Abstract
Purpose
After acute myocardial infarction (AMI), left ventricular (LV) remodelling may occur despite successful reperfusion. This study aimed to investigate by gated single photon emission computed tomography (SPECT) the long-term evolution of myocardial perfusion and LV function after AMI and to identify the predictors of LV remodelling.
Methods
Sixty-eight AMI patients successfully treated by primary percutaneous coronary intervention underwent 99mTc-sestamibi gated SPECT at 1 month (baseline) and over 6-month follow-up after the acute event. LV remodelling was defined as 20% increase in LV end-diastolic volume at follow-up.
Results
At baseline, patients with remodelling (n = 14) showed larger (infarct size 29.3 ± 7.8%) and more transmural (infarct severity 0.28 ± 0.10) infarctions, and reduced LV ejection fraction (35.4 ± 5.6%), but similar LV volume indexes, compared to patients without remodelling (n = 54) (infarct size 20.8 ± 14.4%, p < 0.05, infarct severity 0.40 ± 0.11, p < 0.001, ejection fraction 44.5 ± 9.2, p < 0.001). At stepwise multivariate regression analysis, infarct severity showed the best predictive value for predicting LV remodelling (F = 5.54, p < 0.05). Using the thresholds identified by receiver-operating characteristic curve analysis, infarct size and severity detected patients with remodelling with 75% accuracy and 95% negative predictive value. Infarct resorption (defined as the defect size difference between follow-up and baseline) was comparable between patients with (−4.4 ± 8.4%) and without remodelling (−6.8 ± 9.4%) (p = NS).
Conclusion
Perfusion parameters assessed by gated SPECT in the subacute phase after successfully treated AMI correlate with changes in functional parameters at long-term follow-up. Infarct severity is more effective than infarct size, but both are helpful for predicting LV remodelling.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Left ventricular (LV) remodelling after an acute myocardial infarction (AMI) is defined as the progressive dilatation and change in shape, size and function of the left ventricle, occurring even after an effective reperfusion therapy such as thrombolysis or percutaneous coronary intervention (PCI) [1]. It represents an important cause of heart failure and is a predictor of mortality [2, 3]. Several factors have been demonstrated to influence the evolution of LV volumes after AMI, among which there are size, location and transmurality of the infarction, residual viability in the infarct territory and patency of the infarct-related artery [4]. The relative role of these factors, however, is still unclear. Previous perfusion single photon emission computed tomography (SPECT) data showed that infarct size measured 1 week after AMI is predictive of LV remodelling [5]. Using gated SPECT, a progressive reduction in infarct size was observed after primary PCI and was associated with a favourable short-term evolution of LV function [6]. These results have been confirmed also using cardiac magnetic resonance imaging. Orn et al. [7] showed that only scar size, but neither location nor transmurality, was the primary determinant of long-term LV remodelling. Lund et al. [8] identified an infarct size threshold of 24% as predictive of LV remodelling; moreover, they found that patients with LV remodelling had a greater infarct size reduction, i.e. larger infarct resorption, than patients with preserved LV volumes. In disagreement with these data, studies exploring functional abnormalities by echocardiography [9, 10] or the presence of Q waves on the electrocardiogram [11] indicated that infarct transmurality and the presence of residual viability in the infarct territory could be more important than the infarct size in influencing LV remodelling. The relation between infarct severity and LV functional outcome was also confirmed in gated SPECT studies, showing that infarct severity was more effective than infarct size for predicting subsequent LV remodelling [12, 13].
The purpose of this study was to investigate the evolution of perfusion and functional parameters using gated SPECT acquired at 1 month and then over 6 months after AMI in a group of patients successfully treated with primary PCI in order to evaluate the relationship between changes in myocardial perfusion and LV functional outcome at long-term follow-up and the accuracy of baseline perfusion and functional parameters for predicting LV remodelling at follow-up.
Materials and methods
Patient population and study protocol
This study included 68 patients (57 men, mean age 59.7 ± 11.7 years, range 33–87) admitted to our institutions because of their first AMI and submitted to successful primary PCI, defined as Thrombolysis in Myocardial Infarction trial flow grade 3 [14] and residual stenosis of <30% of lumen diameter, within 6 h of symptom onset. The diagnosis of AMI was based on the following criteria: (1) chest pain lasting >30 min and (2) >0.1-mV ST segment elevation in at least two contiguous electrocardiographic leads. Prior AMI was excluded based on history, electrocardiogram and echocardiographic pattern. Other exclusion criteria were cardiac disease other than coronary artery disease and life-limiting noncardiac disease. Patients underwent resting 99mTc-sestamibi gated SPECT at 1 month (baseline) of index AMI (mean 19 ± 14 days) and after a follow-up of at least 6 months (mean 380 ± 358 days, minimum 180 days). The Ethics Committees of our Institutions approved the protocol and all subjects provided informed consent.
Gated SPECT
Baseline and follow-up gated SPECT were acquired 60 min after injection at rest of 99mTc-sestamibi (740 MBq), using a dual-head camera (SKYlight, Philips Medical Systems, Milpitas, CA, USA or e.cam, Siemens Medical Systems, Hoffman Estates, IL, USA) equipped with high-resolution collimators. Acquisition protocol parameters were the following: 180° rotation arc, 32 projections, 60 s/projection, 8 frames/heart cycle and 64 × 64 matrices. The studies were reconstructed using filtered backprojection without attenuation or scatter correction and realigned along the heart axis. Perfusion defects at rest were quantified as percentage of LV wall, with the defect threshold set at 60% of peak uptake [15]. Infarct severity at rest was defined as the lowest ratio of minimal to maximal counts in the short-axis slices examined for infarct size evaluation [16, 17]. Therefore, the lower the infarct severity value the more transmural is the infarction. The QGS algorithm (Cedars-Sinai Medical Center, Los Angeles, CA, USA) was used to measure LV end-diastolic volume (EDV), end-systolic volume (ESV) and ejection fraction (EF) [18]. Volumetric data were corrected for body surface area and expressed as indexes (I). Remodelling was defined as an increase in LVEDVI at follow-up ≥ 20% of the baseline value [19].
Statistical analysis
Data are expressed as mean value ± SD. The comparisons between groups were performed with Student’s t test for unpaired samples or the Mann-Whitney U test, as appropriate. The within-group comparisons were made with Student’s t test for paired samples. The comparison of proportion was made with Fisher’s exact test. Linear regression analysis was used to investigate the possible relationship between perfusion and function. Correlations between the change in infarct size and the changes in functional parameters were analysed using Pearson’s correlation coefficient. Stepwise multivariate and binary analyses including candidate predictive variables were performed by logistic regression analysis in order to identify independent predictors of LV remodelling. Receiver-operating characteristic (ROC) curve analysis was used for the selection of the best cutoff value of gated SPECT parameters significantly different between the two groups for the prediction of LV remodelling. A p value <0.05 was considered statistically significant.
Results
Demographic and clinical characteristics of the patient population are summarized in Table 1. None of the patients had cardiac events during the follow-up period. In the overall study population, at follow-up gated SPECT there was a reduction in the infarct size (from 22.6 ± 13.7% to 16.3 ± 12.2%, p < 0.0001) and an improvement of the infarct severity (from 0.38 ± 0.12 to 0.42 ± 0.14, p < 0.0001). LVEF showed a marginal but significant improvement (from 42.6 ± 9.3% to 44.9 ± 10.8%, p < 0.05). There was a moderate correlation between the change in infarct size and the change in LVEF (r = −0.42, p < 0.0001) and per cent changes in LVEDVI (r = 0.39, p < 0.005) and LVESVI (r = 0.26, p < 0.05) (Fig. 1).
Correlation between infarct size change and a change in LVEF (r = −0.42, p < 0.0001), b per cent change in LVEDVI (r = 0.39, p < 0.005) and c per cent change in LVESVI (r = 0.26, p < 0.05) in all patients (solid line). White dots indicate patients without LV remodelling and black dots patients with LV remodelling. Only patients without LV remodelling showed correlation between infarct size change and a change in LVEF (r = −0.43, p < 0.005), b per cent change in LVEDVI (r = 0.27, p = 0.05) and c per cent change in LVESVI (r = 0.41, p < 0.005) (dashed line)
Results in patients with and without remodelling
There were 14 patients in whom the EDVI increased over the remodelling threshold and 54 patients without remodelling. As shown in Table 1, no significant differences were observed in the main demographic and clinical characteristics of the two groups of patients.
Baseline and follow-up gated SPECT data for patients with and without remodelling are shown in Table 2. In patients without remodelling, there was a significant correlation between the change in infarct size and the change in LVEF (r = −0.43, p < 0.005) and the per cent change in LVESVI (r = 0.41, p < 0.005), whilst the correlation with per cent change in LVEDVI was just borderline (r = 0.27, p = 0.05) (Fig. 1). In patients with LV remodelling, there was no significant correlation between changes in perfusion and in functional parameters.
At baseline, patients with remodelling had larger (p < 0.05) and more transmural (p < 0.001) infarctions as compared to patients without remodelling. Baseline LVEF was significantly (p < 0.001) reduced in patients with remodelling, while LV volume indexes were not different between the two groups. At follow-up, in the group with remodelling, volumes increased significantly (p < 0.001), while infarct size, infarct severity and LVEF did not change (Fig. 2). Conversely, in the group without remodelling there was a significant decrease in infarct size and transmurality (both p < 0.001) that was accompanied by a significant functional improvement with higher LVEF and smaller volume indexes (all p < 0.05) (Fig. 2). Accordingly, at follow-up infarct size (p < 0.005) and severity (p < 0.0001) and LVEF (p < 0.0001) of the remodelling versus non-remodelling patients became more significantly different than at baseline and the volume indexes became significantly larger (both p < 0.0001). The infarct resorption (defined as the defect size difference between follow-up and baseline) was not different between patients with and without remodelling (−4.4 ± 8.4% and −6.8 ± 9.4%, respectively, p = NS) (Fig. 3).
Predictors of LV remodelling
According to stepwise multivariate regression analysis, infarct severity was the only significant predictor of per cent change in EDVI (F = 5.54, p < 0.05). Using stepwise binary logistic regression analysis, baseline infarct severity, LVEF and EDVI were identified as significant predictors of LV remodelling, correctly classifying 85.3% of patients into the two groups (p < 0.05).
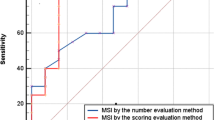
Results of ROC curve analysis of gated SPECT variables are shown in Table 3. According to both infarct size and severity cutoff values extracted from ROC curve analysis, patients were divided into two risk groups. The first group included 27 “high-risk” patients, with infarct size >22.3% and infarct severity <0.36 at baseline. Within this group, 12 of 27 patients (44%) showed LV remodelling at follow-up. The remaining 41 patients composed a “low-risk” group, including patients with both infarct size <22.3% and severity >0.36 (33 patients) or with one abnormal parameter only (either infarct size, 5 patients, or severity, 3 patients). Only 2 of 41 (5%) of these patients presented remodelling at follow-up. By dividing the patients into these two risk groups, the cutoff values of infarct size (22.3%) and infarct severity (0.36), considered together, demonstrated 86% sensitivity, 72% specificity, 44% positive predictive value, 95% negative predictive value and 75% accuracy for predicting remodelling (Fig. 4).
Discussion
We observed that infarct size and severity assessed by perfusion gated SPECT correlate with changes in LV functional parameters at long-term follow-up and are able to predict LV remodelling with clinically acceptable accuracy. The main novel findings of this study are the following: (1) among perfusion parameters, infarct severity was the only significant predictor of LV remodelling according to multivariate analysis and (2) infarct resorption was comparable in patients with and without LV remodelling, despite previous results with cardiac magnetic resonance imaging reporting greater infarct resorption in patients with remodelling [8].
The extent of infarct size in patients treated with primary PCI has been extensively used not only to confirm the success of revascularization [20, 21], but also as a strong prognostic predictor [22, 23]. This study confirms that in patients submitted to successful PCI a spontaneous reduction in infarct size occurs beyond the 1-month evaluation. These findings are in agreement with previous studies reporting a significant late reduction in defect size in paired sestamibi SPECT studies performed early and a few months after AMI in patients treated conservatively or by thrombolysis [6, 24, 25]. Various mechanisms might play a role in this delayed perfusion improvement. The presence of vascular stunning in the region of the infarction may persist for weeks after restoration of blood flow [26] and the gradual recovery of microvascular function may then result in a delayed reduction of the perfusion defect size. Furthermore, the myocardial infarction area may decrease in the weeks after AMI due to oedema reabsorption and phagocytation of dead myocardial cells and collagen production and contraction [27]. We found a significant relationship between late reduction in infarct size and improvement in LV function. This finding might be explained by the fact that a significant reduction in perfusion defect is a prerequisite for LV function recovery, and therefore represents a marker of positive LV remodelling. However, we did not register a significant difference in infarct size reduction between patients with and without LV remodelling. Therefore, we were unable to confirm the cardiac magnetic resonance data showing that patients with LV remodelling had substantially larger infarct resorption compared with patients without remodelling [8]. Conversely, our study demonstrates that the reduction of infarct size beyond the subacute phase may occur in all patients, in agreement with prior scintigraphic reports [6, 24, 25]. This means that infarct resorption could be a spontaneous event occurring after AMI independently of its size and of the patients’ outcome [26, 27]. Analysing separately patients with and without LV remodelling, however, a significant correlation between infarct resorption and LV functional changes was observed only in the latter group. This could imply a causative role of infarct resorption for LV functional recovery.
On the other hand, the lack of correlation between infarct resorption and functional evolution in patients with LV remodelling suggests that other factors play a major role in determining an unfavourable functional outcome. We observed that infarct size and severity could be significant predictors of LV remodelling. Several clinical studies demonstrated that various parameters are predictive of remodelling, including anterior infarct location, patency of the infarct-related artery, perfusion and functional parameters [4–13]. In agreement with these previous findings, the present study showed a number of baseline parameters predictive of remodelling, infarct severity demonstrating the best predictive value. Our results are in disagreement with the studies showing infarct size as the single significant predictor of LV remodelling after AMI [5, 7], but are consistent with previous studies demonstrating that the severity of the infarction might be the best predictor of subsequent changes in LV geometry and performance and is associated with LV volume enlargement at follow-up [12, 13]. Because infarct severity, assessed by SPECT, might be considered an estimate of infarct transmurality, as demonstrated also by several studies [28], our findings indirectly confirm that the presence of residual viability in the infarct territory could favourably influence LV remodelling in long-term follow-up. Indeed, the preservation of viable myocardium in the subepicardium has been demonstrated to be a crucial mechanism for maintaining LV shape and for preventing infarct expansion [29].
According to our data, gated SPECT infarct size and severity demonstrated a potential clinical utility in the early identification of patients who will develop LV remodelling at follow-up. Using the threshold values that were identified by ROC curve analysis, in addition to good sensitivity, specificity and accuracy, infarct size and severity demonstrated a very strong negative predictive value. In the subacute phase of reperfused AMI, this is a major issue regarding the good prognosis and the benign clinical course of these patients [3]. Identification of low-risk patients allows focusing the attention on higher-risk patients who would need a more aggressive therapy and clinical follow-up. Interestingly, the infarct size threshold that we found most effective was practically the same that has been reported using cardiac magnetic resonance imaging [8].
To the best of our knowledge, the present study is possibly the first in which both myocardial perfusion and LV function have been evaluated with gated SPECT 1 month after AMI as well as at long-term follow-up, differently from most prior reports in which functional data were derived from other techniques, or gated SPECT data were collected over a short time interval [5, 6, 12, 13]. 99mTc-Sestamibi gated SPECT combines an accurate evaluation of both infarct size and infarct severity with reliable measures of LV function and volumes [30–33]. In addition, gated SPECT proved to be accurate and robust in the evaluation of LV function, compared to more established modalities [34], and also to have a good reproducibility, even after a prolonged time interval [35]. Another imaging technique capable of providing such double information is cardiac magnetic resonance [7, 8]. Although this technique is more accurate in visualizing AMI scars and measuring LV volumes than gated SPECT, the latter technique still remains the most easily and widely available method to perform stress myocardial perfusion imaging and to detect inducible ischaemia, with the additional advantage of permitting the use of dynamic exercise as stressor. Therefore, in the follow-up of patients already examined early after AMI, the execution of stress-rest perfusion gated SPECT would allow the comprehensive evaluation of both residual ischaemia and LV functional evolution.
This study has some limitations that must be considered. The patient population is relatively small and retrospectively selected according to the availability of the gated SPECT studies. In general, most of the studies dealing with the issue of long-term functional evolution after reperfusion therapy include a limited number of patients. Subjects with a history of prior infarction as well as patients with suboptimal PCI results were not considered; therefore, our observations might not apply to those patients. Finally, perfusion recovery at the follow-up study could be at least in part a consequence of functional improvement, even if there is evidence from previous reports that a delayed perfusion recovery occurs in a significant number of patients after PCI [6, 24, 25]. However, the decrease in infarct size observed in patients with LV remodelling suggests that functional improvement is not the sole determinant of perfusion changes at follow-up.
Conclusion
The results of this study demonstrated a correlation between perfusion parameters measured in the subacute phase after AMI and change of functional parameters at long-term follow-up. Infarct severity and infarct size assessed using gated SPECT are able to predict LV remodelling with clinically acceptable accuracy.
References
Cohn JN, Ferrari R, Sharpe N. Cardiac remodeling–concepts and clinical implications: a consensus paper from an international forum on cardiac remodeling. J Am Coll Cardiol 2000;35:569–82.
Touboul P, Andre-Fouët X, Leizorovicz A, Itti R, Lopez M, Sayegh Y, et al. Risk stratification after myocardial infarction. A reappraisal in the era of thrombolysis. The Groupe d’Etude du Pronostic de l’Infarctus du Myocarde (GREPI). Eur Heart J 1997;18:99–107.
Bax JJ, Schinkel AF, Boersma E, Elhendy A, Rizzello V, Maat A, et al. Extensive left ventricular remodeling does not allow viable myocardium to improve in left ventricular ejection fraction after revascularization and is associated with worse long-term prognosis. Circulation 2004;110(11 Suppl 1):II18–22.
Gaudron P, Eilles C, Kugler I, Ertl G. Progressive left ventricular dysfunction and remodeling after myocardial infarction. Potential mechanisms and early predictors. Circulation 1993;87:755–63.
Chareonthaitawee P, Christian TF, Hirose K, Gibbons RJ, Rumberger JA. Relation of initial infarct size to extent of left ventricular remodeling in the year after acute myocardial infarction. J Am Coll Cardiol 1995;25:567–73.
Castro PF, Corbalan R, Baeza R, Nazzal C, Greig DP, Miranda FP, et al. Effect of primary coronary angioplasty on left ventricular function and myocardial perfusion as determined by Tc-99m sestamibi scintigraphy. Am J Cardiol 2001;87:1181–4.
Orn S, Manhenke C, Anand IS, Squire I, Nagel E, Edvardsen T, et al. Effect of left ventricular scar size, location, and transmurality on left ventricular remodeling with healed myocardial infarction. Am J Cardiol 2007;99:1109–14.
Lund GK, Stork A, Muellerleile K, Barmeyer AA, Bansmann MP, Knefel M, et al. Prediction of left ventricular remodeling and analysis of infarct resorption in patients with reperfused myocardial infarcts by using contrast-enhanced MR imaging. Radiology 2007;245:95–102.
Bolognese L, Buonamici P, Cerisano G, Santini A, Carrabba N, Santoro GM, et al. Early dobutamine echocardiography predicts improvement in regional and global left ventricular function after reperfused acute myocardial infarction without residual stenosis of the infarct-related artery. Am Heart J 2000;139(1 Pt 1):153–63.
Bolognese L, Neskovic AN, Parodi G, Cerisano G, Buonamici P, Santoro GM, et al. Left ventricular remodeling after primary coronary angioplasty: patterns of left ventricular dilation and long-term prognostic implications. Circulation 2002;106:2351–7.
Irimpen AM, Tenaglia AN, Shin DJ, Buda AJ. Lack of ventricular remodeling in non-Q-wave myocardial infarction. Am Heart J 1996;131:466–71.
Lipiecki J, Cachin F, Durel N, de Tauriac O, Ponsonnaille J, Maublant J. Influence of infarct-zone viability detected by rest Tc-99m sestamibi gated SPECT on left ventricular remodeling after acute myocardial infarction treated by percutaneous transluminal coronary angioplasty in the acute phase. J Nucl Cardiol 2004;11:673–81.
Ernande L, Cachin F, Chabrot P, Durel N, Morand D, Boyer L, et al. Rest and low-dose dobutamine Tc-99m-mibi gated-SPECT for early prediction of left ventricular remodeling after a first reperfused myocardial infarction. J Nucl Cardiol 2009;16:597–604.
The TIMI Study Group. The Thrombolysis in Myocardial Infarction (TIMI) trial. Phase I findings. N Engl J Med 1985;312:932–6.
O’Connor MK, Hammel T, Gibbons RJ. In vitro validation of a simple tomographic technique for estimation of percentage myocardium at risk using methoxyisobutyl isonitrile technetium 99m (sestamibi). Eur J Nucl Med 1990;17:69–76.
Christian TF, Schwartz RS, Gibbons RJ. Determinants of infarct size in reperfusion therapy for acute myocardial infarction. Circulation 1992;86:81–90.
Christian TF, O’Connor MK, Schwartz RS, Gibbons RJ, Ritman EL. Technetium-99m MIBI to assess coronary collateral flow during acute myocardial infarction in two closed-chest animal models. J Nucl Med 1997;38:1840–6.
Germano G, Kiat H, Kavanagh PB, Moriel M, Mazzanti M, Su HT, et al. Automatic quantification of ejection fraction from gated myocardial perfusion SPECT. J Nucl Med 1995;36:2138–47.
Bolognese L, Cerisano G, Buonamici P, Santini A, Santoro GM, Antoniucci D, et al. Influence of infarct-zone viability on left ventricular remodeling after acute myocardial infarction. Circulation 1997;96:3353–9.
Gibson WS, Christian TF, Pellikka PA, Behrenbeck T, Gibbons RJ. Serial tomographic imaging with technetium-99m-sestamibi for the assessment of infarct-related artery patency following reperfusion therapy. J Nucl Med 1992;33:2080–5.
Gibbons RJ, Miller TD, Christian TF. Infarct size measured by single photon emission computed tomographic imaging with (99m)Tc-sestamibi: a measure of the efficacy of therapy in acute myocardial infarction. Circulation 2000;101:101–8.
Gibbons RJ, Miller TD. Tc-99m sestamibi infarct size as a surrogate endpoint. J Nucl Cardiol 2005;12:12–9.
Miller TD, Hodge DO, Sutton JM, Grines CL, O’Keefe JH, DeWood MA, et al. Usefulness of technetium-99m sestamibi infarct size in predicting posthospital mortality following acute myocardial infarction. Am J Cardiol 1998;81:1491–3.
Galli M, Marcassa C, Bolli R, Giannuzzi P, Temporelli PL, Imparato A, et al. Spontaneous delayed recovery of perfusion and contraction after the first 5 weeks after anterior infarction. Evidence for the presence of hibernating myocardium in the infarcted area. Circulation 1994;90:1386–97.
Ndrepepa G, Mehilli J, Martinoff S, Schwaiger M, Schömig A, Kastrati A. Evolution of left ventricular ejection fraction and its relationship to infarct size after acute myocardial infarction. J Am Coll Cardiol 2007;50:149–56.
Uren NG, Crake T, Lefroy DC, de Silva R, Davies GJ, Maseri A. Delayed recovery of coronary resistive vessel function after coronary angioplasty. J Am Coll Cardiol 1993;21:612–21.
Reimer KA, Lowe JE, Rasmussen MM, Jennings RB. The wavefront phenomenon of ischemic cell death. 1. Myocardial infarct size vs duration of coronary occlusion in dogs. Circulation 1977;56:786–94.
Hayat SA, Janardhanan R, Moon JCC, Pennell DJ, Senior R. Comparison between myocardial contrast echocardiography and single-photon emission computed tomography for predicting transmurality of acute myocardial infarction. Am J Cardiol 2006;97:1718–21.
Kaul S. There may be more to myocardial viability than meets the eye! Circulation 1995;92:2790–3.
Verberne HJ, Dijkgraaf MG, Somsen GA, van Eck-Smit BL. Stress-related variations in left ventricular function as assessed with gated myocardial perfusion SPECT. J Nucl Cardiol 2003;10:456–63.
De Winter O, De Bondt P, Van De Wiele C, De Backer G, Dierckx RA, De Sutter J. Day-to-day variability of global left ventricular functional and perfusional measurements by quantitative gated SPECT using Tc-99m tetrofosmin in patients with heart failure due to coronary artery disease. J Nucl Cardiol 2004;11:47–52.
Sciagrà R, Imperiale A, Antoniucci D, Migliorini A, Parodi G, Comis G, et al. Relationship of infarct size and severity versus left ventricular ejection fraction and volumes obtained from 99mTc-sestamibi gated single-photon emission computed tomography in patients treated with primary percutaneous coronary intervention. Eur J Nucl Med Mol Imaging 2004;31:969–74.
Sciagrà R, Parodi G, Pupi A, Migliorini A, Valenti R, Moschi G, et al. Gated SPECT evaluation of outcome after abciximab-supported primary infarct artery stenting for acute myocardial infarction: the scintigraphic data of the abciximab and carbostent evaluation (ACE) randomized trial. J Nucl Med 2005;46:722–7.
Acampa W, Caprio MG, Nicolai E, Liuzzi R, De Luca S, Capasso E, et al. Assessment of poststress left ventricular ejection fraction by gated SPECT: comparison with equilibrium radionuclide angiocardiography. Eur J Nucl Med Mol Imaging 2010;37:349–56.
Sciagrà R, Berti V, Genovese S, Pupi A. Reliability of myocardial perfusion gated SPECT for the reproducible evaluation of resting left ventricular functional parameters in long-term follow-up. Eur J Nucl Med Mol Imaging 2010;37:1722–9.
Acknowledgments
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Berti, V., Sciagrà, R., Acampa, W. et al. Relationship between infarct size and severity measured by gated SPECT and long-term left ventricular remodelling after acute myocardial infarction. Eur J Nucl Med Mol Imaging 38, 1124–1131 (2011). https://doi.org/10.1007/s00259-011-1739-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-011-1739-7