Abstract
Abusive head trauma (AHT) is the leading cause of fatal head injuries in children younger than 2 years. An intracranial pathology can exist even in the setting of a normal physical exam. A delay in the diagnosis of AHT can have serious life-threatening consequences for the child and increases the potential the child will be abused again. In this article, we review the traumatic subdural hematoma as well as various morpho-structural patterns of shearing injuries and thrombosis of intracranial bridging veins. This work serves as a summary of patterns of imaging features of intracranial venous injury in AHT, as described in the literature, to facilitate familiarity and early detection of abusive head trauma in the pediatric population. Essentially, in AHT there is a traumatic injury to the bridging vein with either partial or complete tear. This can secondarily result in thrombosis at the terminal end of the bridging vein with blood clots adjacent to the bridging vein.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Abusive head trauma (AHT) is the leading cause of fatal head injuries in the pediatric population younger than 2 years [1]. Overall, about 53% of serious or fatal traumatic brain injuries in children younger than 2 years can be attributed to AHT [1]. Additionally, no single injury is diagnostic for AHT, but it is considered when there is discordance among clinical evaluation findings, imaging findings and the clinical history provided with regard to the mechanism of trauma [2]. Just as the mechanism of injury is multifactorial, the pathophysiology ranges from traumatic neuronal injury, to hypoxic–ischemic or metabolic neuronal injury, to tearing of bridging cortical veins, as we further discuss in this review [3].
A delay in the diagnosis or a missed diagnosis of AHT can have serious life-threatening consequences on the child, not just in the acute setting but in terms of repeated maltreatment in the future. Moreover, the abused child might not have physical signs of abuse [4, 5], and intracranial pathology can exist in the setting of a normal physical exam or lack of retinal hemorrhage [5]. Origin of subdural hematoma (SDH) is a frequently contested topic during medicolegal assessment of AHT. Non-traumatic etiologies for SDH are frequently cited during legal proceedings, to dispute the traumatic nature of AHT [1]. For this reason, one needs to be intimately familiar with imaging features of intracranial venous injury. In this review, we discuss various intracranial venous injury patterns and relevant imaging features.
Subdural hematoma
Subdural hematoma is considered a cardinal injury and is a commonly identified imaging abnormality in AHT [1, 6]. Intracranial SDH is seen in up to 90% of children with AHT [7]. The imaging finding of SDH alone is only moderately specific because it is common in AHT, accidental head trauma and non-traumatic conditions. The specificity of this finding is increased in the setting of relevant history and underlying diffuse parenchymal injury, as articulated by a systematic review in 2011 [8].
Pathophysiology
Traumatic SDH, which includes AHT, has long been believed to be caused by the rupture of bridging veins [9]. Recent imaging data suggest that evidence of bridging vein injury is seen in 40–45% of children with AHT and SDH [2, 10]. It is therefore important to note that when there is a positive finding of rupture of bridging veins, it supports a traumatic cause (although not AHT specifically) of SDH [11, 12]. Current data support the formation of SDHs from tearing of one or more of the 15–20 cortical bridging veins. These veins traverse the cerebral cortex to pia mater to subarachnoid space to the venous sinuses inside the dura mater [13, 14]. It is also noteworthy that the vessel segments that penetrate the dural border cell layer are thinner (10 μm) than those of the subarachnoid portion (50–200 μm), resulting in increased fragility [13].
Imaging
The appearance of intracranial SDH is variable on both CT and MRI. Mixed-density SDHs on CT or mixed-signal-intensity SDHs on MRI are commonly identified during initial presentation [15]. Unclotted blood is isodense when compared to the cerebral cortex and might represent bleeding within the first 3 h after trauma [16, 17]. Additionally, it is relevant to note that the bleed might be isodense to the cortex in children with delayed clotting from coagulopathy. Other conditions such as hemato-hygroma associated with a meningeal tear can also present as isodense or hypodense SDH collections because of an admixture of cerebrospinal fluid (CSF) [18,19,20] and blood. Acute hemorrhage on CT can be iso- or hypoattenuating in the setting of anemia (hemoglobin <8–10 g/dL) [17]. Therefore, in these conditions and in those with small volume, imaging with MRI might be more beneficial [21,22,23]. Dating SDH by the appearance of the hemorrhage alone has been shown to be inaccurate [24]. These findings should be combined with clinical history, examination and other imaging findings to offer a better estimate of the timing of the injury.
Bridging vein thrombosis
Pathophysiology
We discussed that bridging vein rupture is identified as the primary mechanism in the formation of SDH. Visualization of terminal bridging vein thrombosis is considered a significant indicator of a traumatic nature of head injury in the context of AHT [10]. Occasional reports have described the anatomy and traumatology of bridging vein thrombosis in autopsy studies [14, 24,25,26,27,28,29,30,31,32]. However, it has also been noted that the standard autopsy procedure itself can cause artificial postmortem bridging vein thrombosis findings [27].
Imaging
The vertex should be carefully surveyed in all children with suspected AHT for evidence of bridging vein injury (Figs. 1, 2, 3, 4, 5 and 6). Typically, the injured terminal end of a bridging vein appears hyperdense as compared to the cerebral cortex on CT [6]. A gold standard for radiologic imaging for bridging vein injury does not exist, nor do systematic studies investigating the morphology of bridging vein thrombosis [10]. In 1999, bridging vein thrombosis was described using T2-weighted gradient-echo (GRE) in 4 of 14 children with AHT and SDH [33]. More recently, terminal bridging vein thrombosis associated with hypodense SDH was demonstrated in three cases on CT and MRI [11]. Subsequently, terminal bridging vein thrombosis was demonstrated on heme-sensitive susceptibility-weighted imaging (SWI) sequence on MRI in children with AHT-associated SDH [34]. Seven imaging patterns of venous injuries using neuroimaging have been described in AHT, discussed next.
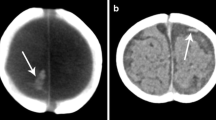
Tadpole or lollipop sign in a 5-month-old boy with abusive head trauma. a Axial non-contrast head CT shows a hyperdense bridging vein (arrow) in the left paramedian plane anterior to the frontal lobe. Bilateral large mixed-density subdural hemorrhages (SDHs) are also evident. b Coronal non-contrast CT head demonstrates the bridging vein (arrow) terminating in a large blood clot (arrowhead), with terminal thrombosis giving it the typical appearance of a lollipop sign or tadpole sign (outline). Bilateral large mixed-density SDHs are also evident. c Sagittal T1-W MRI demonstrates the terminally thrombosed bridging vein (arrow) terminating in a large blood clot (arrowhead). d Coronal T2-W MRI demonstrates the terminally thrombosed bridging vein (arrow) terminating in a large blood clot (arrowhead)
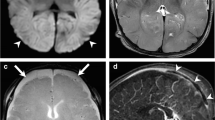
Negative lollipop sign in a 4-month-old boy with abusive head trauma. a Axial non-contrast CT of the head demonstrates bilateral large hypodense subdural hemorrhages (SDHs) with a hyperdense component (measuring 0.47 cm) overlying the right frontal lobe. b Axial fluid-attenuated inversion recovery MRI demonstrates acute injury of a bridging vein (arrow) in this region, with active extravasation and a large blood clot (arrowhead). c Axial T2-W MRI demonstrates acute injury of a bridging vein (arrow) in this region, with active extravasation and a large blood clot (arrowhead). d Axial T2-W MRI above the level of cerebral hemispheres demonstrate a cross-section of multiple bridging veins surrounded by bilateral large SDHs. The left anterior bridging vein (long arrow) is irregular in shape, reflecting injury. A relatively normal appearing bridging vein is on the right side (short arrow). e Axial susceptibility-weighted imaging (SWI) MRI above the level of cerebral hemispheres demonstrates a cross-section of multiple bridging veins surrounded by bilateral large SDHs. The left anterior bridging vein (long arrow) is irregular in shape, reflecting injury. Blooming is also noted along these bridging veins, representing evidence of thrombosis (long arrow and short arrow). f Coronal non-contrast CT head at the level of foramen of Monro demonstrates a hyperdense irregular-shape bridging vein in the left parasagittal region (arrow). g Coronal T2-W MRI confirms an irregular-shape bridging vein (arrow) in this region with bilateral large hyperintense SDHs. h Coronal SWI MRI shows the irregular-shape bridging vein with blooming in the same region (arrow). This is consistent with venous wall injury resulting in distortion with secondary thrombosis. i Coronal T2-W MRI at the level of occipital lobe demonstrates a bridging vein (arrow) traversing the SDH to drain into the superior sagittal sinus. Mild enlargement of the bridging vein is noted within the SDH. This is the negative lollipop sign. j, k Sequential images from coronal SWI MRI at the corresponding level of the occipital lobe demonstrate the complete course of an intact bridging vein. This demonstrates irregularity of the mid-section of the bridging vein with blooming artifact (arrow) and likely represents partial injury or perforation of the bridging vein
Abusive head trauma in a 5-month-old boy. a Sagittal balanced fast field echo (bFFE) MRI demonstrates multiple intact bridging veins (arrows) coursing through the subarachnoid space and a large hyperintense subdural hemorrhage (SDH) draining into the superior sagittal sinus. Note the tethering of the dura at the point of entrance of bridging veins to the subdural space. b Axial T2-W MRI demonstrates multiple bridging veins (arrows) coursing through the large hyperintense SDH. c Axial susceptibility-weighted MRI demonstrates blooming of the bridging veins (arrow and arrowhead), consistent with the evidence of thrombosis (lollipop sign; arrow), coursing through the large hyperintense SDH. d Coronal T2-W MRI demonstrates irregularity along the mid-portion of a bridging vein (arrow), representing evidence of vascular wall injury. Bilateral large hyperintense SDHs are again evident. e Coronal bFFE MRI demonstrates irregularity along the mid-portion of a bridging vein (arrow), representing evidence of vascular wall injury. Bilateral large hyperintense SDHs are again evident
Normal findings in a 3-month-old boy with no history of trauma. High-resolution coronal susceptibility-weighted MR image of a normal sub-millimetric bridging vein shows smooth vessel walls (superior wall, solid arrows; inferior wall, arrowhead). Vein caliber is preserved and the internal flow void appears normal. The superior sagittal sinus is also identified, and within normal limits (dotted arrow)
Interrupted bridging vein in a 3-month-old girl with abusive head trauma. High-resolution coronal susceptibility-weighted imaging identifies a bridging vein at the left convexity with luminal narrowing and without definite obstruction, and at least two focal areas of interruption of the vascular wall (arrows)
Tadpole sign.
Hahnemann et al. [10] compared the CT and MR appearance of bridging vein thrombosis to that of a tadpole. This finding was prevalent in >70% of cases [10]. The body of the tadpole is represented by the oval- to round-shape thrombotic material within the subarachnoid space; the bent tail of the tadpole is represented by the torn bridging vein expanded by the clotted blood (Fig. 1). However, in a subsequent review, only 36% of cases with tadpole sign, as noted on axial SWI, represented bridging vein thrombosis on high-resolution coronal SWI MRI sequence [35].
Simple tubular shape.
In the same study by Hahnemann et al. [10], there was a simple tubular shape of bridging vein thrombosis on MR in three children. This tubular shape does not have the body of the tadpole, only the torn bridging vein expanded by the clotted blood (tubular shape). It is important to note that the presence of these signs should compel the radiologist to search for other signs of AHT such as retinal hemorrhages or fractures [10].
Lollipop sign.
Choudhary et al. [2] described the lollipop sign on MR (particularly GRE), where the parasagittal bridging vein abruptly terminates into a subarachnoid blood clot and does not drain into the venous sinus. The head of the lollipop is the subarachnoid blood clot and the stick is the bridging vein with terminal thrombosis (Fig. 1) [2]. These bridging veins terminate abruptly and do not drain into the superior sagittal sinus. It is also hypothesized that the abrupt termination represents a bridging vein tear and subsequent bridging vein thrombosis at the torn end [2].
Negative lollipop sign.
The bridging vein traverses the subarachnoid blood clot and the subdural hemorrhage and drains into the sinus (Fig. 2) [2]. This might represent a partial tear of the bridging vein without complete disruption or no injury to the traversing bridging vein, but with associated blood clot from adjacent bridging vein injury.
Positive compression sign.
This is described when a cortical vein or sinus abruptly narrows or terminates without any obvious associated intraluminal blood clot (Fig. 7) [2]. Displacement of the veins and sinuses might also be identified. These features can mimic long-segment widespread thrombosis if the images are not carefully evaluated by an experienced pediatric neuroradiologists [2].
Compression sign in different children. This is best identified on three-dimensional (3-D) reconstructed magnetic resonance (MR) venography images. a In a 4-month-old boy with abusive head trauma, 3-D reconstructed MR venography, sagittal view, demonstrates abrupt cutoff of the anterior aspect of the superior sagittal sinus (arrow). There is also a relative paucity of superficial cortical veins bilaterally. b, c In a 3-month-old boy with AHT, 3-D reconstructed MR venography, sagittal view (b) demonstrates abrupt cutoff of the anterior aspect of the superior sagittal sinus (arrow in b). The 3-D reconstructed MR venography posterior view (c) demonstrates an asymmetrical paucity of superficial cortical veins on the right side (arrow). d In a 2-month-old girl with abusive head trauma, 3-D reconstructed MR venography, superior view, demonstrates abrupt change of caliber (arrowhead) along the mid superior sagittal sinus, with stenosis anteriorly (arrow). There is a relative paucity of superficial cortical veins bilaterally. These features of paucity/absence of cortical veins and stenosis of sinuses represent mass effect from subdural hemorrhage or brain swelling. These imaging features should not be misconstrued as evidence of thrombosis and should be correlated with other MRI sequences
Venous thrombosis secondary to trauma.
Venous thrombosis can be seen post trauma and it is important to distinguish between primary versus secondary thrombosis, particularly in the context of AHT. Choudhary et al. [2] described this finding in a 3-month old boy with secondary thrombosis of the left vein of Labbé. This was seen in the setting of bilateral supratentorial and infratentorial SDHs along with evidence of multiple other injuries, which would be most consistent with a secondary thrombosis of the vein of Labbé [2]. Additionally, isolated cortical vein thrombosis has been described in only 6% of venous thrombosis cases [36]. It is also noteworthy that there is significant discordance in interobserver agreement in identifying isolated cortical vein thrombosis using MR venography, which might influence the actual number of cases identified [37].
Rupture of the bridging vein.
This finding has been described by Zuccoli et al. [35], who used high-resolution coronal SWI. High-resolution SWI can help in identifying the walls of the sub-millimetric bridging veins as they enter the superior sagittal sinus at the convexity. The bridging veins are better visualized on coronal imaging because on this plane their longest (longitudinal) axis is vertically oriented to the longitudinal axis of the superior sagittal sinus (Fig. 4). The ruptured bridging vein might present with a focal interruption (Fig. 5) or extensive morphological changes resulting from the combination of multiple shearing forces (Dr. Guilio Zuccoli, personal communication) (Fig. 6). The presence of a clot (bridging vein thrombosis) cannot be distinguished from slow flow on SWI because both appear dark. However, high-resolution coronal SWI can be used as a tool to demonstrate traumatic injury to the bridging veins rather than thrombosis because the latter represents the end-stage phenomenon of the shearing injury applied to abused children during shaking [11, 35].
Essentially, these various patterns demonstrate a common theme of traumatic injury to the bridging vein with either partial or complete tear. This can secondarily result in thrombosis at the terminal end of the bridging vein. Blood clot can also be seen around the torn bridging vein in the subarachnoid or subdural space.
Imaging of the intracranial venous anatomy can be done using a variety of advanced techniques including CT and MR venography, formal angiography, and digital subtraction angiography [2]. MR imaging has been most frequently used because of its noninvasive nature and lack of radiation exposure to the child. The venous anatomy should be carefully examined on all the sequences, particularly on the SWI sequence. Post-contrast 3-D magnetization-prepared rapid gradient echo imaging (MP-RAGE) has also been found to be useful when used either as a routine or an additional sequence in challenging cases [38]. Some inherent limitations of MR include artifacts and anatomical variations in venous anatomy in this patient population [2].
Conclusion
This is a descriptive review of the neuroimaging patterns of venous injury in AHT. Demonstrating morpho-structural alterations to the bridging veins in AHT adds an important piece of information to the multidisciplinary diagnosis of AHT by proving the traumatic nature of intracranial subdural hematomas.
References
Choudhary AK, Servaes S, Slovis TL et al (2018) Consensus statement on abusive head trauma in infants and young children. Pediatr Radiol 48:1048–1065
Choudhary AK, Bradford R, Dias MS et al (2015) Venous injury in abusive head trauma. Pediatr Radiol 45:1803–1813
Christian CW, Block R, Jenny C et al (2009) Abusive head trauma in infants and children. Pediatrics 123:1409–1411
Pfeifer CM, Hammer MR, Mangona KL, Booth TN (2017) Non-accidental trauma: the role of radiology. Emerg Radiol 24:207–213
Rubin DM, Christian CW, Bilaniuk LT et al (2003) Occult head injury in high-risk abused children. Pediatrics 111:1382–1386
Wright JN (2017) CNS injuries in abusive head trauma. AJR Am J Roentgenol 208:991–1001
Fanconi M, Lips U (2010) Shaken baby syndrome in Switzerland: results of a prospective follow-up study, 2002-2007. Eur J Pediatr 169:1023–1028
Kemp A, Jaspan T, Griffiths J et al (2011) Neuroimaging: what neuroradiological features distinguish abusive from non-abusive head trauma? A systematic review. Arch Dis Child 96:1103–1112
Miller JD, Nader R (2014) Acute subdural hematoma from bridging vein rupture: a potential mechanism for growth: clinical article. J Neurosurg 120:1378–1384
Hahnemann ML, Kinner S, Schweiger B et al (2015) Imaging of bridging vein thrombosis in infants with abusive head trauma: the “tadpole sign”. Eur Radiol 25:299–305
Adamsbaum C, Rambaud C (2012) Abusive head trauma: don’t overlook bridging vein thrombosis. Pediatr Radiol 42:1298–1300
Rambaud C (2015) Bridging veins and autopsy findings in abusive head trauma. Pediatr Radiol 45:1126–1131
Yamashima T, Friede RL (1984) Why do bridging veins rupture into the virtual subdural space? J Neurol Neurosurg Psychiatry 47:121–127
Nierenberger M, Wolfram-Gabel R, Decock-Catrin S et al (2013) Investigation of the human bridging veins structure using optical microscopy. Surg Radiol Anat 35:331–337
Bradford R, Choudhary AK, Dias MS (2013) Serial neuroimaging in infants with abusive head trauma: timing abusive injuries — clinical article. J Neurosurg Pediatr 12:110–119
Hedlund GL (2012) Subdural hemorrhage in abusive head trauma: imaging challenges and controversies. J Am Osteopat Coll Radiol 1:23–30
Vezina G (2009) Assessment of the nature and age of subdural collections in nonaccidental head injury with CT and MRI. Pediatr Radiol 39:586–590
Joy HM, Anscombe AM, Gawne-Cain ML (2007) Blood-stained, acute subdural hygroma mimicking a subacute subdural haematoma in non-accidental head injury. Clin Radiol 62:703–706
Offiah C, Forbes WSC, Thorne J (2006) Non-haemorrhagic subdural collection complicating rupture of a middle cranial fossa arachnoid cyst. Br J Radiol 79:79–82
Wittschieber D, Karger B, Niederstadt T et al (2015) Subdural hygromas in abusive head trauma: pathogenesis, diagnosis, and forensic implications. AJNR Am J Neuroradiol 36:432–439
Vázquez E, Delgado I, Sánchez-Montañez A et al (2014) Imaging abusive head trauma: why use both computed tomography and magnetic resonance imaging? Pediatr Radiol 44:S589–S603
Datta S, Stoodley N, Jayawant S et al (2005) Neuroradiological aspects of subdural haemorrhages. Arch Dis Child 90:947–951
Kemp AM, Rajaram S, Mann M et al (2009) What neuroimaging should be performed in children in whom inflicted brain injury (iBI) is suspected? A systematic review. Clin Radiol 64:473–483
Sieswerda-Hoogendoorn T, Postema FAM, Verbaan D et al (2014) Age determination of subdural hematomas with CT and MRI: a systematic review. Eur J Radiol 83:1257–1268
Norman MG, Smialek JE, Newman DE, Horembala EJ (1984) The postmortem examination on the abused child. Pathological, radiographic, and legal aspects. Perspect Pediatr Pathol 8:313–343
Maxeiner H (1997) Detection of ruptured cerebral bridging veins at autopsy. Forensic Sci Int 89:103–110
Maxeiner H (2001) Demonstration and interpretation of bridging vein ruptures in cases of infantile subdural bleedings. J Forensic Sci 46:85–93
Ehrlich E, Maxeiner H, Lange J (2003) Postmortem radiological investigation of bridging vein ruptures. Legal Med 5:225–227
Stein KM, Ruf K, Ganten MK, Mattern R (2006) Representation of cerebral bridging veins in infants by postmortem computed tomography. Forensic Sci Int 163:93–101
Depreitere B, Van Lierde C, Vander Sloten J et al (2006) Mechanics of acute subdural hematomas resulting from bridging vein rupture. J Neurosurg 104:950–956
Han H, Tao W, Zhang M (2007) The dural entrance of cerebral bridging veins into the superior sagittal sinus: an anatomical comparison between cadavers and digital subtraction angiography. Neuroradiology 49:169–175
Monea AG, Baeck K, Verbeken E et al (2014) The biomechanical behaviour of the bridging vein–superior sagittal sinus complex with implications for the mechanopathology of acute subdural haematoma. J Mech Behav Biomed Mater 32:155–165
Barlow KM, Gibson RJ, McPhillips M, Minns RA (1999) Magnetic resonance imaging in acute non-accidental head injury. Acta Paediatr 88:734–740
Yilmaz U, Körner H, Meyer S, Reith W (2015) Multifocal signal loss at bridging veins on susceptibility-weighted imaging in abusive head trauma. Clin Neuroradiol 25:181–185
Zuccoli G, Khan AS, Panigrahy A, Tamber MS (2017) In vivo demonstration of traumatic rupture of the bridging veins in abusive head trauma. Pediatr Neurol 72:31–35
Leach JL, Fortuna RB, Jones BV, Gaskill-Shipley MF (2006) Imaging of cerebral venous thrombosis: current techniques, spectrum of findings, and diagnostic pitfalls. Radiographics 26:S19–S41
Ferro JM, Morgado C, Sousa R, Canhão P (2007) Interobserver agreement in the magnetic resonance location of cerebral vein and dural sinus thrombosis. Eur J Neurol 14:353–356
Klingebiel R, Bauknecht HC, Bohner G et al (2007) Comparative evaluation of 2D time-of-flight and 3D elliptic centric contrast-enhanced MR venography in patients with presumptive cerebral venous and sinus thrombosis. Eur J Neurol 14:139–143
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vilanilam, G.K., Jayappa, S., Desai, S. et al. Venous injury in pediatric abusive head trauma: a pictorial review. Pediatr Radiol 51, 918–926 (2021). https://doi.org/10.1007/s00247-021-05016-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-021-05016-9