Abstract
Purpose
The purpose of this study was to investigate changes in utilisation of antiepileptic drugs (AEDs) in epilepsy and non-epilepsy disorders in Norway and furthermore to study the retention rates of the most commonly used AEDs in these indications in long-term use.
Methods
The data consisted of all prescriptions of AEDs from Norwegian pharmacies in the Norwegian Prescription Database (NorPD) (2004–2012). Variables included anonymous data regarding age, gender, diagnosis specific reimbursement codes and utilisation of AEDs.
Results
In recent years (2008–2012), the utilisation of AEDs in non-epilepsy disorders accounted for 45–53 % of the total use. In epilepsy, the most commonly used AED was lamotrigine, followed by levetiracetam, carbamazepine and valproate. Lamotrigine was also the predominant AED used in psychiatry, while pregabalin and gabapentin were mostly used in neuropathic pain. In migraine, topiramate predominated but accounted for <1 % of the total utilisation of AEDs. The majority of prescriptions were by general practitioners and only 20 % by specialists. Regardless of indication, newer AEDs had higher retention rates (34–48 %) and were used for a longer period before discontinuation.
Conclusions
The use of AEDs in non-epilepsy disorders is increasing and accounted for 53 % in 2012. Newer AEDs were predominantly used and demonstrated higher retention rates than older AEDs in all indications. This nationwide study demonstrates an increased exposure to AEDs in new patient groups, and details in prescription patterns and clinical and safety considerations should be closely monitored. This contributes to long-term post-marketing data of AED and accordingly improved pharmacovigilance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Antiepileptic drugs (AEDs), and especially the newer drugs, are increasingly used in non-epilepsy indications, as in psychiatric disorders, neuropathic pain and migraine [1–6]. New patient groups are therefore exposed to AEDs. AEDs have different mechanisms of action and considerable inter-individual pharmacokinetic variability and are susceptible to cause adverse effects and drug interactions [7, 8]. Careful investigations of AED utilisation in large patient populations in the clinical setting are thus of importance.
Prescription databases may be used to study specific patient populations as children, women of childbearing age and the elderly, prescription patterns and specific drugs to improve our understanding of changes in treatment patterns over time. Such pharmacoepidemiological studies are now more commonly utilised and show a new trend in clinical pharmacology to assess drug utilisation in a clinical population setting [9–13]. This is relevant and important for policy makers (prescribers, pharmacists and health authorities), regarding follow-up of changes in prescription patterns and as an incentive for updating treatment guidelines. Rapid changes have been observed regarding the use of newer AEDs both in epilepsy and non-epilepsy disorders from 2004 [3, 4]. From 2008, reimbursement codes for diagnoses specifically based on the International Statistical Classification of Diseases and Related Health Problems (ICD-10) or the International Classification for Primary Care (ICPC-2) system were implemented into the Norwegian Prescription Database (NorPD). With this methodological improvement, a detailed study was performed with regards to further changes in the use of AEDs in epilepsy and non-epilepsy indications, i.e. psychiatric disorders, neuropathic pain and migraine from 2008 to 2012. Furthermore, long-term changes in utilisation and retention rates from 2004 to 2012 could be studied as a measure of effectiveness (efficacy and tolerability).
The purpose of the present study was to investigate changes in utilisation of AEDs in Norway and furthermore to study the retention rates of the most commonly used AEDs in epilepsy and non-epilepsy disorders (psychiatry, neuropathic pain and migraine).
Methods
Study material from the Norwegian Prescription Database
Data from January 2004 to December 2012 were obtained from NorPD upon request. This database includes pharmacy records based on dispensed and collected prescriptions from all Norwegian pharmacies from 01 January 2004. The database is run by the Norwegian Institute of Public Health and is described and evaluated in previous studies [3, 4, 14–16]. The data in this study contained all prescriptions (from specialists and general practitioners) to patients who received at least one AED during the period 01 January 2008 to 31 December 2012 for any indication to study the use of AEDs in epilepsy vs. non-epilepsy indication using diagnosis-specific reimbursement codes. Furthermore, long-term changes in utilisation and retention rates of most commonly used AEDs in each indication could be studied in detail from 2004 to 2012.
Variables included gender, age groups, encrypted person identifiers instead of identity (ID), defined daily doses (DDDs), prescription category (public refund or not refund) and the specific code for reimbursement or indication. Specific diagnosis-specific reimbursement codes following the classification system for ICD-10 and ICPC-2 were used [17, 18]. Classification of drugs was based upon the Anatomical Therapeutic Chemical (ATC) classification codes where AEDs are defined as N03A. Population of Norway from 2008 to 2012 (as of 01 January) was supplied by Statistics Norway as shown in Table 1 [19].
The study was approved by the Norwegian Institute of Public Health. The ethical considerations included that the data were anonymous with no patient identification, as each patient was given a running number in the data file (pseudonymous), and Statistics Norway provided security for protection of patient information.
Data analyses and calculations
The data were analysed using Structured Query Language (SQL) in a database administration system (mySQL). Kaplan–Meier analyses were carried out using IBM SPSS Statistics 18. For further analysis of the use in non-epilepsy indications, patients using AEDs with the reimbursement code or indication for epilepsy were excluded. The remaining indications were psychiatric disorders, neuropathic pain, migraine prophylaxis or other, as specified in Table 1. The estimate of the use of AEDs in neuropathic pain was based upon reimbursement and self-payment prescriptions (only pregabalin and gabapentin) [20, 21].
The utilisation of AEDs is presented as DDDs/1000 inhabitants/day. For the DDD measure, statistical measures for variability will be too uncertain, due to variability in the consumption of drugs (use of other doses than the DDD, polytherapy, periodic use of drugs, etc.). Time to discontinuation was analysed by the Kaplan–Meier method. A period of 9 years (3285 days, 2004–2012) was used to estimate the retention rates for the most commonly used AEDs in each indication based on findings from the first results from the database: lamotrigine, levetiracetam, carbamazepine and valproate in epilepsy; lamotrigine, carbamazepine, pregabalin and valproate in psychiatric disorders and topiramate, valproate and gabapentin in migraine. Due to introduction of diagnosis-specific reimbursement codes in 2008, the analysis of retention rates for gabapentin, pregabalin and carbamazepine in neuropathic pain was for 5 years (1825 days, 2008–2012). Retention rates (proportion of patients remaining on treatment) may indicate the long-term tolerability and efficacy of the particular drug.
Results
The present study covers the whole population of Norway and reflects detailed information of the prescription patterns of AEDs and the utilisation of AEDs in non-epilepsy disorders, from 2004 to 2012.
Patient characteristics of the population
The age range of the patients included all age groups (per 10 years) from 0 up to 103 years. The gender distribution for all age groups was 50/50 women/men in epilepsy, 58/42 women/men in psychiatry, 59/41 in neuropathic pain and 71/29 in migraine. Six percent of the patients using AEDs in epilepsy were in the age group 0–19 years, and only 0.1 to 0.3 % of the users of AEDs for non-epilepsy disorders were in this age group. Forty-eight percent of the patients using AEDs in non-epilepsy disorders were in the age group 20 to 60 years, and 49 % were older than 60 years (Fig. 1).
Utilisation of AEDs in epilepsy
Over the years, both the number of patients and the utilisation of AEDs in epilepsy have been constant with an average of 40,662 distinctive patients and 6.7 DDD/1000 inhabitants/day (Table 1 and Fig. 2a). The total utilisation of AEDs in epilepsy accounted for 55 to 47 % of the total use of AEDs in 2008 and 2012, respectively. In 2008 to 2012, lamotrigine was the most commonly used AED in epilepsy (1.4–1.5 DDDs/1000 inhabitants/day), followed by levetiracetam (0.7–1.1 DDD/1000 inhabitants/day), carbamazepine (1.0–1.4 DDD/1000 inhabitants/day) and valproate (0.98–1.0 DDD/1000 inhabitants/day) (Fig. 2b). The gender distribution of the users of lamotrigine and valproate was on average 55/45 and 43/57 women/men, respectively. The number of women using valproate in epilepsy has declined with 26 % from 2008 to 2012.
Utilisation of antiepileptic drugs in epilepsy and non-epilepsy disorders in Norway. Total use of AEDs in various indications, 2004–2012 (a). Utilisation of the most common AEDs in epilepsy (b), in psychiatric indications (c), in neuropathic pain (d) and in migraine (e), 2008–2012. DDDs defined daily doses
Increased utilisation of AEDs in non-epilepsy disorders
In total, the prevalence of use of AEDs in non-epilepsy disorders has increased by 35 % from 2008 to 2012, reflected by a similar increase in both psychiatry and neuropathic pain (Fig. 2a). The utilisation of AEDs in non-epilepsy disorders accounted for 45 to 53 % of the total use of AEDs in 2008 to 2012.
Psychiatry
In psychiatry, the increase in the utilisation of AEDs in DDDs/1000 inhabitants/day was 39 % from 2008 to 2012 and accounted for 16 to 20 % of the total use of AEDs (Fig. 2a). The increased utilisation exceeded the increase in prevalence of users. Lamotrigine was the major drug used in psychiatry, constituting 67 to 73 % of the total use of the drug from 2008 to 2012 regardless of psychiatric disorder from 2008 to 2012, which was 1.4 and 2.1 DDDs/1000 inhabitants/day, respectively. Valproate, carbamazepine and pregabalin were minor AEDs prescribed in psychiatry, all accounting for 27 to 32 % of the total use of AEDs, and increased by 20 % from 2008 to 2012 (Fig. 2c). The gender distribution of users of lamotrigine in psychiatry was 63/37 women/men and 50/50 for valproate. The utilisation of AEDs in psychiatric disorders in children (aged less than 10 years) and adolescents (11–19 years) constituted 2 and 442 individuals, respectively. The use accounted for <0.001 and 0.003 DDDs/1000 inhabitants/day, respectively, and represented 0.01 % of the utilisation of AEDs in psychiatry per year from 2008 to 2012.
Neuropathic pain and migraine
The use of AEDs in pain, and mainly neuropathic pain, increased by 40 % from 2008 to 2012 and consisted of 30 % of the total use of AEDs in 2012 (Fig. 2a). The number of patients using AEDs in neuropathic pain has increased by nearly 100 % from 28,444 patients in 2008 to 59,980 patients in 2012 (Table 1). Pregabalin and gabapentin were the main drugs (>93 %) utilised in neuropathic pain and accounted for 2.8 to 4.1 DDDs/1000 inhabitants/day (Fig. 2d). The use of carbamazepine in neuropathic pain was minor, on average 5.5 % of the total use in this indication. Migraine prophylaxis is a minor indication for AEDs, where the predominant drug is topiramate, followed by minor use of valproate and gabapentin. Migraine constituted less than 1 % in total of the use in non-epilepsy indications. The utilisation of topiramate in migraine consisted on average of 0.01 DDDs/1000 inhabitants/day from 2008 to 2012), constituting 83–95 % of the use of AEDs in migraine. Valproate and gabapentin were minor AEDs prescribed in migraine and accounted for only 3.9–15 % of the use (Fig. 2e). The gender distribution of valproate users was on average 73/27 women/men in migraine.
Other and unspecified indications
The percentage of use of AEDs in other, unspecified disorders and especially as off-label use in psychiatry was constant at 3.6 to 5 % of the total consumption of AEDs and accounted for 0.67 to 0.51 DDDs/1000 inhabitants/day from 2008 to 2012, respectively. The use of AEDs without reimbursement or any stated indications included for instance clonazepam, 0.43 DDDs/1000 inhabitants/day. During 2008 to 2012, a number of codes and indications that were used exceeded by large the limited number of main indications given in reimbursement, as stated in this category: 45 different reimbursement codes, 43 ICD-10 codes and 50 ICPC-2 codes, with only a limited number of patients within each category.
Prescription patterns
Due to changes in prescription patterns in Norway in 2008, the average for the years 2009 to 2012 are used to elucidate the prescription patterns. The prescription of AEDs from specialists (ICD-10) was considerably lower than the prescription from general practitioners (ICPC-2). On average, 20 % of the prescriptions in epilepsy, psychiatry and migraine were prescribed by specialists and 15 % in neuropathic pain. No major changes in specialist/general practitioner ratios in prescriptions were seen from 2009 to 2012. The prescriptions with old reimbursement codes accounted for <5 % after the introduction of diagnosis-specific reimbursement codes.
Retention rates for the most commonly used AEDs
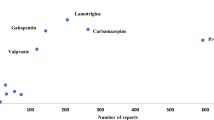
Based on the findings of the most commonly used AEDs in Norway in all indications, survival plots were based upon comparative Kaplan–Meier statistics for comparison between AEDs in different indications. Regardless of indication, newer AEDs have better effectiveness. The mean numbers of days to discontinuation of the most commonly used AEDs are shown in Table 2. The retention rate at year 9 in epilepsy was 48 % for levetiracetam (Fig. 3a). In psychiatric disorders, lamotrigine had a retention rate of 37 % and carbamazepine had a significantly poorer outcome than the other AEDs had. Pregabalin, used predominantly in anxiety, had the highest retention rate of 47 % but was used in a low number of patients (Fig. 3b). At day 1825, pregabalin and gabapentin had retention rates of 36 and 35 %, respectively, in neuropathic pain, and 33 % for carbamazepine (Fig. 3c). In migraine, the prescription numbers were small, but topiramate and valproate had the highest retention rates of 37 and 36 %, respectively (Fig. 3d).
Retention rates of the most commonly used antiepileptic drugs (AEDs) in epilepsy and non-epilepsy indications at 9 years (3285 days) and 5 years (1825 days) for neuropathic pain. The y-axis (survival probability) shows the number of patients, and the x-axis represents time (days). Censored values are indicated by crosses. Carbamazepine (N03AF01), valproate (N03AG01), lamotrigine (N03AX09), levetiracetam (N03AX14), pregabalin (N03AX12), gabapentin (N03AX16), topiramate (N03AX11). ATCcode Anatomical Therapeutic Chemical classification
Discussion
The present study covers the whole population of Norway and reflects detailed information of the increased utilisation of AEDs in non-epilepsy indications, i.e. psychiatry, neuropathic pain and migraine in various patient groups, as a follow-up of changes based on previous studies [3, 4].
Changes in utilisation of AEDs in epilepsy and non-epilepsy, various indications and clinical implications
The present results demonstrate a shift in recent years towards more extensive utilisation of AEDs in non-epilepsy disorders as compared to our results from 2004 to 2007 [3]. A similar increase in other disorders has been shown in e.g. Denmark and Italy using different methodologies during the 1990s to the 2000s [1, 2, 5, 6].
Epilepsy
The utilisation of lamotrigine and valproate has been constant, while the utilisation of carbamazepine has declined as the use of e.g. levetiracetam has increased. The top four most frequently prescribed AEDs in epilepsy are in line with the evidence-based recommendations from the International League Against Epilepsy (ILAE). Carbamazepine, levetiracetam and lamotrigine (in the elderly) are among the AEDs with the highest evidence-based recommendations and are first choices in focal onset seizures in adults. Valproate, carbamazepine and lamotrigine are regarded as first choices (evidence level C) in generalised onset seizures in adultswhile valproate is of choice (evidence level A) in absence seizures in children [22].
Psychiatry
The utilisation of lamotrigine has increased in psychiatric disorders each year since 2004 [3]. Patients with epilepsy often suffer from comorbid conditions, and lamotrigine is in many cases chosen, pointing to rational therapy [23]. Lamotrigine is regarded as a first-line treatment option in bipolar depression in adults, according to recent evidence-based guidelines [24–26]. Pregabalin in generalised anxiety disorder constitutes only limited use. Off-label use of AEDs in psychiatry is an issue of concern, according to all the diagnosis-specific related reimbursement codes that have been registered. Documentation of adverse drug reactions in this group of patients is, however, scarce [27, 28].
Neuropathic pain and migraine
The use of pregabalin and gabapentin has increased in recent years, and they are the predominant AEDs used in neuropathic pain [29]. The use of carbamazepine in neuropathic pain is mainly limited to trigeminal neuralgia, according to previous findings where this indication had a separate reimbursement code [3]. The increase in utilisation of gabapentin may be due to differences in the preference of reimbursement in neuropathic pain [20, 21]. The two drugs have similar efficacy and tolerability profiles [30]. Pregabalin has a potential for abuse as reported from the WHO database from 12 countries and findings from NorPD in Norway [31, 32]. Gabapentin is also at risk based on the similar mechanism of action, and case reports have been published, but it has a large variability in bioavailability [33–36]. This demonstrates a need for surveillance of drug utilisation at an international level. Migraine is still a minor indication for AEDs while the number of patients using topiramate as migraine prophylaxis is increasing [3].
Safety aspects of AEDs in special patient populations and changes in prescriptions
Focus on special patient groups where pharmacokinetic variability and safety is of importance requires careful pharmacological considerations and close monitoring [7, 9, 37]. Gender- and age-specific safety aspects of drug utilisation are thus important to document. The use of AEDs in children is mainly restricted to epilepsy. Lamotrigine is widely used in epilepsy and psychiatry. The use of valproate in women is decreasing and is an important concern regarding adverse effects and teratogenic effects [9, 38]. Nearly 50 % of the patients were more than 60 years old where pharmacological challenges increase. The use of gabapentin and pregabalin in neuropathic pain in elderly patients is important in this regard.
The Norwegian public reimbursement scheme covers the expenditures for all drugs used in chronic indications, and therefore, reimbursement of AEDs is almost complete (including off-label use), in contrast to many European countries [39]. The national authorities require initial use in neuropathic pain before full reimbursement is given for gabapentin and pregabalin. The present data of the prescriptions show a considerable part (>80 %) of prescriptions prescribed by general practitioners as compared to specialists (20 %). However, they may initially be issued by specialists and then continued by general practitioners. This is disquieting, since detailed knowledge of the individual drugs and extent of pharmacological variability and safety concerns are essential.
Retention rates of AEDs in epilepsy and non-epilepsy indications
The retention rate reflects effectiveness (efficacy and/or tolerability) of AEDs, and Kaplan–Meier statistics have not been used in this context as far as the authors are aware of. Overall, the newer AEDs have higher retention rates and a longer mean time to discontinuation than the older drugs. This is in line with other studies of carbamazepine, lamotrigine and levetiracetam [40, 41]. Lack of effect was the primary reason for discontinuation of AEDs in another study [42], but this could not be distinguished in the present study. The present analyses of a nationwide population contribute to long-term safety data of AED use in various indications as part of pharmacovigilance that cannot be provided in post-marketing studies.
Methodological considerations
The NorPD is a validated database well suited for pharmacoepidemiological studies [3, 4, 23]. In NorPD, >90 % of the population is included [16]. The implementation of ICD-10 and ICPC-2 systems from 2008 gives access to more detailed information regarding clinical use of AEDs in non-epilepsy disorders and could be used as a direct measure, in contrast to other studies in Europe [12, 43, 44]. A limitation is that patients treated in hospitals and institutions are not included in NorPD. The term DDD is a defined value for each drug and does not necessarily reflect the actual prescribed daily dose (PDD) in clinical practice. Such studies are important, as concluded in an evaluation of pharmacoepidemiology, to monitor and extend knowledge of safety after authorization [11, 45].
Conclusions
The use of AEDs is increasing in non-epilepsy disorders and accounted for 53 % of the total utilisation in 2012. AEDs are almost completely reimbursed, with only 20 % of prescriptions from specialists and 80 % from general practitioners. Newer AEDs are most commonly used and show the highest retention rates (34–48 %) (2004–2012): levetiracetam in epilepsy, lamotrigine in psychiatry, pregabalin and gabapentin in neuropathic pain and topiramate in migraine. This nationwide study demonstrates an increased exposure to AEDs in new patient groups, and details in prescription patterns and clinical and safety considerations should be closely monitored. This contributes to long-term post-marketing data of AEDs and accordingly improved pharmacovigilance.
Authors’ note on contribution to the manuscript
Arton Baftiu and Cecilie Johannessen Landmark have planned and designed the study and written the first draft and been responsible for the revisions. Arton Baftiu, Cecilie Johannessen Landmark, Ida Rudberg Rusten and Silje Andrea Feet have performed data analyses regarding utilisation of AEDs. Svein I. Johannessen has contributed in the planning, handling and revisions of the study. Pål G. Larsson has performed Kaplan–Meier analyses and has been responsible for the handling of the database. All authors are responsible for the final version of the manuscript.
References
Tsiropoulos I, Gichangi A, Andersen M, Bjerrum L, Gaist D, Hallas J (2006) Trends in utilization of antiepileptic drugs in Denmark. Acta Neurol Scand 113:405–411
Savica R, Beghi E, Mazzaglia G, Innocenti F, Brignoli O, Cricelli C, Caputi AP, Musolino R, Spina E, Trifirò G (2007) Prescribing patterns of antiepileptic drugs in Italy: a nationwide population-based study in the years 2000-2005. Eur J Neurol Off J Eur Fed Neurol Soc 14:1317–1321
Johannessen Landmark C, Larsson PG, Rytter E, Johannessen SI (2009) Antiepileptic drugs in epilepsy and other disorders—a population-based study of prescriptions. Epilepsy Res 87:31–39
Landmark CJ, Fossmark H, Larsson PG, Rytter E, Johannessen SI (2011) Prescription patterns of antiepileptic drugs in patients with epilepsy in a nation-wide population. Epilepsy Res 95:51–59
Oteri A, Trifiro G, Gagliostro MS, Tari DU, Moretti S, Bramanti P, Spina E, Caputi AP, Arcoraci V (2010) Prescribing pattern of anti-epileptic drugs in an Italian setting of elderly outpatients: a population-based study during 2004-07. Br J Clin Pharmacol 70:514–522
Italiano D, Capuano A, Alibrandi A, Ferrara R, Cannata A, Trifiro G, Sultana J, Ferrajolo C, Tari M, Tari DU, Perrotta M, Pagliaro C, Rafaniello C, Spina E, Arcoraci V (2015) Indications of newer and older anti-epileptic drug use: findings from a southern Italian general practice setting from 2005-2011. Br J Clin Pharmacol 79:1010–1019
Johannessen Landmark C, Johannessen SI, Tomson T (2012) Host factors affecting antiepileptic drug delivery-pharmacokinetic variability. Adv Drug Deliv Rev 64:896–910
Johannessen Landmark C (2008) Antiepileptic drugs in non-epilepsy disorders: relations between mechanisms of action and clinical efficacy. CNS Drugs 22:27–47
Landmark CJ, Johannessen SI (2012) Safety aspects of antiepileptic drugs—focus on pharmacovigilance. Pharmacoepidemiol Drug Saf 21:11–20
Takahashi Y, Nishida Y, Asai S (2012) Utilization of health care databases for pharmacoepidemiology. Eur J Clin Pharmacol 68:123–129
Wise L (2011) Risks and benefits of (pharmaco)epidemiology. Ther Adv Drug Saf 2:95–102
Hamer HM, Dodel R, Strzelczyk A, Balzer-Geldsetzer M, Reese JP, Schoffski O, Graf W, Schwab S, Knake S, Oertel WH, Rosenow F, Kostev K (2012) Prevalence, utilization, and costs of antiepileptic drugs for epilepsy in Germany—a nationwide population-based study in children and adults. J Neurol 259:2376–2384
WHO. (2002) The importance of pharmacovigilance. Safety Monitoring of Medicinal Products. World Health Organization 2002.
WHO Collaboration Center. Available at http://www.whocc.no.
The Norwegian Institute of Public Health, The National Prescription Database (NorPD). Available at: http://www.reseptregisteret.no.
Furu K (2008) Establishment of the nationwide Norwegian Prescription Database (NorPD)—new opportunities for research in pharmacoepidemiology in Norway. Nor Epidemiol 18:129–136
ICD-10 classification system. Available at: http://www.who.int/classifications/icd/en/.
ICPC-2 classification system. Available at: https://helsedirektoratet.no/helsefaglige-kodeverk/icpc-2-den-internasjonale-klassifikasjonen-for-primerhelsetjenesten. [Norwegian]
Statistics Norway. Available at: http://www.ssb.no.
The Norwegian Medicines Agency. Reimbursement status for pregabalin. Available at: http://www.legemiddelverket.no.
The Norwegian Medicines Agency. Reimbursement status for gabapentin. Available at: http://www.legemiddelverket.no.
Glauser T, Ben-Menachem E, Bourgeois B, Cnaan A, Guerreiro C, Kalviainen R, Mattson R, French JA, Perucca E, Tomson T (2013) Updated ILAE evidence review of antiepileptic drug efficacy and effectiveness as initial monotherapy for epileptic seizures and syndromes. Epilepsia 54:551–563
Karouni M, Arulthas S, Larsson PG, Rytter E, Johannessen SI, Landmark CJ (2010) Psychiatric comorbidity in patients with epilepsy: a population-based study. Eur J Clin Pharmacol 66:1151–1160
Connolly KR, Thase ME. The clinical management of bipolar disorder: a review of evidence-based guidelines. The Primary Care Companion for CNS Disorders 2011;13
Bramness JG, Groholt B, Engeland A, Furu K (2009) The use of lithium, valproate or lamotrigine for psychiatric conditions in children and adolescents in Norway 2004-2007—a prescription database study. J Affect Disord 117:208–211
Golden AS, Haut SR, Moshe SL (2006) Nonepileptic uses of antiepileptic drugs in children and adolescents. Pediatr Neurol 34:421–432
Citrome L (2009) Adjunctive lithium and anticonvulsants for the treatment of schizophrenia: what is the evidence? Expert Rev Neurother 9:55–71
Mason J, Pirmohamed M, Nunn T (2012) Off-label and unlicensed medicine use and adverse drug reactions in children: a narrative review of the literature. Eur J Clin Pharmacol 68:21–28
Attal N, Cruccu G, Baron R, Haanpaa M, Hansson P, Jensen TS, Nurmikko T (2010) EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol Off J Eur Fed Neurol Soc 17:1113–1188
Perez C, Navarro A, Saldana MT, Masramon X, Rejas J (2010) Pregabalin and gabapentin in matched patients with peripheral neuropathic pain in routine medical practice in a primary care setting: findings from a cost-consequences analysis in a nested case-control study. Clin Ther 32:1357–1370
Landmark CJ, Larsson PG, Rytter E, Johannessen SI (2011) Clarification about pregabalin and the Norwegian Prescription Database. Tidsskr Nor Laegeforen 131:800–801 [Norwegian]
Caster O, Edwards IR, Noren GN, Lindquist M (2011) Earlier discovery of pregabalin’s dependence potential might have been possible. Eur J Clin Pharmacol 67:319–320
Gabapentin and pregabalin: abuse and addiction. Prescrire Int 2012; 21: 152–4.
Kruszewski SP, Paczynski RP, Kahn DA (2009) Gabapentin-induced delirium and dependence. J Psychiatr Pract 15:314–319
Gidal BE, Radulovic LL, Kruger S, Rutecki P, Pitterle M, Bockbrader HN (2000) Inter- and intra-subject variability in gabapentin absorption and absolute bioavailability. Epilepsy Res 40:123–127
Johannessen Landmark C, Beiske G, Baftiu A, Burns ML, Johannessen SI (2015) Experience from therapeutic drug monitoring and gender aspects of gabapentin and pregabalin in clinical practice. Seizure 28:88–91
Patsalos PN, Berry DJ, Bourgeois BF, Cloyd JC, Glauser TA, Johannessen SI, Leppik IE, Tomson T, Perucca E (2008) Antiepileptic drugs—best practice guidelines for therapeutic drug monitoring: a position paper by the subcommission on therapeutic drug monitoring, ILAE Commission on Therapeutic Strategies. Epilepsia 49:1239–1276
Tomson T, Landmark CJ, Battino D (2013) Antiepileptic drug treatment in pregnancy: changes in drug disposition and their clinical implications. Epilepsia 54:405–414
Baftiu A, Johannessen Landmark C, Nikaj V, Neslein IL, Johannessen SI, Perucca E (2015) Availability of antiepileptic drugs across Europe. Epilepsia 56:e191–e197
Saetre E, Perucca E, Isojarvi J, Gjerstad L (2007) An international multicenter randomized double-blind controlled trial of lamotrigine and sustained-release carbamazepine in the treatment of newly diagnosed epilepsy in the elderly. Epilepsia 48:1292–1302
Werhahn KJ, Trinka E, Dobesberger J, Unterberger I, Baum P, Deckert-Schmitz M, Kniess T, Schmitz B, Bernedo V, Ruckes C, Ehrlich A, Kramer G (2015) A randomized, double-blind comparison of antiepileptic drug treatment in the elderly with new-onset focal epilepsy. Epilepsia 56:450–459
Chung S, Wang N, Hank N (2007) Comparative retention rates and long-term tolerability of new antiepileptic drugs. Seizure 16:296–304
de Groot MC, Schuerch M, de Vries F, Hesse U, Oliva B, Gil M, Huerta C, Requena G, de Abajo F, Afonso AS, Souverein PC, Alvarez Y, Slattery J, Rottenkolber M, Schmiedl S, Van Dijk L, Schlienger RG, Reynolds R, Klungel OH (2014) Antiepileptic drug use in seven electronic health record databases in Europe: a methodologic comparison. Epilepsia 55:666–673
Giussani G, Canelli V, Bianchi E, Franchi C, Nobili A, Erba G, Beghi E (2016) A population-based study of active and drug-resistant epilepsies in Northern Italy. Epilepsy Behav: EnB 55:30–37
Wettermark B, Zoega H, Furu K, Korhonen M, Hallas J, Norgaard M, Almarsdottir A, Andersen M, Andersson Sundell K, Bergman U, Helin-Salmivaara A, Hoffmann M, Kieler H, Martikainen J, Mortensen M, Petzold M, Wallach-Kildemoes H, Wallin C, Sørensen H (2013) The Nordic prescription databases as a resource for pharmacoepidemiological research—a literature review. Pharmacoepidemiol Drug Saf 22:691–699
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Norwegian Institute of Public Health. The ethical considerations included that the data were anonymous with no patient identification, as each patient was given a running number in the data file (pseudonymous), and Statistics Norway provided security for protection of patient information.
Disclosure
The authors have no conflicts of interest or any financial disclosures, sponsors or grants regarding this manuscript. The results have not previously been presented.
Additional information
An erratum to this article is available at http://dx.doi.org/10.1007/s00228-017-2252-0.
Rights and permissions
About this article
Cite this article
Baftiu, A., Johannessen Landmark, C., Rusten, I.R. et al. Changes in utilisation of antiepileptic drugs in epilepsy and non-epilepsy disorders—a pharmacoepidemiological study and clinical implications. Eur J Clin Pharmacol 72, 1245–1254 (2016). https://doi.org/10.1007/s00228-016-2092-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-016-2092-3