Abstract
Rationale and objectives
Simultaneous alcohol and nicotine consumption occurs in the majority of individuals with alcohol use disorder (AUD) and nicotine dependence. Varenicline (Var) is used to assist in the cessation of nicotine use, while naltrexone (Nal) is the standard treatment for AUD. Despite evidence that ethanol (EtOH) and nicotine (NIC) co-use produces unique neuroadaptations, preclinical research has focused on the effects of pharmacotherapeutics on a single reinforcer. The current experiments examined the effects of Var and Nal on EtOH, NIC, or EtOH+NIC intake.
Methods
Animals were randomly assigned to one of four drinking conditions of 24-h access to a three-bottle choice paradigm, one of which always contained water. Drinking conditions were water only, 0.07 and 0.14 mg/mL NIC (NIC only), 15% and 30% EtOH (EtOH only), or 15% and 30% EtOH with 0.14 mg/mL NIC (EtOH+NIC). The effects of Var (0, 1, or 2 mg/kg) or Nal (0, 1, or 10 mg/kg) injections on maintenance and relapse consumption were determined during four consecutive days.
Results
Var reduced maintenance and relapse NIC intake but had no effect on EtOH or EtOH+NIC drinking. Conversely, Nal reduced EtOH maintenance and relapse drinking, but had no effect on NIC or EtOH+NIC drinking.
Discussion
The results indicate the standard pharmacological treatments for nicotine dependence and AUD were effective at reducing consumption of the targeted reinforcer but neither reduced EtOH+NIC co-use/abuse. These findings suggest that co-abuse may promote unique neuroadaptations that require models of polysubstance abuse to develop pharmacotherapeutics to treat AUD and nicotine dependence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alcohol use disorder (AUD) and nicotine dependence cause, contribute to, and exacerbate many serious health problems and are among the top contributors to preventable deaths occurring worldwide (Grucza and Bierut 2006). Past research has shown that more than 80% of those afflicted with AUD also exhibit comorbid use of nicotine in comparison to 34% of non-alcoholics (John et al. 2003a, b). Likewise, individuals suffering from nicotine dependence are 10 times more likely to be diagnosed with AUD in their lifetime (DiFranza and Guerrera 1990).
The amount of nicotine use is positively correlated with the rate of AUD, and smoking enhances alcohol consumption in AUD individuals compared with non-smoking AUD individuals (Daeppen et al. 2000; Gulliver et al. 1995). Additionally, the severity of AUD has also been positively correlated to a number of other elements including urge to smoke, years smoked, number of attempts to quit smoking, and age an individual began smoking (John et al. 2003a, b). The intensity of nicotine dependence has been associated with exacerbated bouts of relapse in alcoholics (DiFranza and Guerrera 1990). AUD individuals who concurrently stop smoking have a better chance of remaining abstinent than those who continue to smoke (Daeppen et al. 2000; Gulliver et al. 1995). Preclinical research has consistently reported that nicotine can potentiate EtOH-seeking, and drug-seeking is enhanced in rats simultaneously co-administering EtOH and nicotine (Lê et al. 2014; Hauser et al. 2012a, b). These preclinical findings are paralleled in the human literature that indicate individuals concurrently diagnosed with AUD and nicotine dependence have significantly worse clinical outcomes than those who are only diagnosed with AUD or nicotine dependence (Lajtha and Sershen 2010; Grant et al. 2004).
There are no reports of humans injecting nicotine. In contrast, the use of oral spitless products (e.g., snus, a moist powder tobacco packet in which the byproduct is swallowed) has increased in the USA in the last 20 years (Delnevo et al. 2012). In 2011, Americans spent over 340 million dollars on snus products (Delnevo et al. 2012). In Sweden and Norway, the average annual intake of snus approaches the annual combined budgets of NIAAA and NIDA at 1.3 billion dollars (Digard et al. 2009).
The mixing of alcohol and nicotine for oral consumption is evident throughout most of the USA and the rest of the world. In 2003, the creation of the Nicotini was considered one of the top 10 Ideas of the Year by the New York Times Magazine (NYTM 2003). Nicotine-infused alcohols appear to have established a foothold in high-end bars throughout the US (Martell 2014). In Europe, there are established brands of nicotine-infused alcohols as well as nicotine-infused bitters and salt for the construction of cocktails. According to European standards, there are no known biological consequences of infusing nicotine into alcoholic solutions. Therefore, recently developed animal models of concurrent alcohol and nicotine oral consumption are ecologically valid and that validity is increasing in relevance (Hauser et al. 2012b; Kasten et al. 2016).
The United States Food and Drug Administration (FDA) approved varenicline (Var) for smoking cessation in 2006 (Jorenby et al. 2006; Hurt et al. 2018). Var is the most effective monotherapy at increasing the likelihood of smoking abstinence (Gonzales et al. 2006; Jorenby et al. 2006). Pharmacological analyses have indicated multiple sites of action by Var that may mediate the effects on smoking cessation. Var exhibits the strongest affinity for the α4β2 nicotinic acetylcholine receptor (nAChR), where it acts as a partial agonist. Var interacting with this receptor has been postulated to be the mechanism for clinical efficacy. Var is also a less potent full agonist at α7 and α3β4 nAChRs (Rollema et al. 2007; Grady et al. 2010) and a potent full agonist of 5HT3 receptors (Lummis et al. 2011). It is important to note that nicotine has a higher affinity for the 5HT3 receptors than all cholinergic receptors (Gurley and Lanthorn 1998), suggesting maximally efficacious pharmacotherapies for nicotine dependence are likely to involve an interaction with this system as well.
Preliminary clinical data indicated that Var treatment of nicotine-dependent individuals was associated with a decrease in alcohol consumption (Erwin and Slaton 2014). Research conducted with animals and humans have suggested a role for nAChRs in alcohol use disorder (Blomqvist et al. 1993; Chi and de Wit 2003). Activation of the mesocorticolimbic dopamine system by alcohol and the resulting rewarding effects have been consistently shown to involve central nAChR stimulation (Blomqvist et al. 1993; Soderpalm et al. 2000). A more complete examination of decreased alcohol consumption during Var treatment indicated that it was able to decrease alcohol craving (de Bejczy et al. 2015). Conversely, it is important to note that Var failed to decrease overall alcohol drinking compared with placebo-treated individuals (de Bejczy et al. 2015).
Naltrexone (Nal), a nonselective opioid receptor antagonist, has been shown to reduce the reinforcing effects of alcohol as well as cravings associated with alcohol use (Volpicelli et al. 1992; O’Malley et al. 1996; Soyka and Muller 2017). However, these studies also demonstrate the efficacy of Nal is limited. Overall, the efficacy of Nal for the treatment of AUD is equivocal. Nal is effective at treating AUD in a subset of patients (Gueorguieva et al. 2010) while in other patient populations, Nal has very limited effects (c.f., Petrakis et al. 2012). Nal efficacy for the treatment of AUD is further complicated by data reporting only 1 in 10 AUD patients are actually prescribed relevant pharmacotherapy (Thompson et al. 2017). In addition, Nal suffers from low patient adherence (Thompson et al. 2017).
Although nicotine has little or no action on opioid receptors, the utility of using Nal as a treatment for nicotine dependence has been examined. Clinical trials investigating Nal and smoking cessation have demonstrated minor short-term increases in abstinence rates that diminish over time (Covey et al. 1999; King et al. 2012) or no significant difference from placebo (Wong et al. 1999).
Together, AUD and nicotine dependence are the most common comorbid addiction diagnosis (Grant et al. 2004). It has been suggested that the prevalence of AUD and nicotine dependence comorbidity may stem from interconnected mechanisms underlying these particular disorders (Grucza and Bierut 2006). Preclinical studies indicate that the co-abuse of EtOH+NIC can produce unique CNS changes not observed with abuse of either drug separately (Deehan et al. 2015), and combinations of EtOH and NIC can have synergistic CNS rewarding effects (Truitt et al. 2015).
A better understanding of how efficacious therapeutic drugs are during the distinct condition of concurrent consumption is necessary in order to develop better treatments and preventive measures. Research commonly focuses on the effects of pharmacotherapeutics on a single reinforcer despite mounting preclinical evidence that chronic consumption of EtOH and NIC produces unique neuroadaptations that lessen the efficacy of pharmacotherapies designed to treat AUD or nicotine dependence. Recent data examining the effects of varenicline on concurrent intravenous (i.v.) nicotine and oral alcohol has indicated no reduction in self-administration (Maggio et al. 2018a). Therefore, the current experiments examined the effects of Var or Nal on EtOH, NIC, or EtOH+NIC consumption to test the hypothesis that these compounds would be less effective in reducing NIC and EtOH intake, respectively, when co-abused compared with when abused individually.
Materials and methods
Animals
Adult female alcohol-preferring (P) rats from the 74th generation weighing 250–300 g at the start of the experiment were used. Female animals were utilized in the present study due to the long-term nature of the experiments and ability to maintain stable body weights over time. Epidemiological studies also indicate the number of females diagnosed with AUD is increasing in addition to experiencing heightened susceptibility to ethanol injury compared with males (Ceylan-Isik et al. 2010). Additionally, despite fewer females regularly using nicotine products, studies show lower quit rates than males (Smith et al. 2017; Wetter et al. 1999). These differences are among the growing evidence of sex dimorphism in response to EtOH and NIC as well as pharmacotherapies and highlight the importance of examining females in models of co-abuse. Previous research indicated that EtOH intake of female P rats was not significantly altered by the estrus cycle (McKinzie et al. 1998). Rats were maintained on a 12-h reverse light-dark cycle with lights off at 0900. Food and water were available ad libitum throughout the experiment. The animals used in these experiments were maintained in facilities fully accredited by the Association for the Assessment and Accreditation of Laboratory Animal Care (AAALAC). All research protocols were approved by the institutional animal care and use committee and in accordance with the guidelines of the Institutional Care and Use Committee of the National Institute on Drug Abuse, National Institutes of Health, and the Guide for the Care and Use of Laboratory Animals: Eighth Edition (National Research Council, Institute for Laboratory Animal Research, Division on Earth and Life Sciences 2011). The total number of rats (n = 198) used in the current experiments were as follows: Var on water consumption (n = 18, 6/group), Var on EtOH consumption (n = 26, 8–9/group), Var on NIC consumption (n = 23, 7–8/group), Var on EtOH+NIC (n = 27, 9/group), Nal on water consumption (n = 21, 7/group), Nal on EtOH consumption (n = 25, 7–8/group), Nal on NIC consumption (n = 29, 9–10/group), Nal on EtOH+NIC consumption (n = 29, 9–10/group).
Chemical agents and vehicle
Ethyl alcohol (190 proof; McCormick Distilling Co., Weston, MO, USA) was diluted to 15% and 30% with distilled water for oral EtOH consumption. Nicotine HCl was purchased from Sigma (St. Louis, MO, USA). NIC concentrations of 0.07 or 0.14 mg/mL were calculated based on the salt and were added to a solution of 0.0125% saccharin. This was done only for the NIC-alone condition. The EtOH+NIC solutions consisted of 15 or 30% EtOH and 0.14 mg/mL NIC without saccharin added to the solution. Rats will readily consume nicotine solutions at the concentrations employed (about 4.5–5 mg/kg/day). We observe equivalent levels of nicotine self-administration between rats self-administering EtOH+NIC solution and NIC, if saccharin (0.0125%) is added to the NIC solutions (Hauser et al. 2012b). This is reflected in equivalent blood NIC and cotinine levels in these two groups (Hauser et al. 2012b). Moreover, previous research from our group has found no significant differences in neurochemistry or locomotor activity between animals allowed to consume saccharin and water controls (Deehan et al. 2015; Melendez et al. 2002, 2004) and was therefore not included in the present study.
Varenicline tartrate (Sigma) was dissolved in 3% DMSO. Treatment with 2.5–3 mg/kg Var results in locomotor deficits, decreased food intake, and other nonspecific actions (Ortiz et al. 2012; O’Connor et al. 2010; Rollema et al. 2007). Concentrations of Var used in the current experiments were 0, 1, or 2 mg/kg (i.p.). Naltrexone HCl was obtained from Sigma and dissolved in saline. Nal was given in doses of 0, 1, or 10 mg/kg (s.c.). Doses for Nal were determined by previous studies carried out with adolescent and adult P rats demonstrating as much as 20 mg/kg was necessary to decrease EtOH intake while having no impact on water or food consumption (Dhaher et al. 2012; Sable et al. 2006).
Effects of varenicline and naltrexone on EtOH, NIC, and EtOH+NIC maintenance and relapse consumption
Rats were randomly assigned to one of four three-bottle choice drinking conditions illustrated in Fig. 1, top panel. These consisted of (1) water only, (2) EtOH only with concurrent access to 15 and 30% EtOH and water, (3) NIC only with 0.07 and 0.14 mg/mL in 0.0125% saccharin solutions and water, or (4) EtOH+NIC with 15 and 30% EtOH, each containing 0.14 mg/mL NIC, and water. The EtOH-only, NIC-only, and EtOH+NIC groups were given access to the three bottles throughout the experiments of two reinforcing solutions and one water. Despite the development of effective voluntary oral NIC self-administration models (Hauser et al. 2012b; Deehan et al. 2015), i.v. NIC is commonly employed in an attempt to parallel rapid increases in blood NIC levels produced by smoking, which is not observed during the use of chewing tobacco (Benowitz 1988). However, oral tobacco products, such as snus, produce the same rapid increase in blood NIC levels as observed in smokers. There are no significant differences between smokers and first-time snus users in blood NIC levels during the initial 20-min period (Digard et al. 2013). Additionally, there are a number of limitations inherent in i.v. administration that include the need for food restriction, surgery, catheter patency, and overcoming aversion during the initial test sessions. The duration of the present study therefore required the use of an oral consumption model to examine Var or Nal following chronic drug intake.
Top panel: Illustration of the 3-bottle choice paradigm and 4 drinking conditions examined consisting of (1) water only, (2) EtOH only with concurrent access to 15 and 30% EtOH and water, (3) NIC only with 0.07 and 0.14 mg/mL in 0.0125% saccharin solutions and water, or (4) EtOH+NIC with 15 and 30% EtOH, each containing 0.14 mg/mL NIC, and water. Bottom panel: Experimental timeline for the present study to determine the effects of Var (0, 1, or 2 mg/kg) or Nal (0, 1, or 10 mg/kg) injections on maintenance and relapse consumption determined during 4 consecutive treatment days
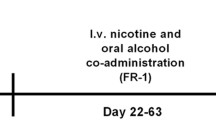
The experimental timeline of the present study is visually represented in the bottom panel of Fig. 1. Rats were given 24-h free-choice access to their assigned solutions for 8 weeks prior to drug testing. Rats were then assigned to two overall groups of Var treated or Nal treated. Var or Nal was administered daily for four consecutive days. Four days of treatment was chosen to allow sufficient time for any additive drug effects, indication of altered efficacy, or behavioral changes to be readily apparent. After the initial Var or Nal treatment period, all rats were allowed 14–20 days of free-choice access to the assigned solutions. All rats were then deprived for 2 weeks of EtOH, NIC, or EtOH+NIC with water constantly available to all rats. Two weeks of deprivation results in an increased amount of EtOH consumption during the initial period of re-exposure (Rodd et al. 2003, 2009; Rodd-Henricks et al. 2001, 2002a, b; Spanagel et al. 1996; Spanagel and Zieglgansberger 1997; Toalston et al. 2008). Similarly, a 2-week deprivation from NIC self-administration results in an increased amount of NIC consumed during re-exposure (Hauser et al. 2012b). The alcohol deprivation effect (ADE) and nicotine deprivation effect (NDE) are valid animal models of drug relapse (Rodd et al. 2003, 2009).
Prior to re-exposure to the previously assigned solution group, rats were again treated with Var or Nal. The doses of Var and Nal were counterbalanced from the initial treatment with respect to past treatment. Specifically, the same subjects used in the Var experiment during the maintenance test were also used during the relapse test for Var. Similarly, for the Nal experiments, the same rats were used for the maintenance and relapse tests. For example, rats treated with 1 mg/kg Nal during the maintenance period were segmented into three groups during the relapse period and received 0, 1, or 10 mg/kg Nal. Var or Nal treatment occurred during the initial 4 days of re-exposure. Additionally, baseline means for maintenance intake were calculated from the last 3 days before Var or Nal treatment and the final three drinking days prior to deprivation for the relapse data.
Solution preference was determined for each subject consuming EtOH and/or NIC daily. The preference of solution consumed has previously been used to examine the reward valence of each solution (Rodd et al. 2003, 2009). With multiple concentrations, statistical analysis of solution preference is complex. It is common to use standard parametric statistics despite preference violating the “independence of measure” assumption of ANOVA/multiple regression analysis and invalidates these statistical tests. Therefore, non-parametric analysis is appropriate. The Kuiper analysis is sensitive to cyclic variations and can be modified to have collection error estimate included in the analysis. However, the general unfamiliarity with this test and the length of the presentation of the data have resulted in preference not being reported for the current study.
Results
Effects of varenicline and naltrexone on water consumption
A repeated measure ANOVA was performed on the average daily water intake (g/kg) of the “water-only” group during “maintenance” consumption in animals treated with Var (Fig. 2, top panel) or Nal (Fig. 2, bottom panel). The analysis revealed that there was a significant Day × Dose interaction term (F16,168 = 5.488; p < 0.001). The interaction term was decomposed by holding “Day” constant and performing individual ANOVAs for each time point. The ANOVAs indicated that there were significant “Dose” differences during the four injection days and the first day post-injection. Post hoc comparisons (Tukey’s b) indicated that consumption of rats in the “water-only” group administered 2 mg/kg Var was reduced compared with saline and 1 mg/kg Var during the four injection days. Conversely, water consumption was enhanced in the 2 mg/kg Var group during the first post-injection day (Fig. 2, top panel). In contrast, Nal treatment did not alter water consumption (Fig. 3, bottom panel; Day, Day × Dose, Dose; p values > 0.05).
Mean (+ SEM) consumption of water in P rats treated with varenicline (top panel) or naltrexone (bottom panel) during maintenance consumption. Asterisk (*) indicates treatment with 2 mg/kg varenicline reduced water consumption compared with saline-treated and 1 mg/kg Val–treated rats. Plus symbol (+) indicates rats previously treated with 2 mg/kg varenicline consumed more water than rats previously treated with saline or 1 mg/kg
Mean (+ SEM) consumption of EtOH in P rats treated with varenicline (top panel) or naltrexone (bottom panel) during maintenance consumption. Asterisk (*) indicates treatment with 1 or 10 mg/kg naltrexone reduced EtOH consumption compared with saline-treated rats, and 1 and 10 mg/kg groups differ from each other. Plus symbol (+) indicates treatment with 1 or 10 mg/kg naltrexone reduced EtOH consumption compared with saline-treated rats
Water animals were never deprived but were treated identically to the other groups. Therefore, there was a water condition to parallel the other “relapse” groups that received a second round of four injection days and received Var or Nal to identify potential nonspecific drug treatment effects (data not shown). In the Var rats, there was a similar Day × Dose interaction term (F16,168 = 3.892; p = 0.005), and post hoc comparisons indicated that 2 mg/kg Var reduced water consumption during all four injection days without a post-injection rebound observed. Again, there was no effect of Nal on water consumption during the “relapse” period (all p values > 0.05).
Effects of varenicline and naltrexone on EtOH consumption
During maintenance testing, Var had no effect on EtOH consumption (Fig. 3; top panel). Statistically, there was no effect of Day, Dose, or Day × Dose interaction (p values > 0.05). In contrast, Nal reduced EtOH consumption during maintenance testing (Fig. 3, bottom panel; Day × Dose interaction, F16,288 = 8.586, p < 0.001). Performing ANOVAs on individual days revealed significant effects of Dose on all four injection days (F2,22 values > 11.404, p values < 0.001). Post hoc comparisons (Tukey’s b) indicated that during the first and fourth injection days, rats treated with 1 or 10 mg/kg Nal consumed less EtOH than saline-treated rats, and the 1 mg/kg Nal group consumed more EtOH than the 10 mg/kg Nal group. EtOH intake recovered to baseline on the first post-injection day.
During EtOH relapse test conditions, Var failed to alter EtOH consumption (Fig. 4, top panel). Statistically, there was a significant effect of Day (F8,184 = 191.65, p < 0.001), but no effect of Dose or Day × Dose interaction (p values > 0.05). These findings forced the analysis to examine the one significant factor (Day), and within-subject comparisons (two-tailed t tests) indicated that EtOH consumption was elevated during the first and second re-exposure day (p < 0.001). In contrast, Nal inhibited the expression of the alcohol deprivation effect (relapse drinking; Day × Dose interaction, F16,176 = 7.756, p < 0.001). Decomposing the significant interaction term by holding Day constant (ANOVAs performed on each day) revealed significant effects of Dose (F2,22 values > 9.493, p values < 0.01) on the first three re-exposure days. On the first and second re-exposure days, post hoc comparisons (Tukey’s b) revealed that all groups were different from each other. During the third re-exposure day, saline-treated and 1 mg/kg Nal–treated rats were significantly different from the 10 mg/kg Nal group. The significant interaction term was also reduced by holding Dose constant, and within-subject (Day) ANOVAs were performed for each Dose group. The analyses revealed that there was a significant “Day” effect in each Dose group (p values < 0.005). In saline-treated rats, within-subject contrasts, two-tailed t tests, revealed that EtOH consumption during the first and second re-exposure days was elevated compared with each baseline intake days (p values < 0.005). In rats treated with 1 mg/kg Nal, there was a significant increase in EtOH consumption only during the first re-exposure day compared with each baseline day (p < 0.01). Treatment with 10 mg/kg Nal not only blocked the expression of the alcohol deprivation effect but also reduced EtOH consumption compared with baseline for the first and second re-exposure days (p values < 0.05).
Mean (+ SEM) consumption of EtOH in P rats treated with varenicline (top panel) or naltrexone (bottom panel) during relapse consumption following a 2-week period of forced abstinence. Baseline means are the final three drinking days prior to the deprivation. Asterisk (*) indicates all varenicline-treated rats consumed more EtOH than baseline intake levels. Plus symbol (+) indicate saline and 1 mg/kg naltrexone–treated rats consumed more EtOH than baseline intake levels, all treatment groups differ from each other, and rats treated with 10 mg/kg naltrexone consumed less EtOH than baseline intake levels. Number sign “#” indicates saline-treated rats consumed more EtOH than baseline intake levels, and all groups are different from each other. Double asterisks (**) indicate EtOH consumption in the 10 mg/kg naltrexone–treated rats is less than that observed in the saline or 1 mg/kg naltrexone–treated rats
Effects of varenicline and naltrexone on nicotine consumption
Var reduced oral NIC consumption during maintenance test conditions (Fig. 5, top panel; Day × Dose interaction, F16,160 = 7.264, p < 0.001). Decomposing the interaction term by examining the effect of Dose on each individual day revealed significant “Dose” differences on the four injection days, and during the second and fourth post-injection days (F2,20 values > 3.774, p values < 0.05). During the four injection days, treatment with 2 mg/kg Var significantly reduced NIC consumption compared with the saline and 1 mg/kg Var groups. Following the termination of Var treatment, NIC consumption was significantly increased during days 2 and 4 of post-injection in the 2 mg/kg Var group compared with saline-treated rats. Nal treatment had no effect on oral NIC consumption (Fig. 5, bottom panel). Statistically, there was no effect of Day, Dose, or Day × Dose interaction (p values > 0.05).
Mean (+ SEM) consumption of NIC in P rats treated with varenicline (top panel) or naltrexone (bottom panel) during maintenance consumption. Asterisk (*) indicates 2 mg/kg varenicline reduced NIC consumption compared with saline and 1 mg/kg varenicline groups. Plus symbol (+) indicates rats previously treated with 2 mg/kg varenicline consumed more NIC that saline controls
A period of forced abstinence resulted in increased oral NIC consumption during the initial period of re-exposure (Fig. 6). Var did alter relapse NIC intake (Fig. 6, top panel, Day × Dose interaction, F = 7.064, p < 0.001). Decomposing the interaction term by holding the factor of Day constant revealed significant effect of Dose during the first three re-exposure days (injection days 1–3; F2,20 values > 3.774, p values < 0.05). Post hoc comparisons (Tukey’s b) indicated that, during the first 3 days of NIC re-exposure, rats treated with 2 mg/kg Var consumed less NIC than the saline-treated and 1 mg/kg Var–treated rats. Alternatively, the significant interaction term was reduced by holding Dose constant and performing repeated measure ANOVAs across Day for each individual treatment group. Rats treated with saline and 1 mg/kg Var consumed significantly more NIC during the first and second re-exposure days compared with baseline (one-way ANOVA, p values < 0.001; two-tailed t tests, p values < 0.032). In contrast, rats treated with 2 mg/kg Var exhibited no significant alteration in NIC consumption across the test period (p = 0.378). In rats treated with Nal, there was no effect of Dose or a Day × Dose interaction (p values > 0.05), but there was a significant effect of Day (F8,208 = 247.68, p < 0.0001). Examining the amount of NIC consumed across days in all treated groups (Fig. 6) revealed that during the first and second re-exposure periods, the amount of NIC consumed was significantly higher than the three baseline days (two-tailed t tests, p values < 0.001).
Mean (+ SEM) consumption of NIC in P rats treated with varenicline (top panel) or naltrexone (bottom panel) during relapse consumption following a 2-week period of forced abstinence. Baseline means are the final three drinking days prior to the deprivation. Asterisk (*) indicates saline and 1 mg/kg varenicline groups are significantly higher from baseline and differ from 2 mg/kg group. Plus symbol (+) indicates saline and 1 mg/kg varenicline groups are different from 2 mg/kg group. Number sign (#) indicates all naltrexone-treated rats consumed more NIC than baseline intake levels
Effects of varenicline and naltrexone on EtOH+nicotine consumption
In general, Var and Nal failed to alter the maintenance consumption of either EtOH or NIC when given concurrently. In Var-treated rats, there were no effects of Day, Dose, or Day × Dose interaction term (p values > 0.05; data not shown) for NIC or EtOH consumption. Similarly, Nal treatment had no effect on co-administration of EtOH+NIC (p values > 0.05).
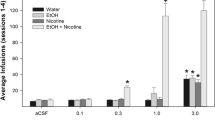
A period of forced EtOH+NIC abstinence produced a prolonged increase in EtOH+NIC consumption that was not altered by Var (Fig. 7) or Nal (Fig. 8) treatment. In Var-treated rats, there was an effect of Day for both NIC and EtOH intake (F8,192 = 239.228 or 208.321, p values < 0.001), but no effect of Dose, or Day × Dose interaction term (p values > 0.05). Examining the effect of Day for both EtOH and NIC consumed for all Var rats revealed that intake for NIC and EtOH was increased during the first four re-exposure days (two-tailed t tests, p values < 0.001). In Nal-treated rats, there was an effect of Day for both NIC and EtOH intake (F8,208 = 219.795 or 175.024, p values < 0.001), but no effect of Dose or Day × Dose interaction term (p values > 0.05). Defining the effect of Day was performed by contrasting the overall average intake for a re-exposure day to that observed during the third baseline day with two-tailed t tests. The analyses indicated that NIC consumption was elevated during the first four re-exposure days (p values < 0.001), and EtOH consumption was elevated for the first five re-exposure days which included the first post-injection day (p values < 0.01).
Mean (+ SEM) consumption of concurrently available NIC (top panel) and EtOH (bottom panel) in P rats treated with varenicline following a period of 2 weeks of forced abstinence. Baseline means are the final three drinking days prior to the deprivation. Overall, the data indicate varenicline was ineffective at reducing EtOH+NIC consumption during relapse drinking. Asterisk (*) indicates NIC consumption was higher in all groups compared with baseline intake. Plus symbol (+) indicates EtOH consumption was higher in all groups compared with baseline intake
Mean (+ SEM) consumption of concurrently available NIC (top panel) and EtOH (bottom panel) in P rats treated with naltrexone following a period of 2 weeks of forced abstinence. Baseline means are the final three drinking days prior to the deprivation. Overall, the data indicate naltrexone was ineffective at reducing EtOH+NIC consumption during relapse drinking. Asterisk (*) indicates NIC consumption was higher in all groups compared with baseline intake. Plus symbol (+) indicates EtOH consumption was higher in all groups compared with baseline intake
Discussion
Overall, the data indicate the two prototypical pharmacotherapeutics for AUD and nicotine dependence were efficacious at reducing, to a degree, the ongoing consumption of the corresponding drug of abuse (Figs. 3, 4, 5, and 6). In contrast, Var and Nal had no effect on reducing the intake of the non-indicated drug of abuse (e.g., Nal on NIC intake; Figs. 3, 4, 5, and 6) or on any aspect of EtOH+NIC co-use (Figs. 7 and 8).
The current experiments examined relapse using the ADE model and a similar NDE model. ADE has been postulated to mimic the increase in alcohol consumption observed following periods of abstinence in humans and animals (Rodd et al. 2003). The ADE model is associated with adaptations in the posterior ventral tegmental area (pVTA) that enhance EtOH reward (Rodd et al. 2005). The NDE has not been examined extensively in the literature since standard i.v. NIC self-administration precludes the testing of chronic nicotine self-administration due to the limited duration of catheter patency. The current data sets indicate that under 24-h free-choice oral drinking conditions, NIC intake is enhanced following a period of deprivation (Figs. 6, 7, and 8). However, studies have not examined NIC reinforcement in the pVTA following a period of deprivation to determine if neuroadaptations have developed that would augment the reinforcing properties of NIC. The lack of basic research addressing NDE mechanisms supports the need to expand on the present study and identify such changes to understand relevant nicotine consummatory behaviors. Similar to past research, relapse EtOH+NIC consumption was significantly greater and prolonged than that in rats consuming EtOH or NIC alone (compare Figs. 7 and 8 with Figs. 4 and 6; Hauser et al. 2012b). It is likely that EtOH+NIC co-abuse may augment neuroadaptations produced by periods of drug abstinence or produce unique neuroadaptations not observed following intake of EtOH or NIC (Deehan et al. 2015).
The current data sets indicate that Var can reduce ongoing and relapse NIC intake (Figs. 5 and 6). It is important to note that rats treated with high doses of Var consumed significant amounts of NIC during the 24-h periods of NIC re-exposure at approximately 6 mg/kg (Fig. 6). Nal had no effect on NIC relapse drinking and all treated groups displayed similar amounts of NIC intake. The data indicate that Nal, but not Var, can reduce EtOH relapse drinking (Fig. 4). The efficacy of Nal to reduce EtOH drinking is altered during relapse conditions. The lower dose of Nal (1 mg/kg) produced a similar reduction in EtOH consumption during ongoing EtOH consumption testing as the higher dose (10 mg/kg; Fig. 3). However, during relapse testing, rats administered 1 mg/kg Nal displayed a blunted ADE that was significantly more than drinking baseline and 10 mg/kg Nal (Fig. 4). Previous research indicated that the efficacy of Nal to reduce EtOH self-administration is decreased under relapse conditions (Dhaher et al. 2012) and the ADE is associated with alterations in the mesolimbic opioid system (Breese et al. 2005). In rats with a history of EtOH+NIC co-abuse, Nal and Var failed to alter relapse co-administration of the two compounds (Figs. 7 and 8), suggesting some unique CNS neuronal changes may have occurred with co-abuse that is not found with the individual abuse of EtOH or NIC.
Previous research indicated that treatment with Var significantly reduced NIC self-administration from mean baseline levels during maintenance and relapse phases of drug intake (Funk et al. 2016; O’Connor et al. 2010; Scuppa et al. 2015). Additional reports support these results but utilized doses > 2 mg/kg Var and therefore, nonspecific motor inhibitory effects cannot be excluded (George et al. 2011; Maggio et al. 2018a). Although 2 mg/kg Var modestly decreased water intake in the “water-only” condition (Fig. 2), it is important to note that preference for water and overall fluid consumption in the other three groups was not altered and remained over 100 g/kg/day. This suggests the potential nonspecific effects of Var at this dose on water consumption were minor and counteracted in the presence of reinforcers.
EtOH drinking was found to be unaltered following treatment with Var consistent with recent reports (Funk et al. 2016; Maggio et al. 2018a, b; Randall et al. 2015; Scuppa et al. 2015). However, some studies examining Var and EtOH intake appear to conflict with the present findings. For example, treatment with 2 mg/kg Var reduced EtOH self-administration to ~ 1.5 g/kg/2-h session following scheduled access and repeated cycles of deprivation (Froehlich et al. 2016, 2017; Czachowski et al. 2018). A number of factors contribute to these differences. The current experiments examined the effects of Var following more than 8 weeks of continuous access to EtOH versus 4 weeks of 2 h/day limited access. The extended EtOH access period could have allowed time to establish lasting adaptations that occur following chronic drinking that decreased the effectiveness of Var compared with animals with less EtOH experience. The previous study notes the importance of maintaining sufficient levels of Var in the blood in order for treatment to remain effective. The current data indicate that administration of 2 mg/kg Var reduces water consumption for a 24-h period (Fig. 2). Therefore, despite the inhibitory gustatory actions of the high dose of Var for 24 h, there was no effect on EtOH consumption.
Two studies applying limited but free access to EtOH have also shown some effectiveness of Var in reducing EtOH self-administration (Holgate et al. 2017; Steensland et al. 2007). A significant reduction in EtOH drinking following Var treatment was found at 2 h (but not at 4 h) during a 4-h drinking in the dark paradigm but was not evident at the conclusion of the session (Holgate et al. 2017). The significant decrease at 2 h could be attributed to the small amount of EtOH being consumed under this study design (blood alcohol concentrations were relatively low with an average of 24 ± 5 mg%; Holgate et al. 2017). This level of EtOH self-administration is likely affected more by Var treatment, in agreement with their previous work, than animals in the present study consuming approximately 6.5 g/kg/day (Steensland et al. 2007).
The current experiments support previous evidence demonstrating the ability of Nal to reduce EtOH drinking (Dhaher et al. 2012; Froehlich et al. 2016; Lê et al. 2014; Steensland et al. 2007). Additionally, results from this study indicated no significant changes to NIC intake when treated with Nal (Lê et al. 2014). This agrees with earlier work involving both animal models and clinical trials. Research examining the impact of only naltrexone on smoking cessation demonstrated very limited (Covey et al. 1999) or no effect at all (Wong et al. 1999). Opioid antagonists are known to enhance nicotine withdrawal in nicotine-dependent animals (Malin et al. 1993, 1996; Biala et al. 2005). For this reason, clinical trials investigating naltrexone and smoking cessation may involve augmentation of treatment with nicotine replacement therapy (NRT) to alleviate some nicotine withdrawal symptoms (O’Malley et al. 2006; Toll et al. 2010). A meta-analysis carried out on naltrexone and smoking cessation that included eight separate trials and 1213 participants concluded that there was no positive effect of naltrexone alone or in combination with NRT on short-term or long-term smoking abstinence (David et al. 2014).
The reality of AUD is that it is not a single drug addiction disease. Most cases of AUD are a polysubstance syndrome and are thus much more complicated than those arising from the use of alcohol alone. Ignoring the polysubstance characteristic of AUD limits our knowledge of the disease and greatly reduces the ability to establish functional treatments. Preclinical studies clearly indicated that acute exposure to EtOH and NIC results in unique responses that are not observed following an acute exposure to EtOH or NIC. The pVTA is a site where pharmacologically relevant levels of both NIC and EtOH can produce reinforcing effects (Exley et al. 2011; Hauser et al. 2014; Truitt et al. 2015; Rodd-Henricks et al. 2000). The pVTA is a site that regulates oral EtOH (Hodge et al. 1993; Rodd et al. 2010) and i.v. NIC (Corrigall et al. 1994) self-administration and is a site where EtOH and NIC can interact synergistically (Truitt et al. 2015). Intra-VTA injections of NIC can enhance dopamine release in the nucleus accumbens shell (AcbSh) produced by systemic administration of EtOH (Tizabi et al. 2002). Rats will self-administer EtOH and NIC directly into the pVTA in a synergistic manner. Furthermore, equivalent microinjections of EtOH+NIC directly into the pVTA result in significant alterations to gene expression in the AcbSh, which includes bdnf, gdnf, and homer2 than either EtOH or NIC alone (Truitt et al. 2015).
Chronic EtOH+NIC co-use/abuse also results in unique neuroadaptations throughout the brain. The oral EtOH+NIC model of self-administration results in equivalent consumption of EOH and NIC in the solo- and poly-drug exposure groups (Hauser et al. 2012b). In the AcbSh, chronic EtOH+NIC self-administration results in enhancement of NIC reward that is not observed in rats consuming equivalent amounts of EtOH or NIC (Deehan et al. 2015). In the medial prefrontal cortex, EtOH+NIC co-use/abuse resulted in a threefold increase in basal glutamate extracellular levels while comparable consumption of EtOH or nicotine had no effect (Deehan et al. 2015). The unique neuroadaptations of chronic EtOH+NIC self-administration could be the biological basis for the pharmacological results reported herein.
The present study indicated there was no effect of Var or Nal treatment on EtOH+NIC maintenance or relapse self-administration. The significant reductions of EtOH consumption by Nal treatment and NIC intake by Var treatment are no longer evident when both reinforcers are presented together. This is consistent with preclinical research from our lab and others demonstrating that acute and chronic exposure to EtOH+NIC results in neuronal alterations specific to co-administration that are not observed with either drug alone (Clark and Little 2004; Deehan et al. 2015; Lé et al. 2014; Tizabi et al. 2002, 2007; Truitt et al. 2015). Similar to the current data set, in P rats concurrently self-administering i.v. NIC and oral EtOH, Var and other smoking cessation agents failed to alter EtOH or NIC consumption (Maggio et al. 2018a). The failure of Var and Nal, as well as the specific α6β2* antagonist r-bPiDI, to alter concurrent oral EtOH and i.v. NIC self-administration has been replicated in a novel model that increases intake levels of both drugs (Maggio et al. 2018b). Therefore, consistent preclinical data has indicated that Var is not effective at reducing EtOH+NIC co-administration.
Despite the disproportionately high rate of EtOH and NIC comorbid abuse, the prevailing pharmacotherapeutic strategy has been to develop treatments that target EtOH or NIC use as separate conditions. This approach has resulted in an inadequate number of approved pharmacological treatment options that, overall, have only demonstrated limited success. For example, a number of meta-analyses revealed that Nal does not increase abstinence rates or decrease the risk of relapse to heavy alcohol drinking. However, the delay to initiation of drinking was increased as well as the total number of days abstinent prior to relapse (Maisel et al. 2013; Jonas et al. 2014; Donoghue et al. 2015). Furthermore, despite FDA approval for Var in 2006, overall smoking cessation rates at the population level in the USA have not risen in over two decades (Zhu et al. 2012). This appears to contradict expected results following dispensing of more than 2.1 million Var prescriptions per year and numerous randomized controlled trials demonstrating the effectiveness of Var (Gonzales et al. 2006; Jorenby et al. 2006; Bolliger et al. 2011; Zhu et al. 2012; Baker et al. 2016; Motschman et al. 2016). These outcomes could in part be explained by the ability of Var clinical trials to recruit nicotine-dependent individuals into abstinence but fail to prevent instances of relapse over placebo-treated smokers (Agboola et al. 2015). Examination of AUDs and nicotine dependence separately in preclinical research and during clinical trials has resulted in approved therapeutics of Nal and Var with relapse rates at greater than one third of patients at a 6-month follow-up and up to 75% at 1 year, respectively (Jorenby et al. 2006; Volpicelli et al. 1997).
The current study demonstrates the failure of Var or Nal to reduce EtOH+NIC consumption. However, potential limitations to the above model should be considered when evaluating these findings. First, future studies should examine the impact of Var or Nal treatment on EtOH+NIC intake when presented separately in the three-bottle choice drinking paradigm, rather than in a combined solution. This would provide further insight into the effect of Var or Nal on their respective reinforcers. When presented together, potential reductions in just EtOH or NIC intake during treatment would be highlighted that otherwise could be obscured with the combined solution paradigm. Second, increasing the number of Var or Nal treatment days would provide additional time for the blood levels of each therapeutic to stabilize. Finally, the inclusion of measurements taken at specific time points during 24-h access would be beneficial. A better representation of drinking behavior during Var or Nal treatment could be determined with data collection points at 2, 4, and 6 h post-treatment.
These results indicate that the standard pharmacological treatments for nicotine dependence or AUD were effective at reducing the consumption of a single targeted drug but neither reduced the amount of EtOH+NIC consumed. Overall, the findings suggest that failures to develop successful treatment for comorbid AUD and nicotine dependence may result from limitations in models used to develop such treatments, specifically through a failure to address the unique neuroadaptations produced by co-use of these drugs. Continued refinement of the preclinical co-abuse model described herein will be invaluable in the pursuit of assessing future pharmacotherapies for the treatment of heavy alcohol drinking smokers.
References
Agboola SA, Coleman T, McNeill A, Leonardi-Bee J (2015) Abstinence and relapse among smokers who use varenicline in a quit attempt-a pooled analysis of randomized controlled trials. Addiction 110(7):1182–1193
Baker TB, Piper ME, Stein JH, Smith SS, Bolt DM, Fraser DL, Fiore MC (2016) Effects of nicotine patch vs varenicline vs combination nicotine replacement therapy on smoking cessation at 26 weeks: A randomized clinical trial. JAMA 315(4):371–379
Benowitz NL (1988) Pharmacologic aspects of cigarette smoking and nicotine addiction. N Engl J Med 319:1318–1330
Biala G, Budzynska B, Kruk M (2005) Naloxone precipitates nicotine abstinence syndrome and attenuates nicotine-induced antinociception in mice. Pharmacol Rep 57(6):755–760
Blomqvist O, Engel JA, Nissbrandt H, Soderpalm B (1993) The mesolimbic dopamine-activating properties of ethanol are antagonized by mecamylamine. Eur J Pharmacol 249:207–213
Breese GR, Chu K, Dayas CV, Funk D, Knapp DJ, Koob GF, Lê DA, O’Dell LE, Overstreet DH, Roberts AJ, Sinha R, Valdez GR, Weiss F (2005) Stress enhancement of craving during sobriety: a risk for relapse. Alcohol Clin Exp Res 29(2):185–195
Ceylan-Isik AF, McBride SM, Ren J (2010) Sex difference in alcoholism: who is at a greater risk for development of alcoholic complication? Life Sci 87:133–138
Chi H, de Wit H (2003) Mecamylamine attenuates the subjective stimulant-like effects of alcohol in social drinkers. Alcohol Clin Exp Res 27:780–786
Clark A, Little HJ (2004) Interactions between low concentrations of ethanol and nicotine on firing rate of ventral tegmental dopamine neurones. Drug Alcohol Depend 75(2):199–206
Corrigall WA, Coen KM, Adamson KL (1994) Self-administered nicotine activates the mesolimbic dopamine system through the ventral tegmental area. Brain Res 653(1–2):278–284
Covey LS, Glassman AH, Stetner F (1999) Naltrexone effects on short-term and long-term smoking cessation. J Addict Dis 18(1):31–40
Czachowski CL, Froehlich JC, DeLory M (2018) The effects of long-term varenicline administration on ethanol and sucrose seeking and self-administration in male P rats. Alcohol Clin Exp Res 42(2):453–460
Daeppen JB, Smith TL, Danko GP, Gordon L, Landi NA, Nurnberger JI, Bucholz KK, Raimo E, Schuckit MA (2000) Clinical correlates of cigarette smoking and nicotine dependence in alcohol-dependent men and women. Alcohol Alcohol 35(2):171–175
David SP, Chu IM, Lancaster T, Stead LF, Evins AE, Prochaska JJ (2014) Systematic review and meta-analysis of opioid antagonists for smoking cessation. BMJ Open 4(3):e004393
de Bejczy A, Löf E, Walther L, Guterstam J, Hammarberg A, Asanovska G, Franck J, Isaksson A, Söderpalm B (2015) Varenicline for treatment of alcohol dependence: a randomized, placebo-controlled trial. Alcohol Clin Exp Res 39(11):2189–2199
Deehan GJ, Hauser SR, Waeiss RA, Knight CP, Toalston JE, Truitt WA, McBride WJ, Rodd ZA (2015) Co-administration of ethanol and nicotine: the enduring alterations in the rewarding properties of nicotine and glutamate activity within the mesocorticolimbic system of female alcohol-preferring (P) rats. Psychopharmacology 232(23):4293–4302
Delnevo CD, Wackowski OA, Giovenco DP, Manderski MT, Hrywna M, Ling PM (2012) Examining market trends in the United States smokeless tobacco use: 2005–2011. Tob Control
Dhaher R, Toalston JE, Hauser SR, Bell RL, McKinzie DL, McBride WJ, Rodd ZA (2012) Effects of naltrexone and LY255582 on ethanol maintenance, seeking, and relapse responding by alcohol-preferring (P) rats. Alcohol 46(1):17–27
DiFranza JR, Guerrera MP (1990) Alcoholism and smoking. J Stud Alcohol 51(2):130–135
Digard H, Errington G, Richter A, McAdams K (2009) Patterns and behaviors of snus consumption in Sweden. Nicotine Tob Res 11:1175–1181
Digard H, Proctor C, Kulasekaran A, Malmqvist U, Richter A (2013) Determination of nicotine absorption from multiple tobacco products and nicotine gum. Nicotine Tob Res 15(1):255–261
Donoghue K, Elzerbi C, Saunders R, Whittington C, Pilling S, Drummond C (2015) The efficacy of acamprosate and naltrexone in the treatment of alcohol dependence, Europe versus the rest of the world: a meta-analysis. Addiction 110(6):920–930
Erwin BL, Slaton RM (2014) Varenicline in the treatment of alcohol use disorders. Ann Pharmacother 48(11):1445–1455
Exley R, Maubourguet N, David V, Eddine R, Evrard A, Pons S, Marti F, Threlfell S, Cazala P, McIntosh JM, Changeux JP, Maskos U, Cragg SJ, Faure P (2011) Distinct contributions of nicotinic acetylcholine receptor subunit alpha4 and subunit alpha6 to the reinforcing effects of nicotine. Proc Natl Acad Sci U S A 108(18):7577–7582
Froehlich JC, Fischer SM, Dilley JE, Nicholson ER, Smith TN, Filosa NJ, Rademacher LC (2016) Combining varenicline (Chantix) with naltrexone decreases alcohol drinking more effectively than does either drug alone in a rodent model of alcoholism. Alcohol Clin Exp Res 40(9):1961–1970
Froehlich JC, Nicholson ER, Dilley JE, Filosa NJ, Rademacher LC, Smith TN (2017) Varenicline reduces alcohol intake during repeated cycles of alcohol reaccess following deprivation in alcohol-preferring (P) rats. Alcohol Clin Exp Res 41(8):1510–1517
Funk D, Lo S, Coen K, Lê AD (2016) Effects of varenicline on operant self-administration of alcohol and/or nicotine in a rat model of co-abuse. Behav Brain Res 296:157–162
George O, Lloyd A, Carroll FI, Damaj MI, Koob GF (2011) Varenicline blocks nicotine intake in rats with extended access to nicotine self-administration. Psychopharmacology 213(4):715–722
Gonzales D, Rennard SI, Nides M, Oncken C, Azoulay S, Billing CB, Watsky EJ, Gong J, Williams KE, Reeves KR (2006) Varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, vs sustained-release bupropion and placebo for smoking cessation: a randomized controlled trial. JAMA. 296(1):47–55
Grady SR, Drenan RM, Breining SR, Yohannes D, Wageman CR, Fedorov NB, McKinney S, Whiteaker P, Bencherif M, Lester HA, Marks MJ (2010) Structural differences determine the relative selectivity of nicotinic compounds for native α4β2*-, α6β2*-, α3β4*- and α7-nicotinic acetylcholine receptors. Neuropharmacology 58(7):1054–1066
Grant B, Hasin D, Chou S, Stinson F, Dawson D (2004) Nicotine dependence and psychiatric disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry 61(11):1107–1115
Grucza R, Bierut L (2006) Co-occurring risk factors for alcohol dependence and habitual smoking: update on findings from the Collaborative Study on the Genetics of Alcoholism. Alcohol Res Health 29(3):172–178
Gueorguieva R, Wu R, Donovan D, Rounsaville BJ, Couper D, Krystal JH, O’Malley SS (2010) Naltrexone and combined behavioral intervention effects on trajectories of drinking in the COMBINE study. Drug Alcohol Depend 107(2–3):221–229
Gulliver S, Rohsenow DJ, Colby SM, Dey AN, Abrams DB, Niaura RS, Monti PM (1995) Interrelationship of smoking and alcohol dependence, use and urges to use. J Stud Alcohol 56(2):202–206
Gurley DA, Lanthorn TH (1998) Nicotinic agonists competitively antagonize serotonin at mouse 5-HT3 receptors expressed in Xenopus oocytes. Neurosci Lett 247(2–3):107–110
Hauser SR, Getachew B, Oster SM, Dhaher R, Ding ZM, Bell RL, McBride WJ, Rodd ZA (2012a) Nicotine modulates alcohol-seeking and relapse by alcohol-preferring (P) rats in a time-dependent manner. Alcohol Clin Exp Res 36(1):43–54
Hauser SR, Katner SN, Deehan GA Jr, Ding ZM, Toalston JE, Scott BJ, Bell RL, McBride WJ, Rodd ZA (2012b) Development of an oral operant nicotine/ethanol co-use model in alcohol-preferring (P) rats. Alcohol Clin Exp Res 36:1963–1972
Hauser SR, Bracken AL, Deehan GA, Toalston JE, Ding ZM, Truitt WA, Bell RL, McBride WJ, Rodd ZA (2014) Selective breeding for high alcohol preference increases the sensitivity of the posterior VTA to the reinforcing effects of nicotine. Addict Biol 19(5):800–811
Hodge CW, Haraguchi M, Erickson H, Samson HH (1993) Ventral tegmental microinjections of quinpirole decrease ethanol and sucrose-reinforced responding. Alcohol Clin Exp Res 17(2):370–375
Holgate JY, Shariff M, Mu EH, Bartlett S (2017) A rat drinking in the dark model for studying ethanol and sucrose consumption. Front Behav Neurosci 11:29
Hurt RT, Ebbert JO, Croghan IT, Schroeder DR, Hurt RD, Hays JT (2018) Varenicline for tobacco-dependence treatment in alcohol-dependent smokers: a randomized controlled trial. Drug Alcohol Depend 184:12–17
John U, Hill A, Rumpf H, Hapke U, Meyer C (2003a) Alcohol high risk drinking, abuse and dependence among tobacco smoking medical care patients and the general population. Drug Alcohol Depend 69(2):189–195
John U, Rumpf H, Hanke M, Gerke P, Hapke U (2003b) Estimation of tobacco- or alcohol-attributable disease rates in national hospital care: an approach based on routine in-patient disease register data and systematic diagnosis of alcohol use disorders. Alcohol Alcohol 38(4):339–346
Jonas DE, Amick HR, Feltner C, Bobashev G, Thomas K, Wines R, Kim MM, Shanahan E, Gass CE, Rowe CJ, Garbutt JC (2014) Pharmacotherapy for adults with alcohol use disorders in outpatient settings: a systematic review and meta-analysis. Jama 311(18):1889–1900
Jorenby DE, Hays JT, Rigotti NA, Azoulay S, Watsky EJ, Williams KE, Billing CB, Gong J, Reeves KR (2006) Efficacy of varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, vs placebo or sustained-release bupropion for smoking cessation: a randomized controlled trial. JAMA 296(1):56–63
Kasten CR, Frazee AM, Boehm SL 2nd (2016) Developing a model of limited-access nicotine consumption in C57Bl/6J mice. Pharmacol Biochem Behav 148L:28–37
King A, Cao D, O’Malley S, Kranzler H, Cai X, deWit H, Matthews A, Stachoviak R (2012) Effects of naltrexone on smoking cessation outcomes and weight gain in nicotine-dependent men and women. J Clin Psychopharmacol 32(5):630–636
Lajtha A, Sershen H (2010) Nicotine: alcohol reward interactions. Neurochem Res 35:1248–1258
Lê AD, Funk D, Lo S, Coen K (2014) Operant self-administration of alcohol and nicotine in a preclinical model of co-abuse. Psychopharmacology 231(20):4019–4029
Lummis SC, Thompson AJ, Bencherif M, Lester HA (2011) Varenicline is a potent agonist of the human 5-hydroxytryptamine3 receptor. J Phamacol Exp Ther 339:125–131
Maggio SE, Saunders MA, Baxter TA, Nixon K, Prendergast MA, Zheng G, Crooks P, Dwoskin LP, Slack RD, Newman AH, Bell RL, Bardo MT (2018a) Effects of the nicotinic agonist varenicline, nicotinic antagonist r-bPiDI, and DAT inhibitor (R)-modafinil on co-use of ethanol and nicotine in female P rats. Psychopharmacology 235(5):1439–1453
Maggio SE, Saunders MA, Nixon K, Prendergast MA, Zheng G, Crooks P, Dwoskin LP, Bell RL, Bardo MT (2018b) An improved model of ethanol and nicotine co-use in female P rats: effects of naltrexone, varenicline, and the selective nicotinic α6β2* antagonist r-bPiDI. Drug Alcohol Depend 193:154–161
Maisel NC, Blodgett JC, Wilbourne PL, Humphreys K, Finney JW (2013) Meta-analysis of naltrexone and acamprosate for treating alcohol use disorders: when are these medications most helpful? Addiction 108(2):275–293
Malin DH, Lake JR, Carter VA, Cunningham JS, Wilson OB (1993) Naloxone precipitates nicotine abstinence syndrome in the rat. Psychopharmacology 112(2–3):339–342
Malin DH, Lake JR, Payne MC, Short PE, Carter VA, Cunningham JS, Wilson OB (1996) Nicotine alleviation of nicotine abstinence syndrome is naloxone-reversible. Pharmacol Biochem Behav 53(1):81–85
Martell N (2014) Tobacco returns to the bar, this time inside cocktails. National Public Radio. Retrieved from https://www.npr.org/
McKinzie DL, Nowak KL, Yorger L, McBride WJ, Murphy JM, Lumeng L, Li T-K (1998) The alcohol deprivation effect in the alcohol-preferring P rat under free drinking and operant access conditions. Alcohol Clin Exp Res 22:1170–1176
Melendez RI, Rodd-Henricks ZA, Engleman EA, Li TK, McBride WJ, Murphy JM (2002) Microdialysis of dopamine in the nucleus accumbens of alcohol-preferring (P) rats during anticipation and operant self-administration of ethanol. Alcohol Clin Exp Res 26:318–325
Melendez RI, Rodd ZA, McBride WJ, Murphy JM (2004) Involvement of the mesopallidal dopamine system in ethanol reinforcement. Alcohol 32:137–144
Motschman CA, Gass JC, Wray JM, Germeroth LJ, Schlienz NJ, Munoz DA, Moore FE, Rhodes JD, Hawk LW, Tiffany ST (2016) Selection criteria limit generalizability of smoking pharmacotherapy studies differentially across clinical trials and laboratory studies: a systematic review on varenicline. Drug Alcohol Depend 169:180–189
National Research Council (2011) Guide for the care and use of laboratory animals, 8th edn. The National Academies Press, Washington, DC
New York Times Magazine (Marshall Selladec) (2003) The 3rd Annual Year in Ideas; Nicotini, The. Published Dec 14, 2003
O’Connor EC, Parker D, Rollema H, Mead AN (2010) The α4β2 nicotinic acetylcholine-receptor partial agonist varenicline inhibits both nicotine self-administration following repeated dosing and reinstatement of nicotine seeking in rats. Psychopharmacology 208(3):365–376
O’Malley SS, Jaffe AJ, Rode S, Rounsaville BJ (1996) Experience of a “slip” among alcoholics treated with naltrexone or placebo. Am J Psychiatry 153(2):281–283
O’Malley SS, Cooney JL, Krishnan-Sarin S, Dubin JA, McKee SA, Cooney NL, Blakeslee A, Meandzija B, Romano-Dahlgard D, Wu R, Makuch R, Jatlow P (2006) A controlled trial of naltrexone augmentation of nicotine replacement therapy for smoking cessation. Arch Intern Med 166(6):667–674
Ortiz NC, O’Neill HC, Marks MJ, Grady SR (2012) Varenicline blocks β2*-nAChR-mediated response and activates β4*-nAChR-mediated responses in mice in vivo. Nicotine Tob Res 14(6):711–719
Petrakis I, Ralevski E, Desai N, Trevisan L, Gueorguieva R, Rounsaville B, Krystal J (2012) Noradrenergic vs serotonergic antidepressant with or without naltrexone for veterans with PTSD and comorbid alcohol dependence. Neuropsychopharmacology 37(4):996–1004
Randall PA, Jaramillo AA, Frisbee S, Besheer J (2015) The role of varenicline on alcohol-primed self-administration and seeking behavior in rats. Psychopharmacology 232(14):2443–2454
Rodd ZA, Bell RL, Kuc KA, Murphy JM, Lumeng L, Li TK, McBride WJ (2003) Effects of repeated alcohol deprivations on operant ethanol self-administration by alcohol-preferring (P) rats. Neuropsychopharmacology 28:1614–1621
Rodd ZA, Bell RL, McQueen VK, Davids MR, Hsu CC, Murphy JM, Li TK, Lumeng L, McBride WJ (2005) Prolonged increase in the sensitivity of the posterior ventral tegmental area to the reinforcing effects of ethanol following repeated exposure to cycles of ethanol access and deprivation. J Pharmacol Exp Ther 315(2):648–657
Rodd ZA, Bell RL, Kuc KA, Murphy JM, Lumeng L, McBride WJ (2009) Effects of concurrent access to multiple ethanol concentrations and repeated deprivations on alcohol intake of high-alcohol-drinking (HAD) rats. Addict Biol 14:152–164
Rodd ZA, Bell RL, Oster SM, Toalston JE, Pommer TJ, McBride WJ, Murphy JM (2010) Serotonin-3 receptors in the posterior ventral tegmental area regulate ethanol self-administration of alcohol-preferring (P) rats. Alcohol 44(3):245–255
Rodd-Henricks ZA, McKinzie DL, Crile RS, Murphy JM, McBride WJ (2000) Regional heterogeneity for the intracranial self-administration of ethanol within the ventral tegmental area of female Wistar rats. Psychopharmacology 149:217–224
Rodd-Henricks ZA, Bell RL, Kuc KA, Murphy JM, McBride WJ, Lumeng L, Li TK (2001) Effects of concurrent access to multiple ethanol concentrations and repeated deprivations on alcohol intake of alcohol-preferring rats. Alcohol Clin Exp Res 25:1140–1150
Rodd-Henricks ZA, Bell RL, Kuc KA, Murphy JM, McBride WJ, Lumeng L, Li TK (2002a) Effects of ethanol exposure on subsequent acquisition and extinction of ethanol self-administration and expression of alcohol-seeking behavior in adult alcohol-preferring (P) rats: I. Periadolescent exposure. Alcohol Clin Exp Res 26:1632–1641
Rodd-Henricks ZA, Bell RL, Kuc KA, Murphy JM, McBride WJ, Lumeng L, Li TK (2002b) Effects of ethanol exposure on subsequent acquisition and extinction of ethanol self-administration and expression of alcohol-seeking behavior in adult alcohol-preferring (P) rats: II. Adult exposure. Alcohol Clin Exp Res 26:1642–1652
Rollema H, Chambers LK, Coe JW, Glowa J, Hurst RS, Lebel LA, Lu Y, Mansbach RS, Mather RJ, Rovetti CC, Sands SB, Schaeffer E, Schulz DW, Tingley FI, Williams KE (2007) Pharmacological profile of the α4β2 nicotinic acetylcholine receptor partial agonist varenicline, an effective smoking cessation aid. Neuropharmacology 52(3):985–994
Sable HJ, Bell RL, Rodd ZA, McBride WJ (2006) Effects of naltrexone on the acquisition of alcohol intake in male and female periadolescent and adult alcohol-preferring (P) rats. Int J Adolesc Med Health 18:139–149
Scuppa G, Cippitelli A, Toll L, Ciccocioppo R, Ubaldi M (2015) Varenicline decreases nicotine but not alcohol self-administration in genetically selected Marchigian Sardinian alcohol-preferring (msP) rats. Drug Alcohol Depend 156:126–132
Smith PH, Weinberger AH, Zhang J, Emme E, Mazure CM, McKee SA (2017) Sex differences in smoking cessation pharmacotherapy comparative efficacy: a network meta-analysis. Nicotine Tob Res 19(3):273–281
Soderpalm B, Ericson M, Olausson P, Blomqvist O, Engel JA (2000) Nicotinic mechanisms involved in the dopamine activating and reinforcing properties of ethanol. Behav Brain Res 113:85–96
Soyka M, Müller CA (2017) Pharmacotherapy of alcoholism - an update on approved and off-label medications. Expert Opin Pharmacother 18(12):1187–1199
Spanagel R, Zieglgansberger W (1997) Anti-craving compounds for ethanol: new pharmacological tools to study addictive processes. Trends Pharmacol Sci 18:54–59
Spanagel R, Hölter SM, Allingham K, Landgraf R, Zieglgänsberger W (1996) Acamprosate and alcohol: I. Effects on alcohol intake following alcohol deprivation in the rat. Eur J Pharmacol 305(1–3):39–44
Steensland P, Simms JA, Holgate J, Richards JK, Bartlett SE (2007) Varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, selectively decreases ethanol consumption and seeking. Proc Natl Acad Sci U S A 104(30):12518–12523
Thompson A, Ashcroft DM, Owens L, van Staa TP, Pirmohamed M (2017) Drug therapy for alcohol dependence in primary care in the UK: a Clinical Practice Research Datalink study. PLoS One 12(3):1–14
Tizabi Y, Copeland RJ, Louis VA, Taylor RE (2002) Effects of combined systemic alcohol and central nicotine administration into ventral tegmental area on dopamine release in the nucleus accumbens. Alcohol Clin Exp Res 26(3):394–399
Tizabi Y, Bai L, Copeland RJ, Taylor RE (2007) Combined effects of systemic alcohol and nicotine on dopamine release in the nucleus accumbens shell. Alcohol Alcohol 42(5):413–416
Toalston JE, Oster SM, Kuc KA, Pommer TJ, Murphy JM, Lumeng L, Bell RL, McBride WJ, Rodd ZA (2008) Effects of alcohol and saccharin deprivations on concurrent ethanol and saccharin operant self-administration by alcohol-preferring (P) rats. Alcohol 42:277–284
Toll B, White M, Wu R, Meandzija B, Jatlow P, Makuch R, O’Malley S (2010) Low-dose naltrexone augmentation of nicotine replacement for smoking cessation with reduced weight gain: a randomized trial. Drug Alcohol Depend 2010(3):200–206
Truitt WA, Hauser SR, Deehan GJ, Toalston JE, Wilden JA, Bell RL, McBride WJ, Rodd ZA (2015) Ethanol and nicotine interaction within the posterior ventral tegmental area in male and female alcohol-preferring rats: evidence of synergy and differential gene activation in the nucleus accumbens shell. Psychopharmacology 232(3):639–649
Volpicelli JR, Alterman AI, Hayashida M, O’Brien CP (1992) Naltrexone in the treatment of alcohol dependence. Arch Gen Psychiatry 49(11):876–880
Volpicelli JR, Rhines KC, Rhines JS, Volpicelli LA, Alterman AI, O’Brien CP (1997) Naltrexone and alcohol dependence. Role of subject compliance. Arch Gen Psychiatry 54:737–742
Wetter DW, Kenford SL, Smith SS, Fiore MC, Jorenby DE, Baker TB (1999) Gender differences in smoking cessation. J Consult Clin Psychol 67(4):555–562
Wong G, Wolter T, Croghan G, Croghan I, Offord K, Hurt R (1999) A randomized trial of naltrexone for smoking cessation. Addiction 94(8):1227–1237
Zhu S, Lee M, Zhuang Y, Gamst A, Wolfson T (2012) Interventions to increase smoking cessation at the population level: how much progress has been made in the last two decades? Tob Control 21(2):110–118
Funding
This study was supported by NIAAA grants AA07611, AA07462, AA10721, AA20908, and AA019366.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 236 kb)
Rights and permissions
About this article
Cite this article
Waeiss, R.A., Knight, C.P., Hauser, S.R. et al. Therapeutic challenges for concurrent ethanol and nicotine consumption: naltrexone and varenicline fail to alter simultaneous ethanol and nicotine intake by female alcohol-preferring (P) rats. Psychopharmacology 236, 1887–1900 (2019). https://doi.org/10.1007/s00213-019-5174-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-019-5174-y