Abstract
Objectives
Longitudinal prescription patterns of antiepileptic drugs (AEDs) have not been described to date in Korea. Here we aimed to describe AED prescribing trends over a 12-year period and assess age differences in AED prescribing patterns in a pediatric epilepsy population.
Methods
We retrieved and analyzed all AED prescribing and dispensing data in 2001–2012 in patients aged 0–18 years with an established diagnosis of epilepsy at the largest tertiary children’s hospital in Korea. AEDs included for analysis were classified as older (i.e., carbamazepine, ethosuximide, phenobarbital, phenytoin, and valproic acid) and newer (i.e., gabapentin, lamotrigine, levetiracetam, oxcarbazepine, pregabalin, topiramate, vigabatrin, zonisamide, lacosamide, and rufinamide) on the basis of market availability before versus after 1991.
Results
A total of 5593 patients with epilepsy were prescribed an AED during the 12-year period. The proportion of newer AED prescriptions was 52.6 % in 2001 and continuously increased to 74.3 % in 2012. Oxcarbazepine was most widely used, followed by valproic acid. While carbamazepine and vigabatrin use progressively decreased over the 12-year period, those of lamotrigine and topiramate rapidly increased. Age differences in prescribing patterns were observed. Polytherapy was observed in 49.7 % of the total population, while 83.9 % of new users were prescribed monotherapy.
Conclusion
This study provided updated information on AED prescription trends for childhood epilepsy. We found a progressive increase in the use of newer AEDs. However, valproic acid, the only prevalent older AED, continued to be widely prescribed. A high rate of polytherapy among the prescriptions overall raises some safety concerns.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The use of newer antiepileptic drugs (AEDs) such as oxcarbazepine, lamotrigine, and topiramate increased over the course of the study period from 52.6 % in 2001 to 74.3 % in 2012. |
Over the 12-year study period, the most commonly prescribed monotherapy was oxcarbazepine, followed by valproic acid. |
For polytherapy, the most prevalent AED was valproic acid, followed by topiramate. |
1 Introduction
Epilepsy is a common chronic neurological disorder in childhood that has the potential to adversely affect educational and social outcomes [1]. The reported median annual incidence rate in pediatric populations is approximately 82.2 per 100,000 [2]. Although other options such as surgery and nerve stimulation are available, the use of antiepileptic drugs (AEDs) remains the mainstay of epilepsy treatment. Several epidemiological studies have evaluated AED prescribing patterns in adult and pediatric populations and reported different trends in the use of second-generation AEDs [3–16]. Prescription patterns have been evaluated most actively in European countries [3–5, 7–13, 17–19], whereas few studies have reported on AED utilization in large pediatric epilepsy cohorts in Asian countries [15, 16]. AED prescribing patterns, particularly with respect to newer AED use in children, vary among countries due to differences in health care systems, AED availability, medication costs, reimbursement systems, epilepsy treatment guidelines, prescribing habits, and other unknown reasons [7]. In Korea, National Health Insurance Cooperation (NHIC), a unique insurer, pays for epilepsy-related health care expenses including AEDs, with only a 30 % co-payment when prescribed for approved indications.
One-year AED prescribing patterns were described in a study using the NHIC database in Korea [20]. However, to the best of our knowledge, no study of the pediatric epilepsy population in Korea has described the initial and longitudinal AED prescription patterns. Thus, the aim of the present study was to describe initial and overall AED prescription trends in children with AED-treated epilepsy over a 12-year period, 2001–2012, at the largest tertiary children’s hospital in Korea. Further, we aimed to assess age differences in AED prescribing patterns in a pediatric epilepsy population.
2 Methods
2.1 Data Source
We retrieved and analyzed all AED prescribing and dispensing data from 2001 to 2012 in an electronic database of Seoul National University Children’s Hospital, the nation’s largest (285-bed) children’s hospital that treats 500 ambulatory pediatric patients daily. The retrieved data contained age, sex, date of prescription issued, generic name, formulary code, dosing regimen, diagnosis code, and hospital utilization history such as ambulatory visit, emergency visit, and inpatient admission information. Approval from the local institutional review board was obtained prior to the data collection and analysis (Approval no.: H-1305-633-492).
2.2 Study Population
The study population was defined as patients aged 0–18 years who were prescribed an AED with an established diagnosis of epilepsy. To assess the pattern of initial AED prescribing in patients treated at this tertiary care children’s hospital, we identified new AED users as those who were not prescribed any AEDs within a 1-year period prior to the first AED prescription in this hospital.
2.3 Study Drugs
The AEDs included in the analysis were classified as older AEDs (i.e., carbamazepine, ethosuximide, phenobarbital, phenytoin, and valproic acid) and newer AEDs (i.e., gabapentin, lamotrigine, levetiracetam, oxcarbazepine, pregabalin, topiramate, vigabatrin, zonisamide, lacosamide, and rufinamide) on the basis of market availability before versus after 1991 [13, 21].
2.4 Data Analysis
2.4.1 AED Utilization Analysis
Instead of using the defined daily dose (DDD) to evaluate AED utilization, we used a concept termed “person-days of treatment”, which indicates the summed number of days of AED treatment. Considering that various dose ranges are required in pediatric patients and changes in AED selection occur frequently, the unit of person-days of treatment was more relevant than DDD. We represented the utilization of individual AEDs and older/newer AEDs as a group as a proportion of AED-treated person-days for all patients for the overall study period and each year.
We also evaluated AED utilization by age group. Patients were categorized into five age groups according to the definition of the National Institute of Child Health and Human Development Pediatric Terminology released in July 2011 [22]: 0–12 months (infancy), 13–24 months (toddler), 2–5 years (early childhood), 6–11 years (middle childhood), and 12–18 years (early adolescence).
2.4.2 Initial AED Treatment Analysis
The pattern of AED prescriptions in new users was evaluated using only the first prescription for each patient. The prescription prevalence was calculated as the number of prescriptions of specific AEDs or groups of interest divided by the total number of AED prescriptions multiplied by 100 %. Prescriptions were counted more than once if more than one AED was prescribed for a single patient.
2.4.3 Mono- and Polytherapy
The prevalence of mono- or polytherapy is shown as proportion of patients. Patients who received two or more AEDs on the same prescription date at least once were classified into the polytherapy group.
2.5 Statistical Analysis
Data are presented with descriptive statistics for demographic and AED utilization characteristics. The distributions of AED utilization by age group were evaluated using Pearson’s Chi-square test using age 0–12 months as the reference group. The AED utilization trends over the 12-year period were verified using the Cochran-Armitage trend test, and the peak significance was tested by the Mack Wolfe test. P values of <0.05 were considered significant and adjusted by Bonferroni correction if necessary.
The data management and statistical analysis were conducted using SAS version 9.3 (SAS Institute, Cary, NC, USA) and R statistical software (Foundation for Statistical Computing, Vienna, Austria).
3 Results
3.1 Patient Population
Over the 12-year study period, a total of 5593 patients with epilepsy were prescribed at least one AED, a mean of 3000 patients were prescribed at least one AED per year, and 4788 patients received their first prescription for an AED (a mean 399 new patients per year). The majority of patients were ≥6 years of age (60.1 % in the population overall, 57.9 % in the new user population), with a high preponderance of male patients. The total population increased in size over the study period, whereas the number of new users remained relatively unchanged. These findings indicate that, due to the chronic nature of the disease, fewer patients were lost during follow-up than were added over time (i.e., incidence). Around half of the patients had focal (partial) epilepsy, while 28.1 % had generalized epilepsy (Table 1).
3.2 Overall AED Utilization
3.2.1 Utilization of AEDs During the 12-Year Study Period
In 2001–2012, 157,110 AED prescriptions (12,227,964 person-days of treatment) were issued. Newer AEDs comprised 67.8 % of the total AED utilization (8,290,665 of 12,227,964 person-days of treatment), with oxcarbazepine (24.3 %) and valproic acid (22.0 %) being the most commonly prescribed in the total population.
During the 12-year period, polytherapy was observed in 2961 patients (47.1 % of the total population); of these patients, 1234 (22.1 % of the total population) were prescribed three or more AEDs. The AEDs most commonly prescribed as monotherapy were oxcarbazepine (34.1 %), valproic acid (30.0 %), lamotrigine (9.6 %), and topiramate (8.7 %). For polytherapy, valproic acid (19.6 %), topiramate (17.4 %), oxcarbazepine (16.5 %), and lamotrigine (14.6 %) were most commonly prescribed.
3.2.2 Changing Trends of AED Utilization over 12 Years
In the total population, the proportion of prescriptions for newer AEDs increased continuously from 52.6 % in 2001 to 74.3 % in 2012 (p < 0.0001). Valproic acid was most commonly used until 2005, continually decreased with the increased use of newer AEDs (p = 0.0023), and then remained the second most prescribed AED. Carbamazepine and vigabatrin showed a rapid decrease in use from 14.4 % and 15.9 % in 2001 to 4.1 and 4.4 % in 2012, respectively (both p < 0.0001). The use of phenytoin and phenobarbital remained fairly low throughout the study period, accounting for <2 % and 3 %, respectively. Since 2006, oxcarbazepine has been the most widely used AED. There was a rapid increase in the use of lamotrigine and topiramate during the 12-year study period (from 6.2 % and 5.9 % in 2001 to 17.7 and 16.9 % in 2012, respectively; p = 0.0002). Levetiracetam became available at the study institution in 2007, and its use continually increased thereafter (p < 0.0001) (Fig. 1).
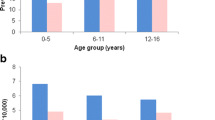
3.2.3 AED Utilization by Age Group
There were significant differences in AED utilization among the five age groups (p = 0.0015). A Bonferroni-corrected post hoc test indicated a statistically significant AED utilization difference between infancy and early childhood (p < 0.01), infancy and middle childhood (p < 0.01), and infancy and early adolescence (p < 0.01). However, no significant AED utilization difference was seen between the infancy and toddler groups.
In patients aged 0–12 months, vigabatrin was the most widely used (32.3 %) AED, followed by valproic acid (24.5 %), lamotrigine (8.5 %), topiramate (8.2 %), phenobarbital (7.9 %), and carbamazepine (7.2 %). The use of vigabatrin and phenobarbital peaked in the infancy group, declined after age 1, and remained fairly constant over the age range of 2–18 years. In patients aged 2–5 years, lamotrigine (23.1 %) was the most widely prescribed AED along with valproic acid (22.4 %).
Valproic acid was widely used across all age groups, with a slow decline after age 2, with the increased use of oxcarbazepine, topiramate, and levetiracetam. Oxcarbazepine was the most utilized AED after age 6. The use of older AEDs decreased as age increased (from 41.6 % in infancy to 27.1 % in early adolescence). Pregabalin, gabapentin, rufinamide, and lacosamide were minimally prescribed, mostly in patients >2 years of age (Fig. 2).
3.3 Prescribing Patterns for Initial AED Treatment
An analysis of the first AED prescriptions in 4788 new users showed that 4015 patients (83.9 %) were prescribed AED monotherapy. There were 2591 (44.2 %) and 3277 (55.8 %) prescriptions of older and newer AEDs among the new user population, respectively. The most frequently selected AED for initial treatment was valproic acid (28.7 %), followed by oxcarbazepine (27.0 %), topiramate (10.1 %), and lamotrigine (10.0 %).
There was a gradual decline in the use of older AEDs as initial monotherapy from 58.0 % in 2003 to 32.5 % in 2009, with a small increase after 2010 (p = 0.002; Fig. 3). Oxcarbazepine (33.3 %) and valproic acid (30.4 %) were the two main AEDs used as initial monotherapy. The proportion of carbamazepine used as monotherapy decreased from 13.3 % in 2003 to 0.7 % in 2012 (p < 0.0001). The decrease in the use of carbamazepine was prominent after 2006. Among the newer AEDs, the use of lamotrigine increased gradually, peaking significantly in 2006–2007 (p = 0.0152) and decreasing thereafter. The use of levetiracetam increased after its introduction in 2007, but the proportion remained low by 2012 (p = 0.0003).
A variety of two-drug combinations were prescribed as initial treatment in 11.3 % of new cases, and the most prevalent combination was oxcarbazepine + valproic acid (12.4 %), followed by topiramate + valproic acid (9.2 %) and carbamazepine + valproic acid (7.9 %).
4 Discussion
This study described the trends of overall and initial AED prescriptions for pediatric epilepsy patients in 2001–2012 at a tertiary children’s hospital in Korea.
4.1 Older Versus Newer AEDs
This study showed that the use of newer AEDs was prevalent in childhood epilepsy patients, with a rapid increase from 53.4 % in 2001 to 74.3 % in 2012. These results conflicted with those from previous reports in which the use of newer AEDs increased but older AEDs remained the mainstay of treatment in children. In Germany, older AEDs were used in 70.4 % of patients, while 48.3 % received new AEDs in 2009 [10]. The use of new AEDs in epilepsy increased from 40 % in 2004 to 49 % in 2009 in Norway [9]. A multinational study also showed that older AEDs were favored over newer AEDs in Italy, the Netherlands, and the UK in 2005 [7]. Older AEDs still remained the dominant epilepsy treatment in 2009 in Singapore [16], and only 22.2 % of patients used new AEDs in 2005–2009 in Hong Kong [15]. Only 16 % of the prescriptions included newer AEDs in 2012 in India [23]. However, similar trends were observed in patients with refractory epilepsy at an Italian tertiary referral hospital in 2006–2007, with newer AEDs representing 54 % of AED prescriptions in children [8].
Although the exact reasons for the rapid increase and dominant use of newer AEDs in Korea could not be obtained from this study, the relatively lower drug cost may partially explain this phenomenon.
4.2 Utilization of Individual AEDs
In this study, oxcarbazepine was the most prevalent AED, followed by valproic acid in overall and initial prescriptions since 2006, while most previous studies reported that valproic acid, the broad-spectrum AED, was the most frequently prescribed AED in children with epilepsy.
A study investigating AED utilization in Dutch children in 1997–2005 showed that the most frequently prescribed AED was valproic acid, followed by carbamazepine and lamotrigine [4]. A multinational study also showed that older AEDs were favored over newer AEDs, with valproic acid being the most commonly used AED in Italy, the Netherlands, and the UK in 2005. Among newer AEDs, topiramate was favored in Italy, while lamotrigine was the most commonly prescribed newer AED in two other countries [7]. In Norway, the most commonly used drugs were valproic acid and lamotrigine in children in 2004–2009 [9]. In Germany, the most preferred AED was valproic acid, followed by carbamazepine and lamotrigine [10]. A cohort study from UK family practice in 2008 showed that valproic acid was most commonly prescribed, followed by lamotrigine and levetiracetam in patients 0–14 years of age [11]. Data from Hong Kong also showed that 82.3 % of patients used either valproic acid or carbamazepine and that topiramate, levetiracetam, and lamotrigine were used in around 7 % of patients [15]. In Singapore, valproic acid (comprising approximately 40 % of the total AED usage), carbamazepine, and phenobarbital were most commonly prescribed in 2000–2009. Among the newer AEDs, levetiracetam was most widely used, followed by topiramate and lamotrigine in 2009 [16]. A cross-sectional study performed in a tertiary teaching hospital in India in 2012 showed that valproic acid was the most commonly prescribed AED, followed by phenytoin [23].
The prevalent use of oxcarbazepine observed in this study has not been documented in previous reports. Oxcarbazepine is structurally related to carbamazepine, has equivalent efficacy, and has many advantages related to its safety profile [24]. The International League Against Epilepsy treatment guideline reported oxcarbazepine as an initial monotherapy for children with partial-onset seizures with Class I evidence [25]. The favorable tolerability profile of oxcarbazepine and the significant proportion of patients with localized-onset epilepsy can partially explain the high prevalence of oxcarbazepine prescriptions. Also, the labeled indications of oxcarbazepine do not have any age restrictions in children in Korea.
In this study, the use of carbamazepine, especially as an initial treatment, decreased significantly, while it was the second most frequently prescribed AED in some previous reports. It may have been replaced by newer AEDs because of its drawbacks, including a significant drug interaction potential and high risk of severe cutaneous adverse reactions [26].
Although levetiracetam is a popular AED in adult patients [27] and its efficacy in the initial monotherapy for patients aged 12 years was demonstrated to be comparable to lamotrigine [28], a low usage of levetiracetam was observed in this study. Its late introduction in Korea and restricted indications for pediatric epilepsy might explain this low usage. Levetiracetam is approved as an initial monotherapy only in adolescents >16 years as well as adjunctive therapy in children ≥1 month with partial epilepsy and in children ≥6 years with primary generalized seizure.
4.3 Age Difference in AED Utilization
This study showed different patterns of AED use by age group even in pediatric patients, which confirmed and expanded upon previous results [6]. In infancy, the most commonly prescribed AED was vigabatrin, which was approved for use as a monotherapy for the treatment of infantile spasms and recommended as secondary therapy after adrenocorticotropic hormone treatment. Although the use of phenobarbital was fairly low across all age groups, its use was highest in the 0–1-year-old group because of its use as a first-line treatment of neonatal seizures.
Lamotrigine, which was the most prevalent newer AED in previous studies [29, 30], was prescribed most frequently in children 2–5 years old. Topiramate comprised 7–8 % of prescriptions for children <2 years of age despite a lack of approval for use in this age group. We can infer that some infants and toddlers require topiramate to control their epilepsy, and its long-term tolerability and effectiveness in children <2 years old with epilepsy were demonstrated in one observational study [31].
4.4 Monotherapy Versus Polytherapy
In the total population, polytherapy was observed in 47.1 % of patients, with more than 22.1 % of prescriptions involving three or more AEDs, a proportion that is greater than those in previous reports. A study conducted in the Netherlands with data from 1997–2005 and data from the USA from 1999–2006 showed that 77.2 % and 73.0 % of children were treated with only one AED, respectively [4, 14]. The higher prevalence of polytherapy indicates that a significant proportion of patients in this population might have been refractory to first-line AEDs. Although polytherapy cannot be avoided in some cases, the use of multiple AEDS raises concerns due to the inherent risk of drug interactions.
Contrary to the findings in the overall population, for children receiving their initial prescription for epilepsy, monotherapy was used in about 83.9 % of cases and valproic acid was the most widely used AED, findings that are consistent with the previous report and guideline [27].
4.5 Study Limitations
Some limitations relating to the use of dispensing data should be considered when interpreting the results of this study. First, we assumed that dispensing data represented the use of AEDs, but we were unable to evaluate the actual use of the dispensed AED. Even though we considered the return history, some dispensed AEDs may not have been used and not returned.
Second, the accuracy of the epilepsy diagnoses may have been limited because they were based on the diagnosis code linked to prescriptions for a claim, which may be affected by coding errors or included as a rule-out criterion. In addition, the data did not contain information regarding epilepsy phenotype, severity, or duration or the therapeutic responsiveness. Therefore, we decided not to evaluate AED use in relation to the different epilepsy subtypes.
Third, since we identified new AED users as those who were not prescribed any AEDs within 1 year from this study hospital and could not consider the prescriptions from other hospitals or clinics, some patients might have received AED prescriptions from their primary physicians before visiting this hospital, which could lead to underestimation of the proportion of patients on monotherapy. However, considering the high proportion of monotherapy in new users, we can infer that the patients who received significant long-term AED therapy before visiting this hospital comprised only a small proportion of the study population.
Finally, the data used for this study came from a single tertiary referral hospital and may not be applicable to the entire population, which may limit the generalizability of this study. The results of this study may be somewhat different from nationwide AED use patterns because a larger proportion of the population may have a complex disease profile and epilepsy that is refractory to conventional AEDs than the general population since they were receiving care at a tertiary hospital. However, the large sample size of this study represents around 10 % of childhood epilepsy patients nationwide considering that 34,265 patients aged 0–19 years visited any health care system with a diagnosis of epilepsy during 2012 according to the national statistics database. In addition, the comparison with 1-year prevalence data based on national claims supports the reliability of the results of this study by providing AED use trends for childhood epilepsy in Korea.
5 Conclusions
The results of this study provide updated information on AED prescription trends for childhood epilepsy. As expected with the growing number of drugs on the market and information available for newer AEDs, the use of newer AEDs showed a progressive increase and appeared popular among AED prescriptions overall. The increase in oxcarbazepine, topiramate, and lamotrigine prescribing indicates that these newer drugs are preferred to the more conventional AEDs. However, valproic acid, the only prevalent older AED, remained widely used owing to its broad-spectrum applicability. Initial AED treatment was primarily prescribed as monotherapy. However, a high rate of polytherapy among the prescriptions overall raises some safety concerns.
References
Camfield PR, Camfield CS. What happens to children with epilepsy when they become adults? Some facts and opinions. Pediatr Neurol. 2014;51:17–23.
Kotsopoulos IA, van Merode T, Kessels FG, de Krom MC, Knottnerus JA. Systematic review and meta-analysis of incidence studies of epilepsy and unprovoked seizures. Epilepsia. 2002;43:1402–9.
Savica R, Beghi E, Mazzaglia G, Innocenti F, Brignoli O, Cricelli C, Caputi AP, Musolino R, Spina E, Trifiro G. Prescribing patterns of antiepileptic drugs in Italy: a nationwide population-based study in the years 2000–2005. Eur J Neurol. 2007;14:1317–21.
van de Vrie-Hoekstra NW, de Vries TW, van den Berg PB, Brouwer OF, de Jong-van den Berg LT. Antiepileptic drug utilization in children from 1997–2005–a study from the Netherlands. Eur J Clin Pharmacol. 2008;64:1013–20.
Alacqua M, Trifiro G, Spina E, Moretti S, Tari DU, Bramanti P, Caputi AP, Arcoraci V. Newer and older antiepileptic drug use in Southern Italy: a population-based study during the years 2003–2005. Epilepsy Res. 2009;85:107–13.
Bielen I, Sruk A, Planjar-Prvan M, Cvitanovic-Sojat L, Kosicek M, Bergman-Markovic B, Baraba R, Butkovic-Soldo S. Age-related pattern of the antiepileptic drug utilization in active epilepsy: a population-based survey. Coll Antropol. 2009;33:659–63.
Hsia Y, Neubert A, Sturkenboom MC, Murray ML, Verhamme KM, Sen F, Giaquinto C, Ceci A, Wong IC. Comparison of antiepileptic drug prescribing in children in three European countries. Epilepsia. 2010;51:789–96.
Malerba A, Ciampa C, De Fazio S, Fattore C, Frassine B, La Neve A, Pellacani S, Specchio LM, Tiberti A, Tinuper P, Perucca E. Patterns of prescription of antiepileptic drugs in patients with refractory epilepsy at tertiary referral centres in Italy. Epilepsy Res. 2010;91:273–82.
Landmark CJ, Fossmark H, Larsson PG, Rytter E, Johannessen SI. Prescription patterns of antiepileptic drugs in patients with epilepsy in a nation-wide population. Epilepsy Res. 2011;95:51–9.
Hamer HM, Dodel R, Strzelczyk A, Balzer-Geldsetzer M, Reese JP, Schoffski O, Graf W, Schwab S, Knake S, Oertel WH, Rosenow F, Kostev K. Prevalence, utilization, and costs of antiepileptic drugs for epilepsy in Germany–a nationwide population-based study in children and adults. J Neurol. 2012;259:2376–84.
Nicholas JM, Ridsdale L, Richardson MP, Ashworth M, Gulliford MC. Trends in antiepileptic drug utilisation in UK primary care 1993–2008: cohort study using the General Practice Research Database. Seizure. 2012;21:466–70.
Strzelczyk A, Haag A, Reese JP, Nickolay T, Oertel WH, Dodel R, Knake S, Rosenow F, Hamer HM. Trends in resource utilization and prescription of anticonvulsants for patients with active epilepsy in Germany. Epilepsy Behav. 2013;27:433–8.
Italiano D, Capuano A, Alibrandi A, Ferrara R, Cannata A, Trifirò G, Sultana J, Ferrajolo C, Tari M, Tari DU, Perrotta M, Pagliaro C, Rafaniello C, Spina E, Arcoraci V. Indications of newer and older anti-epileptic drug use: findings from a southern Italian general practice setting from 2005–2011. Br J Clin Pharmacol. 2015;79:1010–9.
Bourgeois FT, Olson KL, Poduri A, Mandl KD. Comparison of drug utilization patterns in observational data: antiepileptic drugs in pediatric patients. Pediatr Drugs. 2015;13:401–410. doi:10.1007/s40272-015-0139-z.
Kwong KL, Tsui KW, Wu SP, Yung A, Yau E, Eva F, Ma CK, Cherk S, Liu KT, Cheng WW, Yau MM. Utilization of antiepileptic drugs in Hong Kong children. Pediatr Neurol. 2012;46:281–6.
Tan WW, Kong ST, Chan DW, Ho PC. A retrospective study on the usage of antiepileptic drugs in Asian children from 2000 to 2009 in the largest pediatric hospital in Singapore. Pharmacoepidemiol Drug Saf. 2012;21:1074–80.
Mattsson P, Tomson T, Edebol Eeg-Olofsson K, Brannstrom L, Ringback Weitoft G. Association between sociodemographic status and antiepileptic drug prescriptions in children with epilepsy. Epilepsia. 2012;53:2149–55.
Oteri A, Trifiro G, Gagliostro MS, Tari DU, Moretti S, Bramanti P, Spina E, Caputi AP, Arcoraci V. Prescribing pattern of anti-epileptic drugs in an Italian setting of elderly outpatients: a population-based study during 2004–07. Br J Clin Pharmacol. 2010;70:514–22.
Chin RF, Ajetunmobi O, Weir CJ, Wood R. Prescription of emergency antiepileptic medication after a first childhood seizure: analysis of routine administrative data. Epileptic Disord. 2015;17:172–6.
Lee SY, Jung KY, Lee IK, Yi SD, Cho YW, Kim DW, Hwang SS, Kim S, Korean Epilepsy S. Prevalence of treated epilepsy in Korea based on national health insurance data. J Korean Med Sci. 2012;27:285–90.
Lyons B, Abdelmagid E, Banerjee S. Use of newer antiepileptic drugs in children: how NICE are we? Prog Neurol Psychiatry. 2010;14:6–10.
Williams K, Thomson D, Seto I, Contopoulos-Ioannidis DG, Ioannidis JP, Curtis S, Constantin E, Batmanabane G, Hartling L, Klassen T, Sta RCHG. Standard 6: age groups for pediatric trials. Pediatrics. 2012;129(Suppl 3):S153–60.
Bhatt KM, Malhotra SD, Patel KP, Patel VJ. Drug utilization in pediatric neurology outpatient department: a prospective study at a tertiary care teaching hospital. J Basic Clin Pharm. 2014;5:68–73.
Schmidt D, Sachdeo R. Oxcarbazepine for treatment of partial epilepsy: a review and recommendations for clinical use. Epilepsy Behav. 2000;1:396–405.
Glauser T, Ben-Menachem E, Bourgeois B, Cnaan A, Guerreiro C, Kalviainen R, Mattson R, French JA, Perucca E, Tomson T. Updated ILAE evidence review of antiepileptic drug efficacy and effectiveness as initial monotherapy for epileptic seizures and syndromes. Epilepsia. 2013;54:551–63.
Yang MS, Kang MG, Jung JW, Song WJ, Kang HR, Cho SH, Min KU. Clinical features and prognostic factors in severe cutaneous drug reactions. Int Arch Allergy Immunol. 2013;162:346–54.
Chen SY, Wu N, Boulanger L, Sacco P. Antiepileptic drug treatment patterns and economic burden of commercially-insured patients with refractory epilepsy with partial onset seizures in the United States. J Med Econ. 2013;16:240–8.
Rosenow F, Schade-Brittinger C, Burchardi N, Bauer S, Klein KM, Weber Y, Lerche H, Evers S, Kovac S, Hallmeyer-Elgner S, Winkler G, Springub J, Niedhammer M, Roth E, Eisensehr I, Berrouschot J, Arnold S, Schröder M, Beige A, Oertel WH, Strzelczyk A, Haag A, Reif PS, Hamer HM. The LaLiMo Trial: lamotrigine compared with levetiracetam in the initial 26 weeks of monotherapy for focal and generalised epilepsy–an open-label, prospective, randomised controlled multicenter study. J Neurol Neurosurg Psychiatry. 2012;83:1093–8.
Ackers R, Murray ML, Besag FM, Wong IC. Prioritizing children’s medicines for research: a pharmaco-epidemiological study of antiepileptic drugs. Br J Clin Pharmacol. 2007;63:689–97.
Freitas-Lima P, Baldoni Ade O, Alexandre V, Pereira LR, Sakamoto AC. Drug utilization profile in adult patients with refractory epilepsy at a tertiary referral center. Arq Neuropsiquiatr. 2013;71:856–61.
Kim JM, Kwon S, Seo HE, Choe BH, Cho MH, Park SP. Long-term effectiveness and tolerability of topiramate in children with epilepsy under the age of 2 years: 4-year follow-up. J Korean Med Sci. 2009;24:1078–82.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No significant financial support was received for this study.
Conflict of interest
Y.S. Cho, Y.-M. Ah, A.H. Jung, K.J. Kim, and J.-Y. Lee declare that they have no conflict of interest.
Additional information
Y. S. Cho and Y.-M. Ah contributed equally to this work.
Rights and permissions
About this article
Cite this article
Cho, Y.S., Ah, YM., Jung, A.H. et al. Trends in Antiepileptic Drug Prescriptions for Childhood Epilepsy at a Tertiary Children’s Hospital in Korea, 2001–2012. Pediatr Drugs 17, 487–496 (2015). https://doi.org/10.1007/s40272-015-0147-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-015-0147-z