356
Maletius W, Messner K (1999) Eighteen- to twenty-four-year follow-up after complete rupture of the anterior cruciate ligament. Am J Sports Med 27:711–717
McDaniel WJ Jr, Dameron TB Jr (1983) The untreated anterior cruciate ligament rupture. Clin Orthop Relat Res (172):158–163
McDaniel WJ Jr, Dameron TB Jr (1980) Untreated ruptures of the anterior cruciate ligament. A follow-up study. J Bone Joint Surg Am 62:696–705
Meunier A, Odensten M, Good L (2007) Long-term results after primary repair or non-surgical treatment of anterior cruciate ligament rupture: a randomized study with a 15-year follow-up. Scand J Med Sci Sports 17:230–237
Muellner T, Alacamlioglu Y, Nikolic A, Schabus R (1998) No benefit of bracing on the early outcome after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 6:88–92
Nebelung W, Wuschech H (2005) Thirty-five years of follow-up of anterior cruciate ligament-deficient knees in high-level athletes. Arthroscopy 21:696–702
Neyret P, Donell ST, Dejour H (1993) Results of partial meniscectomy related to the state of the anterior cruciate ligament. Review at 20 to 35 years. J Bone Joint Surg Br 75:36–40
Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J (2007) A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med 35:564–574
Scopp JM, Jasper LE, Belkoff SM, Moorman CT III (2004) The effect of oblique femoral tunnel placement on rotational constraint of the knee reconstructed using patellar tendon autografts. Arthroscopy 20:294–299
Sommerlath K, Lysholm J, Gillquist J (1991) The long-term course after treatment of acute anterior cruciate ligament ruptures. A 9 to 16 year followup. Am J Sports Med 19:156–162
Stergiou N, Ristanis S, Moraiti C, Georgoulis AD (2007) Tibial Rotation in Anterior Cruciate Ligament (ACL)-Deficient and ACL-Reconstructed Knees: a theoretical proposition for the development of osteoarthritis. Sports Med 37:601–613
Stevenson WW III, Johnson DL (2007) Vertical grafts—a common reason for functional failure after ACL reconstruction. Orthopedics 30:206–209
Strehl A, Eggli S (2007) The value of conservative treatment in ruptures of the anterior cruciate ligament (ACL). J Trauma 62:1159–1162
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res (198):43–49
Vasara AI, Jurvelin JS, Peterson L, Kiviranta I (2005) Arthroscopic cartilage indentation and cartilage lesions of anterior cruciate ligament-deficient knees. Am J Sports Med 33:408–414
Zysk SP, Refior HJ (2000) Operative or conservative treatment of the acutely torn anterior cruciate ligament in middle-aged patients. A follow-up study of 133 patients between the ages of 40 and 59 years. Arch Orthop Trauma Surg 120:59–64
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kessler, M.A., Behrend, H., Henz, S. et al. Function, osteoarthritis and activity after ACL-rupture: 11 years follow-up results of conservative versus reconstructive treatment. Knee Surg Sports Traumatol Arthr 16, 442–448 (2008). https://doi.org/10.1007/s00167-008-0498-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-008-0498-x