Abstract
Rationale
Co-users of alcohol and nicotine are the largest group of polysubstance users worldwide. Commonalities in mechanisms of action for ethanol (EtOH) and nicotine proposes the possibility of developing a single pharmacotherapeutic to treat co-use.
Objectives
Toward developing a preclinical model of co-use, female alcohol-preferring (P) rats were trained for voluntary EtOH drinking and i.v. nicotine self-administration in three phases: (1) EtOH alone (0 vs. 15%, two-bottle choice), (2) nicotine alone (0.03 mg/kg/infusion, active vs. inactive lever), and (3) concurrent access to both EtOH and nicotine. Using this model, we examined the effects of (1) varenicline, a nicotinic acetylcholine receptor (nAChR) partial agonist with high affinity for the α4β2* subtype; (2) r-bPiDI, a subtype-selective antagonist at α6β2* nAChRs; and (3) (R)-modafinil, an atypical inhibitor of the dopamine transporter (DAT).
Results
In phases 1 and 2, pharmacologically relevant intake of EtOH and nicotine was achieved. In the concurrent access phase (phase 3), EtOH consumption decreased while nicotine intake increased relative to phases 1 and 2. For drug pretreatments, in the EtOH access phase (phase 1), (R)-modafinil (100 mg/kg) decreased EtOH consumption, with no effect on water consumption. In the concurrent access phase, varenicline (3 mg/kg), r-bPiDI (20 mg/kg), and (R)-modafinil (100 mg/kg) decreased nicotine self-administration but did not alter EtOH consumption, water consumption, or inactive lever pressing.
Conclusions
These results indicate that therapeutics which may be useful for smoking cessation via selective inhibition of α4β2* or α6β2* nAChRs, or DAT inhibition, may not be sufficient to treat EtOH and nicotine co-use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In the USA, tobacco use ranks as the leading cause of preventable death (Warren et al. 2014), followed closely behind by alcohol-related death (Mokdad et al. 2004). Roughly 80% of alcoholics are also regular tobacco smokers, making co-use of alcohol (EtOH) and nicotine the most prevalent polysubstance use disorder (Falk et al. 2006). Additionally, co-use poses a threat to successful cessation of both substances, with the likelihood of a successful abstinence attempt being decreased in co-users when compared to users of either substance alone (Chiappetta et al. 2014; McKee and Weinberger 2013; Weinberger et al. 2013). Despite high incidence of co-use, EtOH and nicotine use disorders primarily have been considered as separate substance use disorders (SUDs), and medication development has focused on treating them individually. However, to the extent that there are commonalities in the mechanisms of action for EtOH and nicotine, it may be possible to develop a single pharmacotherapeutic agent to treat cigarette smokers who are also heavy drinkers (Roche et al. 2016).
Animal models have been utilized successfully to model and test treatments for either EtOH or nicotine use disorders separately (Van Skike et al. 2016), as well as for other SUDs (Koob et al. 2009), but relatively few studies have examined voluntary co-use of EtOH and nicotine in the same animal (Bell et al. 2016; McBride et al. 2014). Critical for testing pharmacotherapeutics for EtOH and nicotine co-use disorder is developing a translational animal model that produces pharmacologically relevant levels of concomitant voluntary oral EtOH consumption and i.v. nicotine self-administration.
Lê et al. (2010) developed a two-lever choice procedure for operant self-administration of EtOH and nicotine when both substances are available concurrently. Since that original report, variations of that procedure have been published, with each study showing that two-lever choice will induce reliable EtOH and nicotine co-self-administration (Cippitelli et al. 2015; Funk et al. 2016; Scuppa et al. 2015). In this general procedure, two levers are available concurrently during a limited access (60 min) session; responding on one lever delivers EtOH (12% solution, 0.19 mL per delivery into a drinking receptacle) and responding on the other lever delivers nicotine (0.03 mg/kg/infusion i.v.). The response requirement on each lever is typically a fixed ratio (FR) 3.
While the original two-lever choice procedure (Lê et al. 2010) produces reliable co-administration of both EtOH and nicotine, there are some limitations to the model in terms of its utility for preclinical screening of candidate medications for potential efficacy in decreasing co-use. If a candidate medication decreases lever pressing for both EtOH and nicotine simultaneously, it is difficult to determine if the drug is specifically decreasing the reinforcing effect of both EtOH and nicotine concurrently or is simply producing a non-specific suppression of ongoing responding. To address this limitation, the current study employed a novel model in which a two-bottle choice (EtOH vs. water) was combined with two-lever procedure (active vs. inactive for nicotine). The intended advantage of this modified procedure was to determine if potential pharmacotherapies will specifically decrease both EtOH drinking and nicotine self-infusions, while leaving both water intake and inactive lever pressing unchanged.
For this novel model, we used selectively bred EtOH-preferring (P) rats, a translational genetic model of alcoholism (Bell et al. 2012; McBride et al. 2014). Since heterogeneous stock rats generally consume only modest amounts of EtOH voluntarily (Cicero and Smithloff 1973), selective breeding techniques have been used to elicit pharmacologically relevant levels of EtOH consumption (Barkley-Levenson and Crabbe 2014; Bell et al. 2012). Additionally, criteria for an animal model of alcoholism have been proposed which mimic criteria for humans with EtOH use disorder (Bell et al. 2012; Cicero and Smithloff 1973; Lester and Freed 1973). Importantly, P rats also voluntarily consume not only intoxicating amounts of EtOH which meet these criteria, but also readily self-administer i.v. nicotine in amounts twice that of non-preferring, Wistar, and Long-Evans rats (Lê et al. 2006; Rezvani et al. 2010). Additionally, female P rats have been shown to voluntarily consume higher amounts of EtOH than male P rats (Bell et al. 2011). Thus, female P rats may be especially advantageous for screening potential medications for EtOH and nicotine co-use.
Using this novel model in female P rats, we evaluated three drugs: (1) varenicline, (2) 1,10-bis(3-methyl-5,6-dihydropyridin-1(2H)-yl)decane dihydrochloride (r-bPiDI), and (3) 2-[(R)-(diphenylmethyl)sulfinyl]acetamide ((R)-modafinil, RMOD; see Fig. 1). Varenicline, a clinically available partial agonist at α4β2* nicotinic acetylcholine receptors (nAChRs), has been demonstrated to reduce nicotine self-administration in animals (George et al. 2011; O’Connor et al. 2010; Rollema et al. 2007), reduce tobacco craving, withdrawal, and its reinforcing effects in humans (Gonzales et al. 2006; Jorenby et al. 2006; McKee et al. 2013), as well as increasing smoking abstinence rates (Ebbert et al. 2016; Gonzales et al. 2006; Nides et al. 2006). However, effects of varenicline on EtOH consumption in laboratory animals (Feduccia et al. 2014; Froehlich et al. 2017; Funk et al. 2016; Steensland et al. 2007) and in humans (de Bejczy et al. 2015; Plebani et al. 2013; Schacht et al. 2014; Verplaetse et al. 2016) have been mixed, indicating that more work is needed, especially regarding EtOH and nicotine co-use. r-bPiDI, a potent and selective α6β2* nAChR antagonist, has also been shown to decrease nicotine-evoked dopamine release and nicotine self-administration (Beckmann et al. 2015). However, it is not known if r-bPiDI alters EtOH self-administration, tested either alone or when combined with nicotine. RMOD, an atypical inhibitor of the dopamine transporter (DAT) without abuse liability, was selected based on a report demonstrating that RMOD attenuates nicotine self-administration, nicotine-induced reinstatement, and cue-induced nicotine-seeking in P rats (Wang et al. 2015). However, it is not known if RMOD also alters EtOH self-administration, tested either alone or combined with nicotine. For each drug, pretreatments were given during either the co-use phase (experiment 1) or the EtOH only phase (experiment 2).
Methods
Animals
Selectively bred female P rats (n = 25, generation 79–83) were obtained from Indiana University School of Medicine (provided by NIAAA/NIH) and began training between PND 55 to 65. Rats were housed individually upon arrival in a temperature-controlled colony room under a 12:12-h light/dark cycle. All testing procedures occurred during the light phase (7:00 am–7:00 pm) were in accordance with the NIH Guide for the Care and Use of Laboratory Animals (8th edition, 2011) and were approved by the Institutional Animal Care and Use Committee at the University of Kentucky. Some of the rats (n = 5) used in this study had a brief experimental history prior to the current experiment that involved exposure to saccharin- or quinine-flavored water and acute injections of a novel drug unrelated to the drugs tested here. In experiment 1 (total n = 17), animals were trained in both voluntary oral EtOH consumption and i.v. nicotine SA and were given drug pretreatments during the co-use phase. In experiment 2 (n = 8), animals were only trained in voluntary oral EtOH consumption and then were given drug pretreatments with varenicline, r-bPiDI, and RMOD.
Drugs
EtOH was prepared in a concentration of 15% v/v 190 proof EtOH (Pharmco-AAPER, Shelbyville, KY) diluted in distilled water. Nicotine hydrogen tartrate (Sigma-Aldrich, San Diego, CA) was dissolved in a 0.9% NaCl (saline) solution, to which NaOH was added to obtain a pH of 7.0 ± 0.05; nicotine dosage was based on freebase weight. Varenicline (6,7,8,9-tetrahydro-6,10-methano-6H pyrazino[2,3-h][3]benzazepine tartrate), a generous donation from the National Institute on Drug Abuse (NIDA) (Bethesda, MD), was dissolved in saline. r-bPiDI (1,10-bis(3-methyl-5,6-dihydropyridin-1(2H)-yl)decane) was synthesized at the University of Arkansas for Medical Sciences (Little Rock, AK) and dissolved in saline. RMOD was synthesized at the National Institute on Drug Abuse-Intramural Research Program, Medicinal Chemistry Section (Baltimore, MD) and dissolved in sterile water containing 10% DMSO and 15% Tween-80. All test drug solutions were prepared immediately before each injection and administered i.p. 15 min prior to the start of the session, with doses based on formula weights. For surgery, rats were anesthetized via i.p. injections of 55/7.5/7.5 mg/kg ketamine (Henry Schein Animal Health, Dublin, OH)/xylazine (LLOYD Laboratories, Shenandoah, IA)/sterile water. Respective drug doses were determined from the literature (e.g., Beckmann et al. 2015; George et al. 2011; Wang et al. 2015).
Apparatus
All training and testing sessions were conducted in standard two-lever operant chambers (ENV-001; MED Associates, St. Albans, VT). Two response levers were located on either side of a recessed food tray. Located above each lever was a white cue light. Nicotine infusions were delivered by a syringe pump, and food pellets were delivered by a pellet dispenser. A computer, linked to a Med Associates interface, recorded responses, and controlled infusions during the experimental session. Each chamber was modified to allow access to two 100-ml Richter feeding tube glass bottles (Model 900010; Dyets, Inc., Bethlehem, PA) on the wall of the chamber opposite the levers. The design of the bottles allowed them to be fixed securely to the outside of the chambers with lipped feeding tube holders (Model 901100; Dyets, Inc., Bethlehem, PA) such that only the drinking spout could be accessed by rats while inside the chambers.
Procedures
Experiment 1: drug pretreatments during co-use of EtOH and nicotine (phase 3)
EtOH acclimation (pre-training)
To allow for acclimation to the taste and smell of EtOH, rats were given one bottle of 20% EtOH as the sole source of liquid for 72 consecutive hours in the home cage (Simms et al. 2010). During this time, food was available ad libitum.
EtOH access (phase 1)
In phase 1, rats began daily 60-min two-bottle choice sessions by being placed in the operant conditioning chambers with the levers retracted. For the duration of each session, rats were given free access to two bottles, one bottle of water and one bottle of 15% EtOH (v/v). Both bottles were presented on the same wall of the chamber, one on the left side and the other on the right, with the position of solutions alternating daily. During these sessions, rats could drink freely from both bottles. Access to water was restricted to these daily 1-h sessions.
EtOH and water consumption were measured by weighing each bottle immediately prior to and immediately after access sessions to determine differences in weight. On the tenth day of EtOH access, blood ethanol concentration (BEC) was determined at a single time point (90 min after the start of the session) from plasma derived from tail blood. BEC was measured by a GM7 Analyser (Analox, London, UK). Animals were trained in this phase for at least 10 days until the average EtOH consumption stabilized, i.e., there were no significant differences in average consumption across four sessions (~ 14–20 days). Prior to the next phase, animals were placed back on free access to water in the home cage.
Nicotine access (phase 2)
Animals were trained to lever press for i.v. injections of nicotine (0.03 mg/kg/infusion) using the general methods previously described (Bardo et al. 1999; Corrigall and Coen 1989). At the beginning of phase 2, rats were restricted to 8–12 g of food/day in the home cage until the completion of lever press training for food pellets. In the operant conditioning chambers, rats were initially trained to acquire lever pressing for palatable food pellets (45 mg Dustless Precision Pellets, Bio-Serv, Frenchtown, NJ). Responses on one lever (active lever, counterbalanced for position across rats) resulted in illumination of a cue light located directly above the lever and the delivery of one food pellet into the receptacle; responding on the other lever (inactive) had no programmed consequence. The cue light signaling the delivery of the food pellet remained illuminated for an additional 20-s time-out (TO) period after pellet delivery; responding on either lever during this TO period had no programmed consequence. Response requirements for food pellet delivery increased under an incrementing FR schedule, beginning with FR1 (three sessions), followed by FR3 (three sessions), and then FR5, where it remained until responding for food stabilized (at least five consecutive sessions with no significant differences in responding between sessions and at least two times more responding on the active lever vs. inactive lever; ~ 14 days).
Prior to surgery, rats were given 24-h ad libitum access to food and water in the home cage. Rats then underwent surgery under anesthesia to implant a chronic indwelling catheter into the jugular vein; catheters were flushed daily with heparinized saline to maintain patency. Following surgery, rats were given 5–7 days of recovery with ad libitum access to food and water in the home cage. Following the recovery period, rats were trained to self-administer nicotine (0.03 mg/kg/infusion) using a two-lever procedure. During this time, rats were given 12–15 g of food/day in the home cage. Similar to the food training procedure, during 60-min daily sessions in the operant chambers, responses on one lever (active lever, counterbalanced for position across rats) resulted in illumination of a cue light located directly above the lever and an infusion of 0.03 mg/kg nicotine (0.1 mL over 5.9 s); responding on the other lever (inactive) had no programmed consequence. The cue light signaling the nicotine infusion remained illuminated for an additional 20-s TO period after termination of the infusion; responding on either lever during this TO period had no programmed consequence. The FR-rate was increased incrementally and stabilized at FR5, such that the animals showed consistent FR5 responding across at least three consecutive sessions (~ 14 days), after which rats were moved to the concurrent access phase.
For one group of animals (n = 12), bottles were removed from the operant chambers throughout Phase 2; water (no EtOH) was available continuously in the home cage. For the remaining animals (n = 5), access to both water and EtOH bottles in the operant conditioning chambers continued throughout phase 2. This procedural variation had no effect on intake of EtOH, water, or nicotine when stable responding was reached in the final phase of the experiment (phase 3), as described below. Stability in responding was defined as no significant difference in average EtOH consumption, water consumption, or nicotine intake across five sessions.
Concurrent access (phase 3)
During phase 3, the FR5 schedule for nicotine infusions remained as described in phase 2, while access to 15% EtOH and water bottles (alternated daily between the left and right side of the chamber wall) was returned to the operant sessions (for the animals that underwent phase 2 without bottle access (n = 12); see above). During phase 3, water again was removed from the home cage as in phase 1, and food provision (12–15 g per day) continued as in phase 2. Each rat underwent at least ten consecutive training sessions (with no significant differences in average daily EtOH consumption, water consumption, or nicotine intake across five sessions; ~ 10 days) in this phase prior to beginning drug pretreatment testing.
Drug pretreatments
For animals in experiment 1, drug pretreatments began after operant responding and drinking stabilized in phase 3 (after at least ten sessions and with no significant differences in average daily EtOH consumption, water consumption, or nicotine intake across five sessions; ~ 14–20 days). Each drug was prepared fresh prior to administration and was given 15 min prior to the start of the testing session. For varenicline, the test dose was 3 mg/kg; for r-bPiDI, the test doses were 10 or 20 mg/kg; and for RMOD, the test doses were 30, 56, or 100 mg/kg. Each drug dose was given in counterbalanced order, including the appropriate vehicle control. A minimum of two maintenance sessions (no pretreatment) separated each dose or drug pretreatment test session.
Experiment 2: drug pretreatments during use of EtOH only (phase 1)
Animals in this experiment were trained under the same procedures described for EtOH acclimation (pre-training) and EtOH access (phase 1). Drug pretreatments began on day 15 of phase 1. After EtOH consumption stabilized (after at least ten sessions and with no significant differences in average daily EtOH or water consumption across five consecutive sessions; 15 days), drug treatments began using the same doses and procedure as described in experiment 1.
Data analysis
For both experiments, consumption from the EtOH and water bottles were measured in g per kg body weight. For EtOH, the weight of liquid consumed during each session was converted to g of EtOH by multiplying the specific gravity of EtOH by the concentration of EtOH used (15% v/v/kg body weight/session). For experiment 1, active and inactive lever presses for nicotine infusions were recorded by the automated system used to operate the operant chambers (ENV-001; MED Associates, St. Albans, VT). Consumption differences of EtOH and nicotine, averaged across the last 3 days of each experiment phase, were analyzed by two-tailed t tests. A Pearson correlation analysis was used to analyze the association between EtOH intake and nicotine infusions.
Effects of varenicline on EtOH and water consumption and on lever presses for nicotine (active vs. inactive) earned during concurrent access sessions, were analyzed by two-tailed paired t test analyses (vehicle vs. drug for each operant lever). Effects of r-bPiDI and RMOD on EtOH and water consumption (experiments 1 and 2), and lever presses for nicotine (active vs. inactive) earned during concurrent access sessions (experiment 1), were analyzed by one-way, repeated-measures ANOVA. Post hoc analyses using Dunnett’s test comparing each dose against the vehicle control (α = 0.05), were conducted when appropriate. All statistical analyses were conducted using Prism 5.0 (Graph Pad Software Inc., San Diego, CA). Within-session effects of varenicline, r-bPiDI, and RMOD on the number of nicotine infusions earned across10-min intervals were analyzed by mixed model ANOVAs and post hoc analyses were conducted using subsequent Bonferroni posttests where appropriate (α = 0.05).
Results
Experiment 1: pretreatments during co-use of EtOH and nicotine
Initial training
Acquisition across sessions for baseline levels of EtOH consumption, water consumption, active lever presses, and inactive lever presses for nicotine across phases 1–3 are shown in Fig. 2. In phase 1 (EtOH alone), both EtOH and water consumption gradually increased across the sessions (Fig. 2a, c); for EtOH F(13, 312) = 3.92, p < 0.05 and for water F(13, 312) = 4.19, p < 0.05. However, both EtOH and water consumption eventually stabilized, as there were no significant differences in consumption across the last four sessions. In phase 2 (nicotine alone), active lever pressing increased as the FR requirement increased and became stable across the last three FR5 sessions of this phase (Fig. 2e); across all sessions F(10, 131) = 51.72, p < 0.05. In phase 3 (EtOH + nicotine), EtOH consumption increased across sessions, F(13, 237) = 2.10, p < 0.05 (Fig. 2b), while water consumption, active lever presses, and inactive lever presses did not change significantly across sessions (Fig. 2d, f).
Experiment 1 acquisition across sessions for a EtOH consumption in phase 1 (EtOH alone), b EtOH consumption in phase 3 (EtOH + nicotine), c water consumption in phase 1 (EtOH alone), d water consumption in phase 3 (EtOH + nicotine), e number of active and inactive lever presses for nicotine in phase 2 (nicotine alone), and f number of active vs. inactive lever presses for nicotine in phase 3 (EtOH + nicotine). Values represent mean ± SEM
A direct comparison of the average baseline levels of EtOH consumption, water consumption, active lever presses, and inactive lever presses collapsed across the last three sessions within each of the phases 1–3 are shown in Fig. 3. Results from a two-tailed paired t test showed that there was a significant decrease in EtOH consumption between phase 1 (EtOH alone) to phase 3 (EtOH + nicotine); t(2) = 10.25, p < 0.05 (Fig. 3a). Similarly, there was a significant decrease in water consumption from phase 1 to phase 3; t(2) = 5.29, p < 0.05 (Fig. 3b). In contrast, there was a significant increase in nicotine infusions from phase 2 (nicotine alone) to phase 3 (EtOH + nicotine); t(2) = 7.09, p < 0.05 (Fig. 3c). Additionally, across individual rats, there was a significant negative correlation between EtOH consumption and nicotine infusions during phase 3, r = − 0.58, p < 0.05 (see Fig. 4).
Experiment 1 total intake across the access phases. Graphs depict average intake differences for a EtOH consumption in phase 1 (EtOH alone) vs. phase 3 (EtOH + nicotine), b water consumption in phase 1 vs. phase 3, and c number of infusions of nicotine in phase 2 (nicotine alone) vs. phase 3. Values represent mean ± SEM. *p < 0.05 vs. phase 1 or 2
Blood EtOH concentrations
Figure 5 shows BECs in phases 1 and 3. Consistent with the decrease in EtOH consumption, there was a significant decrease in BEC in phase 3 (EtOH + nicotine) versus phase 1 (EtOH alone); t(23) = 4.63, p < 0.01.
Effect of varenicline pretreatment
Figure 6 shows EtOH consumption, water consumption, active lever presses for nicotine, and inactive lever presses after varenicline pretreatment in phase 3 (n = 5). Analyses for phase 3 revealed that varenicline had no significant effect on EtOH consumption (Fig. 6a). While water consumption was increased slightly by varenicline, this effect was not statistically significant (Fig. 6b). In contrast to liquid consumption, the number of active lever presses for nicotine was significantly reduced by varenicline (3 mg/kg) compared to vehicle; t(4) = 2.83, p < 0.05 (Fig. 6c). However, varenicline did not significantly alter the number of inactive lever presses (Fig. 6d).
Experiment 1 pretreatment with varenicline (0 and 3 mg/kg) in phase 3 (EtOH + nicotine) (n = 5). Graphs depict the effects of varenicline on a EtOH consumption, b water consumption, c number of active lever presses for nicotine, and d number of inactive lever presses. Values represent mean ± SEM. *p < 0.05 vs. vehicle (0)
Effect r-bPiDI pretreatment
Figure 7 shows EtOH consumption, water consumption, active lever presses for nicotine, and inactive lever presses after r-bPiDI pretreatment in phase 3 (n = 17). Analyses revealed there was no significant effect of r-bPiDI on EtOH consumption or inactive lever presses at either dose (Fig. 7a, d). However, there was a significant effect of r-bPiDI pretreatment on water consumption, F(2,16) = 5.37, p < 0.05 (Fig. 7b). Subsequent Dunnett’s tests revealed that water consumption significantly increased at 20 mg/kg r-bPiDI compared to vehicle control. Analyses also revealed a significant effect of r-bPiDI treatment on active lever presses, F(2,16) = 4.28, p < 0.05 (Fig. 7c). Subsequent Dunnett’s tests revealed that active lever presses for nicotine significantly decreased at 20 mg/kg r-bPiDI compared to vehicle control.
Experiment 1 pretreatment with r-bPiDI (0, 10, and 20 mg/kg) in phase 3 (EtOH + nicotine) (n = 17). Graphs depict the effects of r-bPiDI on a EtOH consumption, b water consumption, c number of active lever presses for nicotine, and d number of inactive lever presses. Values represent mean ± SEM. *p < 0.05 vs. vehicle (0)
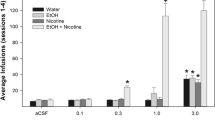
Effect of RMOD pretreatment
Figure 8 shows EtOH consumption, water consumption, active lever presses for nicotine, and inactive lever presses after RMOD pretreatment in phase 3 (n = 5). Analyses revealed no significant effect of RMOD on either EtOH or water consumption (Fig. 8a, b), and there was no significant effect of RMOD on inactive lever presses (Fig. 8d). Analyses revealed a significant effect of RMOD on active lever presses, F(3, 12) = 4.77, p < 0.05 (Fig. 8c), with a subsequent Dunnett’s test showing a significant decrease in active lever presses following 100 mg/kg RMOD compared to vehicle.
Experiment 1 pretreatment with RMOD (0, 30, and 56 mg/kg) in phase 3 (EtOH + nicotine) (n = 5). Graphs depict the effects of RMOD on a EtOH consumption, b water consumption, c number of active lever presses for nicotine, and d number of inactive lever presses. Values represent mean ± SEM. *p < 0.05 vs. vehicle (0)
Within-session nicotine SA
Figure 9 shows the number of active lever presses for nicotine in 10-min intervals during the concurrent access phase (phase 3). Analyses for varenicline revealed a significant main effect for dose, F(1, 8) = 7.80, p < 0.05, and a significant interaction, F(5, 8) = 8.18, p < 0.05. Subsequent Bonferroni posttests revealed a significant difference in responding between vehicle and 3.0 mg/kg varenicline during the first 10-min interval, t(40) = 6.14, p < 0.05 (Fig. 9a). Analyses for r-bPiDI revealed a significant main effect for interval, F(5, 48) = 28.93, p < 0.05, with no significance shown by the Bonferroni posttest (Fig. 9b). Analyses for RMOD showed a significant main effect for dose, F(3, 35) = 4.75, p < 0.05, a significant main effect for interval, F(5, 35) = 3.18, p < 0.05, and a significant interaction, F(15, 35) = 1.72, p < 0.05. Subsequent Bonferroni posttest revealed significant differences in responding during the first 10-min interval for 30, 56, and 100 mg/kg RMOD (t(175) = 2.71, p < 0.05; t(175) = 2.94, p < 0.05; t(175) = 5.18, p < 0.05, respectively) compared to vehicle. Additionally, analyses revealed a significant difference in responding for nicotine at 100 mg/kg RMOD during the 20-min interval compared to vehicle, t(175) = 3.02, p < 0.05 (Fig. 9c). As there was no automated system to keep track of EtOH consumption rates, we are unable to provide this within-session data for EtOH.
Experiment 2: pretreatments during use of EtOH only
Since EtOH use was low during the co-use phase (experiment 1), this experiment tested the same drug pretreatments during phase 1, when use of EtOH was relatively higher. Figure 10 shows EtOH consumption and water consumption for experiment 2 (n = 8) following drug pretreatments. Analyses revealed that varenicline (3 mg/kg) had no significant effect on EtOH consumption (Fig. 10a). However, water consumption was significantly increased at this dose, t(7) = 4.30, p < 0.05 (Fig. 10b). Analyses also revealed that r-bPiDI had no significant effect on EtOH consumption or water consumption (Fig. 10c, d). For RMOD pretreatment, analyses revealed a significant effect of RMOD on EtOH consumption, F(3, 21) = 14.97, p < 0.05 (Fig. 10e), with subsequent Dunnett’s test showing a significant decrease in EtOH consumption following 100 mg/kg RMOD compared to vehicle. There was no effect of any dose of RMOD on water consumption (Fig. 10f).
Experiment 2 pretreatment with varenicline (0 and 3 mg/kg), r-bPiDI (0, 10, and 20 mg/kg), and RMOD (0, 30, and 56 mg/kg) in phase 3 (n = 8). Graphs depict the effects of varenicline on a EtOH consumption and b water consumption, the effects of r-bPiDI on c EtOH consumption and d water consumption, and the effects of RMOD on e EtOH consumption and f water consumption. Values represent mean ± SEM. *p < 0.05 vs. vehicle (0)
Discussion
The current study used a novel model of EtOH and nicotine co-use in female P rats to assess the effects of varenicline, r-bPiDI, and RMOD on co-use behavior. In this study, the two-bottle and two-lever choice model allowed access to both EtOH and nicotine concurrently. However, in contrast to a previous co-use model (Lê et al. 2010), the current model also measured choice for a natural reward (water), as well as nonreinforced operant behavior (inactive lever pressing), thus allowing for assessment of nonspecific changes in ongoing behavior following pharmacotherapeutic pretreatments. With this new model, abuse-relevant levels of EtOH and nicotine intake were achieved when each substance was given alone. However, during the co-use phase (phase 3), nicotine intake increased and EtOH intake decreased relative to the intake of each substance alone, consistent with results from previous co-use models (Funk et al. 2016; Scuppa et al. 2015).
When EtOH was given alone (phase 1), rats voluntarily consumed ~ 1.6 g/kg/h, which is comparable to binge drinking five to six standard alcoholic beverages for humans (Grant and Bennett 2003; McKee et al. 2008; Udo et al. 2013). This amount of EtOH consumption produced a BEC of ~ 85 mg/dL paralleling our previous work (Bell et al. 2011), just above the definition of intoxication to impairment (National Institute on Alcohol Abuse and Alcoholism, 2017). Additionally, the P rats used in this study were selectively bred, generations 79–83. Results from previous research show that adult female P rats from generations 66–69 also consume approximately 1.6 g/kg/h of EtOH (Bell et al. 2011), indicating consistent levels of EtOH drinking across a range of P rat generations.
For nicotine, rats in the current study show rates of nicotine self-administration during both the nicotine access phase (~ 19 infusions of 0.03 mg/kg i.v. nicotine) and the concurrent access phase (~ 22 infusions of 0.03 mg/kg i.v. nicotine) that are comparable to those seen in a previous study by Lê et al. (2006), showing nicotine self-administration rates of ~ 20–25 infusions of 0.03 mg/kg i.v. nicotine in 44th generation selectively bred P rats. For nicotine, substantial intake is considered to be ~ 0.5 mg/kg/h i.v. nicotine (16 infusions of 0.03 mg/kg nicotine), as this amount of intake is sufficient to produce pharmacologically relevant levels of nicotine and cotinine in plasma (Corrigall 1992; Corrigall and Coen 1989; Shoaib and Stolerman 1992). The steady-state-peak plasma levels of nicotine seen in humans are on average 40 ng/mL (Yamazaki et al. 2010). In rats, it has been determined that 0.5 mg/kg/h of i.v. nicotine results in ~ 65.4 ng/mL of plasma nicotine (Shoaib and Stolerman 1992). Rats in the current study averaged ~ 0.65 mg/kg/h of i.v. nicotine, enough to exceed pharmacologically relevant levels of plasma nicotine. Taken together, these results show that there is consistency in EtOH and nicotine intake across a wide range of selectively bred P rats, providing support for using P rats in the development of a translational model of EtOH and nicotine co-use.
One limitation to the co-use model described here relates to the relatively low EtOH consumption during the concurrent access phase (phase 3). In contrast to the drinking levels during the EtOH access phase (phase 1), when EtOH and nicotine were given concurrently (phase 3), EtOH consumption was only ~ 0.5 g/kg/h, which achieved an average BEC of only ~ 25 mg/dL. This amount is comparable to humans drinking approximately two standard alcoholic beverages/h (Grant and Bennett 2003; McKee et al. 2008; Udo et al. 2013). Nonetheless, the decrease in EtOH intake in the presence of nicotine availability is consistent with previous concurrent access studies (Funk et al. 2016; Scuppa et al. 2015). Interestingly, however, the decrease in EtOH consumption in the presence of nicotine in the current study was greater than that observed previously (Funk et al. 2016; Scuppa et al. 2015). This may reflect a difference between P rats (current study) versus Marchigian Sardinian alcohol-preferring (msP) and Wistar rats (previous studies). Alternatively, in contrast to those previous studies that used a two-lever choice procedure (EtOH vs. nicotine), the current study included water, a natural reinforcer. Based on the notion of response competition among multiple drug and nondrug reinforcers (Carroll et al. 1991), the inclusion of both nicotine and water as alternative reinforcers may have been responsible for the greater suppression of EtOH consumption observed here.
The current results also show a significant increase in nicotine intake when EtOH is concurrently available. While this finding is consistent with clinical evidence that EtOH increases cigarette smoking (Henningfield et al. 1984; McKee et al. 2009; Mello et al. 1980), it conflicts with preclinical studies showing a decrease in nicotine self-administration when EtOH is available concurrently (Funk et al. 2016; Scuppa et al. 2015). In contrast to those previous preclinical studies, however, it is notable that the rate of nicotine self-administration in the absence of EtOH in the current study was higher than the rates reported by Scuppa et al. (2015) and Funk et al. (2016). These differences across studies reflect, at least in part, strain and/or sex differences because the current study used female P rats, whereas the study by Scuppa et al. (2015) used selective bred male msP rats and the study by Funk et al. (2016) used outbred male Wistar rats. Previous work has shown that P rats self-administer nicotine at higher rates than Wistar rats (Lê et al. 2006) and that females acquire nicotine self-administration and show more motivation for nicotine compared to males (Donny et al. 2000). Thus, the EtOH-induced increase in nicotine self-administration observed here may be unique to female P rats when compared to other breeds. Importantly, as previously stated, EtOH-induced increases in nicotine intake have been observed in humans (Henningfield et al. 1984; McKee et al. 2009; Mello et al. 1980), which suggests that female P rats display characteristics that more closely mimic the human condition, making them a better model for human behavior.
When tested during the co-use phase, varenicline specifically decreased nicotine-reinforced lever pressing, without altering inactive lever pressing, EtOH consumption or water consumption. Although several studies have demonstrated that varenicline reduces EtOH consumption in humans (Falk et al. 2015; Litten et al. 2013; McKee et al. 2013), conflicting evidence for the effects of varenicline on EtOH craving and consumption has been reported (de Bejczy et al. 2015; Schacht et al. 2014; Verplaetse et al. 2016). In conflict with the results of the current study, several preclinical studies have also demonstrated that pretreatment with varenicline reduces EtOH consumption in rodents (Froehlich et al. 2017; Kamens et al. 2010; Sotomayor-Zarate et al. 2013; Steensland et al. 2007) when EtOH was available in the absence of nicotine. This may be explained by the different breeds used by Kamens et al. (2010), Sotomayor-Zarate et al. (2013), and Steensland et al. (2007). Additionally, in the study by Froehlich et al. (Alcohol Facts and Statistics, n.d.), EtOH consumption in male P rats (78th generation) was reduced by varenicline. However, these pretreatments occurred daily for 5 days, while the pretreatments in the current study were only given to females on 1 day. It is possible that the differences seen in the current study were due to the acute administration vs. chronic administration of varenicline.
Furthermore, in preclinical examinations of co-use of EtOH and nicotine, there is conflicting evidence of the effectiveness of varenicline in reducing EtOH consumption in rodents (Funk et al. 2016; Randall et al. 2015; Scuppa et al. 2015). Among the three preclinical studies that have examined the effects of varenicline on EtOH and nicotine co-use, only one study reported that varenicline significantly decreased both nicotine and EtOH self-administration during concurrent access (Cippitelli et al. 2015). In contrast, the two other studies showed that varenicline decreased nicotine self-administration, but not EtOH self-administration (Funk et al. 2016; Scuppa et al. 2015), a finding that is corroborated by the current results. Thus, on balance, while it is possible that EtOH consumption levels were too low to detect significant effects of pretreatment, preclinical evidence to date does not support the utility of varenicline as a pharmacotherapeutic for heavy drinking tobacco smokers.
One caveat to this experiment is that only one dose of varenicline (3.0 mg/kg) was tested. While Cippitelli et al. (2015) found that varenicline reduced EtOH consumption at 1.5 mg/kg, Scuppa et al. (2015) found that a higher dose of 3 mg/kg had no effect on EtOH consumption and results from Funk et al. (2016) show that 3 mg/kg varenicline reduced both EtOH consumption and food intake. These results indicate that perhaps a lower dose of varenicline could be more effective for reducing EtOH consumption in co-use models, but more research is needed.
When tested in the co-use phase, like varenicline, r-bPiDI decreased nicotine SA, but not EtOH consumption. The decrease in nicotine self-administration was expected based on the findings of a previous report (Beckmann et al. 2015). These results, in combination with previous investigations of the neuropharmacology of r-bPiDI, suggest that α6β2* nAChRs play an important role in the maintenance of nicotine intake, but not EtOH intake. Additionally, the decrease in nicotine-evoked DA release produced by r-bPiDI is likely to contribute, at least in part, to the decrease in nicotine self-administration produced by r-bPiDI (Beckmann et al. 2015). While other less selective nAChR antagonists, such as mecamylamine, decrease nicotine self-administration, cue-induced reinstatement, and nicotine-seeking behavior in animals (DeNoble and Mele 2006; Glick et al. 1996) and in humans when combined with a transdermal nicotine patch (Rose 2006; Rose 2008; Rose et al. 1994), they can also produce aversive peripheral side effects, which limits their success in clinical trials (Bevins and Caggiula 2009; Shytle et al. 2002). The selectivity of r-bPiDI for central α6β2* nAChRs may eliminate problems with peripheral side effects seen with previously tested nAChR antagonists, but further research is needed.
The failure of r-bPiDI to decrease EtOH consumption in the current study is inconsistent with a study by Srisontiyakul et al. (2016). Importantly, however, the study by Srisontiyakul et al. used the quaternary ammonium bPiDI (N,N-decane-1,10-diyl-bis-3-picolinium diiodide), whereas the current study used the neutral chemically reduced, tertiary amino derivative of bPiDI (i.e., r-bPiDI) which presumably allows for greater bioavailability and blood-brain barrier penetration. These findings suggest that while α6β2* nAChRs may be involved in both nicotine and EtOH maintenance, it is possible that there are important pharmacokinetic and/or pharmacodynamic differences between the actions of bPiDI and r-bPiDI affecting these behaviors. Unfortunately, beyond the current study, there are no other studies on the effects of these compounds on EtOH and nicotine co-use.
Further, when tested in the co-use phase, like varenicline and r-bPiDI, RMOD decreased nicotine self-administration, but not EtOH consumption. This finding is consistent with previous research showing that RMOD decreases nicotine self-administration using P rats (Wang et al. 2015). These effects are likely due, at least in part, to RMOD binding to DAT and thereby preventing nicotine-induced dopamine release in Acb (Wang et al. 2015), an action that also is seen with r-bPiDI (Beckmann et al. 2015). Further examination of RMOD using electrophysiology has shown slowed dopamine neuron firing in a dopamine D2 receptor-dependent manner, which may also relate to its nicotine self-administration decreasing effects (Avelar et al. 2017). Taken together, these results suggest that nicotine-induced dopamine release plays an important role in the maintenance of nicotine self-administration and that blocking this dopamine release is an effective method for reducing nicotine reinforcement. Clearly, pharmacotherapeutic agents that act to block nicotine-induced dopamine release merit further exploration as potential smoking cessation treatments.
To our knowledge, there have been no other investigations of the effects of RMOD on EtOH intake. We hypothesized that the atypical DAT blocker RMOD would decrease EtOH intake based on previous findings demonstrating that EtOH potentiates DAT function and increases DAT expression in cell-based models (Mayfield et al. 2001; Methner and Mayfield 2010; Riherd et al. 2008). Additionally, work with rats selectively bred for high EtOH consumption has revealed that chronic EtOH intake increases dopamine reuptake in Acb of both P (Sahr et al. 2004) and high alcohol-drinking HAD1 rats (Carroll et al. 2006). Consistent with our hypothesis, RMOD decreased EtOH intake during phase 1 when nicotine access was not available, however, RMOD failed to decrease EtOH consumption when both EtOH and nicotine were available concurrently. This suggests that this DAT modulator may not be a viable pharmacotherapy to treat co-use of EtOH and nicotine, but it may be a viable option for treatment EtOH use in individuals who are not smokers. Alternatively, results from the triple monoamine uptake inhibitor, amitifadine, show robust decreases in both nicotine self-administration (Levin et al. 2015) and EtOH self-administration or drinking (O’Tousa et al. 2015; Warnock et al. 2012) when tested separately. It remains to be determined if blockade of multiple monoamine transporters would be effective in an EtOH and nicotine co-use model.
Given that concurrent access makes it difficult to disentangle the time course that each reinforcer is self-administered, it may be that EtOH consumption was initiated before nicotine self-administration, which would be consistent with previous research and descriptions of EtOH “loading” at the beginning of EtOH self-administration sessions (Williams and Broadbridge 2009). Subsequently, the rats may have focused on the more salient interoceptive cues of intravenous nicotine relative to EtOH consumption. Conversely, it may be that EtOH consumption and/or its cues enhanced nicotine self-administration. This latter hypothesis has some support from the literature, such that co-administration of EtOH and nicotine produces an additive effect on their reinforcing effects and associated dopamine release in nucleus accumbens (Acb) (Ericson et al. 2009; Sajja et al. 2010; Sajja and Rahman 2012; Tizabi et al. 2007). Furthermore, results from within-session interval data in the current study show that following pretreatment with vehicle, lever pressing for nicotine is highest during the first 10-min interval, and decreases to a steady level for the rest of the 1-h session. Interestingly, lever pressing for nicotine was significantly decreased during the first 10-min interval following pretreatment with varenicline (3 mg/kg) and RMOD (30, 56, and 100 mg/kg), with suppression of responding for nicotine continuing into the 20-min interval for only the highest dose of RMOD. These results show that overall decreases in nicotine intake are primarily due to the decreases in responding during the first 10-min interval of the session.
In summary, toward the development of a preclinical model for screening potential pharmacotherapies for EtOH and nicotine co-use, the novel model used here offers the advantage of including control for nonspecific suppression of behavior (i.e., water consumption and non-reinforced lever pressing). However, relatively low levels of EtOH consumption were obtained during the EtOH and nicotine co-use phase. With the drugs tested in this model, varenicline, r-bPiDI, and RMOD all reduced nicotine self-administration, but not EtOH consumption during the co-use phase, while producing no significant suppressant effect within the dose ranges tested. Interestingly, although RMOD did not decrease EtOH consumption during concurrent access, EtOH consumption was significantly decreased when EtOH was available alone. These results indicate that therapeutics which may be useful for smoking cessation via selective inhibition of α4β2* or α6β2* nAChRs, or DAT inhibition as afforded by the atypical inhibitor RMOD, may not be sufficient to treat EtOH and nicotine co-use. Further optimization of the current co-use model will be beneficial for assessing novel medications that may be effective in treating tobacco smokers who are heavy drinkers.
References
Alcohol Facts and Statistics. In: Alcoholism NIoAAa (ed). U.S. Department of Health and Human Services, June 2017, www.niaaa.nih.gov
Avelar AJ, Cao J, Newman AH, Beckstead MJ (2017) Atypical dopamine transporter inhibitors R-modafinil and JHW 007 differentially affect D2 autoreceptor neurotransmission and the firing rate of midbrain dopamine neurons. Neuropharmacology 123:410–419
Bardo MT, Green TA, Crooks PA, Dwoskin LP (1999) Nornicotine is self-administered intravenously by rats. Psychopharmacology 146:290–296
Barkley-Levenson AM, Crabbe JC (2014) High drinking in the dark mice: a genetic model of drinking to intoxication. Alcohol (Fayetteville, NY) 48:217–223
Beckmann JS, Meyer AC, Pivavarchyk M, Horton DB, Zheng G, Smith AM, Wooters TE, McIntosh JM, Crooks PA, Bardo MT, Dwoskin LP (2015) r-bPiDI, an alpha6beta2* nicotinic receptor antagonist, decreases nicotine-evoked dopamine release and nicotine reinforcement. Neurochem Res 40:2121–2130
de Bejczy A, Lof E, Walther L, Guterstam J, Hammarberg A, Asanovska G, Franck J, Isaksson A, Soderpalm B (2015) Varenicline for treatment of alcohol dependence: a randomized, placebo-controlled trial. Alcohol Clin Exp Res 39:2189–2199
Bell RL, Rodd ZA, Smith RJ, Toalston JE, Franklin KM, McBride WJ (2011) Modeling binge-like ethanol drinking by peri-adolescent and adult P rats. Pharmacol Biochem Behav 100:90–97
Bell RL, Sable HJ, Colombo G, Hyytia P, Rodd ZA, Lumeng L (2012) Animal models for medications development targeting alcohol abuse using selectively bred rat lines: neurobiological and pharmacological validity. Pharmacol Biochem Behav 103:119–155
Bell RL, Hauser S, Rodd ZA, Liang T, Sari Y, McClintick J, Rahman S, Engleman EA (2016) A genetic animal model of alcoholism for screening medications to treat addiction. Int Rev Neurobiol 126:179–261
Bevins RA, Caggiula AR (2009) The motivational impact of nicotine and its role in tobacco use. Springer
Carroll ME, Carmona GG, May SA (1991) Modifying drug-reinforced behavior by altering the economic conditions of the drug and a nondrug reinforcer. J Exp Anal Behav 56:361–376
Carroll MR, Rodd ZA, Murphy JM, Simon JR (2006) Chronic ethanol consumption increases dopamine uptake in the nucleus accumbens of high alcohol drinking rats. Alcohol (Fayetteville, NY) 40:103–109
Chiappetta V, Garcia-Rodriguez O, Jin CJ, Secades-Villa R, Blanco C (2014) Predictors of quit attempts and successful quit attempts among individuals with alcohol use disorders in a nationally representative sample. Drug Alcohol Depend 141:138–144
Cicero TJ, Smithloff BR (1973) Alcohol oral self-administration in rats: attempts to elicit excessive intake and dependence. Alcohol Intoxication and Withdrawal I Springer:213–224
Cippitelli A, Wu J, Gaiolini KA, Mercatelli D, Schoch J, Gorman M, Ramirez A, Ciccocioppo R, Khroyan TV, Yasuda D, Zaveri NT, Pascual C, Xie X, Toll L (2015) AT-1001: a high-affinity α3β4 nAChR ligand with novel nicotine-suppressive pharmacology. Br J Pharmacol 172:1834–1845
Corrigall WA (1992) A rodent model for nicotine self-administration. Animal models of drug addiction:315–344
Corrigall WA, Coen KM (1989) Nicotine maintains robust self-administration in rats on a limited-access schedule. Psychopharmacology 99:473–478
DeNoble VJ, Mele PC (2006) Intravenous nicotine self-administration in rats: effects of mecamylamine, hexamethonium and naloxone. Psychopharmacology 184:266–272
Donny EC, Caggiula AR, Rowell PP, Gharib MA, Maldovan V, Booth S, Mielke MM, Hoffman A, McCallum S (2000) Nicotine self-administration in rats: estrous cycle effects, sex differences and nicotinic receptor binding. Psychopharmacology 151:392–405
Ebbert JO, Croghan IT, Hurt RT, Schroeder DR, Hays JT (2016) Varenicline for smoking cessation in light smokers. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco 18:2031–2035
Ericson M, Lof E, Stomberg R, Soderpalm B (2009) The smoking cessation medication varenicline attenuates alcohol and nicotine interactions in the rat mesolimbic dopamine system. J Pharmacol Exp Ther 329:225–230
Falk DE, Yi HY, Hiller-Sturmhofel S (2006) An epidemiologic analysis of co-occurring alcohol and tobacco use and disorders: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Alcohol research & health : the journal of the National Institute on Alcohol Abuse and Alcoholism 29:162–171
Falk DE, Castle IJ, Ryan M, Fertig J, Litten RZ (2015) Moderators of varenicline treatment effects in a double-blind, placebo-controlled trial for alcohol dependence: an exploratory analysis. J Addict Med 9:296–303
Feduccia AA, Simms JA, Mill D, Yi HY, Bartlett SE (2014) Varenicline decreases ethanol intake and increases dopamine release via neuronal nicotinic acetylcholine receptors in the nucleus accumbens. Br J Pharmacol 171:3420–3431
Froehlich JC, Nicholson ER, Dilley JE, Filosa NJ, Rademacher LC, Smith TN (2017) Varenicline reduces alcohol intake during repeated cycles of alcohol reaccess following deprivation in alcohol-preferring (P) rats. Alcohol Clin Exp Res 41:1510–1517
Funk D, Lo S, Coen K, Le AD (2016) Effects of varenicline on operant self-administration of alcohol and/or nicotine in a rat model of co-abuse. Behav Brain Res 296:157–162
George O, Lloyd A, Carroll FI, Damaj MI, Koob GF (2011) Varenicline blocks nicotine intake in rats with extended access to nicotine self-administration. Psychopharmacology 213:715–722
Glick S, Visker K, Maisonneuve I (1996) An oral self-administration model of nicotine preference in rats: effects of mecamylamine. Psychopharmacology 128:426–431
Gonzales D, Rennard SI, Nides M, Oncken C, Azoulay S, Billing CB, Watsky EJ, Gong J, Williams KE, Reeves KR (2006) Varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, vs sustained-release bupropion and placebo for smoking cessation: a randomized controlled trial. Jama 296:47–55
Grant KA, Bennett AJ (2003) Advances in nonhuman primate alcohol abuse and alcoholism research. Pharmacol Ther 100:235–255
Henningfield JE, Chait LD, Griffiths RR (1984) Effects of ethanol on cigarette smoking by volunteers without histories of alcoholism. Psychopharmacology 82:1–5
Jorenby DE, Hays J, Rigotti NA et al (2006) Efficacy of varenicline, an α4β2 nicotinic acetylcholine receptor partial agonist, vs placebo or sustained-release bupropion for smoking cessation: a randomized controlled trial. Jama 296:56–63
Kamens HM, Andersen J, Picciotto MR (2010) Modulation of ethanol consumption by genetic and pharmacological manipulation of nicotinic acetylcholine receptors in mice. Psychopharmacology 208:613–626
Koob GF, Kenneth Lloyd G, Mason BJ (2009) Development of pharmacotherapies for drug addiction: a Rosetta stone approach. Nat Rev Drug Discov 8:500–515
Lê AD, Li Z, Funk D, Shram M, Li TK, Shaham Y (2006) Increased vulnerability to nicotine self-administration and relapse in alcohol-naive offspring of rats selectively bred for high alcohol intake. J Neurosci : Off J Soc Neurosci 26:1872–1879
Lê AD, Lo S, Harding S, Juzytsch W, Marinelli PW, Funk D (2010) Coadministration of intravenous nicotine and oral alcohol in rats. Psychopharmacology 208:475–486
Lester D, Freed EX (1973) Criteria for an animal model of alcoholism. Pharmacol Biochem Behav 1:103–107
Levin ED, Wells C, Johnson JE, Rezvani AH, Bymaster FP, Rose JE (2015) Amitifadine, a triple monoamine re-uptake inhibitor, reduces nicotine self-administration in female rats. Eur J Pharmacol 764:30–37
Litten RZ, Ryan ML, Fertig JB, Falk DE, Johnson B, Dunn KE, Green AI, Pettinati HM, Ciraulo DA, Sarid-Segal O, Kampman K, Brunette MF, Strain EC, Tiouririne NA, Ransom J, Scott C, Stout R (2013) A double-blind, placebo-controlled trial assessing the efficacy of varenicline tartrate for alcohol dependence. J Addict Med 7:277–286
Mayfield RD, Maiya R, Keller D, Zahniser NR (2001) Ethanol potentiates the function of the human dopamine transporter expressed in Xenopus oocytes. J Neurochem 79:1070–1079
McBride WJ, Rodd ZA, Bell RL, Lumeng L, Li TK (2014) The alcohol-preferring (P) and high-alcohol-drinking (HAD) rats—animal models of alcoholism. Alcohol (Fayetteville, NY) 48:209–215
McKee SA, Weinberger AH (2013) How can we use our knowledge of alcohol-tobacco interactions to reduce alcohol use? Annu Rev Clin Psychol 9:649–674
McKee SA, O'Malley SS, Shi J, Mase T, Krishnan-Sarin S (2008) Effect of transdermal nicotine replacement on alcohol responses and alcohol self-administration. Psychopharmacology 196:189–200
McKee SA, Harrison EL, O'Malley SS, Krishnan-Sarin S, Shi J, Tetrault JM, Picciotto MR, Petrakis IL, Estevez N, Balchunas E (2009) Varenicline reduces alcohol self-administration in heavy-drinking smokers. Biol Psychiatry 66:185–190
McKee SA, Young-Wolff KC, Harrison EL, Cummings KM, Borland R, Kahler CW, Fong GT, Hyland A (2013) Longitudinal associations between smoking cessation medications and alcohol consumption among smokers in the International Tobacco Control Four Country survey. Alcohol Clin Exp Res 37:804–810
Mello NK, Mendelson JH, Sellers ML, Kuehnle JC (1980) Effect of alcohol and marihuana on tobacco smoking. Clin Pharmacol Ther 27:202–209
Methner DNR, Mayfield RD (2010) Ethanol alters endosomal recycling of human dopamine transporters. J Biol Chem 285:10310–10317
Mokdad AH, Marks JS, Stroup DF, Gerberding JL (2004) Actual causes of death in the United States, 2000. JAMA 291:1238–1245
National Institute on Alcoholism and Alcohol Abuse (2017) Alcohol facts and statistics. https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/alcohol-facts-and-statistics. Accessed 16 February 2018
Nides M, Oncken C, Gonzales D, Rennard S, Watsky EJ, Anziano R, Reeves KR (2006) Smoking cessation with varenicline, a selective alpha4beta2 nicotinic receptor partial agonist: results from a 7-week, randomized, placebo- and bupropion-controlled trial with 1-year follow-up. Arch Intern Med 166:1561–1568
O’Connor EC, Parker D, Rollema H, Mead AN (2010) The α4β2 nicotinic acetylcholine-receptor partial agonist varenicline inhibits both nicotine self-administration following repeated dosing and reinstatement of nicotine seeking in rats. Psychopharmacology 208:365–376
O'Tousa DS, Warnock KT, Matson LM, Namjoshi OA, Linn MV, Tiruveedhula VV, Halcomb ME, Cook J, Grahame NJ, June HL (2015) Triple monoamine uptake inhibitors demonstrate a pharmacologic association between excessive drinking and impulsivity in high-alcohol-preferring (HAP) mice. Addict Biol 20:236–247
Plebani JG, Lynch KG, Rennert L, Pettinati HM, O'Brien CP, Kampman KM (2013) Results from a pilot clinical trial of varenicline for the treatment of alcohol dependence. Drug Alcohol Depend 133:754–758
Randall PA, Jaramillo AA, Frisbee S, Besheer J (2015) The role of varenicline on alcohol-primed self-administration and seeking behavior in rats. Psychopharmacology 232:2443–2454
Rezvani AH, Slade S, Wells C, Petro A, Lumeng L, Li TK, Xiao Y, Brown ML, Paige MA, McDowell BE, Rose JE, Kellar KJ, Levin ED (2010) Effects of sazetidine-A, a selective alpha4beta2 nicotinic acetylcholine receptor desensitizing agent on alcohol and nicotine self-administration in selectively bred alcohol-preferring (P) rats. Psychopharmacology 211:161–174
Riherd DN, Galindo DG, Krause LR, Mayfield RD (2008) Ethanol potentiates dopamine uptake and increases cell surface distribution of dopamine transporters expressed in SK-N-SH and HEK-293 cells. Alcohol (Fayetteville, NY) 42:499–508
Roche DJ, Ray LA, Yardley MM, King AC (2016) Current insights into the mechanisms and development of treatments for heavy drinking cigarette smokers. Curr Addict Reports 3:125–137
Rollema H, Chambers LK, Coe JW, Glowa J, Hurst RS, Lebel LA, Lu Y, Mansbach RS, Mather RJ, Rovetti CC, Sands SB, Schaeffer E, Schulz DW, Tingley Iii FD, Williams KE (2007) Pharmacological profile of the α4β2 nicotinic acetylcholine receptor partial agonist varenicline, an effective smoking cessation aid. Neuropharmacology 52:985–994
Rose JE (2006) Nicotine and nonnicotine factors in cigarette addiction. Psychopharmacology 184:274–285
Rose JE (2008) Disrupting nicotine reinforcement. Ann N Y Acad Sci 1141:233–256
Rose JE, Behm FM, Westman EC, Levin ED, Stein RM, Ripka GV (1994) Mecamylamine combined with nicotine skin patch facilitates smoking cessation beyond nicotine patch treatment alone. Clin Pharmacol Therapeutics 56:86–99
Sahr AE, Thielen RJ, Lumeng L, Li TK, McBride WJ (2004) Long-lasting alterations of the mesolimbic dopamine system after periadolescent ethanol drinking by alcohol-preferring rats. Alcohol Clin Exp Res 28:702–711
Sajja RK, Rahman S (2012) Neuronal nicotinic receptor ligands modulate chronic nicotine-induced ethanol consumption in C57BL/6J mice. Pharmacol Biochem Behav 102:36–43
Sajja RK, Dwivedi C, Rahman S (2010) Nicotinic ligands modulate ethanol-induced dopamine function in mice. Pharmacology 86:168–173
Schacht JP, Anton RF, Randall PK, Li X, Henderson S, Myrick H (2014) Varenicline effects on drinking, craving and neural reward processing among non-treatment-seeking alcohol-dependent individuals. Psychopharmacology 231:3799–3807
Scuppa G, Cippitelli A, Toll L, Ciccocioppo R, Ubaldi M (2015) Varenicline decreases nicotine but not alcohol self-administration in genetically selected Marchigian Sardinian alcohol-preferring (msP) rats. Drug Alcohol Depend 156:126–132
Shoaib M, Stolerman IP (1992) MK801 attenuates behavioural adaptation to chronic nicotine administration in rats. Br J Pharmacol 105:514–515
Shytle RD, Penny E, Silver AA, Goldman J, Sanberg PR (2002) Mecamylamine (Inversine): an old antihypertensive with new research directions. J Hum Hypertens 16(7):453–457
Simms JA, Bito-Onon JJ, Chatterjee S, Bartlett SE (2010) Long-Evans rats acquire operant self-administration of 20% ethanol without sucrose fading. Neuropsychopharmacol : Off Publ Am Coll Neuropsychopharmacol 35:1453–1463
Sotomayor-Zarate R, Gysling K, Busto UE, Cassels BK, Tampier L, Quintanilla ME (2013) Varenicline and cytisine: two nicotinic acetylcholine receptor ligands reduce ethanol intake in University of Chile bibulous rats. Psychopharmacology 227:287–298
Srisontiyakul J, Kastman HE, Krstew EV, Govitrapong P, Lawrence AJ (2016) The nicotinic α6-subunit selective antagonist bPiDI reduces alcohol self-administration in alcohol-preferring rats. Neurochem Res 41:3206–3214
Steensland P, Simms JA, Holgate J, Richards JK, Bartlett SE (2007) Varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, selectively decreases ethanol consumption and seeking. Proc Natl Acad Sci U S A 104:12518–12523
Tizabi Y, Bai L, Copeland RL, Jr., Taylor RE (2007) Combined effects of systemic alcohol and nicotine on dopamine release in the nucleus accumbens shell. Alcohol and alcoholism (Oxford, Oxfordshire) 42: 413–416
Udo T, Harrison EL, Shi J, Tetrault J, McKee SA (2013) A preliminary study on the effect of combined nicotine replacement therapy on alcohol responses and alcohol self-administration. Am J Addict 22:590–597
Van Skike CE, Maggio SE, Reynolds AR, Casey EM, Bardo MT, Dwoskin LP, Prendergast MA, Nixon K (2016) Critical needs in drug discovery for cessation of alcohol and nicotine polysubstance abuse. Prog Neuro-Psychopharmacol Biol Psychiatry 65:269–287
Verplaetse TL, Pittman BP, Shi JM, Tetrault JM, Coppola S, McKee SA (2016) Effect of lowering the dose of varenicline on alcohol self-administration in drinkers with alcohol use disorders. J Addict Med 10:166–173
Wang X-F, Bi G-H, He Y, Yang H-J, Gao J-T, Okunola-Bakare OM, Slack RD, Gardner EL, Xi Z-X, Newman AH (2015) R-modafinil attenuates nicotine-taking and nicotine-seeking behavior in alcohol-preferring rats. Neuropsychopharmacol : Off Publ Am Coll Neuropsychopharmacol 40:1762–1771
Warnock KT, Yang AR, Yi HS, June HL Jr, Kelly T, Basile AS, Skolnick P, June HL (2012) Amitifadine, a triple monoamine uptake inhibitor, reduces binge drinking and negative affect in an animal model of co-occurring alcoholism and depression symptomatology. Pharmacol Biochem Behav 103:111–118
Warren GW, Alberg AJ, Kraft AS, Cummings KM (2014) The 2014 Surgeon General’s report: “The health consequences of smoking—50 years of progress”: a paradigm shift in cancer care. Cancer 120:1914–1916
Weinberger AH, Pilver CE, Hoff RA, Mazure CM, McKee SA (2013) Changes in smoking for adults with and without alcohol and drug use disorders: longitudinal evaluation in the US population. Am J Drug Alcohol Abuse 39:186–193
Williams KL, Broadbridge CL (2009) Potency of naltrexone to reduce ethanol self-administration in rats is greater for subcutaneous versus intraperitoneal injection. Alcohol (Fayetteville, NY) 43:119–126
Yamazaki H, Horiuchi K, Takano R, Nagano T, Shimizu M, Kitajima M, Murayama N, Shono F (2010) Human blood concentrations of cotinine, a biomonitoring marker for tobacco smoke, extrapolated from nicotine metabolism in rats and humans and physiologically based pharmacokinetic modeling. Int J Environ Res Public Health 7:3406–3421
Acknowledgements
Supported by NIH grants R01AA025591, UL1TR000117, U19DA17548, P50DA05312, T32DA016176, and U24AA015512.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All testing procedures occurred during the light phase (7:00 am–7:00 pm) were in accordance with the NIH Guide for the Care and Use of Laboratory Animals (8th edition, 2011) and were approved by the Institutional Animal Care and Use Committee at the University of Kentucky.
Conflict of interest
The University of Kentucky holds a patent on r-bPiDI and a potential royalty stream to Dwoskin and Crooks may occur consistent with University of Kentucky policy.
Rights and permissions
About this article
Cite this article
Maggio, S.E., Saunders, M.A., Baxter, T.A. et al. Effects of the nicotinic agonist varenicline, nicotinic antagonist r-bPiDI, and DAT inhibitor (R)-modafinil on co-use of ethanol and nicotine in female P rats. Psychopharmacology 235, 1439–1453 (2018). https://doi.org/10.1007/s00213-018-4853-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-018-4853-4