Abstract
Rationale
Second-generation antipsychotics have some beneficial effect on cognition. Recent studies, furthermore, indicate differential effects of second-generation antipsychotics on impairment in executive cognitive function.
Objective
We evaluated the effect of the second-generation antipsychotic drug, sertindole, on extracellular levels of dopamine (DA), acetylcholine (ACh), and glutamate (Glu) in the rat medial prefrontal cortex (mPFC). Risperidone was studied for comparison. Moreover, selective serotonin 5-HT2A, 5-HT2C, and 5-HT6 receptor antagonists were used, given alone and in combination with the preferential DA D2 receptor antagonist, haloperidol, to further clarify the action of the two drugs.
Materials and methods
Rats were treated acutely with vehicle or drugs, and extracellular levels of neurotransmitters were assessed by microdialysis in freely moving animals.
Results
Sertindole and risperidone significantly increased extracellular levels of DA. Haloperidol; the 5-HT2A receptor antagonist, M100907; the 5-HT2C receptor antagonist, SB242084; and the 5-HT6 receptor antagonist, GSK-742457, induced minor increases in levels of DA, but the three latter compounds raised the DA levels notably in combination with haloperidol. Sertindole and risperidone significantly increased the extracellular levels of ACh but only sertindole raised the extracellular levels of Glu. The selective 5-HT6 receptor antagonist, SB-271046, significantly increased the extracellular levels of Glu.
Conclusion
Sertindole and risperidone markedly increased extracellular levels of DA in mPFC. The built-in 5-HT2A/5-HT2C/D2 receptor antagonism of the two drugs might be involved in this action. Both drugs increased the extracellular levels of ACh but only sertindole enhanced Glu levels. The high affinity of sertindole for the 5-HT6 receptor compared to risperidone may differentiate sertindole from risperidone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several lines of evidence suggest that current antipsychotics have one common denominator regarding their mechanism of action; they interfere with dopaminergic neurotransmission in the brain (Arnt and Skarsfeldt 1998). Moreover, current antipsychotics have the ability to block dopamine (DA) D2 receptors to a varying degree at therapeutically relevant doses (Talbot and Laruelle 2002). While conventional D2 receptor-blocking antipsychotics primarily have clinical effect on positive symptoms of schizophrenia, the second-generation antipsychotics, which have a broader receptor profile, seem to have some beneficial effects on negative symptoms and moderate effects on cognitive deficits as well (Meltzer and McGurk 1999; O'Grada and Dinan 2007; Pratt et al. 2008; Remington and Kapur 2000). The additional 5-HT2A receptor antagonistic property of some second-generation antipsychotics is assumed to be involved in their therapeutic mechanism of action (Wood et al. 2006).
Dopaminergic hypofunction in the prefrontal cortex (PFC) has been suggested to be associated with the etiology of negative symptoms and cognitive dysfunction of schizophrenia (Abi-Dargham and Moore 2003; Stone et al. 2007). The lack of ability of D2 receptor antagonism alone to robustly mediate DA neurotransmission in the PFC (Ago et al. 2005; Kuroki et al. 1999; Li et al. 2005) may be implicated in the lack of effect of conventional antipsychotics on negative symptoms and cognitive dysfunction (Didriksen et al. 2007; Grayson et al. 2007). In contrast, second-generation antipsychotics have been reported to produce increases in DA levels in the medial prefrontal cortex (mPFC; Kuroki et al. 1999). Kuroki et al. (1999) suggested that the ability of some antipsychotics to produce greater increases in extracellular levels of DA in the mPFC compared to the nucleus accumbens may in part be related to weak D2 receptor affinity relative to 5-HT2A receptor antagonism. Moreover, 5-HT1A receptor agonism (Ago et al. 2005; Bortolozzi et al. 2007) and alpha2-adrenoceptor antagonism (Devoto et al. 2004) have been proposed to be capable of releasing prefrontal DA.
Acetylcholine (ACh) activity has been suggested to be of significance for attention and various aspects of cognition (Gray and Roth 2007). Shirazi-Southall et al. (2002) demonstrated that the second-generation antipsychotics, olanzapine and clozapine, markedly increased the levels of ACh in the rat hippocampus, leaving the conventional antipsychotics, haloperidol, thioridazine, and chlorpromazine, with a very modest increase. Furthermore, clozapine, olanzapine, risperidone, and ziprasidone, but not haloperidol, sulpiride, and thioridazine, increased ACh release in the rat mPFC (Ichikawa et al. 2002b). In the latter study, none of the drugs affected the level of ACh in the nucleus accumbens or striatum. The multireceptor profile of the second-generation antipsychotics is probably involved in these ACh effects, but so far it has not been possible to clarify the mechanism of action (Ichikawa et al. 2002a, c; Shirazi-Southall et al. 2002).
As previously mentioned, dopaminergic hypofunction in the PFC is thought to have a major role in the etiology of negative symptoms and cognitive dysfunction of schizophrenia (Abi-Dargham and Moore 2003; Stone et al. 2007). However, in humans, the N-methyl-d-aspartate (NMDA) receptor antagonists, phencyclidine (PCP) and ketamine, induce psychotic symptoms and neurocognitive disturbances with similarities to those observed in schizophrenia (Enomoto et al. 2007; Javitt 2007; Krivoy et al. 2008; Stone et al. 2007; Tan et al. 2007). Thus, it has been hypothesized that insufficient glutamate (Glu) neurotransmission is involved in the pathophysiology of schizophrenia. This hypothesis has led to clinical trials with several positive NMDA modulators with encouraging findings (for review, see Javitt 2007). Although single administration of an NMDA antagonist to rodents seems to reflect some facets of schizophrenia (Enomoto et al. 2007), withdrawal from repeated NMDA antagonist treatment reproduces schizophrenia-like psychosis (positive/negative symptoms and cognitive dysfunctions) and induces neurochemical and neuroanatomical changes (Abdul-Monim et al. 2007; Cochran et al. 2003; Enomoto et al. 2007; Hajszan et al. 2006; Noda et al. 2000). Thus, the latter approach might be a valuable animal model of schizophrenia. Though single injection with the NMDA antagonist, MK-801, has been reported to increase extracellular levels of Glu in the mPFC (Lopez-Gil et al. 2007; Zuo et al. 2006), repeated administration of MK-801 decreased Glu levels in the mPFC (Zuo et al. 2006). Interestingly, 5-HT6 antagonism has been demonstrated to increase Glu release in the rat PFC (Dawson et al. 2001).
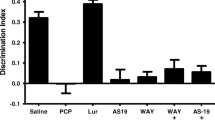
Second-generation antipsychotics may improve cognitive impairments in schizophrenic patients since sertindole, risperidone, and clozapine, but not haloperidol, were observed to reverse cognitive deficits induced by repeated PCP administration measured by the Morris water maze (Didriksen et al. 2007). Recent animal studies indicate differential effects of second-generation antipsychotics on impairment in executive cognitive function, since sertindole induced a significant reversal of impairment in extradimensional set shifting, while risperidone, olanzapine, and clozapine were ineffective (Goetghebeur and Dias 2009; Rodefer et al. 2008). The latter differences may be associated with different receptor profiles. As indicated in Table 1, sertindole and risperidone have a broad receptor profile with shared potent antagonistic effects on the D2 receptor subfamily as well as on the 5-HT2A, 5-HT2C, and the alpha1-adrenergic receptors. Moreover, sertindole has high 5-HT6 receptor affinity, while that of risperidone is negligible (Arnt and Skarsfeldt 1998; Leysen 2000).
In the present work, we studied the effects of sertindole on extracellular levels of neurotransmitters in the brain. Furthermore, the effects of risperidone and haloperidol as well as selective antagonists of the 5-HT2A, 5-HT2C, or 5-HT6 receptor on extracellular levels of neurotransmitters in the rat mPFC were studied. The drug doses chosen in these experiments were based on a study demonstrating antipsychotic-like action in the conditioned avoidance response model where drug effects were related to plasma levels of drugs and D2 receptor occupancy (Olsen et al. 2008).
Materials and methods
Animals
Male Sprague–Dawley rats (Charles River), initially weighing 250 g, were used. The animals were housed two per cage in Makrolon cages (20 × 35 cm) with one plastic house for enrichment. The animals were kept in an animal room at room temperature under a 12-h light/dark cycle (lights on at 0600 hours). Food and water were available ad libitum. The rats had a minimum of 5 days adaptation in the animal facility prior to the initiation of experiments and the animals were brought to the experimental room the day before the experiment. Ethical permission for the procedures used in this study was granted by the Animal Welfare Committee, appointed by the Danish Ministry of Justice and all animal procedures were carried out in compliance with EC Directive 86/609/EEC and with Danish law regulating experiments on animals.
Compound administration
Sertindole (free base; H. Lundbeck A/S) was dissolved in isotonic water to which was added a small amount of acetic acid and administered per os (p.o.) in a volume of 5 mL/kg. Risperidone (free base; Jansen) and haloperidol (free base; Sigma) were dissolved in saline to which was added a small amount of HCl and tartaric acid, respectively. M100907 (R(+)-α-(2,3-dimethoxyphenyl)-1-[2-(4-fluorophenylethyl)-4-piperdine-methanol]; free base; Axon Biochemicals BV) was dissolved in 0.1 M methanesulfonic acid. SB242084 (6-chloro-5-methyl-1-[6-(2-methylpiridin-3-yloxy)pyridin-3-yl carbamoyl] indoline; dihydrochloride; Sigma), GSK742457 (3-benzenesulfonyl-8-piperazin-1-yl-quinoline; free base, Custom Synthesis, Sundia Meditech), and SB-271046 (5-chloro-N-(4-methoxy-3-piperazin-1-yl-phenyl)-3-methyl-2-benzothio-phenesulfonamide; hydrochloride; Axon Biochemicals BV) were dissolved in 10% 2-hydroxypropyl-beta-cyclodextrin. Risperidone, haloperidol, M100907, SB242084, and GSK742457 were administered subcutaneously (s.c.) in volumes of 2.5 mL/kg. SB-271046 was administered s.c. in a volume of 5 mL/kg.
Microdialysis
Male Sprague–Dawley rats were anesthetized and intracerebral guide cannulas (CMA/12) were stereotaxically implanted into the brain positioning the dialysis probe tip in the mPFC (coordinates = 3.2 mm, anterior to bregma; 0.8 mm, lateral; 4.0 mm ventral to dura) or the nucleus accumbens (coordinates = 1.7 mm, anterior to bregma; 0.7 mm, lateral; 8.0 mm ventral to dura; Paxinos and Watson 1998). The microdialysis probe (CMA/12, 0.5 mm diameter, 2 or 3 mm length) was inserted through the guide cannula and perfused with filtered Ringer's solution (145 mm NaCl, 3 mM KCl, 1 mM MgCl2, and 1.2 mM CaCl2 [+0.5 μM neostigmine for ACh measurements]) at a constant flow rate of 1 μL/min.
Analysis of dialysate DA
The content of DA in the dialysates was analyzed by means of high-performance liquid chromatography (HPLC) with electrochemical detection. The monoamines were separated by reverse-phase liquid chromatography (ODS 150 × 2 mm column). The mobile phase consisted of 150 mM NaH2PO4, 4.8 mM citric acid monohydrate, 3 mM dodecyl sulfate, 50 μM ethylenediaminetetracetic acid, 11.3% methanol, and 16.7 % acetonitrile (pH 5.6); flow rate of 0.2 mL/min. Electrochemical detection was accomplished using a coulometric detector; potential was set at E2 = 200 mV (Coulochem II, ESA). The lowest level of quantification was 0.5 fmol/20 μL.
Analysis of dialysate Glu
The content of Glu in the dialysates was determined by means of HPLC with fluorescence detection after precolumn online derivatization with o-phthalaldehyde (OPA) using a fully automated HPLC fluorescence system (Agilent 1100). The reaction buffer was a 0.4 M boric acid buffer adjusted to pH 9.0 with NaOH. Using the autoinjector of the HPLC system, 5 μL reaction buffer, 1 μL OPA derivatization solution (OPA; 10 mg/mL), and 1 μL microdialysis sample was mixed and allowed to react for 2 min and thereafter injected onto the HPLC system. Glu was separated on a Hypersil AA-ODS column (5 μm, 2.1 × 200 mm, Agilent) with oven temperature of 40°C. Flow rate was 0.45 mL/min. Mobile phase A consisted of 20 mM sodium acetate, 0.018% triethylamine, and 3% tetrahydrofuran (pH 7.2). Mobile phase B consisted of 20 mM sodium acetate, 40% acetonitrile, and 40% methanol. A linear gradient was applied from 0 min (A/B = 100:0 v/v) to 7 min (A/B = 40:60 v/v) after which (from 8 min) elution was carried out with mobile phase B alone. A 5 min re-equilibration period was allowed between samples. The Agilent 1100 fluorescence detector was set to excitation at 340 nm and emission at 450 nm. The lowest level of quantification was 100 fmol/µL.
Analysis of dialysate ACh
The content of ACh in the dialysates was analyzed by means of HPLC with electrochemical detection using a mobile phase consisting of 100 mM Na2HPO4, 2.0 mM octane sulfonic acid, 0.5 mM tetramethyl ammonium chloride, and 0.005% MB (ESA), pH 8.0. A precolumn enzyme reactor (ESA) containing immobilized choline oxidase eliminated choline from the injected sample (10 μL) prior to separation of ACh on the analytical column (ESA ACH-250); flow rate 0.35 mL/min, temperature 35°C. After the analytical column, the sample passed through a postcolumn solid-phase reactor (ESA) containing immobilized acetylcholine esterase and choline oxidase. The latter reactor converted ACh to choline and subsequently choline to betaine and H2O2. The latter was detected electrochemically by using a platinum electrode; potential was set at E1 = 300 mV (Coulochem III, ESA, model 5040). The lowest level of quantification was 25 fmol/10 μL.
Data presentation
The mean value of three consecutive dialysis samples immediately preceding compound administration served as the basal level for each experiment and data were converted to percentage of basal (mean basal preinjection values normalized to 100%). All data are presented as mean values ± SEM. Data were analyzed by two-way analysis of variance followed by the Bonferroni post hoc test for between-groups multiple comparisons. Data were evaluated by SigmaStat version 3.0.1.
Results
Basal levels of neurotransmitters in the dialysates from rat mPFC
Basal levels of DA, Glu, and ACh in the dialysates obtained from rats used in the study were 2.4 ± 0.2 fmol/20 μL (n = 35, rats used for sertindole and risperidone experiments), 22.0 ± 3.0 pmol/20 μL (n = 32), and 302.6 ± 30.0 fmol/10 μL (n = 24), respectively.
Effects of sertindole and risperidone on the level of DA in dialysates from rat mPFC
Administration of sertindole (2.5 and 10 mg/kg p.o.; F 2,286 = 42.60, p < 0.001) and risperidone (1 mg/kg s.c.; F 1,100 = 133.24, p < 0.001) significantly increased extracellular levels of DA in the mPFC compared to vehicle-treated animals (Fig. 1a, b). Moreover, sertindole (2.5 and 10 mg/kg p.o.) and risperidone (1 mg/kg s.c.) induced equivalent and significant increases in the extracellular levels of DA in the nucleus accumbens (by 200% and 190%, respectively) compared with their respective effects in the mPFC (data not shown).
Time-dependent effects of sertindole and risperidone on the level of DA in dialysates from rat mPFC. The drugs were administered at t = 0 (arrow). Data are presented as the means ± SEM. a Sertindole and b risperidone induced significant increases in extracellular DA. *p < 0.05 versus vehicle treatment
Effects of haloperidol, M100907, SB242084, GSK-742457, and the combination of haloperidol plus M100907, SB242084, or GSK-742457 on the level of DA in dialysates from rat mPFC
The administration of haloperidol alone (0.5 mg/kg s.c.) enhanced the DA levels to a minor degree in the mPFC (122 % at t = 60 min, normalizing the preinjection levels to 100%) compared to vehicle-treated animals (F 1,48 = 7.45, p = 0.009). M100907 (0.5 mg/kg s.c.; F 1,40 = 7.4, p = 0.01) induced a minor but significant overall increase in the DA levels. SB242084 (0.5 mg/kg s.c.; F 1,62 = 3.9, p = 0.052) also tended to increase the DA levels when administered alone (Fig. 2a). GSK-742457 (1.25 mg/kg s.c.; F 1,84 = 8.06, p = 0.006) induced a slight but significant overall increase in the DA levels (Fig. 2b). However, the combinations of haloperidol plus M100907 (F 1,63 = 31.58, p < 0.001), SB242084 (F 1,55 = 40.36, p < 0.001), or GSK742457 (F 1,111 = 26.50, p > 0.001) induced robust increases in the extracellular levels of DA compared to that in vehicle-treated animals (Fig. 2a, b).
a Effects of haloperidol (0.5 mg/kg s.c.), M100907 (0.5 mg/kg s.c.), SB242084 (0.5 mg/kg s.c.), and the combinations of haloperidol plus M100907 and haloperidol plus SB242084 on the level of DA in dialysates from rat mPFC. b Effects of haloperidol (0.5 mg/kg s.c.), GSK742457 (1.25 mg/kg s.c.), and the combination of haloperidol and GSK742457 on the level of DA in dialysates from rat mPFC. The compounds were administered at t = 0 (arrow). Data are presented as the means ± SEM. *p < 0.05 versus vehicle treatment
Effects of sertindole and risperidone on the level of ACh in dialysates from rat mPFC
Both sertindole (10 mg/kg p.o.; F 1,213 = 20.94, p < 0.001) and risperidone (1 mg/kg s.c.; F 1,131 = 22.21, p < 0.001) significantly increased the extracellular levels of ACh in the mPFC compared to vehicle-treated animals (Fig. 3a, b).
Time-dependent effects of sertindole and risperidone on the level of ACh in dialysates from rat mPFC. The drugs were administered at t = 0 (arrow). Data are presented as the means ± SEM. a Sertindole and b risperidone significantly increased extracellular levels of ACh in the mPFC. *p < 0.05 versus vehicle treatment
Effects of sertindole and risperidone on the level of Glu in dialysates from rat mPFC
Sertindole (10 mg/kg p.o.; F 1,99 = 15.89, p < 0.001), but not risperidone (1 mg/kg s.c.), significantly increased the extracellular level of Glu in the mPFC compared to vehicle-treated animals (Fig. 4a, b).
Time-dependent effects of sertindole and risperidone on the level of Glu in dialysates from rat mPFC. The drugs were administered at t = 0 (arrow). Data are presented as the means ± SEM. a Sertindole significantly increased extracellular levels of Glu in the mPFC. b Risperidone did not affect the levels of extracellular Glu. *p < 0.05 versus vehicle treatment
Effect of SB-271046 on the level of Glu in dialysates from rat mPFC
SB-271046 (10 mg/kg s.c.; F 1,84 = 16.44, p < 0.001) significantly increased the extracellular level of Glu in the mPFC compared to vehicle-treated animals (Fig. 5).
Discussion
In the present study, the selected doses of sertindole and risperidone have been shown to induce D2 receptor occupancies that correspond to therapeutically effective levels (Olsen et al. 2008) and induce behavioral effects in a number of animal models of psychosis (Arnt and Skarsfeldt 1998). Moreover, the risperidone dose has been used frequently to study the effect on neurotransmitter systems (Kuroki et al. 1999; Shirazi-Southall et al. 2002).
As previously mentioned, both sertindole and risperidone have a broad receptor profile with shared potent effects on the D2 receptor subfamily as well as on the 5-HT2A, 5-HT2C, and alpha1-adrenergic receptors (Arnt and Skarsfeldt 1998). Furthermore, sertindole has high 5-HT6 receptor affinity, while that of risperidone is negligible (Leysen 2000; Table 1).
In this study, we demonstrated that acute treatment with sertindole increases the extracellular levels of DA in the mPFC and nucleus accumbens. This was also observed for risperidone. Accordingly, other second-generation antipsychotics have been reported to increase DA levels in the mPFC (Bortolozzi et al. 2007; Ichikawa et al. 2002a; Kuroki et al. 1999). The increase in extracellular levels of DA in the nucleus accumbens induced by sertindole and risperidone may primarily be due to blockade of presynaptic D2 receptors (Westerink and De Vries 1989), since D2/3 receptor affinities of antipsychotics correlate to their preferential effects on DA levels in the nucleus accumbens (Kuroki et al. 1999). The increase in mPFC DA levels induced by second-generation antipsychotics appears to involve additional receptors giving the fact that most prefrontal dopaminergic neurons do not possess D2 autoreceptors (Lammel et al. 2008). In the present study, haloperidol induced a small increase in the DA levels in the mPFC in agreement with other observations (Li et al. 2005; Liegeois et al. 2002).
Serotonergic pathways seem to be of significance for the regulation of extracellular DA in the mPFC (Gobert et al. 2000; Li et al. 2005). In the rat, prefrontal 5-HT2A receptors are located on pyramidal neurons and, to a lower degree, on GABAergic interneurons (Cornea-Hebert et al. 1999; Jakab and Goldman-Rakic 2000). Local activation of 5-HT2A receptors in the mPFC influences DA neuron activity in the ventral tegmental area (VTA) and DA release in the mesocortical pathway (Bortolozzi et al. 2005). The 5-HT2A antagonist, M100907, has been reported to increase (Schmidt and Fadayel 1995) or exert no effect on DA levels in the mPFC (Liegeois et al. 2002). It has been suggested that the increase in DA levels in the mPFC, relative to those in the nucleus accumbens, following the administration of second-generation antipsychotics, which produce relatively weaker D2 receptor blockade and more potent 5-HT2A receptor blockade, largely depend on combined D2/5-HT2A receptor blockade (Kuroki et al. 1999; Li et al. 2005; Liegeois et al. 2002). At higher doses, which produce greater D2 receptor occupancy, other mechanisms may be involved, e.g., alpha2-adrenoceptor (Devoto et al. 2004) or 5-HT2C receptor antagonism (Gobert et al. 2000; Pozzi et al. 2002). It has been suggested that the combination of D2 and 5-HT2A receptor blockade increases DA release via the 5-HT1A receptor since some (Ichikawa et al. 2001) but not all (Assie et al. 2005) studies have shown that the 5-HT1A antagonist, WAY100635, antagonizes DA release induced by the D2 and 5-HT2A receptor combination. In the present study, M100907 alone induced a minor but significant increase in extracellular DA levels, but in combination with haloperidol, M100907 robustly enhanced the DA levels in the mPFC, indicating that the D2/5-HT2A antagonism of sertindole and risperidone may critically control the DA release in the mPFC. However, at present, the mechanism of action of the combined D2 and 5-HT2A antagonism on extracellular levels of DA in the mPFC is unclear.
As previously mentioned, sertindole and risperidone have 5-HT2C receptor antagonistic properties (Arnt and Skarsfeldt 1998). A recent study on 5-HT2C receptor immunoreactivity revealed that 5-HT2C receptors are located on GABAergic interneurons in the VTA and on DA neurons in the middle VTA (Bubar and Cunningham 2007). Systemic administration of the selective 5-HT2C receptor agonist, WAY-163909, decreased the number of spontaneously active DA neurons in the VTA (Marquis et al. 2007). Administration of the selective 5-HT2C receptor agonist, Ro-60-0175, locally into the VTA antagonized stress-induced increases in DA levels in the mPFC without affecting basal DA levels (Pozzi et al. 2002). Thus, 5-HT2C receptors may regulate DA efflux in the mesocortical system by activating tonic GABA inhibition or influencing 5-HT2C receptors on DA neurons in the VTA. In the present study, a lower dose of SB242084 (0.5 mg/kg s.c.) tended to increase the DA levels in the mPFC, but the increase did not reach statistical significance (p = 0.052). However, in combination with haloperidol, SB242084 enhanced the DA levels distinctly in the mPFC compared to the vehicle-treated animals, suggesting that the D2/5-HT2C antagonism of sertindole and risperidone may also contribute to the DA release in the mPFC.
In the present study, the administration of the potent 5-HT6 antagonist, GSK-742457 (Upton et al. 2008), induced a slight but significant increase in the mPFC DA levels when injected alone. When combined with haloperidol, the increase in DA levels was distinct compared to vehicle-treated animals. The dose of GSK-742457 in the present study has been shown to yield approximately 90% occupancy at the 5-HT6 receptor in vivo (unpublished in-house data), consistent with data reported by Upton et al. (2008). In a recent study, the 5-HT6 antagonist, SB-271046 at 10 mg/kg p.o., produced augmented levels of DA and noradrenaline without altering the serotonin levels in the mPFC (Lacroix et al. 2004). Another study using the 5-HT6 receptor antagonist, SB-399885, reported that this antagonist did not affect basal levels of DA in the rat mPFC significantly and had no effect on haloperidol (0.1 mg/kg s.c.)-induced DA efflux but potentiated risperidone (1.0 m/kg s.c.)-induced DA efflux (Li et al. 2007). This indicates that 5-HT6 antagonism may affect cortical DA levels positively when administered alone or in combination with current antipsychotics. However, since sertindole and risperidone have similar effects on the DA levels, the 5-HT6 antagonistic effect of sertindole may not be of significant importance for the effect on the DA levels.
Sertindole may enhance DA levels in the mPFC by affecting the above-mentioned receptor types. Restoration of prefrontal DA levels would be expected to increase transmission through the D1 receptor, which may alleviate cognitive impairments and negative symptoms (Abi-Dargham and Moore 2003).
In the present study, sertindole, like risperidone, was found to increase the extracellular levels of ACh in the mPFC. As previously described, second-generation antipsychotics markedly increased the levels of ACh in the rat hippocampus, leaving conventional antipsychotics with a very modest increase (Shirazi-Southall et al. 2002). Moreover, olanzapine, but not haloperidol, increased ACh release in the rat mPFC (Ichikawa et al. 2002b). In the latter study, none of the drugs affected the level of ACh in the nucleus accumbens or striatum. So far, it has not been possible to clarify the mechanism by which second-generation antipsychotics affect ACh levels. The combination of M100907 and haloperidol, which enhances DA release in the mPFC, did not affect the ACh release (Ichikawa et al. 2002a). Shirazi-Southall et al. (2002) reported that 5-HT2A, 5-HT2C, D2, or 5-HT6 receptor antagonism alone increased ACh levels approximately 50% in the rat hippocampus without attaining statistical significance, while olanzapine and clozapine, both possessing high affinities for muscarinic receptors, induced robust ACh increases. The selective 5-HT6 receptor antagonists, 4-(2-bromo-6-pyrrolidin-1-ylpyridine-4-sulfonyl)phenyl-amine (Riemer et al. 2003) and SB-399885 (Hirst et al. 2006), increased rat cortical ACh levels significantly. However, since sertindole and risperidone have similar effects on the ACh levels, the 5-HT6 antagonistic effect of sertindole may not be of significant importance for the effect on the ACh levels. A recent study showed that local infusion of the D2 receptor agonist, quinelorane, into the nucleus accumbens simultaneous with the infusion of NMDA blocked the nucleus accumbens NMDA receptor-mediated increases in ACh in the rat mPFC (Brooks et al. 2007), indicating a complex regulation of the ACh efflux in the mPFC. It is, however, likely that the broad receptor profile of the second-generation antipsychotics is involved in the facilitating effect on the ACh neurotransmission in the mPFC.
It should be noted that, in the present work, the drug effects on ACh levels were measured in the presence of neostigmine in the perfusion solution to detect potential effects of the drugs reliably. However, increased basal levels of ACh due to ACh esterase inhibition are assumed to activate muscarinic autoreceptors (Moor et al. 1998). Thus, this condition may complicate the interpretation of results from experiments with drugs, which have additional muscarinic receptor antagonism, e.g., clozapine produced greater increases in the ACh levels in mPFC in the presence of neostigmine (Ichikawa et al. 2002b). However, since sertindole and risperidone do not block muscarinic receptors (Table 1), this is not considered an issue in the present study.
In the present study, sertindole and SB-271046 increased the extracellular levels of Glu in the mPFC. Enhanced extracellular levels of Glu in the rat frontal cortex induced by SB-271046 have been observed previously (Dawson et al. 2000, 2001). Thus, the potent affinity of sertindole for the 5-HT6 receptor may be involved in the effect on the Glu levels. It is notable that the onset of increases in Glu levels induced by sertindole and SB-271046 seems to be rather slow. This might indicate that the effect of the compounds on Glu levels is mediated through indirect mechanisms. However, plasma levels of SB-271046 peaks 3–4 h after administration (Routledge et al. 2000). This may also explain the slow onset of increase in Glu levels as regards SB-271046.
It is well-established that acute PCP treatment increases release of brain Glu levels in the brain (Enomoto et al. 2007; Jentsch and Roth 1999). Adams and Moghaddam (2001) concluded that the acute PCP Glu activation model lacks predictive validity for current antipsychotics, since haloperidol, clozapine, and M100907 were ineffective in inhibiting the dopaminergic and motoric effects of acute PCP (Adams and Moghaddam 2001). By comparing acute and repeated PCP treatments, it has been concluded that care should be taken when arguing for a complete isomorphism between acute NMDA antagonist-induced behavioral deficits in animals and symptoms of schizophrenia (Enomoto et al. 2007; Jentsch and Roth 1999). In contrast, repeated PCP treatment has been suggested to be a valid animal model of schizophrenia (for reviews, see Jentsch and Roth 1999; Enomoto et al. 2007). Subchronic treatment with PCP induced increased depolarization of pyramidal neurons in the PFC after the application of exogenous NMDA (Arvanov and Wang 1999). This may indicate an upregulation of NMDA receptors due to reduced glutamatergic transmission. In the same study, it was demonstrated that clozapine administration prevented the functional hypersensitivity. Accordingly, acute administration of the NMDA antagonist, MK-801, increased the extracellular levels of Glu in the mPFC (Lopez-Gil et al. 2007; Zuo et al. 2006), while repeated administration of MK-801 decreased Glu levels in the mPFC (Zuo et al. 2006). Moreover, basal DA levels seem to be reduced in the rat PFC after subchronic PCP (Jentsch and Roth 1999). Since released Glu facilitate cholinergic transmission in the PFC (Parikh et al. 2008), a normalization of glutamatergic hypofunction may positively affect DA and ACh functions in the PFC. The selective 5-HT6 antagonist, SB-399885, was shown to fully reverse the deficit in spatial learning in aged rats and scopolamine-induced deficit in the novel recognition paradigm (Hirst et al. 2006).
The increase in extracellular Glu levels in the PFC, which may be regulated by 5-HT6 receptor antagonism, differentiates sertindole from risperidone. As previously described, sertindole induced a significant reversal of impairment in extradimensional set shifting, while risperidone was ineffective (Goetghebeur and Dias 2009; Rodefer et al. 2008).
Basal level of Glu of synaptic origin may be difficult to measure due to the fact that Glu apparently barely escapes the synaptic cleft during basal conditions. Astroglial cells have been suggested to be an important source of basal Glu levels (Schousboe and Waagepetersen 2006) and more than 60% of the basal extracellular level of Glu has been suggested to be of nonsynaptic origin (Bogen et al. 2008; Fonnum 1984). Microdialysis experiments using potassium depolarization and extracellular calcium removal have indicated small releasable pools of synaptic Glu in the brain (Frantz et al. 2002; Herrera-Marschitz et al. 1996). However, a variety of studies have detected synaptic Glu release by microdialysis by means of chemical, electrical, and behavioral stimulation (for review, see van der Zeyden et al. 2008). Despite the fact that the source of the reported Glu changes after acute and chronic NMDA antagonist and 5-HT6 antagonist treatments is unclear at present, it is likely that the increased Glu levels facilitate the function of the NMDA receptor.
One consideration for any drug that acts to modulate Glu would be the potential for excitotoxicity. However, various strategies aimed at different neurotransmitter systems actually alter the activity of glutamatergic neurons. For example, ACh esterase inhibitors increase the release of Glu (Dijk et al. 1995b), while 5-HT1A antagonism potentiates the effects of both muscarinic agonists and NMDA on Glu release (Dijk et al. 1995a). Thus, it is possible that cognitive benefits of drugs directed at these targets involve actions on glutamatergic neurons. More direct approaches include ampakines, which are positive modulators of the action of Glu at AMPA receptors (Arai and Kessler 2007), and as previously mentioned, strategies for increasing the NMDA receptor function (Javitt 2007). In the context of reduced Glu function in schizophrenia and the fact that the above compounds have actions, which modulate the efficacy of Glu released in normal synaptic transmission, an excitotoxicity potential would appear to be less of a concern. In comparison, cerebral ischemia has been reported to induce fivefold to eightfold increase in extracellular Glu levels in the rat brain (Benveniste 2009; Dohmen et al. 2005).
In the present study, we demonstrate that the second-generation antipsychotic drug, sertindole, enhances extracellular levels of DA, ACh, and Glu in the rat mPFC. Thus, restoration of insufficient dopaminergic and glutamatergic transmission and strengthening of the cholinergic transmission in the PFC may be involved in the beneficial effects of sertindole on cognitive function and the superior effect against negative symptoms compared to risperidone reported in a clinical study on sertindole and risperidone (Azorin et al. 2006).
References
Abdul-Monim Z, Neill JC, Reynolds GP (2007) Sub-chronic psychotomimetic phencyclidine induces deficits in reversal learning and alterations in parvalbumin-immunoreactive expression in the rat. J Psychopharmacol 21:198–205
Abi-Dargham A, Moore H (2003) Prefrontal DA transmission at D1 receptors and the pathology of schizophrenia. Neuroscientist 9:404–416
Adams BW, Moghaddam B (2001) Effect of clozapine, haloperidol, or M100907 on phencyclidine-activated glutamate efflux in the prefrontal cortex. Biol Psychiatry 50:750–757
Ago Y, Nakamura S, Baba A, Matsuda T (2005) Sulpiride in combination with fluvoxamine increases in vivo dopamine release selectively in rat prefrontal cortex. Neuropsychopharmacology 30:43–51
Arai AC, Kessler M (2007) Pharmacology of ampakine modulators: from AMPA receptors to synapses and behavior. Curr Drug Targets 8:583–602
Arnt J, Skarsfeldt T (1998) Do novel antipsychotics have similar pharmacological characteristics? A review of the evidence. Neuropsychopharmacology 18:63–101
Arvanov VL, Wang RY (1999) Clozapine, but not haloperidol, prevents the functional hyperactivity of N-methyl-d-aspartate receptors in rat cortical neurons induced by subchronic administration of phencyclidine. J Pharmacol Exp Ther 289:1000–1006
Assie MB, Ravailhe V, Faucillon V, Newman-Tancredi A (2005) Contrasting contribution of 5-hydroxytryptamine 1A receptor activation to neurochemical profile of novel antipsychotics: frontocortical dopamine and hippocampal serotonin release in rat brain. J Pharmacol Exp Ther 315:265–272
Azorin JM, Strub N, Loft H (2006) A double-blind, controlled study of sertindole versus risperidone in the treatment of moderate-to-severe schizophrenia. Int Clin Psychopharmacol 21:49–56
Benveniste H (2009) Glutamate, microdialysis, and cerebral ischemia: lost in translation? Anesthesiology 110:422–425
Bogen IL, Risa O, Haug KH, Sonnewald U, Fonnum F, Walaas SI (2008) Distinct changes in neuronal and astrocytic amino acid neurotransmitter metabolism in mice with reduced numbers of synaptic vesicles. J Neurochem (in press)
Bortolozzi A, az-Mataix L, Scorza MC, Celada P, Artigas F (2005) The activation of 5-HT receptors in prefrontal cortex enhances dopaminergic activity. J Neurochem 95:1597–1607
Bortolozzi A, Az-Mataix L, Toth M, Celada P, Artigas F (2007) In vivo actions of aripiprazole on serotonergic and dopaminergic systems in rodent brain. Psychopharmacology (Berl) 191:745–758
Brooks JM, Sarter M, Bruno JP (2007) D2-like receptors in nucleus accumbens negatively modulate acetylcholine release in prefrontal cortex. Neuropharmacology 53:455–463
Bubar MJ, Cunningham KA (2007) Distribution of serotonin 5-HT2C receptors in the ventral tegmental area. Neuroscience 146:286–297
Cochran SM, Kennedy M, McKerchar CE, Steward LJ, Pratt JA, Morris BJ (2003) Induction of metabolic hypofunction and neurochemical deficits after chronic intermittent exposure to phencyclidine: differential modulation by antipsychotic drugs. Neuropsychopharmacology 28:265–275
Cornea-Hebert V, Riad M, Wu C, Singh SK, Descarries L (1999) Cellular and subcellular distribution of the serotonin 5-HT2A receptor in the central nervous system of adult rat. J Comp Neurol 409:187–209
Dawson LA, Nguyen HQ, Li P (2000) In vivo effects of the 5-HT(6) antagonist SB-271046 on striatal and frontal cortex extracellular concentrations of noradrenaline, dopamine, 5-HT, glutamate and aspartate. Br J Pharmacol 130:23–26
Dawson LA, Nguyen HQ, Li P (2001) The 5-HT(6) receptor antagonist SB-271046 selectively enhances excitatory neurotransmission in the rat frontal cortex and hippocampus. Neuropsychopharmacology 25:662–668
Devoto P, Flore G, Pira L, Longu G, Gessa GL (2004) Alpha2-adrenoceptor mediated co-release of dopamine and noradrenaline from noradrenergic neurons in the cerebral cortex. J Neurochem 88:1003–1009
Didriksen M, Skarsfeldt T, Arnt J (2007) Reversal of PCP-induced learning and memory deficits in the Morris' water maze by sertindole and other antipsychotics. Psychopharmacology (Berl) 193:225–233
Dijk SN, Francis PT, Stratmann GC, Bowen DM (1995a) NMDA-induced glutamate and aspartate release from rat cortical pyramidal neurones: evidence for modulation by a 5-HT1A antagonist. Br J Pharmacol 115:1169–1174
Dijk SN, Francis PT, Stratmann GC, Bowen DM (1995b) Cholinomimetics increase glutamate outflow via an action on the corticostriatal pathway: implications for Alzheimer's disease. J Neurochem 65:2165–2169
Dohmen C, Kumura E, Rosner G, Heiss WD, Graf R (2005) Extracellular correlates of glutamate toxicity in short-term cerebral ischemia and reperfusion: a direct in vivo comparison between white and gray matter. Brain Res 1037:43–51
Enomoto T, Noda Y, Nabeshima T (2007) Phencyclidine and genetic animal models of schizophrenia developed in relation to the glutamate hypothesis. Methods Find Exp Clin Pharmacol 29:291–301
Fonnum F (1984) Glutamate: a neurotransmitter in mammalian brain. J Neurochem 42:1–11
Frantz K, Harte M, Ungerstedt U, O'Connor WT (2002) A dual probe characterization of dialysate amino acid levels in the medial prefrontal cortex and ventral tegmental area of the awake freely moving rat. J Neurosci Methods 119:109–119
Gobert A, Rivet JM, Lejeune F, Newman-Tancredi A, dhumeau-Auclair A, Nicolas JP, Cistarelli L, Melon C, Millan MJ (2000) Serotonin(2C) receptors tonically suppress the activity of mesocortical dopaminergic and adrenergic, but not serotonergic, pathways: a combined dialysis and electrophysiological analysis in the rat. Synapse 36:205–221
Goetghebeur P, Dias R (2009) Comparison of haloperidol, risperidone, sertindole, and modafinil to reverse an attentional set-shifting impairment following subchronic PCP administration in the rat-a back translational study. Psychopharmacology (Berl) 202:287–293
Gray JA, Roth BL (2007) Molecular targets for treating cognitive dysfunction in schizophrenia. Schizophr Bull 33:1100–1119
Grayson B, Idris NF, Neill JC (2007) Atypical antipsychotics attenuate a sub-chronic PCP-induced cognitive deficit in the novel object recognition task in the rat. Behav Brain Res 184:31–38
Hajszan T, Leranth C, Roth RH (2006) Subchronic phencyclidine treatment decreases the number of dendritic spine synapses in the rat prefrontal cortex. Biol Psychiatry 60:639–644
Herrera-Marschitz M, You ZB, Goiny M, Meana JJ, Silveira R, Godukhin OV, Chen Y, Espinoza S, Pettersson E, Loidl CF, Lubec G, Andersson K, Nylander I, Terenius L, Ungerstedt U (1996) On the origin of extracellular glutamate levels monitored in the basal ganglia of the rat by in vivo microdialysis. J Neurochem 66:1726–1735
Hirst WD, Stean TO, Rogers DC, Sunter D, Pugh P, Moss SF, Bromidge SM, Riley G, Smith DR, Bartlett S, Heidbreder CA, Atkins AR, Lacroix LP, Dawson LA, Foley AG, Regan CM, Upton N (2006) SB-399885 is a potent, selective 5-HT6 receptor antagonist with cognitive enhancing properties in aged rat water maze and novel object recognition models. Eur J Pharmacol 553:109–119
Ichikawa J, Ishii H, Bonaccorso S, Fowler WL, O'Laughlin IA, Meltzer HY (2001) 5-HT(2A) and D(2) receptor blockade increases cortical DA release via 5-HT(1A) receptor activation: a possible mechanism of atypical antipsychotic-induced cortical dopamine release. J Neurochem 76:1521–1531
Ichikawa J, Dai J, Meltzer HY (2002a) 5-HT(1A) and 5-HT(2A) receptors minimally contribute to clozapine-induced acetylcholine release in rat medial prefrontal cortex. Brain Res 939:34–42
Ichikawa J, Dai J, O'Laughlin IA, Fowler WL, Meltzer HY (2002b) Atypical, but not typical, antipsychotic drugs increase cortical acetylcholine release without an effect in the nucleus accumbens or striatum. Neuropsychopharmacology 26:325–339
Ichikawa J, Li Z, Dai J, Meltzer HY (2002c) Atypical antipsychotic drugs, quetiapine, iloperidone, and melperone, preferentially increase dopamine and acetylcholine release in rat medial prefrontal cortex: role of 5-HT1A receptor agonism. Brain Res 956:349–357
Jakab RL, Goldman-Rakic PS (2000) Segregation of serotonin 5-HT2A and 5-HT3 receptors in inhibitory circuits of the primate cerebral cortex. J Comp Neurol 417:337–348
Javitt DC (2007) Glutamate and schizophrenia: phencyclidine, N-methyl-d-aspartate receptors, and dopamine–glutamate interactions. Int Rev Neurobiol 78:69–108
Jentsch JD, Roth RH (1999) The neuropsychopharmacology of phencyclidine: from NMDA receptor hypofunction to the dopamine hypothesis of schizophrenia. Neuropsychopharmacology 20:201–225
Krivoy A, Fischel T, Weizman A (2008) The possible involvement of metabotropic glutamate receptors in schizophrenia. Eur Neuropsychopharmacol 18:395–405
Kuroki T, Meltzer HY, Ichikawa J (1999) Effects of antipsychotic drugs on extracellular dopamine levels in rat medial prefrontal cortex and nucleus accumbens. J Pharmacol Exp Ther 288:774–781
Lacroix LP, Dawson LA, Hagan JJ, Heidbreder CA (2004) 5-HT6 receptor antagonist SB-271046 enhances extracellular levels of monoamines in the rat medial prefrontal cortex. Synapse 51:158–164
Lammel S, Hetzel A, Hackel O, Jones I, Liss B, Roeper J (2008) Unique properties of mesoprefrontal neurons within a dual mesocorticolimbic dopamine system. Neuron 57:760–773
Leysen J (2000) Receptor profile of antipsychotics. In: Ellenbroek BA, Cools AR (eds) Atypical antipsychotics. Birkhäuser, Basel, Switzerland, pp 57–81
Li Z, Ichikawa J, Huang M, Prus AJ, Dai J, Meltzer HY (2005) ACP-103, a 5-HT2A/2C inverse agonist, potentiates haloperidol-induced dopamine release in rat medial prefrontal cortex and nucleus accumbens. Psychopharmacology (Berl) 183:144–153
Li Z, Huang M, Prus AJ, Dai J, Meltzer HY (2007) 5-HT6 receptor antagonist SB-399885 potentiates haloperidol and risperidone-induced dopamine efflux in the medial prefrontal cortex or hippocampus. Brain Res 1134:70–78
Liegeois JF, Ichikawa J, Meltzer HY (2002) 5-HT(2A) receptor antagonism potentiates haloperidol-induced dopamine release in rat medial prefrontal cortex and inhibits that in the nucleus accumbens in a dose-dependent manner. Brain Res 947:157–165
Lopez-Gil X, Babot Z, Margos-Bosch M, Sunol C, Artigas F, Adell A (2007) Clozapine and haloperidol differently suppress the MK-801-increased glutamatergic and serotonergic transmission in the medial prefrontal cortex of the rat. Neuropsychopharmacology 32:2087–2097
Marquis KL, Sabb AL, Logue SF, Brennan JA, Piesla MJ, Comery TA, Grauer SM, Ashby CR Jr, Nguyen HQ, Dawson LA, Barrett JE, Stack G, Meltzer HY, Harrison BL, Rosenzweig-Lipson S (2007) WAY-163909 [(7bR, 10aR)-1, 2, 3, 4, 8, 9, 10, 10a-octahydro-7bH-cyclopenta-[b][1, 4]diazepino[ 6, 7, 1hi]indole]: a novel 5-hydroxytryptamine 2C receptor-selective agonist with preclinical antipsychotic-like activity. J Pharmacol Exp Ther 320:486–496
Meltzer HY, McGurk SR (1999) The effects of clozapine, risperidone, and olanzapine on cognitive function in schizophrenia. Schizophr Bull 25:233–255
Moor E, Schirm E, Jacso J, Westerink BH (1998) Effects of neostigmine and atropine on basal and handling-induced acetylcholine output from ventral hippocampus. Neuroscience 82:819–825
Noda Y, Kamei H, Mamiya T, Furukawa H, Nabeshima T (2000) Repeated phencyclidine treatment induces negative symptom-like behavior in forced swimming test in mice: imbalance of prefrontal serotonergic and dopaminergic functions. Neuropsychopharmacology 23:375–387
O'Grada C, Dinan T (2007) Executive function in schizophrenia: what impact do antipsychotics have? Hum Psychopharmacol 22:397–406
Olsen CK, Brennum LT, Kreilgaard M (2008) Using pharmacokinetic-pharmacodynamic modelling as a tool for prediction of therapeutic effective plasma levels of antipsychotics. Eur J Pharmacol 584:318–327
Parikh V, Man K, Decker MW, Sarter M (2008) Glutamatergic contributions to nicotinic acetylcholine receptor agonist-evoked cholinergic transients in the prefrontal cortex. J Neurosci 28:3769–3780
Paxinos G, Watson C (1998) The rat brain in sterotaxic coordinates. Academic, San Diego
Pozzi L, Acconcia S, Ceglia I, Invernizzi RW, Samanin R (2002) Stimulation of 5-hydroxytryptamine (5-HT(2C)) receptors in the ventrotegmental area inhibits stress-induced but not basal dopamine release in the rat prefrontal cortex. J Neurochem 82:93–100
Pratt JA, Winchester C, Egerton A, Cochran SM, Morris BJ (2008) Modelling prefrontal cortex deficits in schizophrenia: implications for treatment. Br J Pharmacol 153(Suppl 1):S465–S470
Remington G, Kapur S (2000) Atypical antipsychotics: are some more atypical than others? Psychopharmacology (Berl) 148:3–15
Riemer C, Borroni E, Levet-Trafit B, Martin JR, Poli S, Porter RH, Bos M (2003) Influence of the 5-HT6 receptor on acetylcholine release in the cortex: pharmacological characterization of 4-(2-bromo-6-pyrrolidin-1-ylpyridine-4-sulfonyl) phenylamine, a potent and selective 5-HT6 receptor antagonist. J Med Chem 46:1273–1276
Rodefer JS, Nguyen TN, Karlsson JJ, Arnt J (2008) Reversal of subchronic PCP-induced deficits in attentional set shifting in rats by sertindole and a 5-HT(6) receptor antagonist: comparison among antipsychotics. Neuropsychopharmacology 33:2657–2666
Routledge C, Bromidge SM, Moss SF, Price GW, Hirst W, Newman H, Riley G, Gager T, Stean T, Upton N, Clarke SE, Brown AM, Middlemiss DN (2000) Characterization of SB-271046: a potent, selective and orally active 5-HT(6) receptor antagonist. Br J Pharmacol 130:1606–1612
Schmidt CJ, Fadayel GM (1995) The selective 5-HT2A receptor antagonist, MDL 100, 907, increases dopamine efflux in the prefrontal cortex of the rat. Eur J Pharmacol 273:273–279
Schousboe A, Waagepetersen HS (2006) Glial modulation of GABAergic and glutamatergic neurotransmission. Curr Top Med Chem 6:929–934
Shirazi-Southall S, Rodriguez DE, Nomikos GG (2002) Effects of typical and atypical antipsychotics and receptor selective compounds on acetylcholine efflux in the hippocampus of the rat. Neuropsychopharmacology 26:583–594
Stone JM, Morrison PD, Pilowsky LS (2007) Glutamate and dopamine dysregulation in schizophrenia—a synthesis and selective review. J Psychopharmacol 21:440–452
Talbot PS, Laruelle M (2002) The role of in vivo molecular imaging with PET and SPECT in the elucidation of psychiatric drug action and new drug development. Eur Neuropsychopharmacol 12:503–511
Tan HY, Callicott JH, Weinberger DR (2007) Dysfunctional and compensatory prefrontal cortical systems, genes and the pathogenesis of schizophrenia. Cereb Cortex 17(Suppl 1):i171–i181
Upton N, Chuang TT, Hunter AJ, Virley DJ (2008) 5-HT6 receptor antagonists as novel cognitive enhancing agents for Alzheimer's disease. Neurotherapeutics 5:458–469
van der Zeyden M, Oldenziel WH, Rea K, Cremers TI, Westerink BH (2008) Microdialysis of GABA and glutamate: analysis, interpretation and comparison with microsensors. Pharmacol Biochem Behav 90:135–147
Westerink BH, De Vries JB (1989) On the mechanism of neuroleptic induced increase in striatal dopamine release: brain dialysis provides direct evidence for mediation by autoreceptors localized on nerve terminals. Neurosci Lett 99:197–202
Wood MD, Scott C, Clarke K, Cato KJ, Patel N, Heath J, Worby A, Gordon L, Campbell L, Riley G, Davies CH, Gribble A, Jones DN (2006) Pharmacological profile of antipsychotics at monoamine receptors: atypicality beyond 5-HT2A receptor blockade. CNS Neurol Disord Drug Targets 5:445–452
Zuo DY, Zhang YH, Cao Y, Wu CF, Tanaka M, Wu YL (2006) Effect of acute and chronic MK-801 administration on extracellular glutamate and ascorbic acid release in the prefrontal cortex of freely moving mice on line with open-field behavior. Life Sci 78:2172–2178
Acknowledgements
The authors would like to thank Anette Frederiksen, Jeanett Raun Lott, and Nina Guldhammer for the skilful technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mørk, A., Witten, L.M. & Arnt, J. Effect of sertindole on extracellular dopamine, acetylcholine, and glutamate in the medial prefrontal cortex of conscious rats: a comparison with risperidone and exploration of mechanisms involved. Psychopharmacology 206, 39–49 (2009). https://doi.org/10.1007/s00213-009-1578-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-009-1578-4