Abstract
Purpose
The purpose of this study was to measure the rate of substitution failure to generic antiepileptic drugs (AEDs) compared to two other pharmacotherapeutic classes (neuroleptics, beta-blockers).
Methods
We conducted a cohort study involving beneficiaries of the French health insurance system from January 2009 to November 2012. Substitution failure to generic drugs was estimated by the rate of switchback (i.e. from generic drug back to its branded drug). We selected the patients who had a dispensation of a branded AED for 60 days or more during the 90 days preceding the generic substitution. Cox proportional hazard regression was used to model time to switchback for antiepileptics vs. other therapeutic classes in the 90 days after generic substitution, adjusting for age, gender and polytherapy.
Results
The cohort included 6727 patients of whom 1947 were exposed to AEDs, 2398 to neuroleptics and 2382 to beta-blockers. The switchback rate was 62% for AEDs. AED users were more likely to switch back as compared to beta-blocker (crude hazard ratio 1.87; 95% CI 1.68–2.07 for patients under 75) or neuroleptic users. The same observation was made in patients above 75 years (crude hazard ratio 1.36; 95% CI 1.16–1.60).
Conclusions
Compared to beta-blocker users, AED users were more likely to switch back to the branded drug, whereas this difference was not observed with neuroleptics. These results could reflect a poor acceptance of switching AEDs to generic compounds in France.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Generic drugs are used to contain pharmaceutical costs in healthcare by introducing an element of price competition once the patent of the innovator (branded) drug has expired, generally after a dozen years or sooner. The goals of this strategy are to decrease healthcare expenditures in developed countries (in France, an estimated 13.4 billion euros were saved by the Social Security in 2012) and to facilitate healthcare access in developing countries. However, the therapeutic equivalence of generic drugs has been put into question, especially for antiepileptic drugs (AEDs) and immunosuppressants [1, 2]. Before approval, candidate generic drugs must demonstrate systemic exposures (two one-sided 95% confidence intervals (CIs), around maximal concentration (Cmax) and area under the curve) that are within the prespecified equivalence boundaries of 80 to 125%. For some drugs needing strictly controlled plasma concentrations, such as antiepileptics or immunosuppressants, where over- or underdosing might result in serious toxicity or life-threatening treatment failure, the European Medical Agency (EMA) gives a limit of 90.00–111.11% for the AUC range [3]. However, a study comparing bioequivalence parameters of generic and brand name antiepileptics [4] suggested a difference of AUC higher than 15% between two generics of the same drug (e.g. oxcarbazepine 25–30%).
A review focused on randomized clinical trials and observational studies [5] showed a controversial result: no significant loss of efficacy was found for generic compared to brand name in clinical trials (concerning only older AEDs), while observational studies showed a significant association between substitution of brand name antiepileptic drugs and increase in the risk of hospitalization. An observational study showed that the refilling of an AED was associated with an elevated risk of seizure-related events and an increase in hospitalizations, whatever the nature of change: brand name drug to generic, generic to brand name or generic to another one [5, 6]. A recent study showed that seizures were not increased when branded levetiracetam was interchanged with a generic equivalent [7]. Finally, two Canadian studies comparing switch and switchback rates in subjects exposed to AED with those exposed to drugs for chronic diseases (statins, antidepressants) found a higher switchback rate in patients exposed to AED [8, 9].
In France, there has been some distrust regarding generic drugs, especially for antiepileptics, which is likely to have impacted antiepileptic substitution and switchback rates to branded medicines compared with other chronic treatments. The aim of the study was to estimate the rate of substitution failure to generic AEDs compared to two other pharmacotherapeutic classes used in chronic diseases (beta-blockers and neuroleptics).
Methods
Data source
In France, the National Health Insurance Scheme comprises several specific plans and covers the whole population, that is to say 63.4 million inhabitants in 2008. The general scheme, the Health Insurance Fund for Salaried Workers (CNAM-TS), covers approximately 86% of the population. The National Health Insurance Fund for Agricultural Workers and Farmers (MSA) and the scheme for the self-employed (RSI) represent 5% each, and 12 additional schemes cover the remaining 4%. The information system SNIIRAM, for “Système National Inter-Regime De l’Assurance Maladie”, contains individualized, anonymous and exhaustive data on all health spending reimbursements [10].
Participants, design and settings
We conducted a comparative cohort study using anonymous data from individuals covered by the general scheme from January 2009 to November 2012. The reimbursement database (ERASME, “Extraction, Recherches, Analyses pour un Suivi Médico-Economique”, maintained by the CNAM-TS) exhaustively records all healthcare expenditures that are reimbursed, including medicinal products and outpatient medical and nursing care prescribed or executed by any healthcare professional (general practitioners, specialists, nurses, clinical lab biologists, pharmacists, etc.). This database does not inform directly about the medical indication of each reimbursement but provides the status of patients in regard to many chronic diseases that are considered as severe and costly (ALD, “Affection de longue durée”). These long-term diseases are 100% reimbursed after agreement of a social security physician and are recorded according to ICD-10 classification.
The long-term diseases scheme concerned 9.5 million people from the French general scheme on 31 December 2012 [11].
For each pharmacological class, a sample of the study population was selected based on the following criteria: eligible patients who continuously used the branded drugs for ≥3 months (T3) preceding the generic switch (T0) (Fig. 1). “Continuous use” was defined as a maximum gap of 60 days between two dispensings.
The study population was categorized into two groups by age class (<75 vs. ≥75 years). Exclusion criteria were (a) event occurring on the day of inclusion, (b) history of stroke or cancers and (c) pregnancy during the study. Study group assignment was done on the basis of drug exposure during the whole period of the study (1 January 2009 to 30 November 2012), based on the Anatomical Therapeutic Chemical (ATC) classification (C07 for beta-blockers, N05A for neuroleptics and N03 for antiepileptics).
Exposure definition and measurement
The period of exposure to a generic drug was defined as the period between first fill and up to occurrence of the event or censoring (Fig. 1). Generic drugs were identified and described with package codes used for reimbursement by the health insurance system (CIP). Both pharmacotherapeutic classes chosen as reference are also used in chronic diseases. Beta-blocker drugs are used mainly for cardiovascular diseases (except for propranolol that can also be used for migraines), and neuroleptics are psychotropic drugs used chronically.
Outcome definition and measurement
“Switchback” was defined as a switching from the branded drug to the generic and then back to the branded drug. Patients who were lost to follow-up were censored.
Covariates
Risk factors considered were age (<75 vs. ≥75 years), gender and monotherapy or polytherapy patients (polytherapy patients were those using at least one other drug from the same therapeutic class at the same time as the drug under study).
Statistical analysis
We described the characteristics of drug users according to pharmacotherapeutic class using numbers and percentages for qualitative variables, and median and interquartile range for quantitative variables. Switchback probabilities were estimated using the Kaplan–Meier method, which is a conditional probability approach based on the subjects who were on the generic drug at the beginning of the interval. This represents the probability that a patient will eventually switch back to the branded drug after being switched to the generic. We used Kaplan–Meier curves and log-rank tests for univariate switchback survival analyses in patients exposed to AEDs and non-exposed groups. We used univariate and multivariate adjusted Cox proportional hazards model to evaluate the association between antiepileptic use vs. other therapeutic classes and risk of switchback, adjusting for age, gender and polytherapy. Crude and adjusted hazard ratios and their corresponding 95% confidence intervals were computed. Statistical analyses were performed using SAS 9.4® (SAS® Institute Inc., Cary, NC, USA).
Results
Description of the cohort population
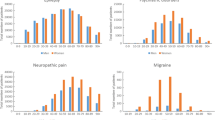
Among the 6964 patients extracted, 237 exhibited at least one exclusion criterion and then 6727 were finally included. Among these patients, 1947 (28.9%) were exposed to AEDs, 2398 to neuroleptics and 2382 to beta-blockers. Table 1 shows the baseline characteristics of these patients. Neuroleptic and antiepileptic users were younger than beta-blocker users (mean age 54.6 and 51.8 years vs. 70.7 years). In contrast to AED and beta-blocker users (with a sex ratio of 42 and 49%, respectively), the percent of males was higher in neuroleptic users (54%). Table 2 presents the repartition of different reimbursed drugs for each pharmacotherapeutic class. The three most used AEDs were levetiracetam, carbamazepine and lamotrigine, while the three most frequent neuroleptics were olanzapine, risperidone and sulpiride. Beta-blocker users used mainly bisoprolol and nebivolol. Propanolol users represented 1% of patients with beta-blocker.
Relation between exposure to pharmacotherapeutic classes and switchback rate
Only patients with non-missing value for age or gender are maintained in the multivariable analysis (n = 6701). Table 3 compares the rate of switchback of patients from generic to branded drugs for AEDs, beta-blockers and neuroleptics, according to age class (±75 years). AEDs had higher switchback rates compared with other drugs (62 vs. 45% for neuroleptics and 42% for beta-blockers). The switchback rate for AEDs is reduced in those after 75 years as compared to those under 75 (65 vs. 50%), but remained more elevated than for neuroleptics and beta-blockers.
Table 4 presents the univariate and multivariate Cox models of switchback patterns for AEDs compared to those for neuroleptics and beta-blockers (used as the reference), stratified according to age class (±75 years). The comparison of patients exposed to neuroleptics to those exposed to beta-blockers did not show significant difference for switch back to branded drug in both age classes. Among patients under 75 years, the AED switchback rate (65%) was significantly higher than beta-blockers (crude HR 1.87; 95% CI 1.68–2.07; p < 0.0001). No further adjustment was performed as gender and polytherapy were not associated with switchback in univariate analyses. In patients ≥75 years, the rate of switchback for AEDs was lower (50%) but remained significantly higher than for beta-blockers (crude HR 1.36; 95% CI 1.16–1.60; p < 0.001), even after adjustment on gender (adjusted HR 1.36; 95% CI 1.16–1.60, p < 0.002).
Discussion
According to our findings, antiepileptic drug users were 1.5 times more likely to switch back from generic to branded drugs after generic substitution, as compared to beta-blocker users. This difference was not observed when comparing beta-blocker users and neuroleptic users. This increase in switchback rate is less important in patients aged 75 and more. This could be explained by an increased vigilance of prescribers and pharmacists for generic substitution in this population, illustrated by an agreement between pharmacist and health insurance to maintain the same brand/generic drug along dispensing for long-term use of drugs [12]. A study performed in Denmark has shown that substitution in the elderly did not seem to impact long-term adherence to drugs [13]. The Canadian study performed in 2007 showed that the switchback rate was 2.4-fold higher for antiepileptics compared to that for other drug classes [9]. Our results differed from both Canadian studies whereas both studies showed an increased probability of switching back with antiepileptics. The variations between switchback rates according to countries, with a higher rate in France, could be explained by differences in national health policy. In Canada, since 2006, the reimbursement of the branded drug when the generic exists requires a special administrative request by the prescriber (special application form combining the identification of the patient, prescriber, drug and reason for requesting the reimbursement of the branded drug) [9].
Choice of the comparator
In order to assess our hypothesis of a higher switchback rate for antiepileptics in reason of a more pronounced nocebo effect, we have chosen controls among drugs used for chronic disease, i.e. beta-blockers, cardiovascular drugs and neuroleptics, other drugs in which the nocebo effect is also expected to have a significant impact.
Strengths and limitations
This observational study is based on data from the main health insurance scheme. These pre-registered and complete real-life data are not likely to be impacted by study implementation. Use of the French health insurance database is increasing since its implementation in 2003, and the validity of the ERASME database has been established [10, 14, 15]. ERASME covers 87% of the general population, ensuring sufficient representativeness and completeness. Data from reimbursement are intrinsically linked with dispensing data. Antiepileptics, neuroleptics and beta-blockers are available on medical prescription only and are then recorded in the ERASME database.
Several limitations have to be acknowledged. There is no referenced long-term condition for arterial hypertension, so patients with beta-blockers were selected on the basis of drugs received and not on disease. In addition, one beta-blocker, propranolol, is also indicated in migraine, which is likely to overestimate the switchback rate for arterial hypertension. However, propranolol represented no more than 1% of beta-blocker users. Furthermore, adverse drug reactions (ADRs) could also lead to the withdrawal of a generic and switch back to brand name, but the lack of medical data including ADRs, related to the characteristics of our data source, did not allow us to analyse this criterion.
Another limitation is that the year of substitution was not taken into account as a confounding factor. Indeed, there have been many regulatory changes in the conditions of generic substitution and their dispensing in France in the later years. This could have affected switchback rates. Finally, residual confounding remains a limitation of our work, with a lack of medical and social variables. Prior substitution before study start was not taken into account. However, studies have shown that patients with previous substitution are less likely to demonstrate a lack of observance as compared to naive patients [16]. Nevertheless, available data seem sufficient in regard to their impact in treatment observance.
We have chosen switchback from the generic to the branded drug as an indicator of substitution failure. Medical chart review and linkage with hospital data (PMSI, “Programme de Médicalisation des Systèmes d’Information”) could complete data analysis with detailed information on clinical factors, reasons for generic substitution or substitution between different brand names. The PMSI enables to identify risk of hospitalization in relation to drug use [17]. Investigating hospitalization after switchback to the branded drug should enable to assess the relation between switchback and effectiveness of the generic drug and to further precise the failure of generic substitution.
Comparison with existing literature
Our study and both Canadian studies exhibited an increase in the probability of switching back to the branded drug with antiepileptic drugs [8, 9]. A study performed in Denmark in 2013 has shown that substitution was less frequent for antiepileptic drugs as compared to that for other drug classes, reflecting the suspicion of neurologists toward generic drugs [18]. This study revealed that young age increased the odds of experiencing a generic switch, as compared to older patients (40–49 years). Finally, the switchback rate according to pharmacologic and therapeutic classes is highly impacted by marketing strategies [19]. These marketing strategies are also observed for antiepileptics, particularly for pregabalin, traditionally used in epilepsy but more recently indicated in neuropathic pain [20]. According to a French study [20], there is a wide variation in generic substitution rates between drugs of the same pharmacotherapeutic class, in particular for oral hypoglycaemic drugs.
Implication for research and practice
This study provides an overview of the patterns of generic substitution practices in France. A positive perception from physicians, pharmacists and patients and knowledge of generic drugs are two essential prerequisites to promote their use at a larger scale. Further governmental initiatives to facilitate generic prescription should be focused on this aspect [13, 21]. Appearance of the drugs could also have an impact on patients’ observance [22], as a switch between two drugs with different colours or aspects may be problematic in some patients.
Conclusion
Compared to beta-blocker users, AED users were more likely to switch back to the branded drug, whereas this difference was not observed with neuroleptics. These results could reflect a poor acceptance of switching AEDs to generic compounds in France. With many drugs reaching the end of their patent protection, use of generic drugs should rise in the next years, mainly for economic reasons. A better understanding of the factors limiting the success of generic substitution is then crucial to maintain this growing number of patients under treatment.
References
Berg MJ, Gross RA, Tomaszewski KJ et al (2008) Generic substitution in the treatment of epilepsy: case evidence of breakthrough seizures. Neurology 71:525–530. doi:10.1212/01.wnl.0000319958.37502.8e
Gauzit R, Lakdhari M (2012) Generic antibiotic drugs: is effectiveness guaranteed? Med Mal Infect 42:141–148
Committee for Medicinal Products for Human Use. Guideline on the investigation of bioequivalence. CPMP/EWP/QWP/1401/98 Rev.1/Corr**2010 http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2010/01/WC500070039.pdf. Accessed 5 december 2016.
Krauss GL, Caffo B, Chang Y-T et al (2011) Assessing bioequivalence of generic antiepilepsy drugs. Ann Neurol 70:221–228. doi:10.1002/ana.22452
Kesselheim AS, Stedman MR, Bubrick EJ et al (2010) Seizure outcomes following the use of generic versus brand-name antiepileptic drugs. Drugs 70:605–621. doi:10.2165/10898530-000000000-00000
Talati R, Scholle JM, Phung OP et al (2012) Efficacy and safety of innovator versus generic drugs in patients with epilepsy: a systematic review. Pharmacotherapy 32:314–322. doi:10.1002/j.1875-9114.2012.01099.x
Vari MS, Pinto F, Mencaroni E et al (2016) Safety of overnight switch from brand-name to generic levetiracetam. Clin Drug Investig 36:87–91. doi:10.1007/s40261-015-0351-1
LeLorier J, Duh MS, Paradis PE et al (2008) Clinical consequences of generic substitution of lamotrigine for patients with epilepsy. Neurology 70:2179–2186. doi:10.1212/01.wnl.0000313154.55518.25
Andermann F, Duh MS, Gosselin A, Paradis PE (2007) Compulsory generic switching of antiepileptic drugs: high switchback rates to branded compounds compared with other drug classes. Epilepsia 48:464–469. doi:10.1111/j.1528-1167.2007.01007.x
Martin-Latry K, Bégaud B (2010) Pharmacoepidemiological research using French reimbursement databases: yes we can! Pharmacoepidemiol Drug Saf 19:256–265. doi:10.1002/pds.1912
Prévalences des ALD, 2012. http://www.ameli.fr/fileadmin/user_upload/documents/Prevalences_2012_mise_en_garde.pdf. Accessed 28 Sep 2016
Imbaud D, Morin A, Picard S, Toujas F (2012) Evaluation de la politique française des médicaments génériques. http://leciss.org/sites/default/files/Rapport%20IGAS_medicaments%20generiques_2012.pdf. Accessed 26 September 2016.
Olesen C, Harbig P, Barat I, Damsgaard EM (2013) Generic substitution does not seem to affect adherence negatively in elderly polypharmacy patients. Pharmacoepidemiol Drug Saf 22:1093–1098
Latry P, Molimard M, Bégaud B, Martin-Latry K (2010) How reimbursement databases can be used to support drug utilisation studies: example using the main French national health insurance system database. Eur J Clin Pharmacol 66:743–748. doi:10.1007/s00228-010-0819-0
Noize P, Bazin F, Dufouil C et al (2009) Comparison of health insurance claims and patient interviews in assessing drug use: data from the Three-City (3C) Study. Pharmacoepidemiol Drug Saf 18:310–319. doi:10.1002/pds.1717
Rathe J, Andersen M, Jarbøl DE et al (2015) Generic switching and non-persistence among medicine users: a combined population-based questionnaire and register study. PLoS One 10:e0119688. doi:10.1371/journal.pone.0119688
Durrieu G, Batz A, Rousseau V et al (2014) Use of administrative hospital database to identify adverse drug reactions in a pediatric university hospital. Eur J Clin Pharmacol 70:1519–1526. doi:10.1007/s00228-014-1763-1
Rathe J, Larsen P, Andersen M et al (2013) Associations between generic substitution and patients’ attitudes, beliefs and experiences. Eur J Clin Pharmacol 69:1827–1836. doi:10.1007/s00228-013-1539-z
Sommet A, Georgel B, Poutrain J-C et al (2013) Différences de taux de substitution des médicaments génériques en Midi-Pyrénées en fonction des classes pharmaco-thérapeutiques. Revue d’Épidémiologie et de. Santé Publique 61:539–544. doi:10.1016/j.respe.2013.08.001
Wise J (2015) Doctors are warned not to prescribe generic pregabalin for pain control. BMJ 350:h1724–h1724. doi:10.1136/bmj.h1724
Dylst P, Vulto A, Simoens S (2013) Demand-side policies to encourage the use of generic medicines: an overview. Expert Rev Pharmacoecon Outcomes Res 13:59–72. doi:10.1586/erp.12.83
Kesselheim AS (2013) Variations in pill appearance of antiepileptic drugs and the risk of nonadherence. JAMA Intern Med 173:202. doi:10.1001/2013.jamainternmed.997
Acknowledgements
We would like to thank the direction of medical services of the National Health Insurance Fund for Salaried Workers for the Midi-Pyrénées area (DRSM-CNAMTS).
Authors’ contributions
All the authors have participated in the study design. AM, AP and VR analysed the data. AM, AP and HB wrote the first draft of the manuscript. All the authors participated in the result interpretation and have read and approved the final version of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
The project was not a biomedical research project and therefore did not need the Research Ethics Committee’s approval. The anonymity of patients was strictly preserved throughout the data entry and analysis process.
Rights and permissions
About this article
Cite this article
Molinier, A., Palmaro, A., Rousseau, V. et al. Does substitution of brand name medications by generics differ between pharmacotherapeutic classes? A population-based cohort study in France. Eur J Clin Pharmacol 73, 471–477 (2017). https://doi.org/10.1007/s00228-016-2185-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-016-2185-z