Abstract
Rationale
The co-abuse of ethanol (EtOH) and nicotine (NIC) increases the likelihood that an individual will relapse to drug use while attempting to maintain abstinence. There is limited research examining the consequences of long-term EtOH and NIC co-abuse.
Objectives
The current experiments determined the enduring effects of chronic EtOH, NIC, or EtOH + NIC intake on the reinforcing properties of NIC and glutamate (GLU) activity within the mesocorticolimbic (MCL) system.
Methods
Alcohol-preferring (P) rats self-administered EtOH, Sacc + NIC, or EtOH + NIC combined for 10 weeks. The reinforcing properties of 0.1–3.0 μM NIC within the nucleus accumbens shell (AcbSh) were assessed following a 2–3-week drug-free period using intracranial self-administration (ICSA) procedures. The effects of EtOH, Sacc, Sacc + NIC, or EtOH + NIC intake on extracellular levels and clearance of glutamate (GLU) in the medial prefrontal cortex (mPFC) were also determined.
Results
Binge intake of EtOH (96–100 mg%) and NIC (21–27 mg/mL) were attained. All groups of P rats self-infused 3.0 μM NIC directly into the AcbSh, whereas only animals in the EtOH + NIC co-abuse group self-infused the 0.3 and 1.0 μM NIC concentrations. Additionally, self-administration of EtOH + NIC, but not EtOH, Sacc or Sacc + NIC, resulted in enduring increases in basal extracellular GLU levels in the mPFC.
Conclusions
Overall, the co-abuse of EtOH + NIC produced enduring neuronal alterations within the MCL which enhanced the rewarding properties of NIC in the AcbSh and elevated extracellular GLU levels within the mPFC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alcohol use and smoking are two of the leading preventable causes of disease and death in the USA (Mokdad et al. 2004). For many individuals, the co-use/abuse of alcohol (EtOH) and nicotine (NIC) go hand in hand (John et al. 2003a, b; DiFranza and Guerrera 1990). Within the clinical population, EtOH and/or NIC addiction proceeds in a chronic recurring fashion with alternating periods of abstinence and relapse (NIDA 2014). Individuals that co-abuse EtOH and NIC exhibit a significantly poorer clinical outcome (i.e., higher relapse rates), when attempting to maintain abstinence, than individuals who use only one of the drugs (Lajtha and Sershen 2010). Thus, there is a need to better understand the neurobiological mechanisms underlying the interactions of EtOH and NIC that contribute to their high co-morbidity and increased risk of relapse when an individual co-abuses these drugs.
The medial prefrontal cortex (mPFC) is involved in higher-order processing/cognitive functioning in mammals and possesses reciprocal projections with several subcortical brain structures within the mesolimbic reward pathway (Hoover and Vertes 2007; Steketee 2003). There is evidence that the GLU system within the mPFC is involved in the manifestation of drug-seeking (Ma et al. 2014; Miller and Marshall 2004; Peters et al. 2008: Stefanik et al. 2013) and an alteration in the homeostatic balance of glutamate (GLU) in this area may precipitate drug relapse (Kalivas 2009). The mPFC receives major GLU projections from the basolateral nucleus of the amygdala (BLA), dorsal thalamus, and the hippocampus (Hoover and Vertes 2007) and sends GLU afferents to downstream reward associated structures including the nucleus accumbens (Acb) (Steketee 2003). Thus, alteration in GLU functioning within the mPFC would affect downstream structures also intricately linked to drug reward and relapse. Given that recent research has indicated chronic EtOH (Holmes et al. 2012) or chronic NIC (Wang et al. 2007, 2008) have both been shown to alter GLU function within the mPFC, it is likely that this structure possesses an important role in the co-abuse of EtOH and NIC.
Several subcortical structures within the mesocorticolimbic (MCL) system have been established as critical components of drug reward/reinforcement. Animals will directly self-administer EtOH and NIC into the posterior ventral tegmental area (pVTA) at pharmacologically relevant concentrations (Hauser et al. 2014; Rodd et al. 2004). Moreover, EtOH is self-infused into the nucleus accumbens shell (AcbSh) (Engleman et al. 2009). A recent study provided evidence that EtOH and NIC act synergistically to produce reinforcement within the pVTA. Male and female alcohol-preferring (P) rats exhibited reliable operant responding for a combination of subthreshold concentrations of EtOH and NIC (50 mg% and 1 μM, respectively) but failed to reliably infuse either compound alone (Truitt et al. 2015). Exposure of midbrain slices to low concentrations of EtOH and NIC resulted in stimulation of VTA dopamine (DA) neurons that was not observed following equivalent exposure to EtOH or NIC alone (Clark and Little 2004). To date, there has been limited research examining the interactions of chronic EtOH and NIC. Recently, chronic EtOH and NIC consumption was readily obtained through the use of an operant oral self-administration model (Hauser et al. 2012). In this paradigm, the drug intake of alcohol-preferring (P) rats produced binge-like blood-EtOH levels and blood-NIC levels comparable to that observed in chain smokers (Hauser et al. 2012), providing a useful model in which to examine the neurobiological ramifications of EtOH and NIC co-abuse.
The current experiments were conducted to examine the consequences of the chronic co-abuse of EtOH and NIC followed by an imposed abstinence on the rewarding properties of NIC within the AcbSh as well as basal extracellular levels and clearance of GLU within the mPFC. The hypothesis to be tested was that EtOH and NIC co-abuse produces enduring behavioral and neurobiological alterations within the MCL system that are not observed following the abuse of EtOH or NIC individually.
Materials and methods
Animals
Female P rats, from the 68th to 71st generations weighing 250–320 g at the time of surgery were used. Rats were double-housed upon arrival and maintained on a 12-h reverse light–dark cycle (lights off at 0900 hours). Food and water were freely available except in the test chamber. Animals used in this study were maintained in facilities fully accredited by the Association for the Assessment and Accreditation of Laboratory Animal Care (AAALAC). All research protocols were approved by the institutional animal care and use committee and are in accordance with the guidelines of the Institutional Care and Use Committee of the National Institute on Drug Abuse, NIH, and the Guide for the Care and Use of Laboratory Animals (Research Institute for Laboratory Animal Research 2011).
EtOH, sacc + NIC, and EtOH and NIC operant self-administration
Ethyl alcohol (190 proof; McCormick Distilling Co., Weston, MO) was diluted using distilled water to concentrations of 10, 20, and 30 % v/v. NIC HCl was purchased from Sigma (St. Louis, USA). NIC concentrations of 0.07 and 0.14 mg/mL (salt) were dissolved in 0.0125 % saccharin (Sacc) or 10, 20, and 30 % EtOH for operant oral self-administration sessions.
Self-administration of EtOH and EtOH + NIC occurred in three-lever operant conditioning chambers (Coulbourn Instruments) contained within ventilated, sound-attenuated enclosures. Water was available constantly throughout testing through a drinking sprout located on the wall opposite the levers. Naive P rats were placed into the operant conditioning chamber, without prior training. Operant conditioning sessions were 60-min in duration and occurred daily for 10 weeks (Rodd et al. 2006). All levers were maintained on an FR1 schedule of reinforcement for 4 weeks then increased to an FR-3 schedule for 3 weeks, and then to an FR-5 schedule for 3 weeks. Animals in the EtOH alone group had concurrent access to 10, 20, and 30 % EtOH. The EtOH and NIC (EtOH + NIC) co-administration group was given concurrent access to 10, 20, and 30 % EtOH with 0.14 mg/mL NIC added to each. The water control group had water available from all three levers. All Sacc + NIC groups had concurrent access to 0.0125 % Saccharin (Sacc) with 0.07 or 0.14 mg/mL NIC in a two-lever operant conditioning chamber to obtain similar blood-nicotine levels as rats in the EtOH + NIC group. Past data indicated these procedures would result in equivalent blood and intake levels for NIC across all groups (Hauser et al. 2012).
It is important to note that a Sacc alone group was only employed during the GLU no-net-flux experiment. Prior research indicated that Sacc does not induce neurochemical alterations in the Acb during operant conditioning (Melendez et al. 2002, 2004). Therefore, use of a Sacc alone control group was limited to the GLU no-net-flux experiment to minimize overall animal numbers and cost.
Effects of chronic EtOH, Sacc + NIC, and EtOH + NIC intake on the self-infusion of NIC into the AcbSh
All animals received 10 weeks of access to their assigned fluids and were then deprived for 1 week prior to surgery. Further details of the surgical procedure, test chambers, and general test conditions are provided in other reports (e.g., Hauser et al. 2014; Rodd et al. 2005). Briefly, animals were implanted with a guide cannula aimed at the AcbSh at least 7 days after the last operant oral self-administration session. All rats experienced a least 2 weeks of abstinence prior to testing. The ICSA operant conditioning chamber was equipped with two levers. Depression of the “active lever” (FR1 schedule of reinforcement) caused the delivery of a 100-nl bolus of infusate over 5 s followed by a 5-s time-out period. During both the 5-s infusion period and 5-s time-out period, responses on the active lever did not produce further infusions. Responses on the “inactive lever” were recorded but did not result in infusions. The assignment of active and inactive lever with respect to the left or right position was counterbalanced among subjects. The active and inactive levers remained the same for each rat throughout the experiment. The number of infusions and responses on the active and inactive lever were recorded. The duration of each test session was 4 h, and sessions occurred every other day.
Rats with previous drinking history of water, EtOH, Sacc + NIC, or EtOH + NIC (n = 135) were randomly assigned to one of five NIC concentration groups (n = 6–8/drinking history/NIC concentration). A vehicle group received infusions of artificial cerebral spinal fluid (aCSF) for all seven sessions. The other groups received infusions of 0.1, 0.3, 1.0, or 3.0 μM NIC for the first four sessions (acquisition). During the fifth and sixth sessions, all animals received infusions of aCSF and the original infusate was returned on the seventh session (reinstatement).
Effects of chronic EtOH, Sacc, sacc + NIC, and EtOH + NIC consumption on basal extracellular levels and clearance of GLU in the mPFC
All animals underwent operant conditioning identical to that previously reported by Hauser et al. (2012). Approximately 9 days after the completion of operant testing, all animals were anesthetized using 2 % isoflurane and implanted unilaterally with a single guide cannula (Plastics One, Inc., Roanoke, VA, USA) aimed approximately 1.0 mm above the mPFC (AP +3.0 mm, ML −0.7 mm, DV −2.0 mm; Paxinos and Watson 2005). Immediately following surgery a dummy stylet was inserted into the cannula and remained in place until probe insertion. Following surgery, all rats were single housed and provided 7 days to recover prior to the start of testing. During the final 3 days of recovery, all rats underwent daily handling and habituation to the microdialysis chambers. On the final recovery day, loop style microdialysis probes (active length 2.0 mm, Spectra/Por RC, inner diameter 200 μM, molecular weight cutoff 13,000, Spectrum Laboratories, Inc., Rancho Dominguez, CA) were inserted into the mPFC following handling/habituation. Approximately 24 h after probe insertion (16 days after the final operant conditioning session), five groups of rats (n = 6–8/group: water, EtOH, Sacc + NIC, EtOH + NIC, or Sacc) underwent quantitative microdialysis for GLU in the mPFC in which samples were collected every 10 min, at a flow rate of 2 μl/min, by perfusing aCSF followed by aCSF containing 1 of 3 GLU concentrations (1, 5, and 10 μM) in randomized order across rats. Each GLU concentration was perfused for a total of five samples (50 min). Following the completion of microdialysis, animals were euthanized, brains were extracted, and histological analysis was performed to verify placement of the microdialysis probes in the mPFC. All samples were analyzed using high-pressure chromatography (HPLC) with electrochemical detection. Animals with a probe location outside the mPFC were excluded from statistical analyses.
Histology
At the termination of the ICSA and microdialysis experiments, 1 % bromophenol blue (0.5 μL) was injected or perfused through the microdialysis probe. Subsequently, the animals were given a fatal dose of carbon dioxide and then decapitated. Brains were removed and immediately frozen at −70 °C. Frozen brains were subsequently equilibrated at −15 °C in a cryostat microtome and then sliced into 40-μm sections. Sections were then stained with cresyl violet and examined under a light microscope for verification of the injection site using the rat brain atlas of Paxinos and Watson (2005).
Statistical analysis
Data analysis for the ICSA experiment consisted of a drinking history × concentration × session mixed ANOVA with a repeated measure of “session” was performed on the number of infusions. Additionally, for each individual group, lever discrimination was determined by a lever (active or inactive) × session mixed ANOVA with a repeated measure of session. Quantitative microdialysis data were analyzed using multiple linear regression and one-way ANOVAs as previously described (Ding et al. 2013). The slope (extraction fraction; in vivo recover of GLU) and the x intercept (basal GLU level) were calculated by comparing the GLU concentration perfused through the probe with the GLU concentration that was collected for each sample. Group differences were analyzed with multiple linear regression modeling and the effects of EtOH and/or NIC were analyzed with one-way ANOVAs using SAS System for Windows version 8.02 (SAS Institute Incorporated, Cary, NC).
Results
Operant oral self-administration
During the final week of operant testing, rats exhibited binge-like intake of the test solutions at levels that produced blood ethanol concentrations (BECs) in excess of 96 mg% and blood NIC levels in excess of 21 mg/mL with no significant differences in lever responding between groups (data not shown). The rate of acquisition of EtOH, NIC, and EtOH + NIC self-administration was comparable; therefore, the total duration and amount of drug exposure was equivalent between groups (Hauser et al. 2012).
Effects of chronic EtOH, NIC, and EtOH + NIC consumption on the self-infusion of NIC into the AcbSh
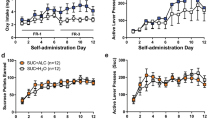
The mixed ANOVA conducted on the average number of infusions received during the initial four ICSA test sessions (Fig. 1) revealed a significant “drinking history” × “nicotine concentration” interaction (F 12,115 = 26.61; p < 0.0001). However, there was no significant effect of drinking history for each NIC concentration on the self-infusion of either aCSF or 0.1 μM NIC into the AcbSh (F values < 0.323; p values < 0.81). In contrast, there were significant effects of drinking history for the self-infusion of 0.3, 1.0, and 3.0 μM NIC into the AcbSh (F values > 37.62; p values < 0.0001). Post hoc analysis (Tukey’s b) indicated that 0.3, 1.0, and 3.0 μM NIC were self-infused more frequently into the AcbSh by rats with a past drinking history of EtOH + NIC than in all other groups. Examining the effect of “NIC concentration” in each drinking history group revealed that the number of self-infusion varied across the concentration of NIC self-administered (F values > 15.89; p values < 0.001). Rats with a past drinking history of water, EtOH, or NIC, self-infused 3.0 μM NIC directly into the AcbSh at a significantly higher rate than aCSF. Rats that consumed EtOH + NIC self-infused significantly more 0.3, 1.0, and 3.0 μM NIC than aCSF controls while the 1.0 and 3.0 μM NIC groups received significantly more self-infusions than the 0.3 μM NIC group.
The mean (± SEMs) number of infusions into the AcbSh by P rats for all concentrations of NIC during the initial four ICSA sessions for the water (n = 36), EtOH (n = 36), NIC (n = 31), or EtOH + NIC (n = 32) groups. Rats in the EtOH + NIC group exhibited a significantly higher number of self-infusions for 1.0 and 3.0 μM NIC compared to all other groups (p < 0.0001). Similarly, EtOH + NIC exposed animals self-infused significantly more 0.3 μM NIC than their cohorts in the water, EtOH, or NIC groups. Animals that had previously self-administered water, EtOH, or NIC exhibited a significantly higher number of self-infusions for 3.0 μM NIC than their counterparts in all other groups (p < 0.001)
A repeated measure ANOVA with a within-subject factor of “session” and between-subject factors of “drinking history” and “nicotine concentration” was performed on the number of active lever responses. Overall, the analysis revealed a significant drinking history × nicotine concentration × session interaction (F 72,690 = 3.48; p < 0.0001). There was no significant effect of session or drinking history for the aCSF or 0.1 μM NIC groups (data not shown) (F values < 1.27; p values > 0.237). Rats that self-infused 0.3, 1.0, or 3.0 μM NIC exhibited significant drinking history × session interactions (F values > 2.34; p values < 0.008). The active lever presses for each individual session by rats self-infusing 0.3 μM NIC (Fig. 2) revealed a significant effect of drinking history during the second to fourth test sessions (F 3,22 values > 9.87; p < 0.0001). Post hoc comparisons revealed that the EtOH + NIC group responded significantly more on the active lever during these sessions compared to all other groups.
The data for mean (± SEMs) number of lever responses on the active and inactive levers for the water (n = 6), EtOH (n = 7), NIC (n = 7), or EtOH + NIC (n = 6) groups during seven sessions of ICSA testing with 0.3 μM NIC. Only animals that had previously consumed EtOH + NIC exhibited a significant active lever preference for 0.3 μM NIC (sessions 2–4; p < 0.001). Following aCSF substitution (sessions 5 and 6), reinstatement of 0.3 μM NIC (session 7) produced a robust increase in active lever responding compared to both the inactive lever and pre-substitution level responding (p < 0.0001)
Evidence for extinction during aCSF substitution was evident by the lack of an effect of drinking history during session 6 (F 3,22 = 1.738; p = 0.19). The return of NIC into the infusate during session 7 resulted in significant effect of drinking history (F 3,22 = 33.1; p < 0.0001) as the EtOH + NIC group responded more on the active lever compared to all other groups. Rats self-infusing 1.0 or 3.0 μM NIC (Figs. 3 and 4) exhibited a significant effect of drinking history on active lever responses during sessions 1–4 (F values > 16.1; p values < 0.0001), and post hoc comparisons indicated that lever responses were greater in the EtOH + NIC group compared to all other groups. Further examination of the three-way interaction for active lever responding revealed that responding for 3.0 μM NIC (Fig. 4) was significantly higher in rats with a past drinking history of water, EtOH, or NIC compared to aCSF controls. In rats with a past drinking history of EtOH + NIC, active lever responding for 0.3, 1.0, or 3.0 μM NIC was greater than for aCSF (1.0 and 3.0 μM NIC > 0.3 μM NIC).
The data for mean (± SEMs) number of lever responses on the active and inactive levers for the water (n = 8), EtOH (n = 7), NIC (n = 7), or EtOH + NIC (n = 6) groups across seven sessions of ICSA testing with 1.0 μM NIC. Only animals in the EtOH + NIC group exhibited a significant active lever preference for 1.0 μM NIC (sessions 1–4 and 7; p < 0.001) (asterisks)
The data for mean (± SEMs) number of lever responses on the active and inactive levers for the water (n = 8), EtOH (n = 6), NIC (n = 6), or EtOH + NIC (n = 6) groups across seven sessions of ICSA testing with 3.0 μM NIC. Rats in all four groups exhibited a significant active lever discrimination for 3.0 μM NIC (p < 0.001) (asterisks). Animals that had previously self-administered EtOH + NIC exhibited a significantly higher level of responding on the active lever compared to all other groups (sessions 2–4 and 7; p < 0.0001) (plus signs). Animals did not show lever discrimination during aCSF substitution (sessions 5 and 6)
Rats self-infusing 3.0 μM NIC displayed lever discrimination between the active and inactive lever (p values < 0.003) during sessions 1–4 and 7. Lever discrimination was not observed during session 6 in all groups (p > 0.23). Lever discrimination was observed in rats with a past drinking history of EtOH + NIC self-infusing 0.3 and 1.0 μM NIC (bottom right panels; Figs. 2 and 3), sessions 2–4 and 1–4, respectively (p values < 0.004). These rats failed to discriminate between active and inactive levers during sessions 5 and 6 (aCSF substitution).
There was a significant drinking history × nicotine concentration × session interaction (F 72,690 = 1.93; p < 0.001) for inactive lever responding. Post hoc analysis revealed that for rats self-infusing NIC during sessions 1–4 (as indicated by significantly higher level of responding compared to aCSF controls), there was an increase in inactive lever responding during the firstt aCSF substitution session (session 6; Figs. 2, 3, and 4). Increase in inactive lever responding during the first aCSF substitution session has been observed for cocaine and EtOH ICSA in P rats (Rodd et al. 2005; Rodd-Henricks et al. 2002; Katner et al. 2011). This increase in inactive lever responding is thought to be indicative of drug-seeking.
Effects of chronic EtOH, NIC, and EtOH + NIC consumption on basal extracellular levels and clearance of GLU in the mPFC
Representative probe placements within the mPFC are illustrated in Fig. 5. Animals with cannula/probe placements outside of the mPFC were excluded from analyses. Analysis of the x intercepts using a univariate ANOVA revealed a significant effect of group on basal extracellular GLU levels, F(4,29) = 7.10, p < 0.05. Analyzing the main effect further, a Tukey’s b post hoc analysis found that extracellular GLU levels were significantly higher in the EtOH + NIC group (8.1 ± 2 μM) than all other groups: water 2.3 ± 0.5 μM, EtOH 3.5 ± 0.75 μM, SAC 2.7 ± 0.4 μM, SAC + NIC 1.7 ± 0.5 μM (Fig. 6; p < 0.05). With regard to GLU clearance, a univariate ANOVA on the extraction fractions obtained via multiple linear regression analysis revealed a significant effect of group, F(4,29) = 17.15, p < 0.05. An additional Tukey’s b post hoc analysis observed a significantly higher level of GLU clearance in the mPFC of rats that consumed SAC + NIC (70 ± 3 %) compared to all other groups: naive 30 ± 5 %, EtOH 20 ± 7 %, EtOH + NIC 24 ± 4 %, and SAC 35 ± 2 % (p < 0.05).
Displays the mean (± SEMs) basal extracellular levels (top panel) and clearance (bottom panel) of GLU in the mPFC of naive (n = 8), EtOH (n = 7), EtOH + NIC (n = 6), SAC + NIC (n = 6), and SAC alone (n = 7) groups. Animals in the EtOH + NIC group exhibited significantly higher basal extracellular levels of GLU compared to all other groups (p < 0.05) (asterisks). Rats in the SAC + NIC group exhibited a significantly higher level of GLU clearance within the mPFC (p < 0.05) (plus signs)
Discussion
Overall, the current data indicates that the effects of EtOH and NIC co-abuse cannot be summarized as simple modifications to neuroadaptations produced by comparable intake of EtOH or NIC. In contrast to the expected additive or synergistic effects of EtOH and NIC co-abuse, the data indicate that co-abuse modifies glutamatergic functioning within the mPFC in a unique manner. Further, the present data are the first to indicate that NIC is self-administered within the AcbSh. Smokers can readily obtain blood NIC concentrations that exceed the levels that were used in the current experiment (Benowitz 1997). P rats will orally self-administer solutions of EtOH + NIC (15 % and 0.14 mg/mL) at rates that produce blood EtOH and NIC concentrations that approach those used in the current experiments (>80 mg% and 27 ng/mL, respectively; Hauser et al. 2012). The actual concentration of NIC in the brain following microinjection is likely lower than those achieved in the current ICSA experiments and may approach the levels observed following oral EtOH + NIC self-administration in P rats (167 nM; 0.167 μM). Thus, the ICSA findings suggest that biologically relevant levels of NIC are reinforcing within the AcbSh.
The reinforcing properties of NIC in the AcbSh are likely to be mediated, in part, by the dopaminergic and glutamatergic systems. Local application of NIC into the AcbSh increases extracellular concentrations of DA and GLU (Toth et al. 1992; Marshall et al. 1997). Microinjections of DA antagonists into the AcbSh block the rewarding properties of systemically administered NIC (Sun et al. 2014). Chronic systemic administration of EtOH and NIC can alter GLU levels within the Acb (Lallemand et al. 2011). Nicotinic acetylcholine receptors (NAchRs; α4β2, α6β2, and α4α6β2β3) in the AcbSh are located presynaptically on DA terminals that emerge from distinct DA fiber pathways possessing distinct firing characteristics (Meyer et al. 2008). Presynaptic α7 NAchRs on glutamatergic input into the AcbSh positively mediate the release of GLU and indirectly mediate the release of DA (c.f., Livingstone and Wonnacott 2009). Activation of α7 receptors by NIC stimulated the release of GLU which acts on ionotropic presynaptic GLU receptors that stimulate DA release (Innocent et al. 2008). In addition, alterations in the stoichiometry of the α4β2 NAchR from a (α4)2(β2)3 to an (α4)3(β2)2 greatly enhances the sensitivity of the receptor to the actions of NIC (Nelson et al. 2003). However, alterations in NAchRs produced by NIC exposure are typically short lived and would likely not be present during subsequent ICSA testing (at least 14 days after last operant conditioning session; Nelson et al. 2003).
Similar to the ICSA dataset, the analysis of the effects of chronic EtOH, NIC, or EtOH + NIC consumption on the glutamatergic system in the mPFC indicated enduring unique alterations produced by EtOH + NIC co-abuse (Fig. 6). Chronic EtOH + NIC co-abuse resulted in a persistent (16 days following last operant self-administration session) alteration in basal GLU levels within the mPFC (>3-fold increase compared to water controls). Consumption of equivalent levels of EtOH or NIC did not alter basal GLU levels (Fig. 6; top panel). Such an increase of GLU levels within the mPFC has been postulated as an indicator of a predisposition for heightened drug-seeking (Kalivas 2009). Manipulations that reduce GLU activity in discrete regions of the mPFC can inhibit drug-seeking and NIC reward (Paterson et al. 2003; Kalivas and O’Brien 2008). P rats that co-abused EtOH and NIC expressed a greater and more prolonged context-induced drug-seeking than P cohorts that self-administered equivalent levels of EtOH or NIC (Hauser et al. 2012). The current data indicate that during a comparable time period used to test context-induced drug-seeking (14 days), chronic EtOH + NIC co-abuse results in a significant increase in basal GLU levels in the mPFC. Therefore, it is plausible that increased basal GLU levels in the mPFC may contribute to the behavioral manifestation of heightened drug-seeking.
Chronic NIC consumption increased the recovery/clearance of GLU in the mPFC which was not observed following equivalent consumption of NIC in the EtOH + NIC co-abuse group (Fig. 6; bottom panel). The increase in recovery/clearance suggests that chronic NIC consumption resulted in an increase in GLU release in the mPFC which produced a compensatory reaction of an increased removal of the neurotransmitter in an effort to maintain the homeostatic level of GLU in the region. The divergence in the alteration of the GLU system produced by chronic NIC (consistent basal levels, increased clearance) and EtOH + NIC (increased basal levels, no alteration in clearance) consumption would suggest that the additional consumption of EtOH in the co-abuse group inhibited the neuroadaptations observed in the NIC alone group or that co-abuse of EtOH + NIC activated distinct pathways that do not parallel that observed following NIC consumption.
A possible factor in the alterations observed in GLU functioning within the mPFC could have been exposure to isoflurane anesthetic. Isoflurane interacts with GABA-A receptors and can produce memory deficits (Zurek et al. 2012, Saab et al. 2010). However, such memory deficits generally disappear within 72 hrs and it is likely that the effects of isoflurane would have dissipated during the 7-day interval between surgery and the microdialysis and ICSA experiments.
In general, the current data indicate that chronic EtOH and NIC self-administration results in unique neuroadaptations that are not observed following equivalent EtOH or NIC self-administration, which alter the rewarding properties of NIC within the AcbSh and GLU activity within the mPFC. However, it is not possible with the current experimental design to determine if the effects observed were due to the chronic co-abuse of EtOH and NIC or if the effects were a factor of the co-abuse of these drugs coupled with drug-free period of imposed abstinence. Since the majority of alcoholics and NIC-dependent individuals co-abuse/use EtOH and NIC, the successful development of pharmacotherapeutics for the treatment of these disorders will be predicated upon a better understanding of the interaction between these two drugs within the brain.
References
Benowitz NL (1997) Systemic absorption and effects of nicotine from smokeless tobacco. Adv Dent Res 11:336–341
Clark A, Little HJ (2004) Interaction between low concentrations of ethanol and nicotine on firing rate of ventral tegmental dopamine neurons. Drug Alcohol Depend 75:199–206
DiFranza JR, Guerrera MP (1990) Alcoholism and smoking. J Stud Alcohol 51:130–135
Ding ZM, Rodd ZA, Engleman EA, Bailey JA, Lahiri DK, McBride WJ (2013) Alcohol drinking and deprivation alter basal extracellular glutamate concentrations and clearance in the mesolimbic system of alcohol-preferring (P) rats. Addict Biol 18:297–306
Engleman EA, Ding ZM, Oster SM, Toalston JE, Bell RL, Murphy JM, McBride WJ, Rodd ZA (2009) Ethanol is self-administered into the nucleus accumbens shell, but not the core: evidence of genetic sensitivity. Alcohol Clin Exp Res 12:2162–71
Hauser SR, Katner SN, Deehan GA Jr, Ding ZM, Toalston JE, Scott BJ, Bell RL, McBride WJ, Rodd ZA (2012) Development of an oral operant nicotine/ethanol co-use model in alcohol-preferring (p) rats. Alcohol Clin Exp Res 36:1963–72
Hauser SR, Bracken AL, Deehan GA Jr, Toalston JE, Ding ZM, Truitt WA, Bell RL, McBride WJ, Rodd ZA (2014) Selective breeding for high alcohol preference increases the sensitivity of the posterior VTA to the reinforcing effects of nicotine. Addict Biol 19:800–11
Holmes A, Fitzgerald PJ, MacPherson KP, DeBrouse L, Colacicco G, Flynn SM, Masneuf S et al (2012) Chronic alcohol remodels prefrontal neurons and disrupts NMDAR-mediated fear extinction encoding. Nat Neurosci 15:1359–61
Hoover WB, Vertes RP (2007) Anatomical analysis of afferent projections to the medial prefrontal cortex in the rat. Brain Struct Funct 212:149–79
Innocent N, Linvingstone PD, Hone A, Kimura A, Young T, Whiteaker P, McIntosh JM, Wonnacott S (2008) alphaConotoxin ArlB[V11L, V16D] is a potent and selective antagonist at rat and human native alpha 7 nicotinic acetycholine receptors. J Pharmacol Exp Ther 327:529–37
John U, Hill A, Rumpf H, Meyer C (2003a) Alcohol high risk drinking, abuse, and dependence among tobacco smoking medical care patients and the general population. Drug Alcohol Depend 64:233–241
John U, Meyer C, Rumpf HJ, Schumann A, Thyrian JR, Hapke U (2003b) Strength of the relationship between tobacco smoking, nicotine dependence and the severity of alcohol dependence syndrome criteria in a population-based sample. Alcohol Alcohol 38:606–612
Kalivas PW (2009) The glutamate homeostasis hypothesis of addiction. Nat Rev Neurosci 10:561–72
Kalivas PW, O’Brien C (2008) Drug addiction as a pathology of staged neuroplasticity. Neuropsychopharmacology 33:166–80
Katner SN, Oster SM, Ding ZM, Deehan GA Jr, Toalston JE, Hauser SR, McBride WJ, Rodd ZA (2011) Alcohol-preferring (P) rats are more sensitive than Wistar rats to the reinforcing effects of cocaine self-administered directly into the nucleus accumbens shell. Pharmacol Biochem Behav 99:688–95
Lajtha A, Sershen H (2010) Nicotine: alcohol reward interactions. Neurochem Res 35:1248–58
Lallemand F, Ward RJ, De Witte P, Verbanck P (2011) Binge drinking +/− chronic nicotine administration alters extracellular glutamate and arginine levels in the nucleus accumbens of adult male and female Wistar rats. Alcohol Alcohol 46:373–82
Livingstone PD, Wonnacott S (2009) Nicotinic acetylcholine receptors and the ascending dopamine pathways. Biochem Pharmacol 78:744–55
Ma YY, Lee BR, Wang X, Guo C, Liu L, Cui R, Lan Y et al (2014) Bidirectional modulation of incubation of cocaine craving by silent synapse-base remodeling of prefrontal cortex to accumbens projections. Neuron 83:1453–67
Marshall DL, Redfern PH, Wonnacott S (1997) Presynaptic nicotinic modulation of dopamine release in the three ascending pathways studied by in vivo microdialysis: comparison of naive and chronic nicotine-treated rats. J Neurochem 68:1511–9
Melendez RI, Rodd-Henricks ZA, Engleman EA, Li TK, McBride WJ, Murphy JM (2002) Microdialysis of dopamine in the nucleus accumbens of alcohol-preferring (P) rats during anticipation and operant self-administration of ethanol. Alcohol Clin Exp Res 26:318–25
Melendez RI, Rodd ZA, McBride WJ, Murphy JM (2004) Involvement of the mesopallidal dopamine system in ethanol reinforcement. Alcohol 32:137–44
Meyer EL, Yoshikami D, McIntosh JM (2008) The neuronal nicotinic acetylcholine receptors α4* and α6* differentially modulate dopamine release in mouse striatal slices. J Neurochem 105:1761–69
Miller CA, Marshall JF (2004) Altered prelimbic cortex output during cue-elicited drug seeking. J Neurosci 4:6889–97
Mokdad AH, Marks JS, Stroup DF, Gerberding JL (2004) Actual causes of death in the United States, 2000. JAMA 291:1238–1245
National Institute on Drug Abuse (2014) The science of drug addiction: the basics. Available via http: http://www.drugabuse.gov/publications/media-guide/science-drug-abuse-addiction-basics. Accessed 10 Aug 2015
Nelson ME, Kuryatov A, Choi CH, Zhou Y, Lindstrom J (2003) Alternate stoichiometries of alpha4beta2 nicotinic acetylcholine receptors. Mol Pharmacol 63:332–41
Paterson NE, Semenova S, Gasparini F, Markou A (2003) The mGluR5 antagonist MPEP decreased nicotine self-administration in rats and mice. Psychopharmacology (Berl) 167:257–64
Paxinos G, Watson C (2005) The rat brain in stereotaxic coordinates, 5th edn. Academic Press, New York
Peters J, LaLumiere RT, Kalivas PW (2008) Infralimbic prefrontal cortex is responsible for inhibiting cocaine seeking in extinguished rats. J Neuorsci 28:6046–53
Research Institute for Laboratory Animal Research (2011) Guide for the Care and Use of Laboratory Animals, 8th edn. The National Academies Press, Washington, D.C
Rodd ZA, Melendez RI, Bell RL, Kuc KA, Zhang Y, Murphy JM, McBride WJ (2004) Intracranial self-administration of ethanol within the ventral tegmental area of male Wistar rats: evidence for involvement of dopamine neurons. J Neurosci 24:1050–7
Rodd ZA, Bell RL, Zhang Y, Murphy JM, Goldstein A, Zaffaroni A, Li TK, McBride (2005) Regional heterogeneity for the intracranial self-administration of ethanol and acetaldehyde within the ventral tegmental area of alcohol-preferring (P) rats: involvement of dopamine and serotonin. Neuropsychopharmacology 30:330–8
Rodd ZA, McKinzie DL, Bell RL, McQueen VK, Murphy JM, Schoepp DD, McBride WJ (2006) The metabotropic glutamate 2/3 receptor agonist LY404039 reduces alcohol-seeking but not alcohol self-administration in alcohol-preferring (P) rats. Behav Brain Res 171:207–15
Rodd-Henricks ZA, McKinzie DL, Li TK, Murphy JM, McBride WJ (2002) Cocaine is self-administered into the shell but not the core of the nucleus accumbens of Wistar rats. J Pharmacol Exp Ther 303:1216–26
Saab BJ, Maclean AJ, Kanisek M, Zurek AA, Martin LJ, Roder JC, Orser BA (2010) Short-term memory impairment after isoflurane in mice is prevented by the α5 γ-aminobutyric acid type A receptor inverse agonist L-655,708. Anethesiology 113:1061–71
Stefanik MT, Moussawi K, Kupchik YM, Smith KC, Miller RL, Huff ML, Deisseroth K, Kalivas PW, LaLumiere RT (2013) Optogenetic inhibition of cocaine seeking in rats. Addict Biol 18:50–53
Steketee JD (2003) Neurotransmitter systems of the medial prefrontal cortex: potential role in sensitization to psychostimulants. Brain Res Rev 41:203–28
Sun N, Laviolette SR, Addiction Research Group (2014) Dopamine receptor blockade modulates the rewarding and aversive properties of nicotine via dissociable neuronal activity patterns in the nucleus accumbens. Neuropsychopharmacology 12:2799–815
Toth E, Sershen H, Hashim A, Vizi ES, Lajtha A (1992) Effect of nicotine on extracellular levels of neurotransmitters assessed by microdialysis in various brain regions: role of glutamic acid. Neurochem Res 17:265–271
Truitt WA, Hauser SR, Deehan GA Jr, Toalston JE, Wilden JA, Bell RL, McBride WJ, Rodd ZA (2015) Ethanol and nicotine interaction within the posterior ventral tegmental area in male and female alcohol-preferring rats: evidence of synergy and differential gene activation in the nucleus accumbens shell. Psychopharmacology 232:639–49
Wang F, Chen H, Steketee JD, Sharp BM (2007) Upregulation of ionotropic glutamate receptor subunits within specific mesocorticolimbic regions during chronic nicotine self-administration. Neuropsychopharm 32:103–9
Wang F, Chen H, Sharp BM (2008) Neuroadaptive changes in the mesocortical glutamatergic system during chronic nicotine self-administration and after extinction in rats. J Neurochem 106:943–56
Zurek AA, Bridgwater EM, Orser BA (2012) Inhibition of α5 γ-aminobutyric acid type A receptors restores recognition memory after general anesthesia. Anesth Analg 114:845–55
Acknowledgments
The research in this manuscript was supported by grants from the National Institute on Alcohol Abuse and Alcoholism: AA019366, AA07611, AA07462, AA012262.
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Deehan, G.A., Hauser, S.R., Waeiss, R.A. et al. Co-administration of ethanol and nicotine: the enduring alterations in the rewarding properties of nicotine and glutamate activity within the mesocorticolimbic system of female alcohol-preferring (P) rats. Psychopharmacology 232, 4293–4302 (2015). https://doi.org/10.1007/s00213-015-4056-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-015-4056-1