Abstract
Introduction
Discriminating among benign chondroid tumors, low-grade chondrosarcomas, and grade 2/3 chondrosarcomas is frequently difficult with standard imaging modalities. We systematically reviewed the literature to determine the performance of PET-CT in making this distinction.
Methods
A systematic review was performed identifying 811 PubMed- and Embase-indexed articles containing combinations of “chondrosarcoma,” “enchondroma,” “chondroid,” “cartilage” and “PET/CT,” “PET,” “positron.” Eight articles including 166 lesions were included. Age, gender, tumor size, histologic grade, and SUVmax values were extracted for individual lesions when possible and otherwise recorded as aggregated data. Comparisons in SUVmax among benign, low-grade, and intermediate-/high-grade chondroid neoplasms were made.
Results
Individual SUVs were available for 101 lesions; 65 additional lesions were reported as aggregated data. There were 101 malignant and 65 benign tumors. Benign tumors were seen more frequently in females (p = 0.04, Fischer’s exact test), but malignancy was not associated with age or lesion size. SUVmax was lower for benign (1.6 ± 0.7) than malignant tumors (4.4 ± 2.5) (p < 0.0001, t-test). SUVmax was lower for grade 0/1 (2.0 ± 0.7) than grade 2/3 (6.0 ± 3.2) (p < 0.0001, t-test). Increasing SUVmax correlated with higher grade chondroid tumors (Spearman’s rank, ρ = 0.78). SUVmax ≥4.4 was 99% specific for grade 2/3 chondrosarcoma.
Conclusions
SUVmax correlates with histologic grade in intraosseous chondroid neoplasms; very low SUVmax supports a diagnosis of benign tumor, while elevated SUVmax is suggestive of higher grade chondrosarcoma.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Differentiation among chondroid neoplasms of bone continues to pose problems in diagnosis and management for both radiologists and orthopaedic oncologists [1]. Treatment options vary depending on whether a lesion is diagnosed as an enchondroma/osteochondroma, where asymptomatic lesions can be followed; low-grade chondrosarcoma, where intralesional curettage or close surveillance is advocated; or intermediate/high-grade chondrosarcoma, where wide resection is appropriate. Clinically, chondrosarcoma is classically associated with an increase in pain, but the presenting signs and symptoms are often nonspecific and can frequently be attributed to other musculoskeletal pathologies (such as rotator cuff tear, osteoarthritis, etc.). Furthermore, there are overlapping radiologic features particularly between enchondroma and low-grade chondrosarcoma [1], but also between low and intermediate/high-grade chondrosarcoma and across imaging modalities (radiography, CT, TC99m bone scintigraphy, and MRI) [2, 3].
Because of these diagnostic difficulties, image-guided percutaneous biopsy is often performed in an attempt to obtain a definitive diagnosis. While percutaneous biopsy of chondroid neoplasms has a reported accuracy of 86% [4], the underlying heterogeneity of these tumors makes them susceptible to under-sampling [5] and inadequate initial treatment. Thus, more accurate diagnostic techniques are needed to aid in clinical decision-making and surgical planning.
One modality that may be currently under-utilized is 18F-FDG PET-CT, which offers direct assessment of tumor metabolic activity. There have been preliminary investigations into the value of PET-CT in distinguishing low-/intermediate-grade chondrosarcomas from benign chondroid neoplasms, but these studies have been conducted with relatively small sample sizes [6,7,8]. The purpose of our study was to systematically review the literature to determine whether PET-CT can aid in differentiating benign from malignant chondroid tumors.
Materials and methods
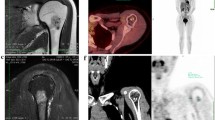
IRB approval was waived for this study because data were collected from existing publications available to the public. The PubMed and EMBASE search engines were used to identify all relevant publications since 1995. Articles including the following terms and Boolean operators: (“chondrosarcoma” OR “enchondroma” OR “chondroid” OR “cartilage”) AND (“PET” OR “positron”) were initially searched. Before commencing our search, certain inclusion and exclusion criteria were defined. Articles were considered eligible if they met the following inclusion criteria: (1) the target population consisted of patients with chondrogenic bone tumors; (2) PET-CT of these tumors was described adequately; (3) at least five chondroid bone tumors were included. Case reports, review papers, expert opinion articles, editorials, letters to the editor, publications on congress proceedings, and manuscripts that contained redundantly reported data were excluded (Fig. 1). Most of the citations were excluded after examining the title or retrieved abstract. Additional relevant articles were identified by reviewing these included articles and searching for both references contained in the manuscript and publications that subsequently cited the manuscripts. Reviewers were not blinded to the names of authors, institutions, or journals.
Information recorded from the publications included: patient demographics (age and gender), tumor histology and grade, tumor size, and maximum standardized uptake value (SUVmax). Dedifferentiated chondrosarcomas were considered grade 2/3 tumors. Chondromyxoid fibromas and chondroblastomas were excluded because of their dissimilar histologic matrix, containing mixed myofibroblastic (in chondromyxoid fibromas) and epithelioid (in chondroblastoma) components [9,10,11]. When possible, individual SUVmax values were recorded; otherwise, means of SUVmax were recorded as aggregate data. Weighted averages of SUVs were calculated so that pooled sample means and standard deviations were available for the different tumor groups. To avoid bias that would result from selectively eliminating cases with missing standard deviations (SDs), these values were imputed for the aggregate data from two articles [7, 12]; to do this, we used histology-specific SDs derived from data on individual lesions, specifically, imputed SDs of 0.81 for 19 benign tumors and 4.4 for 11 chondrosarcomas where the grade was unspecified.
Demographics were compared among subjects with available individual data, and differences between those with benign and malignant tumors were examined using Fischer’s exact tests and two-sample t-tests. Funnel plots and forest plots were generated to assess for publication bias and study heterogeneity (Comprehensive Meta-Analysis, v. 3, Biostat, Englewood, NJ, USA). Statistical analysis was performed using Stata 13.1 (StataCorp, College Station, TX, USA). For all analyses, results were considered statistically significant for p < 0.05.
Results
There were a total of 166 chondroid neoplasms identified in eight articles that met inclusion criteria (Table 1) [6,7,8, 12,13,14,15,16]. Of all 166 tumors, there were 65 benign (osteochondroma or enchondroma) and 101 malignant tumors: 45 low-grade chondrosarcomas and 56 intermediate or high grade chondrosarcomas. Of these, the individual tumor SUVmax was available for 101 subjects, collated from 6 articles; among these, there were 33 benign and 68 malignant lesions; gender was reported for 96 subjects: there were 59 females and 37 males. Mean age was 46.7 (range 20–85 years). For malignancy, mean age was 45.9 years, statistically no different than the 48.3 years of those with benign tumors (p = 0.49, two-sample t-test). Among benign lesions there was a female predominance (24 females: 7 males), whereas malignant lesions showed a more even gender distribution (35 females: 30 males), p = 0.04 (Fischer’s exact test). There was a trend toward larger lesions being malignant, with mean maximum diameter of 7.0 cm (SD 3.5 cm, n = 46) vs. benign at 5.4 cm (SD 3.9 cm, n = 17), p = 0.13 (two-sample t-test).
Forest plots (Fig. 2) were constructed according to tumor histology (benign, low-grade, and intermediate/high-grade chondrosarcoma) and demonstrate significant differences in reported values of SUVmax between benign and malignant tumors: benign chondroid lesion SUVmax averaged 1.62 (SD 0.74) vs. the all chondrosarcoma mean of 4.43 (SD 2.46) (p < 0.0001, unpaired t-test). Moreover, benign lesions were less FDG avid than low-grade chondrosarcomas, which showed a mean SUVmax of 2.5 (SD 0.9) (p < 0.0001). When grouped together, benign/low-grade chondrosarcoma had a lower SUVmax than grade 2/3 chondrosarcoma: 2.0 (SD 0.7) vs. 6.0 (SD 3.2), respectively, p < 0.0001.
Forest plots show the range of SUVmax for individual studies, grouped according to tumor histology. There was considerable heterogeneity among studies when subgrouped in this fashion, with I2 values of 78% and 94% for the benign and low-grade tumors, respectively, but no heterogeneity in the intermediate/high-grade category (I2 = 0%). The high heterogeneity for low-grade neoplasms derives, in part, from the small number of studies in this review, as I2 depends on degrees of freedom (n-1). The trend for higher grade tumors showing increased SUVmax is apparent when the plots are compared against each other (n.b.: difference in scale for low-grade tumors vs. grade 2/3 chondrosarcoma)
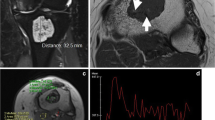
For individual lesions (Fig. 3), SUVmax correlated with histologic grade (Spearman ρ = 0.78; p < 0.0001), as mean SUVmax showed incremental increases with grade going from 2.5, to 4.7, to 7.7 for grade 1, 2, and grade 3 chondrosarcomas, respectively. When the SUVmax was higher than 4.4, specificity for grade 2/3 chondrosarcoma was 99%: of the 66 benign/low-grade lesions for which individual data were available, only one grade 1 chondrosarcoma had a SUVmax (5.8) above this value, and no benign tumors did (highest SUVmax for a benign tumor was 2.0). Conversely, a very low SUVmax (≤2) is very likely to be a grade 0 chondroid tumor: 31/37 tumors with SUVmax <2.0 were benign (84% PPV). However, it should be pointed out that 46/101 tumors had individual SUVs that fell between these values, emphasizing the need for correlative clinical history and other imaging studies in such cases.
Dot plot depicting 96 individual SUVmax values of chondroid tumors collated from six articles (among 101 individual SUVmax values, grade was unavailable for 5 chondrosarcomas, and these were excluded from this plot). SUVmax correlates with histologic grade, with mean SUVmax from the entire data set for benign enchondroma/osteochondroma 1.6, grade 1 chondrosarcoma 2.5, and grade 2/3 chondrosarcoma 6.0. Grades 2 and 3 chondrosarcomas are combined because clinically they are treated similarly. Below a SUVmax of 2 (solid line), a chondroid tumor is highly likely to be benign; above a SUVmax of 4.5 (dashed line), a chondroid tumor is highly likely to be an intermediate- or high-grade chondrosarcoma. PET-CT may thus assist in clinical decision-making and managing patient expectations when SUVs fall beyond these threshold values. Values between 2 and 4.5 are sufficiently non-specific as to require careful correlation among radiography, MRI, and the patient’s clinical presentation to determine the need for percutaneous biopsy or interval follow-up
Discussion
Our review of the published data supports the use of PET-CT as a useful adjunct to conventional imaging in the characterization of chondroid tumors of bone. Accurate imaging diagnosis is essential in guiding management decisions about whether a lesion can be observed, or whether biopsy is needed, and secondly, if a biopsy is performed, whether the histology and imaging findings are concordant. Some authors have reported complications, such as infection or post-procedural fracture, in up to 10% of cases treated intralesionally [17]. Thus, there is a need for identifying patients who can be safely observed rather than operated upon. While distinguishing features of high-grade chondrosarcoma have been reported to include bone expansion, periostitis, extraosseous soft tissue masses, and increased longitudinal tumor diameter [1, 18], substantial difficulty persists in differentiating enchondroma from grade 1 chondrosarcoma even among subspecialist musculoskeletal radiologists. Recently, Crim, et al. reported accuracy of only 21% radiographically, and 58% when incorporating MRI, in making this distinction [19]. Bone scintigraphy, a conventional adjunct to anatomic imaging, shows considerable overlap between enchondroma and low-grade chondrosarcoma [20, 21], with 35% of low-grade chondrosarcomas and 21% of enchondromas exhibiting increased radiotracer uptake [22]. Underlying tumor heterogeneity further confounds diagnosis by engendering biopsy sampling error and histologic under-grading, particularly in pelvic tumors where biopsy concordance with the final resection specimen may be as low as 36% [5].
By offering a means to interrogate tumor metabolic activity as a surrogate for biologic aggressiveness, PET-CT holds the potential to greatly augment the radiologic heuristics employed when confronted with chondroid lesions clinically. Prior retrospective reviews of PET-CT and FDG avidity in bone tumors have included relatively few cases of chondroid tumors, leaving questions regarding its utility in this group of neoplasms largely unanswered [23, 24]. Larger series have suggested SUVmax thresholds of 2.2–2.3 for distinguishing between benign/low-grade and malignant chondroid tumors [8, 14], yielding sensitivities and specificities ≥90% in their respective series. What has not been emphasized in those studies, however, and what we have gleaned from our meta-analysis of multiple publications is the substantial overlap of SUVmax values among both benign and malignant chondroid tumors, resulting in poor specificity for when SUVmax falls between 2 and 4.5. This range of nonspecific SUVmax includes approximately 46% of lesions for which individual SUVmax was available in this meta-analysis.
That said, the significant overlap of histologies through a range of lower SUVmax values should not obscure the clinical import of more extreme SUVmax values. Values in the lower SUV extremes could help the treating clinician/surgeon decide whether simple surveillance is appropriate; for higher SUV extremes, biopsy would be indicated. In fact, our meta-analysis revealed only a single grade 1 chondrosarcoma (and no benign lesions) with a SUVmax >4.4. For lesions with high SUVmax but low-grade chondrosarcoma on needle biopsy, the patient could be counseled regarding the potential for subsequent histologic upgrading based on tissue received from curettage. Thus, our findings suggest that an improved management algorithm could incorporate a strategy of active surveillance when SUVmax is very low and biopsy when SUVmax is high; as SUVmax exceeds the mid 4 to 5 range, suspicion of grade 2/3 chondrosarcoma should rise accordingly.
Based on our results showing that higher grade chondrosarcoma correlates with increased SUVmax values, PET-CT could also reduce the problem of core needle biopsy sampling error. By identifying the region of greatest SUVmax for percutaneous biopsy, PET-CT could reduce the rate of false-negative biopsies. Finally, PET-CT offers the potential to serve as an initial staging study in the setting of malignancy and potentially as a useful adjunct in postoperative imaging surveillance [25].
We acknowledge several limitations to this systematic literature review. While PET offers the potential to quantify radiotracer uptake as a surrogate of tumor grade, there are various technical factors that influence SUV calculations, such as the injected radiotracer dose, patient weight, blood glucose levels (higher blood glucose drives SUV lower), lesion size (for lesions <2–3 cm, measured SUV is less than the true SUV), time interval between radiotracer injection and scanning, image reconstruction algorithms, and scanner calibration [26]. Although SUVmax is less affected than SUVmean by these sources of measurement error and bias, alternative means of volumetrically quantifying whole tumor metabolic activity, or “total lesion glycolysis,” have shown promise in independently predicting overall survival in bone and soft tissue sarcoma [27]. Future studies normalizing lesional SUVmax to blood pool SUVmax could also help mitigate these sources of variability.
One salient limitation of this systematic review was that it was not possible to correlate PET-CT results with other imaging modalities (radiography and MRI) or with clinical signs and symptoms. A second limitation stems from variability in histologic assessment across studies given the various institutions represented. Ideally, correlative studies of histology would be based on a uniform standard for histologic grading or performed by a single pathologist to minimize error associated with interobserver variability. Additionally, chondrosarcoma subtypes (e.g., conventional, myxoid, clear cell) were not reported frequently enough to enable correlative statistics by histologic subtype. In the context of these modality and methodological dependencies, we advocate the use of PET-CT as an adjunct that could better inform treatment decisions, with radiologists working in conjunction with orthopedic surgeons and bone and soft tissue pathologists in determining practical institution-specific thresholds.
Conclusion
In conclusion, this systematic review shows that PET-CT could serve as a useful adjunct in the assessment of chondroid tumors, as SUVmax correlates with histologic grade. While there is considerable overlap of SUVmax values among benign and malignant chondroid neoplasms, particularly in the SUVmax range of 2–4.5, more extreme values provide useful information regarding underlying biologic aggressiveness that can help guide management.
References
Logie CI, Walker EA, Forsberg JA, Potter BK, Murphey MD. Chondrosarcoma: a diagnostic imager’s guide to decision making and patient management. Semin Musculoskelet Radiol. 2013;17(2):101–15.
Murphey MD, Walker EA, Wilson AJ, Kransdorf MJ, Temple HT, Gannon FH. From the archives of the AFIP: imaging of primary chondrosarcoma: radiologic-pathologic correlation. Radiographics. 2003;23(5):1245–78.
Choi B-B, Jee W-H, Sunwoo H-J, Cho J-H, Kim J-Y, Chun K-A, et al. MR differentiation of low-grade chondrosarcoma from enchondroma. Clin Imaging. 2013;37(3):542–7.
Jennings R, Riley N, Rose B, Rossi R, Skinner JA, Cannon SR, et al. An evaluation of the diagnostic accuracy of the grade of preoperative biopsy compared to surgical excision in chondrosarcoma of the long bones. Int J Surg Oncol. 2010;2010:270195.
Roitman PD, Farfalli GL, Ayerza MA, Múscolo DL, Milano FE, Aponte-Tinao LA. Is needle biopsy clinically useful in preoperative grading of central chondrosarcoma of the pelvis and long bones? Clin Orthop. 2016.
Feldman F, Van Heertum R, Saxena C, Parisien M. 18FDG-PET applications for cartilage neoplasms. Skelet Radiol. 2005;34(7):367–74.
Costelloe CM, Chuang HH, Chasen BA, Pan T, Fox PS, Bassett RL, et al. Bone windows for distinguishing malignant from benign primary bone tumors on FDG PET/CT. J Cancer. 2013;4(7):524–30.
Jesus-Garcia R, Osawa A, Filippi RZ, Viola DCM, Korukian M, de Carvalho Campos Neto G, et al. Is PET-CT an accurate method for the differential diagnosis between chondroma and chondrosarcoma? SpringerPlus. 2016;5:236.
Cleven AHG, Höcker S, Briaire-de Bruijn I, Szuhai K, Cleton-Jansen A-M, Bovée JVMG. Mutation analysis of H3F3A and H3F3B as a diagnostic tool for Giant cell tumor of bone and Chondroblastoma. Am J Surg Pathol. 2015;39(11):1576–83.
Romeo S, Eyden B, Prins FA, Briaire-de Bruijn IH, Taminiau AHM, Hogendoorn PCW. TGF-beta1 drives partial myofibroblastic differentiation in chondromyxoid fibroma of bone. J Pathol. 2006;208(1):26–34.
de Silva MVC, Reid R. Chondroblastoma: varied histologic appearance, potential diagnostic pitfalls, and clinicopathologic features associated with local recurrence. Ann Diagn Pathol. 2003;7(4):205–13.
Shin D-S, Shon O-J, Han D-S, Choi J-H, Chun K-A, Cho I-H. The clinical efficacy of (18)F-FDG-PET/CT in benign and malignant musculoskeletal tumors. Ann Nucl med. 2008;22(7):603–9.
Brenner W, Conrad EU, Eary JF. FDG PET imaging for grading and prediction of outcome in chondrosarcoma patients. Eur J Nucl med Mol Imaging. 2004;31(2):189–95.
Lee FY-I, Yu J, Chang S-S, Fawwaz R, Parisien MV. Diagnostic value and limitations of fluorine-18 fluorodeoxyglucose positron emission tomography for cartilaginous tumors of bone. J Bone Joint Surg am. 2004;86–A(12):2677–85.
Purandare NC, Rangarajan V, Agarwal M, Sharma AR, Shah S, Arora A, et al. Integrated PET/CT in evaluating sarcomatous transformation in osteochondromas. Clin Nucl med. 2009;34(6):350–4.
Strobel K, Exner UE, Stumpe KDM, Hany TF, Bode B, Mende K, et al. The additional value of CT images interpretation in the differential diagnosis of benign vs. malignant primary bone lesions with 18F-FDG-PET/CT. Eur J Nucl med Mol Imaging. 2008;35(11):2000–8.
Dierselhuis EF, Gerbers JG, Ploegmakers JJW, Stevens M, Suurmeijer AJH, Jutte PC. Local treatment with adjuvant therapy for central atypical cartilaginous tumors in the long bones: analysis of outcome and complications in one hundred and eight patients with a minimum follow-up of two years. J Bone Joint Surg am. 2016;98(4):303–13.
Douis H, Singh L, Saifuddin A. MRI differentiation of low-grade from high-grade appendicular chondrosarcoma. Eur Radiol. 2014;24(1):232–40.
Crim J, Schmidt R, Layfield L, Hanrahan C, Manaster BJ. Can imaging criteria distinguish enchondroma from grade 1 chondrosarcoma? Eur J Radiol. 2015;84(11):2222–30.
Arsos G, Venizelos I, Karatzas N, Koukoulidis A, Karakatsanis C. Low-grade chondrosarcomas: a difficult target for radionuclide imaging. Case report and review of the literature. Eur J Radiol. 2002;43(1):66–72.
Kaya GC, Demir Y, Ozkal S, Sengoz T, Manisali M, Baran O, et al. Tumor grade-related thallium-201 uptake in chondrosarcomas. Ann Nucl med. 2010;24(4):279–86.
Ferrer-Santacreu EM, Ortiz-Cruz EJ, Díaz-Almirón M, Pozo Kreilinger JJ. Enchondroma versus chondrosarcoma in long bones of appendicular skeleton: clinical and radiological criteria—a follow-up. J Oncol. 2016;2016:8262079.
Liu F, Zhang Q, Zhu D, Li Z, Li J, Wang B, et al. Performance of positron emission tomography and positron emission tomography/computed tomography using fluorine-18-fluorodeoxyglucose for the diagnosis, staging, and recurrence assessment of bone sarcoma. Medicine (Baltimore) [Internet]. 2015 11 [cited 2016 Nov 30];94(36). Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4616630/
Tian R, Su M, Tian Y, Li F, Li L, Kuang A, et al. Dual-time point PET/CT with F-18 FDG for the differentiation of malignant and benign bone lesions. Skelet Radiol. 2009;38(5):451–8.
Sheikhbahaei S, Marcus C, Hafezi-Nejad N, Taghipour M, Subramaniam RM. Value of FDG PET/CT in patient management and outcome of skeletal and soft tissue sarcomas. PET Clin. 2015;10(3):375–93.
Kinahan PE, Fletcher JW. Positron emission tomography-computed tomography standardized uptake values in clinical practice and assessing response to therapy. Semin Ultrasound CT MR. 2010;31(6):496–505.
Andersen KF, Fuglo HM, Rasmussen SH, Petersen MM, Loft A. Volume-based F-18 FDG PET/CT imaging markers provide supplemental prognostic information to histologic grading in patients with high-grade bone or soft tissue sarcoma. Medicine (Baltimore). 2015;94(51):e2319.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Subhawong, T.K., Winn, A., Shemesh, S.S. et al. F-18 FDG PET differentiation of benign from malignant chondroid neoplasms: a systematic review of the literature. Skeletal Radiol 46, 1233–1239 (2017). https://doi.org/10.1007/s00256-017-2685-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-017-2685-7