Abstract
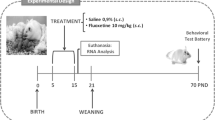
Selective serotonin reuptake inhibitor (SSRI)-type antidepressants are often prescribed to depressive pregnant women for their less adverse side effects. However, growing evidences have shown increased congenital malformations and poor neonatal adaptation in the perinatal SSRI-exposed human infants as well as animal pups. In this study, we examined the effects of early exposure of fluoxetine, the most popular SSRI-type antidepressant, on the developing somatosensory system. Physiological saline or fluoxetine (10 mg/kg) was subcutaneously injected into neonatal rats from P0 to P6. Somatosensory-related behaviors were examined in adolescence (P30–P35). Morphological features of the primary somatosensory cortex were checked at P7 and P35. The tactile and thermal perceptions as well as locomotor activity were affected by neonatal fluoxetine treatment. At the morphological level, the number of branch tips of thalamocortical afferents to the somatosensory cortex was reduced in the fluoxetine-treated rats. Furthermore, the spiny stellate neurons in the layer IV somatosensory cortex had reduced dendritic span and complexity with fewer branches, shorter dendritic length, and smaller dendritic field. The spine density of spiny stellate neurons was significantly reduced whereas the spine length of mushroom- and branched-type was increased. Taken together, these results indicate that neonatal fluoxetine administration has long-lasting effects on the function and structure in the somatosensory system. Sensory information processing may be disturbed in the neonatal fluoxetine-treated animals due to the structural deformation in the thalamocortical afferents and dendritic structures of the spiny stellate neurons in the layer IV somatosensory cortex.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Depressive disorders are often experienced among women during their childbearing years (Blazer et al. 1994). As such, antidepressants may be given to pregnant women for treating depression (Ververs et al. 2006). Selective serotonin reuptake inhibitor (SSRI)-type antidepressants are often prescribed due to their less adverse side effects (Källén 2004). SSRIs easily pass through the blood–brain barrier, inhibit the serotonin transporter (5HTT), and increase the extracellular serotonin level in the brain (Baumann and Rochat 1995). Serotonin toxicity resulting from SSRI ingestion has been noted and cautioned (Nelson et al. 2007). Moreover, growing evidence from both human and animal studies underscore congenital malformations and poor neonatal adaptation in perinatal SSRI-exposed infants and pups (Chambers et al. 1996; Laine et al. 2003; Moses-Kolko et al. 2005; Sanz et al. 2005; Bar-Oz et al. 2007; Borue et al. 2007; Noorlander et al. 2008; Van den Hove et al. 2008). Early SSRI exposure might be linked to cardiovascular malformations (Bar-Oz et al. 2007), whereas SSRI administration during late pregnancy could be associated with serotonin withdrawal syndromes (Moses-Kolko et al. 2005). Since serotonin plays important roles during brain development, the influence of SSRI on the developing nervous system is obvious (Xu et al. 2004; Oberlander et al. 2005; Maciag et al. 2006; Lisboa et al. 2007) yet the underlying mechanisms are poorly understood.
Some SSRI-related neonatal symptoms (such as convulsions, irritability, abnormal crying, and tremors) are transient, and may disappear within few weeks (Laine et al. 2003; Sanz et al. 2005). However, some changes following early SSRI exposure seem to be long lasting. The expression of tryptophan hydroxylase, the key enzyme for serotonin synthesis, in brainstem raphe nuclei, the center of pain modulation, is constantly reduced after neonatal SSRI treatment (Maciag et al. 2006). In human studies, it has been reported that newborns prenatally exposed to SSRI exhibit blunted somatosensation, particularly pain reactivity, and this phenomenon persists for months (Oberlander et al. 2005). This finding suggests that early exposure to SSRI during a developmentally sensitive period may cause long-term alterations in brain development and function.
Pharmacological treatments, including SSRI, in rodents which elevate serotonin levels cause impaired axonal patterning in the somatosensory cortex (Cases et al. 1996; Vitalis et al. 1988; Young-Davies et al. 2000; Xu et al. 2004). It is most effective when the drugs are given within an early period, first two postnatal weeks, which corresponds to the third trimester of human fetal stage (Romijn et al. 1991). The rodent whisker-to-somatosensory cortex pathway is an excellent model system for examining the mechanisms in the cortical development (Gaspar et al. 2003; Luo et al. 2003). Patches of thalamocortical afferent (TCA) arbors and their postsynaptic partners, layer IV spiny stellate neurons, form discrete modules known as “barrels” that replicate the patterned distribution of whiskers on the contralateral snout (Woolsey and Van der Loos 1970). An earlier study has demonstrated that neonatal SSRI administration from postnatal day 0 (date of birth, P0) to P8 reduces the size of the cortical barrels by interfering with the refinement of the TCA arbors (Xu et al. 2004). These results provide the possible anatomical basis for the early SSRI exposure-related functional impairments.
Neonatal SSRI exposure might disorganize the shaping of axonal and dendritic structures, which lead to altered behavioral performances. To test this hypothesis, we examined structural alterations in the barrel cortex of fluoxetine-treated rat pups and their somatosensory-related behaviors. The results demonstrate that neonatal fluoxetine administration has long-lasting effects on the structure and function of the somatosensory system.
Materials and Methods
Subjects
Newborn (postnatal day 0, P0) Wistar rat pups of both sexes were used in this study. All rat pups were kept with their mother until weaned after three weeks of age. Animals were housed in the Laboratory Animal Center of National Taiwan University College of Medicine under 12-h light/dark cycle with free access to food and water. Some rats were sacrificed for TCA labeling at P7. Others were raised and used for behavioral examinations (P30–P35). After behavioral tests, all rats were sacrificed and the brains were processed for Golgi-Cox impregnation. Body weight of rat pups was measured weekly. All animal handling was in accordance with a protocol approved by National Taiwan University College of Medicine and College of Public Health Institutional Animal Care and Use Committee.
Drug Treatment
Rat pups received physiological saline (Control, n = 36) or fluoxetine hydrochloride (F 0–6, n = 42, 10 mg/kg/day in physiological saline) subcutaneously from P0 to P6. The dosage was comparable to the previous neonatal SSRI studies (Xu et al. 2004; Maciag et al. 2006; Ansorge et al. 2008). This period was chosen because the thalamocortical afferents achieve adult-like pattern by the end of the first postnatal week (Rebsam et al. 2002). This period also corresponds to the third trimester in human pregnancy (Romijn et al. 1991).
Behavioral Examinations
Adolescent rats (P30–P35) of control group (n = 15) and fluoxetine-treated group (n = 12) were used in behavioral tests.
Hotplate Test
The hotplate test was conducted by placing the rat on a metal surface of the hot plate meter (Ugo Basile, Comerio, Italy) maintained at 50°C. The latency to first licking of a hind paw was recorded. The tested animal was removed after 60 s if no response was made to prevent tissue damage and 60 s was given as a record.
Gap-Crossing Test
The gap-crossing apparatus was modified from Hutson and Masterton (1986). In brief, the custom-made apparatus (78 × 29.5 × 29.5 cm in length × width × height) was built from wood. The floor was 21 cm high and composed of two platforms (39 cm long) with a gap in between (Fig. 3a). One platform was covered with a ceiling as the dark side, and the other platform was left uncovered as the bright side. Once placed in the bright side, all rats moved to the dark side instinctively without training. To reduce the explorative activity, a set of transparent plastic wall was used to form a no return path in the bright side. The gap distance between two sides could be widened centimeter by centimeter. The gap-crossing procedure was conducted in a series of increasing gap distance until the maximum crossable distance was determined.
Open Field Test
The open field behavioral testing was conducted by using a photobeam activity system (San Diego Instruments, San Diego, CA) under low light conditions. Animals were habituated to the testing environment 30 min before test. The animal was placed into the center of the clear plastic activity chamber (45.7 × 45.7 × 38 cm in length × width × height) equipped with 16 × 16 infrared beams in each directions with 2.5 cm interval and then the horizontal activity was detected. Vertical activity was detected with another set of photobeams 5.5 cm above the chamber floor. Activity was recorded for 15 min. Central (17.5 × 17.5 cm2) and peripheral counts for fine movement, ambulation, and total rearing counts were recorded.
Histology
DiI Labeling of Thalamocortical Afferents
One day after the last drug treatment (P7), rats (for control group, n = 21; for fluoxetine-treated group, n = 30) were sacrificed by overdose of chloral hydrate and perfused transcardially with phosphate-buffered saline followed by fixative (4% paraformaldeyhde in phosphate buffer, pH 7.4). After perfusion, the brain was extracted and postfixed in the same fixative. Sections were cut at a nonconventional angle combination to preserve the thalamocortical projections (Lee et al. 2005a). Cutting angles were slightly adjusted for the rat pups. Two to three thick sections (300 μm) per hemisphere were taken for TCA labeling. One small crystal of DiI (Molecular Probes, Eugene, OR) was picked and inserted into the ventroposteromedial nucleus of thalamus with a 30-gage needle under a dissection microscope. Sections were then placed in the fixative and kept in the dark for 4–6 weeks at room temperature for dye diffusion. DiI-labeled thalamocortical afferents were then examined under a fluorescence or confocal microscope for image processing.
Golgi-Cox Impregnation
After the behavioral examinations, adolescent rats (for control group, n = 15; for fluoxetine-treated group, n = 12) were sacrificed, perfused, and fixed for morphological analyses. To visualize dendritic structures, Golgi-Cox method was used (Lee et al. 2005b). In brief, flattened cortices were immersed into an impregnation solution (mixture of solution A: 1.0 g potassium dichromate and 1.0 g mercuric chloride in 85 ml distilled water with solution B: 0.8 g potassium chromate and 0.5 g sodium tungstate in 20 ml distilled water) at room temperature for 4–5 days. After impregnation, specimens were cut tangentially at thickness of 100 μm with a vibratome. Sections were collected and reacted with 15% ammonium hydroxide for 2 min and rinsed thoroughly in distilled water. Subsequently, sections were placed in diluted (1:5) rapid fixer solution (Ilford, Marly, Switzerland) for 10 min and rinsed thoroughly in distilled water. All sections were then counterstained with cresyl violet (Nissl stain), dehydrated through series of alcohols and mounted with Depex (Electron Microscopy Sciences, Washington, PA).
Morphometric Analysis
Axons
DiI-labeled thalamocortical afferents were examined under a Leica TCS SP2 confocal microscope (Heidelberg, Germany). Cases in which a single axon could be traced from the internal capsule were collected. Reconstructions were made from image stacks using imageJ software (1.36, NIH, Bethesda, MD) and photoshop software (Adobe, San Jose, CA). The lateral extent and terminal tips of each individual afferent arbor were measured.
Dendrites
Golgi-Cox-impregnated neurons from adolescent rats were examined under an Olympus light microscope (Tokyo, Japan) with a 40× lens and reconstructed using a cameralucida drawing tube. Layer IV spiny stellate cells were chosen for morphological examinations by the following criteria: (1) in the barrel wall; (2) spiny appearance; (3) orientated dendrites; and (4) complete dendritic arbor. The dendrites derived directly from the soma are the first-order branches or primary dendrites. The daughter branches arising from that are second-order branches, and so on. The point at which a dendrite gives rise to two daughter branches is called a branching point. The termination of a dendrite is called a terminal ending. The dendritic field area was defined as the outline of terminal endings. The somatodendritic parameters, the soma size, dendritic field area, and total dendritic length were measured from the two-dimensional display by ImageJ program. The number of primary dendrites, branching points, and terminal endings were counted manually. The concentric sphere method of Sholl (1953) was used to analyze dendritic branching complexity.
Dendritic Spines
The number of total dendritic spines was counted from Golgi-Cox-impregnated layer IV spiny stellate neurons. The spine density was determined from the 1st to 4th dendritic orders. Dendritic spines were further classified by their morphology (Sorra and Harris 2000): mushroom (spine head is greater than 0.6 μm in diameter), branched, stubby (short without head), and thin (long with a head less than 0.6 μm in diameter). The length of individual spines (distance between the spine tip and stalk of dendrite) was also measured.
Statistical Analysis
The two-tailed Student’s t-test was applied for statistical evaluation of mean. Data were expressed as mean ± SEM. The statistical criterion for significance was P < 0.05.
Results
Body Weight
During and after fluoxetine treatment, rat pups had significantly reduced body weight (24% reduction at P7, as compared with saline-treated rats, Fig. 1). It was comparable with the result of neonatal paroxetine injections (Xu et al. 2004). After the cessation of drug treatment, the body weight of fluoxetine-exposed rats gradually caught up. At P28, there was no significant difference in body weight between saline- and drug-treated rats.
Body weight of rats in saline (control) and drug-treated (F 0–6) groups. Animals were weighed every week after birth (P0). They had comparable body weight at the beginning (P0). After treatment, fluoxetine-exposed rats had slightly but significantly reduced body weight at the first (P7), second (P14), and third (P21) weeks. At the fourth week (P28), however, rats in both groups had similar body weight. Results are mean ± SEM. (*P < 0.05, ***P < 0.001, Student’s t-test)
Somatosensory-Related Behavioral Performances
The structure of the somatosensory cortex is affected by neonatal SSRI treatment (Xu et al. 2004). We therefore tested if the somatosensory-related behavioral performances were likewise affected. The function of spinothalamic pathway (carrying pain and thermal information) was examined by hotplate for determining the threshold for thermal pain. Compared with the control animals (17.8 ± 5.73 s), fluoxetine-treated rats have longer latency (37.8 ± 13.01 s, P < 0.001) to the first licking on the hotplate, implying a higher thermal threshold (Fig. 2). This result corresponded well with the blunted pain reactivity of prenatal SSRI-treated infants (Oberlander et al. 2005) and suggested that early fluoxetine exposure may cause long-term perceptual effects on the pain system.
To examine the function of medial lemniscal sensory pathway (carrying tactile information), a gap-crossing test was used (Fig. 3). A rat was placed in the bright side of the testing apparatus and would scuttle to the dark side by animal nature without training. Normally, the maximum crossable gap distance of adolescent rats (P30–P35) was between 6 and 8 cm (7.07 ± 0.22 cm, n = 15). Rats are tactile animals and many behaviors are reliant on whisker-specific perception. To prove the maximum crossable distance is whisker dependent, another set of same-aged rats were used. All whiskers on both sides of the face were completely cut right before the gap-crossing test. These whisker-cut rats behaved normally while crossing short gap distance (0–4 cm). When the gap distance was widened up to 5 cm, some extended their head and spent much more time by the edge. The maximum crossable distance of the whisker-cut rats was significantly reduced (5.05 ± 0.28 cm, P < 0.001, n = 13) compared with controls. Fluoxetine-exposed adolescent rats had significant shorter maximum crossable gap distance (4.54 ± 0.37 cm, P < 0.001, n = 12) compared with saline-treated (control) rats but similar to the age-matched whisker-cut rats (Fig. 3b). The whisker function-dependent gap-crossing performance was altered in the fluoxetine-treated rats. This result implied that in these rats, the whisker-specific tactile function is impaired.
The gap-crossing test. Lateral and top views of the testing apparatus are illustrated (a). Normally, the maximum crossable gap distance of adolescent rats (P30–P35) was between 6 and 8 cm (7.07 cm in average). The fluoxetine-exposed (F 0–6) rats (n = 12) had significant shorter crossable gap distance compared with the saline-treated (control) rats (n = 15) but similar to whisker-cut rats (n = 13) of the same age (b). Results are mean ± SEM. (***P < 0.001, Student’s t-test)
While the perceptive function of the adolescent rats is affected by neonatal fluoxetine treatment, their explorative activity may be affected as well. To test this possibility, an open field test was conducted. Total fine movement counts were indistinguishable between two groups (160.4 ± 6.8 in controls, 154.3 ± 6.6 in fluoxetine-treated rats, respectively, P = 0.54, Fig. 4a). However, the total ambulation counts in the drug-treated rats were reduced (1106.12 ± 75.14, n = 12, as compared with controls, 1380.22 ± 97.81, n = 15, P < 0.05), especially in the central area (212.1 ± 30.61, as compared with controls, 335.92 ± 29.33, P < 0.05, Fig. 4b). No significant difference in the peripheral area was found (1044.3 ± 104.21 in controls, 894 ± 50.71 in fluoxetine-treated rats, respectively, P = 0.24). Furthermore, the counts of rearing were also reduced in these rats (144.81 ± 8.52) compared with controls (178.22 ± 10.64, P < 0.05, Fig. 4c). These results suggested that the altered explorative behavior was due to neonatal fluoxetine treatment.
Locomotor activity in the open field. For saline (control, n = 15) and fluoxetine-treated (F 0–6, n = 12) animals, the total fine movement counts within 15 min were indistinguishable (a). However, fluoxetine-treated (F 0–6) rats, exhibited less ambulation within 15 min compared with controls practically in the central region (b). The rearing counts in fluoxetine-treated (F 0–6) rats were also reduced (c). Results are mean ± SEM. (*P < 0.05, Student’s t-test)
Thalamocortical Afferent Arbors
The anatomical basis for the somatosensory-related functional impairments was then examined. Barrel patterns are composed of patches of TCA arbors and their postsynaptic partners, layer IV cortical neurons. The TCAs reach the adult-like pattern by the end of the first postnatal week (Rebsam et al. 2002); therefore, we examined the morphology of DiI-labeled TCAs in P7 rats. Individual TCAs were imaged and reconstructed from the image stacks (Fig. 5a, b). TCAs in P7 control rats had adult-like afferent arbors (Fig. 5a) whereas in the drug-treated group, TCA patches appeared smaller (Fig. 5b). However, in some cases, overshoot or much wider arbors were seen (Fig. 5b, the two from the right). Due to great variation within the drug-treated group, no significant difference in the widest extent was found between the two groups (281.4 ± 36 μm in controls, n = 9 arbors, 6 animals; 293.9 ± 34 μm in fluoxetine-treated rats, n = 28 arbors, 12 animals, P = 0.79, Fig. 5c). The heterogeneity in lateral extent of individual TCAs just fits well with the previous observation of smaller and less segregated TCA patches in neonatal paroxetine-treated rats (Xu et al. 2004). Individually reconstructed TCAs provided more detailed information. The branching pattern of TCAs was analyzed. In fluoxetine-treated animals, the TCAs had fewer branches and the number of terminal tip was significantly reduced (19.84 ± 2.92 as compared with controls, 40.33 ± 2.32, P < 0.01, Fig. 5d). These findings were similar to the phenotype in mice lacking monoamine oxidase A (MAOA), the key enzyme that catalyzes serotonin (Rebsam et al. 2002).
DiI-labeled thalamocortical afferents of P7 rats. Thalamocortical afferents were labeled with DiI and reconstructed (a, b). TCAs in fluoxetine-treated group (F 0–6, n = 28) have smaller arbor clusters compared with the control ones (n = 9) but not statistically significant (c). Note that in some cases, overshot or much wider arbors were seen (two from the right in b). Nevertheless, TCAs in fluoxetine-treated rats exhibited fewer terminal tips within layer IV compared with the controls (d). Layer IV is delineated by the two short bars. Bar is 80 μm in (a) and (b). Results are mean ± SEM. (**P < 0.01, Student’s t-test)
Dendritic Arbors
The major postsynaptic targets of TCAs are the layer IV cortical neurons in the somatosensory cortex. The layer IV spiny stellate neurons are glutamatergic, receiving excitatory inputs from TCAs and relaying sensory information to other layers within a cortical column (Lübke et al. 2000). These cells are located in the barrel wall and orientate most of their dendrites toward the barrel hollow forming synapses with TCA arbors (Datwani et al. 2002). Golgi-Cox-impregnated neurons in the barrel field were chosen according to their location, orientation, and spiny appearance (Fig. 6a). The cells from the control (n = 52 neurons from 8 animals) and fluoxetine-exposed rats (n = 76 neurons from 8 animals) had comparable soma size (P = 0.1) and same number of primary dendrites (3.1 ± 0.16 vs. 3.1 ± 0.1, P = 0.99), ensuring that the same type of cells was collected. These reconstructed neurons were then subjected to morphometric analysis. Compared with the neurons in saline-treated rats, those in fluoxetine-treated rats had smaller (26.6% reduction) dendritic field (64036.22 ± 2182.51 μm2, as compared with control, 85291.14 ± 3987.52 μm2, P < 0.001, Fig. 6b) and shorter total dendritic length (653.62 ± 16.92 μm, as compared with controls, 821.91 ± 27.91 μm in controls, P < 0.001, Fig. 6c). Neurons in fluoxetine-treated rats also had reduced dendritic complexity: fewer intersections in the distal region of Sholl’s concentric rings (Fig. 6d), less dendritic orders (5.12 ± 0.14 as compared with controls, 6.52 ± 0.16, P < 0.001, Fig. 6e), and fewer terminal endings (653.63 ± 17.42 μm, as compared with controls, 821.92 ± 27.91 μm, P < 0.001, Fig. 6f).
Layer IV spiny stellate cells in the rat barrel cortex. Golgi-Cox-impregnated layer IV spiny stellate cells were reconstructed with the aid of cameralucida drawing system. In this illustration, all dendritic spines are omitted (a). The layer IV spiny stellate cells in fluoxetine-treated rats (n = 76 neurons) had smaller dendritic field (b) and reduced total dendritic length (c) compared with normal ones (n = 52 neurons). Dendritic complexity was estimated by Sholl analysis (d). The number of intersections in the proximal region (within 40 μm from the soma) was indistinguishable between the two groups, whereas fewer intersections were counted in the distal region (beyond 40 μm from the soma) in fluoxetine-treated cases. These cells also had fewer dendritic orders (e) and less terminal endings (f). Bar is 100 μm. Results are mean ± SEM. (***P < 0.001, Student’s t-test)
Dendritic Spines
The density and shape of dendritic spines of layer IV spiny stellate neurons in the barrel field were also examined (Fig. 7). The highest dendritic order in all examined neurons was between 4 and 8; therefore, the calculation of spine density was limited from the 1st to 4th dendritic orders. The primary dendrite had the lowest spine density in both saline-treated and fluoxetine-treated groups and no difference was found between two groups. However, in the neurons of fluoxetine-treated rats, the spine density was significantly (P < 0.001) reduced in the 2nd (0.59 ± 0.11/μm, vs. 1.21 ± 0.11/μm of controls), 3rd (0.69 ± 0.04/μm, as compared with controls, 1.18 ± 0.05/μm), and 4th (0.79 ± 0.07/μm, as compared with controls, 1.32 ± 0.13/μm) dendritic orders (Fig. 7b). With decreased spine density and presynaptic TCA terminal tips (Fig. 5d), these findings indicate that the functional synaptic contacts between TCAs and layer IV cortical neurons might be greatly reduced.
Density and length of the dendritic spines. The dendritic spines of layer IV spiny stellate cells in the somatosensory cortex were revealed by Golgi-Cox impregnation method (a). Spine density was determined at each dendritic order (1st to 4th). The density of total spine was significantly reduced in fluoxetine-treated (F 0–6) rats compared with controls, especially in the 2nd, 3rd, and 4th dendritic orders (b). However, in the fluoxetine-treated rats, the length of mushroom- and branched-type spines was increased (c). Bar is 5 μm in (a). Results are mean ± SEM. (*P < 0.05, ***P < 0.001, Student’s t-test)
Dendritic spines were further classified by their morphology: mushroom, branched, stubby, and thin (Sorra and Harris 2000). The length of mushroom-type and branched-type spines was increased in the neurons of fluoxetine-exposed rats (mushroom-type: 1.52 ± 0.06 μm in fluoxetine-treated rats, 1.31 ± 0.06 μm in controls, P < 0.05; branched-type: 1.93 ± 0.11 μm in fluoxetine-treated rats, 1.42 ± 0.07 μm in controls, P < 0.001). However, the length of stubby and thin spines was not affected by neonatal fluoxetine treatment (Fig. 7c).
Discussion
This is the first study demonstrating that neonatal fluoxetine exposure during the first postnatal week, corresponding to the third trimester of human pregnancy, causes long-lasting effects on the structure and consequentially the function of the somatosensory system. At the behavioral level, fluoxetine-treated rats exhibit blunt thermal and tactile perceptions and less explorative activity. In the structural aspect, thalamocortical afferents to the somatosensory cortex have fewer branches in layer IV and layer IV spiny stellate neurons have reduced dendritic occupancy, complexity, and spine density but elongated length in mushroom and branched spines. The results suggest that sensory information processing may be disturbed in the neonatal fluoxetine-treated animals due to structural deformation in thalamocortical afferents and dendritic structures of the spiny stellate neurons in layer IV somatosensory cortex.
Serotonergic Regulation in the Developing Somatosensory Cortex
For neural development in rodents, the critical window for the somatosensory system formation is the first two postnatal weeks (see Inan and Crair 2007 for a review). During this period, serotonin transporter (5-HTT), the target of SSRI, and serotonin1B receptor (5-HT1BR) display transient high expression level in the TCAs (Bennett-Clarke et al. 1993, 1996; Lebrand et al. 1996, 1998). The serotonin level, as well as 5-HTT and 5-HT1BR functions, are highly regulated; any manipulation that results in elevated serotonin level, reduced 5-HTT function, or activated 5-HT1BR activity disturbs TCA patterning and barrel formation (Cases et al. 1996; Vitalis et al. 1988; Young-Davies et al. 2000; Persico et al. 2001; Salichon et al. 2001; Kesterson et al. 2002; Rebsam et al. 2002; Xu et al. 2004). Electrophysiological recordings have demonstrated that serotonin inhibits the glutamatergic neurotransmission between thalamic axons and neurons in the barrel cortex and the serotonin-induced reduction of glutamate release is mediated by 5-HT1BR (Rhoades et al. 1994; Laurent et al. 2002). In other words, increased serotonin level resulted from SSRI treatment may activate 5-HT1BR and thus suppressing the release of glutamate. Many lines of evidence have suggested synaptic activity-dependent retrograde signaling system is involved in the shaping of axonal arbors (see Debski and Cline 2002; Schmidt 2004 for reviews). Reduced neurotransmitter release may thus weaken this system and interfere with the refinement of TCAs. In fact, insufficient glutamate release has been shown to be a pathogenic factor for the exuberant TCA morphology in the barrelless mice (Lu et al. 2006). In this study, pharmacological blockade of 5-HTT by fluoxetine during early postnatal period may build excess serotonin surrounding the developing TCA terminals, activating 5-HT1BR, inhibiting the release of glutamate, and lead to disorganized TCA morphology (Fig. 5).
In addition to the altered TCA arbors, the dendritic characteristics of their postsynaptic partners, layer IV cortical neurons are also affected by neonatal fluoxetine treatment (Fig. 6). In adult animals, continual fluoxetine administration to rodents increases the total dendritic length of hippocampal CA1 neurons (Norrholm and Ouimet 2000) as well as newly generated granule cells in the dentate gyrus (Wang et al. 2008). These results seem opposite to the present finding. However, the time window chosen in this study is quite unique, the 5-HTT and 5-HT1BR are transiently expressed in the barrel field during this period. Rather than the trophic effect (Brezun and Daszuta 2000), serotonin here suppresses the dendritic development and presumably through interfering with the excitatory neurotransmission. In supporting this hypothesis, data have shown that blockade of synaptic currents during the first postnatal week leads to decreased total length of basal dendritic tree of CA1 hippocampal neurons in rat (Groc et al. 2002). Taken together, the present findings suggest that serotonin acts as a regulator of glutamatergic transmission during neural development for the sculpting of growing TCAs and their postsynaptic partners (Erzurumlu and Kind 2001; Gaspar et al. 2003).
In the cortex-specific NMDAR knockout mice, the synaptic activity in the barrel cortex is reduced (Iwasato et al. 2000) and disorganized TCAs and altered dendritic structures in layer IV spiny stellate cells are reported (Datwani et al. 2002; Lee et al. 2005a). However, the phenotypes of the knockout mice are somewhat different from the present findings. These discrepancies may indicate different compensatory mechanisms in response to genetic and pharmacological manipulations yet also imply that in addition to the glutamatergic pathway, other systems are as well affected by early SSRI treatment. It is known that the 5-HT2ARs are also transiently expressed in the developing barrel cortex (Mansour-Robaey et al. 1998). Since, misexpression of 5-HT2AR affects dendritic morphogenesis (Bou-Flores et al. 2000), it is very likely that 5-HT2AR plays important role in the dendritic phenotype observed in the SSRI-exposed animals. Agonist and antagonist of 5-HT2AR are now being used to test this possibility. Moreover, the involvement of other serotonin or glutamate receptors in the process of axonal and dendritic refinement still remains to be clarified (Muñoz et al. 1999; Hannan et al. 2001; Spires et al. 2005).
Morphological abnormalities in dendritic spine are often seen in various types of mental disorders (Kaufmann and Moser 2000; Fiala et al. 2002; Calabrese et al. 2006). Spine number is decreased in patients and animal models of schizophrenia (Glantz and Lewis 2000; Silva-Gómez et al. 2003), epilepsy (Swann et al. 2000), and Alzheimer’s disease (Baloyannis et al. 2007; Knobloch and Mansuy 2008), whereas elongated spines are present in mentally retarded children (Purpura 1974) and animal models (McKinney et al. 2005; Khelfaoui et al. 2007). This study demonstrates for the first time that neonatal fluoxetine exposure alters dendritic structures. Reduced dendritic length, complexity, and spine density are signs of developmental defects (Kaufmann and Moser 2000), whereas elongated spine length is associated with immaturity (Khelfaoui et al. 2007). How fluoxetine affect the developmental program of dendritic structures is largely unknown.
SSRI in the Developing Sensory System
Neonatal fluoxetine exposure reduces the number of presynaptic TCA terminal tips (Fig. 5) and density of postsynaptic dendritic spine in layer IV spiny stellate cells (Fig. 7). The functional synaptic contacts are presumably reduced, rendering excitatory synaptic transmission inadequate. Consequently, the animals are less perceptive to the environmental information. In deed, with intact whiskers, however, the drug-treated rats exhibit short crossable gap distance similar to the whisker-cut rats, implying that their whisker-dependent sensory system is impaired (Fig. 3). A recent study, using functional measurement, local cerebral glucose utilization, has reported that the neural activity in the somatosensory system is reduced in the 5-HTT knockout mice (Esaki et al. 2005). These results validate the functional impairments reported here in fluoxetine-treated rats. Moreover, rodents are tactile animals and whiskers on the face are their major sensory organ; therefore, many behaviors are reliant on whisker functions (Brecht 2007; Petersen 2007; Diamond et al. 2008). With altered somatosensations, fluoxetine-exposed rats also exhibit less explorative activities (ambulation and rearing, Fig. 4), implying the distortion in sensory integration for sensory-related decision making (Celikel and Sakmann 2007) with or without concomitant impairment in sensory-motor coordination. In fact, in a mouse model lacking monoamine oxidase A (MAOA), the key enzyme that metabolizes serotonin, excess serotonin level, absence of barrels, exuberant TCAs, and impaired beam walking ability are reported (Salichon et al. 2001; Rebsam et al. 2002). Clinically, whether early SSRI exposure in human fetuses may generate signs of sensory integration dysfunction (such as sensory ataxia and abnormal stance or gait) later in life has not yet been examined.
Oberlander and colleagues (2005) have reported newborns that prenatally exposed to SSRI exhibit blunted pain reactivity and this phenomenon persist for months. These findings suggest that transplacental exposure of SSRI during a developmentally sensitive period may cause long-term alterations in brain development and function (Oberlander et al. 2005). In this work, we demonstrate that neonatal fluoxetine treatment increases the threshold of thermal pain (Fig. 2). Together, evidences from human and animal studies suggest that early-life fluoxetine exposure may cause long-term perceptual effects on the pain system.
The sensitivity of pain is regulated by serotonin at various levels, including peripheral effects (Millan 2002; Sommer 2004). Originally, serotonin is conceived as an analgesic. In rodents and primates, 5-HTT is transiently expressed in the nonserotonergic sensory ganglion (Lebrand et al. 1998, 2006). SSRI inhibits the reuptake of serotonin and builds excess extracellular serotonin in the sensory pathway, thus attenuate the pain sensation. However, there are still different points of view. Neonatal chronic SSRI treatment (P8–P21) downregulates the expression of tryptophan hydroxylase, the key enzyme for serotonin synthesis, in the brainstem serotonergic raphe nuclei (Maciag et al. 2006). This long-term effect of SSRI treatment may be achieved by a negative feedback regulation of serotonin biosynthesis and explains the reduced serotonin level in 5-HTT knockout mice (Vogel et al. 2003). Therefore, the hyperalgesic effect of serotonin should also be considered (Millan 2002). Formalin-induced pain reaction is greatly reduced by serotonin depletion (Svensson et al. 2006). When the synthesis of serotonin is disrupted prenatally, the formalin-evoked pain behaviors are significantly decreased later in life (Butkevich et al. 2003). Our current project is to explore the impact of early fluoxetine exposure on the development of pain sensitivity and differentiate the roles (analgesic or hyperalgesic) of serotonergic modulation involved.
Emotional Effect of Serotonin
Altered locomotor activity can also be associated with emotional disorders. Anxiety, for example, can be evaluated with the open field test for anxious animals tend to avoid the central region of the field. The 5-HTT knockout mice are known for their anxiety-like behaviors (Holmes et al. 2003). In the open field test, 5-HTT knockout mice show reduced vertical exploration and reduced central but not peripheral horizontal activity (Kalueff et al. 2007). In this study, exact same results are generated in the neonatal fluoxetine-exposed rats (Fig. 4). These results, on one hand, imply that the anxiety-like behaviors might have, at least in part, apathetic perceptual basis. The reduced neural activity in the somatosensory system of 5-HTT knockout mice in a glucose utilization functional assay also supports this scheme (Esaki et al. 2005). Abnormal behaviors may be due to abnormal perception and recognition. On the other hand, we can not exclude the emotional effect of neonatal fluoxetine treatment on the behavioral performances, although it may take several months to build its effect on locomotor activity (Ansorge et al. 2008). Whether early-life fluxetine-exposed rats are more anxious can be examined by numerous behavioral tests. However, these are beyond the scope of the present work. Nevertheless, our findings provide solid anatomical evidences for the impaired somatosensory-related behavioral performance in the drug-treated animals.
In summary, fluoxetine exposure to rat pups during the critical time window corresponding to the third trimester in human pregnancy has long-lasting adverse effects on the function and structure of the somatosensory system. Current clinical guideline permits the use of fluoxetine for treatment of depressive disorder during pregnancy. The present results demonstrate that early SSRI exposure might have more serious long-term sequelae than have been previously assumed. Therefore, caution should be taken with regard to taking SSRI during pregnancy.
References
Ansorge MS, Morelli E, Gingrich JA (2008) Inhibition of serotonin but not norepinephrine transport during development produces delayed, persistent perturbations of emotional behaviors in mice. J Neurosci 28:199–207
Baloyannis SJ, Costa V, Mauroudis I, Psaroulis D, Manolides SL, Manolides LS (2007) Dendritic and spinal pathology in the acoustic cortex in Alzheimer’s disease: morphological and morphometric estimation by Golgi technique and electron microscopy. Acta Otolaryngol 127:351–354
Bar-Oz B, Einarson T, Einarson A, Boskovic R, O’Brien L, Malm H, Bérard A, Koren G (2007) Paroxetine and congenital malformations: meta-analysis and consideration of potential confounding factors. Clin Ther 29:918–926
Baumann P, Rochat B (1995) Comparative pharmacokinetics of selective serotonin reuptake inhibitors: a look behind the mirror. Int Clin Psychopharmacol 10(Suppl 1):15–21
Bennett-Clarke CA, Leslie MJ, Chiaia NL, Rhoades RW (1993) Serotonin 1B receptors in the developing somatosensory and visual cortices are located on thalamocortical axons. Proc Natl Acad Sci USA 90:153–157
Bennett-Clarke CA, Chiaia NL, Rhoades RW (1996) Thalamocortical afferents in rat transiently express high-affinity serotonin uptake sites. Brain Res 733:301–306
Blazer DG, Kessler RC, McGonagle KA, Swartz MS (1994) The prevalence and distribution of major depression in a national community sample: the National Comorbidity Survey. Am J Psychiatry 151:979–986
Borue X, Chen J, Condron BG (2007) Developmental effects of SSRIs: lessons learned from animal studies. Int J Dev Neurosci 25:341–347
Bou-Flores C, Lajard AM, Monteau R, De Maeyer E, Seif I, Lanoir J, Hilaire G (2000) Abnormal phrenic motoneuron activity and morphology in neonatal monoamine oxidase A-deficient transgenic mice: possible role of a serotonin excess. J Neurosci 20:4646–4656
Brecht M (2007) Barrel cortex and whisker-mediated behaviors. Curr Opin Neurobiol 17:408–416
Brezun JM, Daszuta A (2000) Serotonin may stimulate granule cell proliferation in the adult hippocampus, as observed in rats grafted with foetal raphe neurons. Eur J Neurosci 12:391–396
Butkevich IP, Khozhai LI, Mikhailenko VA, Otellin VA (2003) Decreased serotonin level during pregnancy alters morphological and functional characteristics of tonic nociceptive system in juvenile offspring of the rat. Reprod Biol Endocrinol 1:96
Calabrese B, Wilson MS, Halpain S (2006) Development and regulation of dendritic spine synapses. Physiology (Bethesda) 21:38–47
Cases O, Vitalis T, Seif I, De Maeyer E, Sotelo C, Gaspar P (1996) Lack of barrels in the somatosensory cortex of monoamine oxidase A-deficient mice: role of a serotonin excess during the critical period. Neuron 16:297–307
Celikel T, Sakmann B (2007) Sensory integration across space and in time for decision making in the somatosensory system of rodents. Proc Natl Acad Sci USA 104:1395–1400
Chambers CD, Johnson KA, Dick LM, Felix RJ, Jones KL (1996) Birth outcomes in pregnant women taking fluoxetine. N Engl J Med 335:1010–1015
Datwani A, Iwasato T, Itohara S, Erzurumlu RS (2002) NMDA receptor-dependent pattern transfer from afferents to postsynaptic cells and dendritic differentiation in the barrel cortex. Mol Cell Neurosci 21:477–492
Debski EA, Cline HT (2002) Activity-dependent mapping in the retinotectal projection. Curr Opin Neurobiol 12:93–99
Diamond ME, von Heimendahl M, Knutsen PM, Kleinfeld D, Ahissar E (2008) ‘Where’ and ‘what’ in the whisker sensorimotor system. Nat Rev Neurosci 9:601–612
Erzurumlu RS, Kind PC (2001) Neural activity: sculptor of ‘barrels’ in the neocortex. Trends Neurosci 24:589–595
Esaki T, Cook M, Shimoji K, Murphy DL, Sokoloff L, Holmes A (2005) Developmental disruption of serotonin transporter function impairs cerebral responses to whisker stimulation in mice. Proc Natl Acad Sci USA 102:5582–5587
Fiala JC, Spacek J, Harris KM (2002) Dendritic spine pathology: cause or consequence of neurological disorders? Brain Res Brain Res Rev 39:29–54
Gaspar P, Cases O, Maroteaux L (2003) The developmental role of serotonin: news from mouse molecular genetics. Nat Rev Neurosci 4:1002–1012
Glantz LA, Lewis DA (2000) Decreased dendritic spine density on prefrontal cortical pyramidal neurons in schizophrenia. Arch Gen Psychiatry 57:65–73
Groc L, Petanjek Z, Gustafsson B, Ben-Ari Y, Hanse E, Khazipov R (2002) In vivo blockade of neural activity alters dendritic development of neonatal CA1 pyramidal cells. Eur J Neurosci 16:1931–1938
Hannan AJ, Blakemore C, Katsnelson A, Vitalis T, Huber KM, Bear M, Roder J, Kim D, Shin HS, Kind PC (2001) PLC-beta1, activated via mGluRs, mediates activity-dependent differentiation in cerebral cortex. Nat Neurosci 4:282–288
Holmes A, Lit Q, Murphy DL, Gold E, Crawley JN (2003) Abnormal anxiety-related behavior in serotonin transporter null mutant mice: the influence of genetic background. Genes Brain Behav 2:365–380
Hutson KA, Masterton RB (1986) The sensory contribution of a single vibrissa’s cortical barrel. J Neurophysiol 56:1196–1223
Inan M, Crair MC (2007) Development of cortical maps: perspectives from the barrel cortex. Neuroscientist 13:49–61
Iwasato T, Datwani A, Wolf AM, Nishiyama H, Taguchi Y, Tonegawa S, Knöpfel T, Erzurumlu RS, Itohara S (2000) Cortex-restricted disruption of NMDAR1 impairs neuronal patterns in the barrel cortex. Nature 406:726–731
Källén B (2004) Neonate characteristics after maternal use of antidepressants in late pregnancy. Arch Pediatr Adolesc Med 158:312–316
Kalueff AV, Jensen CL, Murphy DL (2007) Locomotory patterns, spatiotemporal organization of exploration and spatial memory in serotonin transporter knockout mice. Brain Res 1169:87–97
Kaufmann WE, Moser HW (2000) Dendritic anomalies in disorders associated with mental retardation. Cereb Cortex 10:981–991
Kesterson KL, Lane RD, Rhoades RW (2002) Effects of elevated serotonin levels on patterns of GAP-43 expression during barrel development in rat somatosensory cortex. Brain Res Dev Brain Res 139:167–174
Khelfaoui M, Denis C, van Galen E, de Bock F, Schmitt A, Houbron C, Morice E, Giros B, Ramakers G, Fagni L, Chelly J, Nosten-Bertrand M, Billuart P (2007) Loss of X-linked mental retardation gene oligophrenin1 in mice impairs spatial memory and leads to ventricular enlargement and dendritic spine immaturity. J Neurosci 27:9439–9450
Knobloch M, Mansuy IM (2008) Dendritic spine loss and synaptic alterations in Alzheimer’s disease. Mol Neurobiol 37:73–82
Laine K, Heikkinen T, Ekblad U, Kero P (2003) Effects of exposure to selective serotonin reuptake inhibitors during pregnancy on serotonergic symptoms in newborns and cord blood monoamine and prolactin concentrations. Arch Gen Psychiatry 60:720–726
Laurent A, Goaillard JM, Cases O, Lebrand C, Gaspar P, Ropert N (2002) Activity-dependent presynaptic effect of serotonin 1B receptors on the somatosensory thalamocortical transmission in neonatal mice. J Neurosci 22:886–900
Lebrand C, Cases O, Adelbrecht C, Doye A, Alvarez C, El Mestikawy S, Seif I, Gaspar P (1996) Transient uptake and storage of serotonin in developing thalamic neurons. Neuron 17:823–835
Lebrand C, Cases O, Wehrlé R, Blakely RD, Edwards RH, Gaspar P (1998) Transient developmental expression of monoamine transporters in the rodent forebrain. J Comp Neurol 401(4):506–524
Lebrand C, Gaspar P, Nicolas D, Hornung JP (2006) Transitory uptake of serotonin in the developing sensory pathways of the common marmoset. J Comp Neurol 499:677–689
Lee LJ, Iwasato T, Itohara S, Erzurumlu RS (2005a) Exuberant thalamocortical axon arborization in cortex-specific NMDAR1 knockout mice. J Comp Neurol 485:280–292
Lee LJ, Lo FS, Erzurumlu RS (2005b) NMDA receptor-dependent regulation of axonal and dendritic branching. J Neurosci 25:2304–2311
Lisboa SF, Oliveira PE, Costa LC, Venâncio EJ, Moreira EG (2007) Behavioral evaluation of male and female mice pups exposed to fluoxetine during pregnancy and lactation. Pharmacology 80:49–56
Lu HC, Butts DA, Kaeser PS, She WC, Janz R, Crair MC (2006) Role of efficient neurotransmitter release in barrel map development. J Neurosci 26:2692–2703
Lübke J, Egger V, Sakmann B, Feldmeyer D (2000) Columnar organization of dendrites and axons of single and synaptically coupled excitatory spiny neurons in layer 4 of the rat barrel cortex. J Neurosci 20:5300–5311
Luo X, Persico AM, Lauder JM (2003) Serotonergic regulation of somatosensory cortical development: lessons from genetic mouse models. Dev Neurosci 25:173–183
Maciag D, Simpson KL, Coppinger D, Lu Y, Wang Y, Lin RC, Paul IA (2006) Neonatal antidepressant exposure has lasting effects on behavior and serotonin circuitry. Neuropsychopharmacology 31:47–57
Mansour-Robaey S, Mechawar N, Radja F, Beaulieu C, Descarries L (1998) Quantified distribution of serotonin transporter and receptors during the postnatal development of the rat barrel field cortex. Brain Res Dev Brain Res 107:159–163
McKinney BC, Grossman AW, Elisseou NM, Greenough WT (2005) Dendritic spine abnormalities in the occipital cortex of C57BL/6 Fmr1 knockout mice. Am J Med Genet B Neuropsychiatr Genet 136B:98–102
Millan MJ (2002) Descending control of pain. Prog Neurobiol 66:355–474
Moses-Kolko EL, Bogen D, Perel J, Bregar A, Uhl K, Levin B, Wisner KL (2005) Neonatal signs after late in utero exposure to serotonin reuptake inhibitors: literature review and implications for clinical applications. JAMA 293:2372–2383
Muñoz A, Liu XB, Jones EG (1999) Development of metabotropic glutamate receptors from trigeminal nuclei to barrel cortex in postnatal mouse. J Comp Neurol 409:549–566
Nelson LS, Erdman AR, Booze LL, Cobaugh DJ, Chyka PA, Woolf AD, Scharman EJ, Wax PM, Manoguerra AS, Christianson G, Caravati EM, Troutman WG (2007) Selective serotonin reuptake inhibitor poisoning: an evidence-based consensus guideline for out-of-hospital management. Clin Toxicol (Phila) 45:315–332
Noorlander CW, Ververs FF, Nikkels PG, van Echteld CJ, Visser GH, Smidt MP (2008) Modulation of serotonin transporter function during fetal development causes dilated heart cardiomyopathy and lifelong behavioral abnormalities. PLoS ONE 3:e2782
Norrholm SD, Ouimet CC (2000) Chronic fluoxetine administration to juvenile rats prevents age-associated dendritic spine proliferation in hippocampus. Brain Res 883:205–215
Oberlander TF, Grunau RE, Fitzgerald C, Papsdorf M, Rurak D, Riggs W (2005) Pain reactivity in 2-month-old infants after prenatal and postnatal serotonin reuptake inhibitor medication exposure. Pediatrics 115:411–425
Persico AM, Mengual E, Moessner R, Hall FS, Revay RS, Sora I, Arellano J, DeFelipe J, Gimenez-Amaya JM, Conciatori M, Marino R, Baldi A, Cabib S, Pascucci T, Uhl GR, Murphy DL, Lesch KP, Keller F (2001) Barrel pattern formation requires serotonin uptake by thalamocortical afferents, and not vesicular monoamine release. J Neurosci 21:6862–6873
Petersen CC (2007) The functional organization of the barrel cortex. Neuron 56:339–355
Purpura DP (1974) Dendritic spine “dysgenesis” and mental retardation. Science 186:1126–1128
Rebsam A, Seif I, Gaspar P (2002) Refinement of thalamocortical arbors and emergence of barrel domains in the primary somatosensory cortex: a study of normal and monoamine oxidase a knock-out mice. J Neurosci 22:8541–8552
Rhoades RW, Bennett-Clarke CA, Shi MY, Mooney RD (1994) Effects of 5-HT on thalamocortical synaptic transmission in the developing rat. J Neurophysiol 72:2438–2450
Romijn HJ, Hofman MA, Gramsbergen A (1991) At what age is the developing cerebral cortex of the rat comparable to that of the full-term newborn human baby? Early Hum Dev 26:61–67
Salichon N, Gaspar P, Upton AL, Picaud S, Hanoun N, Hamon M, De Maeyer E, Murphy DL, Mossner R, Lesch KP, Hen R, Seif I (2001) Excessive activation of serotonin (5-HT) 1B receptors disrupts the formation of sensory maps in monoamine oxidase a and 5-ht transporter knock-out mice. J Neurosci 21:884–896
Sanz EJ, De-las-Cuevas C, Kiuru A, Bate A, Edwards R (2005) Selective serotonin reuptake inhibitors in pregnant women and neonatal withdrawal syndrome: a database analysis. Lancet 365:482–487
Schmidt JT (2004) Activity-driven sharpening of the retinotectal projection: the search for retrograde synaptic signaling pathways. J Neurobiol 59:114–133
Sholl DA (1953) Dendritic organization in the neurons of the visual and motor cortices of the cat. J Anat 87:387–406
Silva-Gómez AB, Rojas D, Juárez I, Flores G (2003) Decreased dendritic spine density on prefrontal cortical and hippocampal pyramidal neurons in postweaning social isolation rats. Brain Res 983:128–136
Sommer C (2004) Serotonin in pain and analgesia: actions in the periphery. Mol Neurobiol 30:117–125
Sorra KE, Harris KM (2000) Overview on the structure, composition, function, development, and plasticity of hippocampal dendritic spines. Hippocampus 10:501–511
Spires TL, Molnár Z, Kind PC, Cordery PM, Upton AL, Blakemore C, Hannan AJ (2005) Activity-dependent regulation of synapse and dendritic spine morphology in developing barrel cortex requires phospholipase C-beta1 signalling. Cereb Cortex 15:385–393
Svensson CI, Tran TK, Fitzsimmons B, Yaksh TL, Hua XY (2006) Descending serotonergic facilitation of spinal ERK activation and pain behavior. FEBS Lett 580:6629–6634
Swann JW, Al-Noori S, Jiang M, Lee CL (2000) Spine loss and other dendritic abnormalities in epilepsy. Hippocampus 10:617–625
Van den Hove DL, Blanco CE, Scheepens A, Desbonnet L, Myint AM, Leonard BE, Prickaerts J, Steinbusch HW (2008) Prenatal maternal paroxetine treatment and neonatal mortality in the rat: a preliminary study. Neonatology 93:52–55
Ververs T, Kaasenbrood H, Visser G, Schobben F, de Jong-van den Berg L, Egberts T (2006) Prevalence and patterns of antidepressant drug use during pregnancy. Eur J Clin Pharmacol 62:863–870
Vitalis T, Cases O, Callebert J, Launay JM, Price DJ, Seif I, Gaspar P (1988) Effects of monoamine oxidase A inhibition on barrel formation in the mouse somatosensory cortex: determination of a sensitive developmental period. J Comp Neurol 393:169–184
Vogel C, Mössner R, Gerlach M, Heinemann T, Murphy DL, Riederer P, Lesch KP, Sommer C (2003) Absence of thermal hyperalgesia in serotonin transporter-deficient mice. J Neurosci 23:708–715
Wang JW, David DJ, Monckton JE, Battaglia F, Hen R (2008) Chronic fluoxetine stimulates maturation and synaptic plasticity of adult-born hippocampal granule cells. J Neurosci 28:1374–1384
Woolsey TA, Van der Loos H (1970) The structural organization of layer IV in the somatosensory region (SI) of mouse cerebral cortex. The description of a cortical field composed of discrete cytoarchitectonic units. Brain Res 17:205–242
Xu Y, Sari Y, Zhou FC (2004) Selective serotonin reuptake inhibitor disrupts organization of thalamocortical somatosensory barrels during development. Brain Res Dev Brain Res 150:151–161
Young-Davies CL, Bennett-Clarke CA, Lane RD, Rhoades RW (2000) Selective facilitation of the serotonin(1B) receptor causes disorganization of thalamic afferents and barrels in somatosensory cortex of rat. J Comp Neurol 425:130–138
Acknowledgments
This work was supported by National Science Council of the Republic of China (Grant No. NSC 96-2628-B-002-053-MY3). The author thanks Drs. R.S. Erzurumlu and F.-C. Zhou for helpful comments on the manuscript and Mr. Y.-C. Wang for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, LJ. Neonatal Fluoxetine Exposure Affects the Neuronal Structure in the Somatosensory Cortex and Somatosensory-Related Behaviors in Adolescent Rats. Neurotox Res 15, 212–223 (2009). https://doi.org/10.1007/s12640-009-9022-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12640-009-9022-4