Abstract
Rationale
Fluoxetine (Prozac®) is the most frequently prescribed drug to battle depression in pregnant women, but its safety in the unborn child has not yet been established. Fluoxetine, a selective serotonin reuptake inhibitor, crosses the placenta, leading to increased extracellular serotonin levels and potentially neurodevelopmental changes in the fetus.
Objectives
The purpose of this study was to elucidate the long-term consequences of prenatal fluoxetine in rats.
Methods
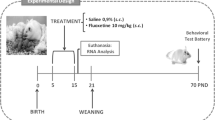
Pregnant rats were injected daily with 12 mg/kg fluoxetine or vehicle from gestational day 11 until birth, and the behavior of the offspring was monitored.
Results
Plasma fluoxetine transfer from mother to pup was 83%, and high levels of fluoxetine (13.0 μg/g) were detected in the pup brain 5 h after the last injection. Fluoxetine-treated dams gave birth to litters 15% smaller than usual and to pups of reduced weight (until postnatal day 7). Furthermore, prenatal fluoxetine exposure significantly increased anxiety in the novelty-suppressed feeding test, the footshock-induced conditioned place aversion test, and the elevated plus maze test (following footshock pre-exposure) during adulthood, and also significantly decreased components of social play behavior at 4 weeks of age, and a strong tendency for increased self-grooming and making less contact in adults. Behavioral despair, anhedonia, and sexual behavior were not different between treatment groups. Finally, the hypothermic response to the 5-HT1A agonist flesinoxan was observed at a lower dose in prenatally fluoxetine-exposed rats than in controls.
Conclusions
Prenatal fluoxetine exposure in rats leads to detrimental behavioral outcomes in later life, which may partly be due to altered 5-HT1A receptor signaling.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Depression is a serious mental disorder that is recurrent, life threatening (due to the risk of suicide), and a major cause of morbidity worldwide (WHO). Pregnancy is a period with high risk for depression, particularly for women with pre-existing psychiatric illnesses. The number of women that are depressed during pregnancy ranges between 7% and 26% (Evans et al. 2001; Kumar and Robson 1984; Moses-Kolko and Roth 2004; O’Hara et al. 1984; Oberlander et al. 2006). Maternal depression can have long-lasting negative cognitive and emotional consequences for the child (reviewed in Talge et al. 2007), for example increased risk of emotional problems (O’Connor et al. 2002), depression (DiPietro et al. 2006), delay in development (Deave et al. 2008), lowered IQ in adolescence (Hay et al. 2008), and impaired language development (Nulman et al. 2002; Paulson et al. 2009). These findings underline the importance of treating maternal depression as early as possible, i.e., during pregnancy. As a result, the number of prescriptions of antidepressants for pregnant women has doubled in the last decade (Andrade et al. 2008; Cooper et al. 2007; Oberlander et al. 2006). Around 25% of the women that are already treated for depression continue antidepressant use during pregnancy, while 0.5% of the women that never received treatment before starts using it (Ververs et al. 2006). This increased antidepressant use during pregnancy has raised questions about the developmental safety of antidepressants, in particular because antidepressants can cross the placenta (Kim et al. 2006; Noorlander et al. 2008).
The most frequently prescribed antidepressant is fluoxetine, a selective serotonin reuptake inhibitor (SSRI) that blocks the serotonin transporter (5-HTT) and increases extra-neuronal serotonin (5-HT) levels. So far, studies on the consequences of prenatal fluoxetine exposure in humans mainly addressed the potential risk of fetal structural malformations and perinatal complications (reviewed in Gentile and Galbally 2010).
While human studies are hampered by time constraints, rodents offer the possibility to study both the short- and long-term consequences of prenatal fluoxetine exposure. Because the first two postnatal weeks in rodents corresponds to the third trimester of human pregnancy (Romijn et al. 1991), most studies so far focused on neonatal fluoxetine exposure and behavior later in life (reviewed in Olivier et al. 2010b). These studies reported increased behavioral despair (Hansen et al. 1997; Lisboa et al. 2007; Popa et al. 2008), increased anxiety (Ansorge et al. 2004, 2008), decreased sexual behavior (Maciag et al. 2006c), reduced aggression (Manhães de Castro et al. 2001), increased REM sleep (Popa et al. 2008), reduced active sleep (Mirmiran et al. 1981), and blunted somatosensory responses (Lee 2009). Juvenile fluoxetine exposure leads to mixed effects; either there are no changes in anxiety and depression-related symptoms (Norcross et al. 2008); transient increased anxiety levels (Oh et al. 2009), or long-lasting increased anxiety levels (Homberg et al. 2011; Iniguez et al. 2010).
Yet, 5-HTT expression starts at midgestation in the raphe nuclei in both humans and rodents (Narboux-Neme et al. 2008), suggesting that fluoxetine exposure at an earlier stage of pregnancy in humans or prenatally in rodents will have significant effects on brain development and later life behavior that are stronger or distinct from those induced by third trimester/neonatal fluoxetine exposure. In this regard, prenatally fluoxetine-treated mice died postnatally from severe heart failure caused by dilated cardiomyopathy (Noorlander et al. 2008). The ones that survived moved less in the center of the open field and displayed increased latency to start eating in the novelty-suppressed feeding test during adulthood (Noorlander et al. 2008). Furthermore, pups born from rat dams prenatally treated with fluoxetine were smaller, gained weight more slowly (Vorhees et al. 1994), and displayed increased sensitivity to the rewarding effects of cocaine during adulthood (Forcelli and Heinrichs 2008). Thus, evidence has been obtained for effects of prenatal fluoxetine exposure, but the insights are still limited. For instance, it is not known whether and how prenatal fluoxetine exposure affects conditioned anxiety, depression-like behavior, social behavior, and 5-HT1A receptor sensitivity.
Therefore, we aimed to investigate the long-term consequences of fluoxetine exposure (12 mg/kg) from midgestation (gestational day 11; GD11) until birth. At the day of birth, fluoxetine blood plasma levels were measured from both the mother as well as from the pups. Moreover, pup bodyweight was measured weekly until adulthood. During adulthood, prenatally fluoxetine-exposed rats and controls were tested in a battery of behaviors known to be sensitive to serotonergic manipulations, including anxiety- and depression-like responses to stress (novelty-suppressed feeding, elevated plus maze, shock-induced conditioned place aversion, sucrose preference and forced swim test) and social behavior (social play, social interaction, and sexual behavior). Because SSRIs are known to exert (part of) their effects by desensitization of the 5-HT1A receptor (reviewed in Kinney et al. 2000), we finally measured flesinoxan-induced hypothermia to assess 5-HT1A receptor sensitivity in prenatally fluoxetine-treated rats.
Material and methods
Animals
To assess the estrous stage, the cycle of female Wistar rats (Harlan laboratories, Horst, The Netherlands) was measured daily in the late afternoon with an impedance checker (Impedance Checker MK-10B, Muromachi; see also Ramos et al. 2001). When a female reached the estrous stage it was placed together with a Wistar male (Harlan laboratories, Horst, The Netherlands) in Macrolon type 3 cage (42 × 26 × 20 cm) with a wire gauze bottom. The next day the cage was explored for a vaginal plug, and if found, this day was considered as GD1. From GD11 until birth (postnatal day (PND) 1) dams were treated daily with 12 mg/kg fluoxetine or 1% methylcellulose (vehicle). Pups were weaned at PND 21. During the experiments, all animals were housed per two in standard Macrolon® type 3 cages in temperature-controlled rooms (21°C ± 1°C) under a standard 12/12-h day/night cycle (lights on at 7:00 a.m.) with food (Sniff, long cut pellet, Bio Services, Uden, The Netherlands) and water available ad libitum. Seven groups of animals were used. Group 1 was used for fluoxetine and norfluoxetine measurements; group 2 was used for litter size and bodyweight measurements; group 3 was used for novelty-suppressed feeding and sexual behavior; group 4 was used for the forced swim test; group 5 was used for social play behavior, open field, elevated plus maze (EPM) without stress, conditioned place aversion, and elevated plus maze test (after stress); group 6 was used for 5-HT1A receptor challenges; and group 7 was used for adult social exploration and the sucrose preference test. Rats that were used for sexual behavior were placed in a reversed day/night cycle (lights on at 7:00 p.m.). Experiments were performed when the animals were at least at PND 65, except for the social play behavior experiments which were performed from PND 28–35. All experiments were carried out according to the guidelines for the Care and Use of Mammals in Neuroscience and Behavioral Research (National Research Council 2003), the principles of laboratory animal care, as well as the Dutch law concerning animal welfare.
Drugs
Treatment of pregnant rats
Prozac (fluoxetine) was derived from the Pharmacy of the Radboud University Nijmegen Medical Centre, The Netherlands and dissolved in distilled water. As a control, a 1% methylcellulose (derived from Genfarma B.V. Maarssen, The Netherlands) solution was used, which was the constituent of the fluoxetine pills that were used. All rats received a daily oral injection of 12 mg/kg, from GD11 until birth in a volume of 5 ml/kg.
Application of fluoxetine and norfluoxetine
Fluvoxamine, norfluoxetine, and fluoxetine were purchased from Sigma-Aldrich Chemie B.V. (Zwijndrecht, The Netherlands). High-performance liquid chromatography (HPLC) grade acetonitril and hexane were obtained from Biosolve B.V. (Valkenswaard, The Netherlands). Isoamylalcohol and hydrochloric acid were purchased from Merck (Darmstadt, Germany). Sodiumhydroxide, phosphoric acid and citric acid monohydrate were from Acros (Geel, Belgium).
5-HT1A challenge
Flesinoxan (HCl [R(+)-N-(2[4-(2,3-dihydro-2-2-hydroxy-methyl-1,4-benzodioxin-5-yl)-1-piperazininyl]ethyl)-4-fluorobenzoamide]) was kindly provided by the department of Psychopharmacology, Utrecht University, Utrecht, The Netherlands. The drug was dissolved in saline (0.9% NaCl), and injected intraperitoneally (i.p.; doses of 0.3, 1, 3, and 10 mg/kg) in a volume of 1 ml/kg.
Measurement of fluoxetine and norfluoxetine in blood plasma
Plasma collection
Five hours after the last fluoxetine injection blood samples were collected from the mother (n = 13) through a tail cut, and blood and brain samples from the pups (one litter, n = 10) by decapitation. Blood was collected in Microvette CB 300 (containing lithium heparin Sarstedt, Germany) tubes and centrifuged for 15 min at 4°C with a speed of 4,000 rpm. Supernatant (plasma) was stored at −20°C until further use.
HPLC
Whole brains were weighed and homogenized in 1.5 ml saline containing fluvoxamine as internal standard using a Potter tube. The brain homogenate (150 μl) or the plasma samples (50 to 100 μl), also containing fluvoxamine as internal standard, were extracted as described by Duverneuil et al. (2003). The concentration of fluoxetine and norfluoxetine in the extract was determined by HPLC. The HPLC system consisted of a pump model P100, an autosampler model AS300 (both from Thermo Separation Products, Waltham, MA, USA), a ERC-3113 degasser (Erma CR. Inc. Tokyo, Japan), a column oven (type 560-CIL, Cluzeau Info Labo, Sainte-Foy-La-Grande, France) an UV-detector (Spectroflow 747, Kratos Analytical Instruments, Ramses, NJ, USA) with wavelength set at 226 nm, integration software package Atlas 2003 (Thermo Electron Corporation, Cheshire UK) and a column (150 × 4.6 mm i.d.) packed with Hypersil BDS C18, 5-μm particle size (Alltech Associates, USA). The mobile phase consisted of a buffer containing 20 mM citric acid and 20 mM phosphoric acid (pH adjusted to 3.8 with NaOH) mixed with acetonitril (55:45). Separation was performed at 32°C using a flow rate of 0.8 ml/min. The concentration of each compound was calculated by comparison with both the internal and external standards. The limit of detection (signal/noise ratio 3:1) was 0.05 μg/g in brain samples and 15 ng/ml in 100 μl of plasma samples.
Litter size and weight
At PND 7, methylcellulose (n = 8) and fluoxetine nests (n = 11) from the first breeding round were checked for the number of pups. Of these, 4 methylcellulose-exposed (28 male and 22 females) and four prenatally fluoxetine-exposed litters (13 males and 21 females) were not used in experiments, but their bodyweight was measured on PND 7, 14, 21, 28, 35, 42, 49, 56, and 63.
Behavioral tests
Novelty-suppressed feeding
The novelty-suppressed feeding test was performed as described before (Olivier et al. 2008b). Male rats (PND 111; ten prenatally methylcellulose and seven prenatally fluoxetine-exposed) were isolated and food deprived. After 24 h of food deprivation (water available ad libitum), rats were placed in a brightly lit (60 W incandescent bulb 1.2 m above the arena) open arena (50 × 50 cm) containing clean wood chip bedding. A round white filter paper, with a radius of 6.25 cm, was placed in the center of the arena, and one home cage food pellet weighing approximately 2 g was placed on the paper. Rats were removed from their home cage, and then placed in one corner of the arena. The latency (s) to begin a feeding episode was recorded (maximum time was 600 s).
Open field
Male rats (PND 104; n = 12 per group) were tested in the open field (OF) test. The OF is a squared arena (100 × 100 × 40 cm), with open top, dark walls (wood), and a dark floor (polyvinylchloride). Testing was done at 10 lux. A camera was installed above the center of the field. Immediately after a rat was placed in the corner of the open field, the movements and position of the animal were recorded and registered automatically by a computerized system (Ethovision, Noldus Equipment, The Netherlands). Reported is the total distance moved (centimeter). Testing was carried out on a 5-min trial. The floor of the open field was cleaned with 70% ethanol solution between trials to prevent transmission of olfactory cues.
Elevated plus maze
Male rats (PND 106; 11 methylcellulose, 10 fluoxetine) were tested in the EPM test. The test was performed as described before (Olivier et al. 2008b). The apparatus was made of polyvinylchloride. It was elevated to a height of 50 cm with two open (50 × 10 cm) and two enclosed arms (50 × 10 × 40 cm) arranged such that the arms of the same type were opposite to each other. The light intensity in the open and closed arms was 12.1 and 4.49 lux, respectively. Rats were placed in the center of the maze, facing one of the open arms, and were allowed to freely explore the maze for period of 5 min. The movements and position of the animals were recorded and registered automatically by a computerized system (Ethovision, Noldus Equipment, The Netherlands). Results were expressed as the mean (± S.E.M.) of time spent (seconds) in the open arms, total distance moved (centimeters), and number of open and closed arm entries (number) in the EPM. The plus maze was cleaned with 70% alcohol solution between trials to prevent transmission of olfactory cues.
Footshock-induced conditioned place aversion
Place conditioning was performed in a box with three compartments. The two outer compartments (30 × 28 × 30 cm) were visually distinctive from one another by means of horizontal black and white stripes or blocks on the wall. The middle compartment (10 × 28 × 30 cm) had a smooth floor texture and white walls. The apparatus had grids on the floor which were connected to a shock generator. All compartments could be separated by means of sliding doors. Time spent (seconds) in the area was measured by Ethovision (Wageningen, Noldus Equipment, The Netherlands). During a pre-test, male rats (PND 165; n = 10 per group) were first allowed to freely explore the box for 15 min to determine possible compartment preferences. If the animal showed a preference for one side (more than 5% difference), the animal received the shocks in the non-preferred compartment. The remaining rats were randomly assigned to receive the shock in one of the two outer compartments. The pre-test was followed by eight training days. On training day 1, 3, 5, and 7, the rats received a shock (0.4 mA, 1 s/min) every minute. On training days 2, 4, 6, and 8, the rats were placed in the other compartment, without receiving shocks. Every training session lasted 20 min. After 8 days of training, a post-test was performed (day 9). The rats were placed in the middle compartment and allowed to freely explore the apparatus for 15 min. The apparatus was cleaned with 70% ethanol solution between trials to prevent transmission of olfactory cues.
EPM after stress
Two days after the conditioned place aversion (CPA) test, male rats (PND 177; n = 10 per group) were tested in the EPM test. First the animals were exposed to the shock compartment of the CPA for 10 min without receiving a shock. Directly after the exposure, animals were placed on the EPM. The test was performed as described above. Results are expressed as the mean (±S.E.M.) of time spent (seconds) in the open arms of the EPM, total distance moved (centimeters), and number of the open and closed arms entries.
Forced swim test
Male rats (PND 130; n = 10 per group) were used for the forced swim test. The forced swim test was performed as reported before (Olivier et al. 2008b). In short, cylindrical glass tanks (50 cm tall; 18 cm diameter), filled to a depth of 30 cm with 22 (+/−1)°C water, were used. Testing consisted of two phases, the induction phase and the test phase. During the induction phase animals were placed in the water for 15 min. After 24 h the rats are placed in the same tanks for 5 min. The movements of the rats were videotaped for off-line measurement of the duration of immobility (seconds). The behavioral variable “immobility” was defined as follows: making no movements for at least 2 s or making only those movements that were necessary to keep the nose above the water. The rats were allowed to slightly move their forepaws or support themselves by pressing their paws against the wall of the cylinder. Active climbing, diving, and swimming along the wall were scored as mobility (seconds).
Sucrose preference
The procedure was performed as described before (Olivier et al. 2008b). Twenty rats (n = 10 per group) were housed individually and habituated to the two-bottle paradigm by offering them water in two plastic drinking cylinders on top of the cage, one on each side. After this habituation period, the two bottles, free-choice, 24 h sucrose vs. water paradigm started. In short, animals were presented either with water in both bottles or, on alternating days, with water and increasing sucrose percentages (2%, 4%, and 8%). Bottles were switched on sucrose days to prevent spatial bias. Fluid consumption (grams) and bodyweight (grams) were measured daily and used to calculate two measurements, namely the preference of sucrose above water (sucrose intake in milliliter divided by total intake × 100%) and the intake in grams of a 100% sucrose solution per kilogram bodyweight (intake in milliliter corrected for the voluminal weight of sucrose and recalculated towards a 100% solution divided by bodyweight in kilogram).
Social play
Testing was performed as described previously (Homberg et al. 2007). Rats, aged 28–35 days, were tested in an acrylic plastic cage (45 × 45 × 55 cm) with approximately 2 cm of wood shavings covering the floor. The test was performed in the dark and filmed with an infrared red camera. Two days preceding the test, the animals (16 male prenatally methylcellulose-exposed rats and 12 male prenatally fluoxetine-exposed rats) were habituated to the test cage during 10 min. The animals of a test pair had no previous common social experience. On the test date, test pairs were isolated for 3.5 h to induce a half maximal increase in the amount of social play behavior (Niesink and Van Ree 1989). Pairs were tested for 15 min in the test cage. Behavior of the animals was recorded on video tape and analyzed afterwards with Keys® (UMC, Nijmegen, The Netherlands). Frequencies and time of the following behaviors were scored: (1) pinning: one of the animals lying with its dorsal surface on the floor of the test cage with the other animal standing over it; (2) pouncing: play soliciting by nosing the partner’s nape; (3) boxing/wrestling: facing each other in vertical position and struggling using the forepaws; (4) following/chasing: moving in the direction of or pursuing the test partner, who moves away; (5) social exploration: sniffing or licking any body part of the test partner. Behavior was assessed per pair of animals. Animals were only used once.
Adult social behavior
Twenty animals (∼PND 87; n = 10 per group) were tested in a social interaction test. The social play behavior procedure was used (as described above), with the exception that the rats were isolated 48 h before the experiment. Frequencies and durations of the following behaviors were scored: (1) social exploration: sniffing or licking any body part of the test partner; (2) self-grooming: forepaw licking, face washing, scratching, body grooming, and genital grooming; (3) following/chasing: moving in the direction of or pursuing the test partner, who moves away. A prenatal fluoxetine-exposed rat was put together with a prenatal methylcellulose-exposed rat. Behavior was assessed per individual animal. Animals were used only once.
Sexual behavior
20 Males (PND 133; 11 prenatally methylcellulose- and 9 prenatally fluoxetine-exposed rats) were housed under reversed day/light rhythm to perform the sex tests, starting 3 weeks prior to the start of the experiment. Outbred female Wistar rats (Harlan, Zeist, The Netherlands) were used as stimulus rats and estrous was induced with a single injection of 50 mg of estradiol benzoate in sesame oil saturated with lecithin 36–42 h prior to testing. Male rats were trained for 30 min once weekly for four consecutive weeks against an estrous female in a Phenotyper (Noldus Equipment, Wageningen, The Netherlands). The floor of the test cage was covered with a bedding and was not refreshed for each test session. Sex tests were performed between 9:00 a.m. and 3:00 p.m. in the dark phase of the reversed light/dark cycle under red light. The rats were placed first in the test cage and allowed to habituate for 10 min. Subsequently, an estrous female was placed into the cage. Male sexual behavior was scored over 30 min. The following parameters were scored for the first ejaculation series using Keys® (UMC, Nijmegen, The Netherlands): number of mounts (M), number of intromissions (I), copulatory efficiency (CE; calculated as \( {\text{CE}} = \left( {\left[ {\# I{ /}\left( {\# I + \# M} \right)} \right] \times {1}00\% } \right) \), and the ejaculatory latency (EL; calculated as time of ejaculation minus the time of the very first behavior of that ejaculation series). After the first ejaculation, the first postejaculatory latency (PEL1) was calculated. Moreover, the total number of ejaculations during the 30 min was scored.
5-HT1A challenges
Telemetry
Thirteen male rats (PND 65; seven prenatally methylcellulose-exposed rats and six prenatally fluoxetine-exposed rats) were used as described before (Olivier et al. 2008a, 2010a).
Surgery
Rats were deeply anesthetized with a mixture of N2O/O2 (1:2) and isoflurane (2.5%; Rhodia Organique Fine limited, Bristol, United Kingdom). Electrocardiogram transmitters (Data Sciences InternationalTM, type TA11CTA-F40 or TA10CTA-F40, St. Paul, MN, USA) were implanted in the abdominal cavity. After surgery, animals were isolated and allowed to recover for 14 days; rats were checked daily during that period.
Radiotelemetry system
The radiotelemetry system consisted of an implantable transmitter (model TA11CTA-F40 or model TA10TA-F40), a telemetric receiver (model RPC-1 and RLA1020; Data Sciences InternationalTM, St. Paul, MN, USA) and an IBM Compaq 486/66 computer. Signals from the transmitters were passed on to the receiver, localized under the animal cage, transforming it into digital information. Data of all animals were sampled every 5 min. Raw data were collected and analyzed by the software package Dataquest A.R.T. version 3.11 (Data Sciences InternationalTM, St. Paul, MN, USA).
Experimental procedure
The effects of the 5-HT1A receptor agonist flesinoxan on injection stress-induced hyperthermia body temperature was studied. Sampling data of the rats started at 6:00 p.m. the day prior to the drug administration to obtain undisturbed baseline values. All doses of flesinoxan (vehicle, 0.3, 1.0, 3.0, and 10 mg/kg) were randomly administered at 1-week intervals to each rat (within-animal design). All injections were given at 11.00 a.m., and the effects were measured up to 5 h after the injection.
Statistical analysis
Body weight data were analyzed using repeated measures ANOVA, with prenatal treatment as between-subject factors and time as within-subject factors. Body weight data were further analyzed per day using independent sample t test. CPA data were analyzed with two-way ANOVA with test days and prenatal treatment as variables. Differences in days (tests) were further analyzed using independent sample t test, as were differences in time spent in the different compartments, and immobility time in the CPA during the post-test. Sexual behavior was analyzed with two-way ANOVA, with least significant difference (LSD) post hoc testing if appropriate. Differences in sexual behavior between the prenatal treatments were analyzed with independent sample t tests. Telemetry data were analyzed using the area under the curve (AUC), which was analyzed by two-way ANOVA with dose and prenatal treatment as variables. Per treatment, data were further analyzed by one-way ANOVA, and LSD post hoc testing where appropriate. Sucrose preference and intake were analyzed using repeated measures ANOVA, with prenatal treatment as between-subject factors and intake/preference as within-subject factors. All other data were analyzed using independent sample t tests, with prenatal treatment was assessed as independent variable level of significance was set at p < 0.05 (n.s. = non-significant). All statistical analyses were performed using the Statistical Package for the Social Sciences version 16.0 for windows (SPSS Inc., Chicago, IL, USA).
Results
Fluoxetine and norfluoxetine levels in blood plasma
Five hours after the last fluoxetine injection fluoxetine levels were 510 ± 28 ng/ml in mother rats and 430 ± 41 ng/ml in newborn rats, indicating that 83% of fluoxetine in the mother plasma is transferred to the pup. Norfluoxetine was detected at levels of 736 ± 23 ng/ml in mother rats and 574 ± 69 ng/ml in newborn rats giving a 78% transfer from mother plasma to the pup. Next to the plasma levels, the fluoxetine and norfluoxetine levels were measured in the brains of the newborns. The level of fluoxetine in the pup brain was 13.0 ± 0.90 μg/g and the level of norfluoxetine was 22.5 ± 1.19 μg/g.
Littersize and weight
Pregnant rats that were treated with fluoxetine gave birth to less pups compared to mothers that where treated with methylcellulose (methylcellulose-treated, 10.7 ± 1.4; fluoxetine-treated, 9.1 ± 0.9; t (1,17) = 2.15; p < 0.05). The weights of the offspring of four methylcellulose-treated and four fluoxetine-treated mothers were followed once a week until day 63 (Fig. 1). A treatment × time interaction was found for body weight (F (8,640) = 3.47; p < 0.01). Furthermore, analyses revealed that on PND 7 the weight of pups that were prenatally exposed to fluoxetine were significantly lower compared to rats that were prenatally exposed to methylcellulose (t (1,83) = 2.02; p < 0.05). From PND 14 to 35, this effect was reversed: the body weights of prenatally fluoxetine-exposed rats were higher compared to methylcellulose-exposed rats at PND 14 (t (1,82) = 5.58; p < 0.001), PND 21 (t (1,82) = 7.22; p < 0.001), PND 28 (t (1,80) = 5.82; p < 0.001), and PND 35 (t (1,82) = 2.70; p < 0.01). From PND 42 on, no significant differences were found (PND 42 (t (1,82) = 0.53; n.s.), PND 49 (t (1,82) = 0.76; n.s.), PND 56 (t (1,82) = 1.02; n.s.), and PND 63 (t (1,23) = 1.25; n.s.).
Behavior
Novelty-suppressed feeding
A significant prenatal treatment effect was found for the latency to start eating in a novel environment (t (1,15) = 3.17; p < 0.05). As shown in Fig. 2, prenatally fluoxetine-exposed rats exhibited a longer latency to start eating than controls.
OF
No differences between prenatal fluoxetine or prenatal methylcellulose-exposed rats were found in the total distance moved (t (1,23) = 1.03; n.s.; data not shown).
EPM
No group differences were found for time spent in the open arm of the EPM (t (1,19) = 0.31; n.s.). The number of open arm entries (t (1,18) = 0.17; n.s.) and number of closed arm entries (t (1,18) = 0.75; n.s.) were also not different between prenatal methylcellulose and prenatal fluoxetine-exposed rats. Moreover, no differences were found in distance moved between groups (t (1,18) = 1.58; n.s.; data not shown).
CPA
No group differences in place preference during the pre-test were observed in the shock (methylcellulose 389 ± 22; fluoxetine 423 ± 35; t (1,17) = 0.84; n.s.), control (methylcellulose 269 ± 11; fluoxetine 241 ± 22; t (1,17) = 1.17; n.s.), or middle compartment (methylcellulose 242 ± 23; fluoxetine 236 ± 38; t (1,17) = 0.12; n.s.).
Across the different test days (pre-test vs. post-test) an overall test day effect was found (F (1,34) = 15,51; p < 0.001), but no treatment effect (F (1,34) = 0.09; n.s.) and treatment × test day interaction (F (1,34) = 1.67; n.s.) for the time spent in the shock compartment. Although subsequent testing within treatment was not allowed based on statistical grounds, Fig. 3 suggested treatment effects during the post-test, which prompted us to continue post hoc testing. Thereby, we found that prenatally fluoxetine-exposed rats spent significantly less time in the shock compartment (T (1,16) = 3.62; p < 0.01) during the post-test compared to the pre-test (Fig. 3a), whereas a tendency was found in prenatally methylcellulose-exposed rats (T (1,18) = 1.92; p = 0.07). The time spent in the shock compartment (methylcellulose 298 ± 40; fluoxetine 243 ± 36; t (1,17) = 0.99; n.s.), the control compartment (methylcellulose 323 ± 28; fluoxetine 400 ± 37; t (1,17) = 1.64; n.s.), and middle compartment (methylcellulose 279 ± 23; fluoxetine 257 ± 17; t (1,17) = 0.76; n.s.) were not different between the prenatally methylcellulose and fluoxetine-exposed rats in the post-test. Figure 3b shows that prenatally fluoxetine-exposed rats froze significantly more during the first post-test compared to prenatally methylcellulose-exposed rats (t (1,17) = 2.38; p < 0.05).
Effect of prenatal fluoxetine exposure on a exploration time (seconds) spent in the shock compartment and b freezing time (seconds) in the whole arena of the conditioned place aversion test during the post-test. Data are represented as mean ± S.E.M. a *p < 0.05 versus pre-test; # 0.1 < p > 0.05 versus pre-test. No differences were found between prenatally methylcellulose and fluoxetine-exposed rats. b *p < 0.05 prenatally fluoxetine-exposed rats versus methylcellulose-exposed rats
Stress-induced EPM
Twenty-four hours after the CPA test, rats were pre-exposed to the footshock-conditioned compartment and then immediately placed on the EPM. Rats that were prenatally exposed to fluoxetine spent significantly less time on the open arms compared to controls (t (1.18) = 2.46; p < 0.05; Fig. 4). No differences were found in the number of open arm entries (t (1,17) = 1.87; n.s.) and number of closed arm entries (t (1,17) = 1.41; n.s.) between prenatally fluoxetine and methylcellulose-exposed rats. Prenatally fluoxetine-exposed rats tended to move less in the EPM compared to methylcellulose-exposed rats (t (1,18) = 2.06; p = 0.06).
Forced swim test
No group differences were found for mobility time (t (1,18) = 0.47; n.s.) and immobility time (t (1,18) = 0.47; n.s.; data not shown).
Sucrose preference
No prenatal treatment × sucrose preference (F (2,30) = 1.42; n.s.) and prenatal treatment x sucrose intake (F (2,30) = 0.57; n.s.) interactions were found (data not shown).
Social play
Prenatally fluoxetine-exposed rats displayed a strong reduction in pinning frequency (t (1,12) = 4.12; p < 0.01) compared to prenatally methylcellulose-exposed rats (Fig. 5). Moreover, boxing/wrestling (t (1,12) = 2.04; p = 0.06) and social exploration frequency (t (1,12) = 1.83; p = 0.09) tended to be reduced in prenatally fluoxetine-exposed rats. No differences in pouncing (t (1,12) = 0.66; n.s.) and following (t (1,11) = 0.70; n.s.) frequencies were found. No differences between groups were found in the duration of the behaviors (data not shown).
Effect of prenatal fluoxetine exposure on social play behavior. Data are represented as mean ± S.E.M. frequency (number) of play behavior. *p < 0.05 prenatally fluoxetine-exposed rats versus methylcellulose-exposed rats. # tendency (0.05 < p < 0.1) prenatally fluoxetine-exposed rats versus methylcellulose-exposed rats
Adult social behavior
No prenatal group differences were found for the frequencies in social exploration (t (1,18) = 0.47; n.s.), self-grooming (t (1,16) = 1.35; n.s.), or chasing/following (t (1,18) = 0.75; n.s.; data not shown). However prenatal fluoxetine-exposed rats tended to spent less time in self-grooming (t (1,18) = 2.07; p = 0.053) and social exploration (t (1,18) = 1.98; p = 0.064) compared to prenatal methylcellulose-exposed rats (data not shown). No differences were found in the time spent on chasing/following (t (1,18) = 0.39; n.s.).
Sexual behavior
The sexual behavior data of the first day were lost due to technical problems with the videotapes. Therefore only the data of day (D)7, D14, and D21 were included in the results. No differences were found between prenatally methylcellulose-exposed and prenatally fluoxetine-exposed rats in ejaculation frequency (t (1,58) = 1.27; n.s.), mount frequency (t (1,43) = 0.56; n.s.), intromission frequency (t (1,46) = 0.58; n.s.), latency to the first ejaculation (t (1,46) = 0.56; n.s.), post ejaculatory latency (t (1,46) = 1.16; n.s.), and copulatory efficiency (t (1,52) = 0.07; n.s.). The mount frequencies were significantly different between days (Fig. 6a; F (2,39) = 11.94; p < 0.001). There were less mounts on D14 (p < 0.05) and D21 (p < 0.001) compared to D7. Also on D21 less mounts were needed than on D14 (p < 0.05). Moreover, the latency to ejaculate for the first time was significantly different between days (Fig. 6b; F (2,42) = 4.45; p < 0.05). The ejaculatory latencies were shorter on D14 (p < 0.05) and D21 (p < 0.05) compared to D7. No differences were found between the ejaculation latencies on D14 and D21. Thus, after 2 weeks of experience, the sexual behavior of the rats was stabilized, with no differences between the prenatally methylcellulose- and prenatally fluoxetine-exposed rats.
5-HT1A challenges
Telemetry
The AUC was calculated from 1 h before the injection to 4 h after the injection. A significant dose effect was found (F (4,51) = 31.97; p < 0.001), but no treatment effect (F (4,51) = 0.05; n.s.) or dose × treatment interaction (F (4,51) = 0.89; n.s.) was obtained. In prenatally methylcellulose-exposed rats, 3.0 mg/kg (p < 0.01) and 10.0 mg/kg flesinoxan (p < 0.001) significantly decreased the body temperature (Fig. 7). Prenatally fluoxetine-exposed rats were more vulnerable, as their body temperature dropped significantly at the 1.0 mg/kg flesinoxan (p < 0.01) dose, which was not seen in methylcelluose-exposed rats (p = 0.09). At 3.0 mg/kg (p < 0.001) and 10.0 mg/kg flesinoxan (p < 0.001), prenatally fluoxetine-exposed rats showed similar reductions in body temperature compared to prenatal methylcellulose-exposed rats.
Discussion
The aim of the present study was to elucidate the long-term effects of prenatal fluoxetine exposure on behavior and 5-HT1A receptor sensitivity of the offspring. We observed that the placental transfer of fluoxetine from mother to pup was 83%. This is comparable with the placental transfer found in human and mouse (Noorlander et al. 2008). The transfer of norfluoxetine, the active metabolite of fluoxetine (Kecskemeti et al. 2005) from mother to pup was 78%, although this may partly be due to the metabolization of fluoxetine into norfluoxetine in the pup. The plasma norfluoxetine/fluoxetine ratio in the present study was 1.44 for the mothers and 1.39 for the pups, which is similar to the 1.3–1.5 ratio found in humans (Lundmark et al. 2001). As SSRIs easily pass the blood brain barrier (Baumann and Rochat 1995) and fluoxetine is transferred from the mother to the fetus through blood plasma, it can also cross the blood brain barrier and enter the brain of the fetus. Indeed, we found 13.0 ± 0.90 μg/g fluoxetine and 22.5 ± 1.19 μg/g norfluoxetine in the pup brains. These findings point out that during development not only the periphery is exposed to elevated 5-HT levels, but also the central nervous system. Given that 5-HT acts as a neurotrophic factor, at least during early development (Gaspar et al. 2003; Homberg et al. 2010), the aberrant brain 5-HT levels may lead to alterations in neurodevelopment. Fluoxetine exposure in the first 3 weeks after birth indeed results in a reduced amount of 5-HT neurons in the dorsal raphe nucleus, smaller 5-HT neuronal cell bodies in the dorsal and medial raphe nuclei, and reduced the number of serotonergic terminals in the hippocampus (Silva et al. 2010). Thus far, it is unknown whether these or other effects also occur with prenatal fluoxetine exposure.
Previous studies have reported that prenatal fluoxetine (and paroxetine) exposure leads to higher neonatal mortality in rodents (Noorlander et al. 2008; van den Hove et al. 2008). In the present study, no differences in mortality were noted, although fluoxetine treatment did affect the litter size, which might suggest prenatal mortality. We observed that fluoxetine-treated dams gave birth to fewer pups compared to mothers that received vehicle. Children whose mothers used fluoxetine during the pregnancy weighed less at birth (Chambers et al. 1996). Accordingly, like Vorhees and colleagues (1994), we also observed that at PND 7 rats that had been prenatally exposed to fluoxetine weighed less compared to control rats. Weight loss is a well-known side-effect of fluoxetine (Michelson et al. 1999). Because fluoxetine was likely washed out during the first week after birth, the reduced pup weight may likely be attributed to prenatal fluoxetine effects. At PND 14, pup weights were normalized, and from PND 14 to 35, weight gain was even increased in prenatally fluoxetine-exposed rats compared to controls. This effect might be due to the fact that fluoxetine-treated mothers had fewer pups, and therefore these pups had more access to mother milk.
Neonatal fluoxetine exposure in mice and rats has an effect on affective behavior. For instance, neonatal fluoxetine exposure increased anxiety levels, as shown by decreased locomotor activity and increased immobility time in the open field (Ansorge et al. 2004; Jiang et al. 2009), reduced locomotor activity in the EPM test (Ribas et al. 2008), and increased latency to start eating in the novelty-suppressed feeding test (Jiang et al. 2009). In addition, neonatal fluoxetine exposure affected depression-like behavior, as reflected by the increased immobility time in the forced swim test (Hansen et al. 1997), and increased anhedonia (Popa et al. 2008). Prenatal fluoxetine exposure in mice also resulted in increased anxiety-like behavior, as reflected by decreased exploratory activity in the center of the open field and increased latency to start eating in the novelty-suppressed feeding test (Noorlander et al. 2008). In line with the latter results, we found that compared to control rats, prenatally fluoxetine-exposed rats needed more time to start eating in the novelty-suppressed feeding test. Because there were no treatment effects on sucrose preference and consumption in the sucrose preference test, it is most likely that this increased latency reflected increased anxiety, rather than a decreased motivation. Interestingly, the prenatally fluoxetine-exposed rats spent less time on the open arms of the EPM after stress. Moreover, prenatally fluoxetine-exposed rats were more immobile and spent less time in the shock compartment during the CPA post-test, although these effects were very mild. These EPM and CPA findings are not likely to be confounded by effects on general locomotor activity, as we did not observe changes in open field activity and open and closed arm entries in the EPM test (with and without prior stress exposure).
For unknown reasons, we did not observe effects of prenatal fluoxetine exposure on depression-like behavior. Behavioral despair in the forced swim test and anhedonia in the sucrose preference test were not different between the treatment groups. In the prenatal exposure paradigm, anxiety-related behavior is apparently more affected than depression-like behavior. The mechanisms underlying these developmental processes are largely unknown, although the 5-HT1A receptor might play a role (see below). Nevertheless, these data indicate that not only neonatal, but also prenatal, fluoxetine exposure affects the development of emotional systems.
There is a wealth of literature that describes the relationship between 5-HT and social behavior. For instance, SSRIs and 5-HT releasing drugs are well known to reduce social play behavior as well as sexual behavior (Clayton et al. 2002; Knutson et al. 1996; Montejo-Gonzalez et al. 1997; Rosen et al. 1999; Rowland et al. 2010; Waldinger et al. 1998). In young rats (age ranging PND 28–35), acute postnatal fluoxetine treatment reduced social play behavior (Homberg et al. 2007). In line with this, we showed that prenatal fluoxetine exposure affects social play behavior as well, without affecting the total duration of social interaction (data not shown). Thus, prenatal as well as postnatal fluoxetine exposure reduces social behavior in young rats, irrespective of the treatment regimen (acute or chronic). With respect to social behavior in later life, postnatal antidepressant treatment is known to impair aggressive behavior (Manhães de Castro et al. 2001) and adult sexual behavior (Neill et al. 1990) in rats. Maciag et al. (2006a, b, c) have shown that neonatal chronic treatment with the SSRI citalopram (PND 8 to 21) results in decreased sexual behavior. Moreover, Iniguez et al. (2010) reported that rats which have been treated with fluoxetine from PND 35 to 50 exhibited increased mount frequencies and decreased ejaculation latencies and frequencies. In contrast to neonatal antidepressant treatment effects, we show that prenatal fluoxetine exposure does not affect sexual behavior. We found that rats learned how to perform sexual behavior after two experiences, since the latency to the first ejaculation was less (and stable) during day 14 and 21 compared to day 7. No differences in the number of ejaculations, mounts, and intromissions were found between the treatment groups. We did find that prenatal fluoxetine treatment tended to reduce the time rats socially interact. Moreover, self-grooming tended to be increased in prenatal fluoxetine-treated rats. Increased self-grooming might reflect increased stress, as rats placed in a novel cage steadily increase grooming (van Erp et al. 1994). Thereby, these findings correspond to increased anxiety-like behavior in prenatally fluoxetine-exposed rats tested in the EPM, CPA, and novelty-suppressed feeding tests (see above). We show here that social behavior may play a role in the effects of prenatal fluoxetine exposure, albeit to a lesser extent than following postnatal fluoxetine treatment, but the exact underlying mechanisms remain to be established.
Interestingly, long-term behavioral outcomes of prenatal fluoxetine exposure correspond strikingly well to phenotypes observed in serotonin transporter knockout (5-HTT−/−) rodents (reviewed in Kalueff et al. 2010), although the effects of prenatal fluoxetine exposure might be milder. For instance, here, we show that prenatal fluoxetine exposure reduced social play, a phenomenon we previously observed in 5-HTT−/− rats (Homberg et al. 2007). Moreover, 5-HTT−/− rats spent less time in the open arm of the EPM, which we also observed in the present study in the prenatally fluoxetine-exposed rats. Yet, the animals had to be pre-exposed to stress before the anxiety-related effects of prenatal fluoxetine became overt. This observation is in line with the finding that 5-HTT−/− mice displayed increased anxiety in the EPM and light/dark box only when exposed to predator odor (Adamec et al. 2006). Finally, while prenatal fluoxetine did not alter sexual behavior, it was reduced in 5-HTT−/− rats, but only after extensive training (Chan et al. 2010). The comparisons between the effects of pharmacological 5-HTT blockade and of lifetime 5-HTT absence suggest that 5-HT-induced neurodevelopmental changes, rather than lifetime effects, explain the observed phenotypes in 5-HTT−/− rodents.
An important factor contributing to the above-mentioned neurodevelopmental changes may involve the 5-HT1A receptor. The 5-HT1A receptor is implicated in neurite branching (Sikich et al. 1990), neurite outgrowth, and neuronal survival (Fricker et al. 2005) during early brain development. In addition, early life 5-HT1A receptor blockade was found to normalize depression-related phenotypes in 5-HTT−/− mice (Alexandre et al. 2006). We observed that 5-HT1A receptor sensitivity was slightly, but significantly, increased in prenatally fluoxetine-exposed rats compared to controls. Thus, although flesinoxan dose-dependently induced hypothermia in both prenatally methylcellulose-exposed rats and prenatally fluoxetine-exposed rats, this effect appeared at a lower dose (1.0 mg/kg) in prenatally fluoxetine-exposed rats compared to the higher dose (3.0 mg/kg) in controls. Yet, the differences were small, and therefore further research is required to study whether 5-HT1A receptor function and the behavioral outcomes of prenatal fluoxetine exposure are (causally) linked.
A potential limitation of the present study is that we did not cross foster the pups derived from fluoxetine and methylcellulose treatment dams. Yet, in the human situation it is the combination of SSRI treatment and maternal behavior (depression) that affects the development of the fetus, and after birth maternal behavior continues to impact the development of the newborn. This situation was mimicked in our study, although the dams were not depressed. The oral injections may have induced some stress, but rather than being a confounding factor, the injection stress can be considered as part of the compound factor that influences fetal development. Another caveat could be that animals of group 5 were assessed in several tests (social play behavior, open field, EPM without stress, CPA, and EPM after CPA-stress), and repeated testing could have affected subsequent behavior. However, social play behavior is a normal, non-stressful, phenomenon and not likely to affect later life behavior. The open field test lasted for only 5 min, and novelty exposure is also part of the EPM test, which was subsequently performed. Because the EPM is relatively mild compared to the CPA test, and the setup is different, it is also not likely that EPM testing influenced CPA post-test performance. Nonetheless, repeated testing can influence elevated plus maze behavior, particularly in response to anxiolytics (File 1990; Lister 1987). However, in our hands there were no differences in open arm time in the methylcellulose-exposed rats before and after CPA, while open arm time was increased after CPA-induced stress in the fluoxetine-exposed rats (data not shown). Hence, it is unlikely that our findings were influenced by repeated testing. Collectively, these results indicate that the prenatally fluoxetine-exposed rats display an anxiety-like phenotype.
In conclusion, besides neonatal, also prenatal fluoxetine exposure has long-lasting effects on neurodevelopment. We show that prenatal fluoxetine exposure leads to anxiety-like, but not depression-like, behavioral outcomes during adulthood, which oppose the effects of SSRIs when applied to adults. Social behavior seems relatively resistant to prenatal fluoxetine exposure. These outcomes are due to neurodevelopmental changes, which may, in part, be mediated by altered 5-HT1A receptor signaling. Yet, it remains to be established which neural circuits and neuronal mechanisms (e.g., neuroplasticity, epigenetics) are involved. We are currently conducting follow-up studies focusing on the corticolimbic and somatosensory systems using functional magnetic resonance imaging and electrophysiological, immunohistochemical, and epigenetic approaches in rats, but partly also in humans. Together, these data provide an important contribution to our understanding of the effects of SSRIs on the unborn child, and may help psychiatrists and pregnant women to balance the risk of mother depression on the one hand, and the potential risk of SSRI-induced neurodevelopmental changes in the offspring on the other hand.
Abbreviations
- 5-HT:
-
Serotonin
- 5-HTT:
-
Serotonin transporter
- 5-HTT−/− :
-
Serotonin transporter knockout
- CE:
-
Copulatory efficiency
- CPA:
-
Conditioned place aversion
- E:
-
Embryonic day
- ECG:
-
Electrocardiogram
- EL:
-
Ejaculatory latency
- GD:
-
Gestational day
- I:
-
Intromission
- I.P.:
-
Intraperitoneal
- M:
-
Mount
- PEL:
-
Postejaculatory latency
- PND:
-
Postnatal day
- SSRI:
-
Selective serotonin reuptake inhibitor
References
Adamec R, Burton P, Blundell J, Murphy DL, Holmes A (2006) Vulnerability to mild predator stress in serotonin transporter knockout mice. Behav Brain Res 170:126–140
Alexandre C, Popa D, Fabre V, Bouali S, Venault P, Lesch KP et al (2006) Early life blockade of 5-hydroxytryptamine 1A receptors normalizes sleep and depression-like behavior in adult knock-out mice lacking the serotonin transporter. J Neurosci 26:5554–5564
Andrade SE, Raebel MA, Brown J, Lane K, Livingston J, Boudreau D et al (2008) Use of antidepressant medications during pregnancy: a multisite study. Am J Obstet Gynecol 198:194–195
Ansorge MS, Zhou M, Lira A, Hen R, Gingrich JA (2004) Early-life blockade of the 5-HT transporter alters emotional behavior in adult mice. Science 306:879–881
Ansorge MS, Morelli E, Gingrich JA (2008) Inhibition of serotonin but not norepinephrine transport during development produces delayed, persistent perturbations of emotional behaviors in mice. J Neurosci 28:199–207
Baumann P, Rochat B (1995) Comparative pharmacokinetics of selective serotonin reuptake inhibitors: a look behind the mirror. Int Clin Psychopharmacol 10(Suppl 1):15–21
Chambers CD, Johnson KA, Dick LM, Felix RJ, Jones KL (1996) Birth outcomes in pregnant women taking fluoxetine. N Engl J Med 335:1010–1015
Chan JS, Snoeren EM, Cuppen E, Waldinger MD, Olivier B, Oosting RS (2010) The serotonin transporter plays an important role in male sexual behavior: a study in serotonin transporter knockout rats. J Sex Med 8(1):97–108. doi:10.1111/j.1743-6109.2010.01961.x
Clayton AH, Pradko JF, Croft HA, Montano CB, Leadbetter RA, Bolden-Watson C et al (2002) Prevalence of sexual dysfunction among newer antidepressants. J Clin Psychiatry 63:357–366
Cooper WO, Willy ME, Pont SJ, Ray WA (2007) Increasing use of antidepressants in pregnancy. Am J Obstet Gynecol 196:544–545
Deave T, Heron J, Evans J, Emond A (2008) The impact of maternal depression in pregnancy on early child development. BJOG 115:1043–1051
DiPietro JA, Novak MF, Costigan KA, Atella LD, Reusing SP (2006) Maternal psychological distress during pregnancy in relation to child development at age two. Child Dev 77:573–587
Duverneuil C, de la Grandmaison GL, de Mazancourt P, Alvarez JC (2003) A high-performance liquid chromatography method with photodiode-array UV detection for therapeutic drug monitoring of the nontricyclic antidepressant drugs. Ther Drug Monit 25:565–573
Evans J, Heron J, Francomb H, Oke S, Golding J (2001) Cohort study of depressed mood during pregnancy and after childbirth. BMJ 323:257–260
File SE (1990) One-trial tolerance to the anxiolytic effects of chlordiazepoxide in the plus-maze. Psychopharmacology (Berl) 100:281–282
Forcelli PA, Heinrichs SC (2008) Teratogenic effects of maternal antidepressant exposure on neural substrates of drug-seeking behavior in offspring. Addict Biol 13:52–62
Fricker AD, Rios C, Devi LA, Gomes I (2005) Serotonin receptor activation leads to neurite outgrowth and neuronal survival. Brain Res Mol Brain Res 138:228–235
Gaspar P, Cases O, Maroteaux L (2003) The developmental role of serotonin: news from mouse molecular genetics. Nat Rev Neurosci 4:1002–1012
Gentile S, Galbally M (2010) Prenatal exposure to antidepressant medications and neurodevelopmental outcomes: a systematic review. J Affect Disord 128(1–2):1–9
Hansen HH, Sanchez C, Meier E (1997) Neonatal administration of the selective serotonin reuptake inhibitor Lu 10-134-C increases forced swimming-induced immobility in adult rats: a putative animal model of depression? J Pharmacol Exp Ther 283:1333–1341
Hay DF, Pawlby S, Waters CS, Sharp D (2008) Antepartum and postpartum exposure to maternal depression: different effects on different adolescent outcomes. J Child Psychol Psychiatry 49:1079–1088
Homberg JR, Schiepers OJ, Schoffelmeer AN, Cuppen E, Vanderschuren LJ (2007) Acute and constitutive increases in central serotonin levels reduce social play behaviour in peri-adolescent rats. Psychopharmacol (Berl) 195:175–182
Homberg JR, Schubert D, Gaspar P (2010) New perspectives on the neurodevelopmental effects of SSRIs. Trends Pharmacol Sci 31:60–65
Homberg JR, Olivier JDA, Blom T, Arentsen T, van Brunschot C, Korte-Bouws G et al (2011) Fluoxetine exerts age-dependent effects on behavior and amygdala neuroplasticity in the rat. PLoS ONE 6(1):e16646. doi:10.1371/journal.pone.0016646
Iniguez SD, Warren BL, Bolanos-Guzman CA (2010) Short- and long-term functional consequences of fluoxetine exposure during adolescence in male rats. Biol Psychiatry 67:1057–1066
Jiang XZ, Liu YQ, Zhang YZ, Zhang LM, Li J, Li YF (2009) Neonatal fluoxetine exposure induced depression-like behaviors in the adult Kunming mice and the antidepressant-like effect of agmatine. Yao Xue Xue Bao 44:716–721
Kalueff AV, Olivier JD, Nonkes LJ, Homberg JR (2010) Conserved role for the serotonin transporter gene in rat and mouse neurobehavioral endophenotypes. Neurosci Biobehav Rev 34:373–386
Kecskemeti V, Rusznak Z, Riba P, Pal B, Wagner R, Harasztosi C et al (2005) Norfluoxetine and fluoxetine have similar anticonvulsant and Ca2+ channel blocking potencies. Brain Res Bull 67:126–132
Kim J, Riggs KW, Misri S, Kent N, Oberlander TF, Grunau RE et al (2006) Stereoselective disposition of fluoxetine and norfluoxetine during pregnancy and breast-feeding. Br J Clin Pharmacol 61:155–163
Kinney GG, Taber MT, Gribkoff VK (2000) The augmentation hypothesis for improvement of antidepressant therapy: is pindolol a suitable candidate for testing the ability of 5HT1A receptor antagonists to enhance SSRI efficacy and onset latency? Mol Neurobiol 21:137–152
Knutson B, Panksepp J, Pruitt D (1996) Effects of fluoxetine on play dominance in juvenile rats. Aggress Behav 22:297–307
Kumar R, Robson KM (1984) A prospective study of emotional disorders in childbearing women. Br J Psychiatry 144:35–47
Lee LJ (2009) Neonatal fluoxetine exposure affects the neuronal structure in the somatosensory cortex and somatosensory-related behaviors in adolescent rats. Neurotox Res 15:212–223
Lisboa SF, Oliveira PE, Costa LC, Venancio EJ, Moreira EG (2007) Behavioral evaluation of male and female mice pups exposed to fluoxetine during pregnancy and lactation. Pharmacology 80:49–56
Lister RG (1987) The use of a plus-maze to measure anxiety in the mouse. Psychopharmacol (Berl) 92:180–185
Lundmark J, Reis M, Bengtsson F (2001) Serum concentrations of fluoxetine in the clinical treatment setting. Ther Drug Monit 23:139–147
Maciag D, Coppinger D, Paul IA (2006a) Evidence that the deficit in sexual behavior in adult rats neonatally exposed to citalopram is a consequence of 5-HT1 receptor stimulation during development. Brain Res 1125:171–175
Maciag D, Simpson KL, Coppinger D, Lu Y, Wang Y, Lin RC et al (2006b) Neonatal antidepressant exposure has lasting effects on behavior and serotonin circuitry. Neuropsychopharmacology 31:47–57
Maciag D, Williams L, Coppinger D, Paul IA (2006c) Neonatal citalopram exposure produces lasting changes in behavior which are reversed by adult imipramine treatment. Eur J Pharmacol 532:265–269
Manhães de Castro R, Barreto Medeiros JM, Mendes da Silva C, Ferreira LM, Guedes RC, Cabral Filho JE et al (2001) Reduction of intraspecific aggression in adult rats by neonatal treatment with a selective serotonin reuptake inhibitor. Braz J Med Biol Res 34:121–124
Michelson D, Amsterdam JD, Quitkin FM, Reimherr FW, Rosenbaum JF, Zajecka J et al (1999) Changes in weight during a 1-year trial of fluoxetine. Am J Psychiatry 156:1170–1176
Mirmiran M, van de Poll NE, Corner MA, van Oyen HG, Bour HL (1981) Suppression of active sleep by chronic treatment with chlorimipramine during early postnatal development: effects upon adult sleep and behavior in the rat. Brain Res 204:129–146
Montejo-Gonzalez AL, Llorca G, Izquierdo JA, Ledesma A, Bousono M, Calcedo A et al (1997) SSRI-induced sexual dysfunction: fluoxetine, paroxetine, sertraline, and fluvoxamine in a prospective, multicenter, and descriptive clinical study of 344 patients. J Sex Marital Ther 23:176–194
Moses-Kolko EL, Roth EK (2004) Antepartum and postpartum depression: healthy mom, healthy baby. J Am Med Womens Assoc 59:181–191
Narboux-Neme N, Pavone LM, Avallone L, Zhuang X, Gaspar P (2008) Serotonin transporter transgenic (SERTcre) mouse line reveals developmental targets of serotonin specific reuptake inhibitors (SSRIs). Neuropharmacology 55:994–1005
Neill D, Vogel G, Hagler M, Kors D, Hennessey A (1990) Diminished sexual activity in a new animal model of endogenous depression. Neurosci Biobehav Rev 14:73–76
Niesink RJ, Van Ree JM (1989) Involvement of opioid and dopaminergic systems in isolation-induced pinning and social grooming of young rats. Neuropharmacology 28:411–418
Noorlander CW, Ververs FF, Nikkels PG, van Echteld CJ, Visser GH, Smidt MP (2008) Modulation of serotonin transporter function during fetal development causes dilated heart cardiomyopathy and lifelong behavioral abnormalities. PLoS ONE 3:e2782
Norcross M, Mathur P, Enoch AJ, Karlsson RM, Brigman JL, Cameron HA et al (2008) Effects of adolescent fluoxetine treatment on fear-, anxiety- or stress-related behaviors in C57BL/6 J or BALB/cJ mice. Psychopharmacol (Berl) 200:413–424
Nulman I, Rovet J, Stewart DE, Wolpin J, Pace-Asciak P, Shuhaiber S et al (2002) Child development following exposure to tricyclic antidepressants or fluoxetine throughout fetal life: a prospective, controlled study. Am J Psychiatry 159:1889–1895
Oberlander TF, Warburton W, Misri S, Aghajanian J, Hertzman C (2006) Neonatal outcomes after prenatal exposure to selective serotonin reuptake inhibitor antidepressants and maternal depression using population-based linked health data. Arch Gen Psychiatry 63:898–906
O’Connor TG, Heron J, Glover V (2002) Antenatal anxiety predicts child behavioral/emotional problems independently of postnatal depression. J Am Acad Child Adolesc Psychiatry 41:1470–1477
Oh JE, Zupan B, Gross S, Toth M (2009) Paradoxical anxiogenic response of juvenile mice to fluoxetine. Neuropsychopharmacology 34:2197–2207
O’Hara MW, Neunaber DJ, Zekoski EM (1984) Prospective study of postpartum depression: prevalence, course and predictive factors. J Abnorm Psychol 93:158–171
Olivier JD, Cools AR, Olivier B, Homberg JR, Cuppen E, Ellenbroek BA (2008a) Stress-induced hyperthermia and basal body temperature are mediated by different 5-HT(1A) receptor populations: a study in SERT knockout rats. Eur J Pharmacol 590:190–197
Olivier JD, Van Der Hart MG, Van Swelm RP, Dederen PJ, Homberg JR, Cremers T et al (2008b) A study in male and female 5-HT transporter knockout rats: an animal model for anxiety and depression disorders. Neuroscience 152:573–584
Olivier JD, Cools AR, Deen PM, Olivier B, Ellenbroek BA (2010a) Blockade of dopamine, but not noradrenaline, transporters produces hyperthermia in rats that lack serotonin transporters. Eur J Pharmacol 629:7–11
Olivier JDA, Blom T, Arentsen T, Homberg JR (2010b) The age-dependent effects of selective serotonin reuptake inhibitors in humans and rodents: a review. Progr Neuro Psychopharmacol Biol Psychiatr. doi:10.1016/j.pnpbp.2010.09.013
Paulson JF, Keefe HA, Leiferman JA (2009) Early parental depression and child language development. J Child Psychol Psychiatry 50:254–262
Popa D, Lena C, Alexandre C, Adrien J (2008) Lasting syndrome of depression produced by reduction in serotonin uptake during postnatal development: evidence from sleep, stress, and behavior. J Neurosci 28:3546–3554
Ramos SD, Lee JM, Peuler JD (2001) An inexpensive meter to measure differences in electrical resistance in the rat vagina during the ovarian cycle. J Appl Physiol 91:667–670
Ribas VR, Aniceto HK, Martins HA, Ribas KH, Guerra-Ribas RM, Fraga SN et al (2008) Neonatal administration of fluoxetine did not alter the anxiety indicators, but decreased the locomotor activity in adult rats in the elevated plus-maze. Arq Neuropsiquiatr 66:844–847
Romijn HJ, Hofman MA, Gramsbergen A (1991) At what age is the developing cerebral cortex of the rat comparable to that of the full-term newborn human baby? Early Hum Dev 26:61–67
Rosen RC, Lane RM, Menza M (1999) Effects of SSRIs on sexual function: a critical review. J Clin Psychopharmacol 19:67–85
Rowland D, McMahon CG, Abdo C, Chen J, Jannini E, Waldinger MD et al (2010) Disorders of orgasm and ejaculation in men. J Sex Med 7:1668–1686
Sikich L, Hickok JM, Todd RD (1990) 5-HT1A receptors control neurite branching during development. Brain Res Dev Brain Res 56:269–274
Silva CM, Goncalves L, Manhaes-de-Castro R, Nogueira MI (2010) Postnatal fluoxetine treatment affects the development of serotonergic neurons in rats. Neurosci Lett 483:179–183
Talge NM, Neal C, Glover V (2007) Antenatal maternal stress and long-term effects on child neurodevelopment: how and why? J Child Psychol Psychiatry 48:245–261
van den Hove DL, Blanco CE, Scheepens A, Desbonnet L, Myint AM, Leonard BE et al (2008) Prenatal maternal paroxetine treatment and neonatal mortality in the rat: a preliminary study. Neonatology 93:52–55
van Erp AM, Kruk MR, Meelis W, Willekens-Bramer DC (1994) Effect of environmental stressors on time course, variability and form of self-grooming in the rat: handling, social contact, defeat, novelty, restraint and fur moistening. Behav Brain Res 65:47–55
Ververs T, Kaasenbrood H, Visser G, Schobben F, de Jong-van den Berg L, Egberts T (2006) Prevalence and patterns of antidepressant drug use during pregnancy. Eur J Clin Pharmacol 62:863–870
Vorhees CV, Acuff-Smith KD, Schilling MA, Fisher JE, Moran MS, Buelke-Sam J (1994) A developmental neurotoxicity evaluation of the effects of prenatal exposure to fluoxetine in rats. Fundam Appl Toxicol 23:194–205
Waldinger MD, Hengeveld MW, Zwinderman AH, Olivier B (1998) Effect of SSRI antidepressants on ejaculation: a double-blind, randomized, placebo-controlled study with fluoxetine, fluvoxamine, paroxetine, and sertraline. J Clin Psychopharmacol 18:274–281
Acknowledgments
We thank Lars Valke, Mariëlle Winters, Loes Schiphouwer, and Anneke Sloet for their practical assistance. This research was financially supported by the Donders Centre for Neuroscience, Radboud University Nijmegen, The Netherlands, and a grant (no. 433-09-311) from The Netherlands Organisation for Scientific Research (NWO), awarded to J. Homberg. The Donders Centre for Neuroscience and NWO had no further role in the design of the study, in the collection, analysis, and interpretation of data, in the writing of the report, and in the decision to submit the paper for publication. The experiments comply with the current laws of the Netherlands.
Conflicts
The authors declare to have no conflicts of interest
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Olivier, J.D.A., Vallès, A., van Heesch, F. et al. Fluoxetine administration to pregnant rats increases anxiety-related behavior in the offspring. Psychopharmacology 217, 419–432 (2011). https://doi.org/10.1007/s00213-011-2299-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-011-2299-z