Abstract
Rational
In humans, the N-methyl-d-aspartate antagonist phencyclidine (PCP) induces behavioral changes that mimic schizophrenia symptoms, including positive and negative symptoms as well as cognitive deficits. In clinic, the cognitive deficits are closely associated with functional outcome. Thus, improvement of cognition may have high impact on patients’ daily life.
Objective
In the present study, three second-generation antipsychotics (sertindole, risperidone, and clozapine) as well as the classical antipsychotic haloperidol were tested for the ability to reverse PCP-induced cognitive deficits in the Morris’ water maze.
Results
The second-generation antipsychotics reversed the PCP-induced cognitive impairment: sertindole (0.63–2.5 mg/kg, s.c.), risperidone (0.04 mg/kg, s.c.; whereas 0.08 and 0.16 mg/kg were without significant effect), and clozapine (0.63 mg/kg, s.c.; while 1.3 mg/kg was without significant effect). The significant effect of sertindole was observed from day 2 onwards, while clozapine and risperidone only had significant effect at day 3. The classical antipsychotic haloperidol (0.010–0.020 mg/kg, s.c.) was ineffective. No compounds influenced swimming speed at the doses used, indicating that motor function was preserved.
Conclusion
These results confirm that repeated PCP administration induces marked cognitive deficits. Further, second-generation antipsychotics like sertindole, clozapine, and risperidone within a certain, often narrow, dose range are able to reverse the impairment and thus might improve cognitive deficits in schizophrenic patients, whereas classical compounds like haloperidol lack this effect. The receptor mechanisms involved in the reversal of PCP’s disruptive effect are discussed and likely include a delicate balance between effects on dopamine D2, 5-HT2A/6, alpha-adrenergic, muscarinic, and histaminergic H1 receptors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Positive psychotic symptoms have, for many years, been considered as the hallmark for schizophrenia and been the target for pharmacological treatment. During the last decade, it has become increasingly evident that schizophrenia is also associated with cognitive dysfunction (Green et al. 2000; Goldberg et al. 1990; Weinberger and Gallhofer 1997), although Kreapelin already observed this a century ago. Cognitive deficits found in schizophrenic patients appear widespread and are related to working memory, learning, and attention. In contrast to psychotic symptoms, cognitive deficits are closely associated with community functioning and outcome measures (Addington and Addington 1999; Green 1996; Harvey et al. 1999; Velling et al. 1997). The cognitive deficits are present at the onset of illness, persist for the most of the patients’ life without remission, and may precede the development of psychotic symptoms (Tollefson 1996; Brewer et al. 2006). Cognitive deficits result in the lack of ability for self-care including frequent hospitalization and increased cost to the community (Sevy and Davidson 1995). Therefore, cognitively beneficial effect of a treatment may have a high impact on the patients’ quality of life. This appreciation has led to the Measurement And Treatment Research to Improve Cognition in Schizophrenia (MATRICS) initiative initiated by NMIH (http://www.matrics.ucla.edu).
Conventional antipsychotic treatments have been reported to lack effect on functional outcome (Mortimer 1997), and some cognitive functions may even be impaired (Cleghorn et al. 1990; Cutmore and Beninger 1990). A number of novel antipsychotic compounds have been developed within the last decade. Like clozapine (Fitton and Heel 1990), they all show a reduced potential to exert extrapyramidal side effects and have some beneficial effect on negative symptoms, e.g., olanzapine (Fulton and Goa 1997) and sertindole (Kane and Tamminga 1997). The effects of the second generation of antipsychotics on cognitive function in schizophrenic patients are inconsistent: Improvement, no effect, as well as impairment have been reported (Goldberg et al. 1993; Meltzer and McGurk 1999; Mortimer 1997), although the conclusion may depend on the type of cognitive domain measured (Hoff et al. 1996). The effect of sertindole on cognitive function in humans has not been investigated extensively. However, a small clinical trial indicates a beneficial effect on some cognitive substrates in schizophrenic patients (Lis et al. 2003).
In preclinical cognition tests, differential effects of antipsychotic treatment have also been reported, with some antipsychotics impairing cognitive function and others apparently without effect (Didriksen 1995; Skarsfeldt 1996; Didriksen et al. 2006). In the Skarsfeldt (1996) study, the effect of classical and second-generation antipsychotics was investigated using the Morris water maze (Morris 1984). The consensus cognitive battery identified by MATRICS, among others, include visual learning and memory (Nuechterlein et al. 2005) and suggest to include “animal models that involve learning the spatial placement of rewards and which requires longer memory periods than typical working memory tasks as these would be expected to require additional retrieval processes that are characteristic of many human visual learning and memory tasks.” The Morris water maze fulfils several of these requirements. Water maze performance is a visual learning and memory task depending upon the coordinated action of several brain regions and neurotransmitter systems (D’Hooge and De-Deyn 2001). Further, water maze performance is dependent on a variety of cognitive substrates including learning, working and long-term memory, retention, and attention and, therefore, relevant for the deficits found in schizophrenia.
As mentioned above, a major unmet need in schizophrenia is improvement of impaired cognition. Cognitive improvement by pharmacological intervention is difficult to show in young healthy animals and may have little predictive validity. Accordingly, it is highly important to develop animal models with low baseline cognitive performance and with relevance to the pathophysiology of schizophrenia. Phencyclidine (PCP) is a widely used animal model of psychosis and induces a variety of cognitive disturbances related to schizophrenia (Javitt and Zukin 1991; Jentsch and Roth 1999).
In the present study, we followed up on our earlier studies of cognitive side effects of antipsychotics administered to naive rats. The effects of selected antipsychotics (sertindole, risperidone, clozapine, and haloperidol) were investigated in PCP-pretreated rats with impaired cognitive performance. Haloperidol was selected as representative for the classical antipsychotics. Clozapine is the prototypical “atypical” drug, whereas risperidone is the most widely used antipsychotic drug belonging to the second generation. Sertindole is a new antipsychotic drug, which in several studies have shown a unique pharmacological profile (Arnt and Skarsfeldt 1998). The PCP regimen used is based on a previous study (Podhorna and Didriksen 2005) in which it was shown that by pretreating with PCP, tolerance develops to the motor disturbances induced, whereas the cognitive deficits persist in the Morris’ water maze.
Materials and methods
Subjects
Subjects (n = 144) were 3-month-old male Wistar rats delivered from Charles River, Germany, weighing approximately 280–300 g at the beginning of the experiments. The rats were kept on a 12:12 h light–dark cycle in groups of two in Macrolon type II cages, with lights on at 0600 hours and under controlled laboratory conditions (temperature 21 ± 2°C, humidity 55 ± 5% relative). Standard rodent food and tap water were available ad libitum. All experiments were performed in accordance with the ethical guidelines for animal research at H. Lundbeck A/S.
Apparatus
The rats were trained in Morris’ water maze. The water maze consisted of a circular, black pool measuring 1.20 m diameter × 0.45 m height. The pool was filled with water (21 ± 1°C) to a depth of 27 cm. A circular escape platform (8 cm in diameter) was placed in the southeast quadrant of the pool just below the water surface. Three start positions were at the perimeter of the pool: one in northwest, one in northeast, and one in southwest.
A video camera monitored the behavior of the rats in the pool, and the video signal was transmitted to a computer and analyzed using the Ethovision system from Noldus Information Technology (The Netherlands). The test room contained several permanent extra maze cues such as the rat housing rack, laboratory table, wall plates, etc. The rats use the extra maze cues as guidance for their spatial location to find the invisible platform. There were no cues inside the maze.
Behavioral procedure
Before the first and each successive trial, the rat was placed on the hidden platform for 15 s (intertrial period) indicating the presence and location of the escape platform. The rats were given three trials per day for three consecutive days. At the start of a trial, the rat was placed in the maze at one of the three different start positions such that, across trials, all three start positions were used. If the rat did not locate the platform within 60 s, the rat was gently placed on the platform.
The following parameters were measured or calculated during each trial; percentage of trials where the rat was unable to find the platform within the total trial time of 60 s (non-finders), swimming distance to reach the platform (m), and swim speed (m/s). Non-finders and swimming distance calculations were used as a measure for the development of spatial memory, whereas the swim speed was used to assess changes in motor function.
Drugs and treatment
Sertindole (H. Lundbeck A/S, Denmark), clozapine (Novartis, Switzerland), and risperidone (Janssen, Belgium) were dissolved in minimum amounts of 0.1 M hydrochloric acid and diluted with saline (distilled water was used for sertindole). Haloperidol (Janssen) was dissolved in 0.1 M tartaric acid and diluted with saline. PCP hydrochloride (synthesized by H. Lundbeck A/S) was dissolved in saline.
All test compounds, except PCP, were administered subcutaneously (s.c.) 60 min before the first daily trial (n = 8 per group). PCP (1.3 mg/kg) was injected s.c. once daily for 6 days, starting 3 days before the first test day in the water maze. On test days, PCP was administered s.c. 30 min before the test. All compounds were injected at a volume of 5 ml/kg body weight complying with the EFPIA/ECVAM guidelines (Diehl et al. 2001).
Statistics
The overall effects (all days included) of the compounds on swimming distance and swim speed were analyzed using Kruskal–Wallis one-way analysis of variance (ANOVA) on ranks followed by all pair-wise multiple comparison procedures by Dunn’s method. Parametric analysis was not allowed as normality test or equal variance test failed. One-way ANOVA or Kruskal–Wallis one−way ANOVA on ranks was performed on each single day dependent on the normality test and equal variance test followed by Student–Newman–Keuls post hoc test. The non-finders were analyzed using a non-parametric χ 2 test (Siegel 1956). The accepted level of significance was p < 0.05. SigmaStat statistical software version 3.01 from Jandel was used for all analyses.
Results
Effects of PCP
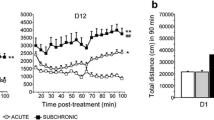
The subchronic (6 days) administration of PCP (1.3 mg/kg, s.c.) caused a significant disruption of learning and memory expressed by an increase in overall swimming distance to the submerged platform in all four experiments (p < 0.05 relative to vehicle; Fig. 1). The number of non-finders was also overall increased (p < 0.05 relative to vehicle calculated by χ 2 test) by the PCP treatment, although the increase did not reach level of significance on any single day in the clozapine experiment (Fig. 2). PCP had no overall effect on swim speed in any of the experiments (p > 0.05); however, a significant increase relative to vehicle was seen at day 3 in the sertindole experiment only (Fig. 3).
The effect of treatment on swimming distance to the submerged platform. Data presented are the average of three daily trials ± SEM. Asterisk p < 0.05 vs PCP on specific days. All compounds were administered s.c. (n = 8 per group). The antipsychotic compounds were administered 60 min and PCP 30 min before the first daily trial
The effect of treatment on non-finder, i.e., percentage of trials where the rat was unable to find the platform within the total trial time of 60 s. Data presented are the average of three daily trials ± SEM. Asterisk p < 0.05 vs PCP on specific days. All compounds were administered s.c. (n = 8 per group). The antipsychotic compounds were administered 60 min and PCP 30 min before the first daily trial
Effects of haloperidol
Haloperidol (0.010 and 0.020 mg kg−1day−1) had no effect on the PCP-induced cognitive impairment. Neither improvement nor further disruption was observed in any of the parameters measured during the three test days (Figs. 1, 2 and 3).
Effects of clozapine
Clozapine (0.63 mg kg−1day−1) reversed the effect of PCP on swimming distance, although this was only significant at day 3 (Fig. 1). The higher dose (1.3 mg/kg) was without effect (Fig. 1). No significant effect was found on non-finders; however, as described in “Effects of PCP,” the PCP-induced increase in non-finders did not reach statistical significance on any single day in this experiment (Fig. 2). Clozapine had no effect on swim speed (Fig. 3).
Effects of risperidone
Swimming distance was significantly shortened by risperidone (0.040 mg/kg/day) in comparison with the PCP-treated group at day 3 (Fig. 1). For non-finders, only the 0.080 mg kg−1day−1 dose group was overall significantly different from the PCP group, but this was only significant at day 3 with non-finders being increased (Fig. 2). Although not significantly different from the PCP group, non-finders were numerically reduced in the 0.040 mg kg−1day−1 dose group at days 2 and 3. Risperidone had no effect on motor function expressed as swim speed (Fig. 3).
Effects of sertindole
Sertindole overall reversed the disruptive effect of PCP on swimming distance (Fig. 1) and non-finders (Fig. 2) at all doses tested (i.e., 0.63, 1.3, and 2.5 mg kg−1day−1). The sertindole-treated groups had significantly shorter swimming distance at days 2 and 3 relative to the PCP-treated group (Fig. 1), and number of non-finders were significantly reduced for the 0.63 mg kg−1day−1 treated group at day 2 and for all sertindole-treated groups at day 3 (Fig. 2) revealed by the χ 2 test. The effect of sertindole on motor function expressed as swim speed did not differ from the PCP-treated group (Fig. 3).
Discussion
The present study aimed to follow up on previous studies in naive rats in which we determined the minimum effective doses of antipsychotics impairing learning and memory in the water maze, as a measure of cognitive side effects (Skarsfeldt 1996; Didriksen et al. 2006). The main previous finding was that different antipsychotics showed a large variation in the potential for inducing cognitive disturbances in comparison with their potencies in animal models of psychosis, e.g., inhibitory effects on amphetamine-induced behaviors (for review, see Arnt and Skarsfeldt 1998). Haloperidol and risperidone showed marked cognitive side effects at doses effective in psychosis models, while clozapine and sertindole were effective in the psychosis models but without detrimental effects on cognition (Skarsfeldt 1996; Arnt and Skarsfeldt 1998; Didriksen et al. 2006).
The objective of the present experiments was to examine the ability of these four drugs to reverse cognitive impairments induced by N-methyl-d-aspartate (NMDA) receptor blockade using PCP. The results indicate that the conventional antipsychotic haloperidol, as expected, did not reverse the detrimental effect of PCP, while clozapine and risperidone improved performance at a single low dose at day 3 of testing. In contrast, sertindole induced reversal across all three doses tested. The effect appeared already at day 2 of testing, and the disrupted behavior was fully normalized at day 3.
When comparing the effect of different drugs, it is essential that doses are chosen on a fair basis, thereby minimizing bias. This is particularly important if lack of efficacy is seen to avoid false negative results. The information relevant for dose selection is, for example, the efficacies determined in animal models for psychosis as well as plasma levels and central nervous system receptor occupancies are relevant for the clinical use of the drugs.
In the previous study of naive rats (Skarsfeldt 1996), minimum effective doses impairing water maze behavior were the following: haloperidol 0.040 mg/kg, s.c., risperidone 0.31 mg/kg, s.c., clozapine >10 mg/kg, s.c. (although 5.0–10 mg/kg induced transient impairment at days 1–2), and sertindole >2.5 mg/kg, s.c. Accordingly, dose selection for the present study was for haloperidol 0.010 and 0.020 mg/kg, for risperidone 0.040, 0.080, and 0.16 mg/kg, for clozapine 0.63 and 1.3 mg/kg (as pilot studies indicated a worsening of performance at 2.5, 5, and 10 mg/kg in combination with PCP), and for sertindole 0.63, 1.3, and 2.5 mg/kg. For haloperidol and risperidone, the selected doses show relevant dopamine (DA) D2 receptor occupancy in rats using the same route of administration (Natesan et al. 2006; Brennum, H. Lundbeck, unpublished). For sertindole, the clinically recommended doses (12–24 mg/day) lead to plasma concentrations of 35–100 ng/ml (Tamminga et al. 1997). After treatment with a single oral dose of 2.5 mg/kg, we have previously reported a plasma level of 129 ng/ml (Didriksen et al. 2006), and due to the long half-life of 13–15 h (H. Lundbeck, data on file), two- to threefold accumulation is obtained at pseudo steady state after repeated administration for about 3 days (Didriksen et al. 2006). Thus, a dose range of 0.63–2.5 mg kg−1day−1, s.c. is suggested to cover clinically relevant exposures. Clozapine has much lower affinity for DA D2 receptors than the other compounds, both in vitro and in vivo (Arnt and Skarsfeldt 1998; Leysen 2000), but has also been shown to be clinically effective at lower DA D2 occupancies (Kapur et al. 1999). Side effects limit the dose range that can be chosen, as indicated above. However, the doses used in the present study are effective in models for antipsychotic potential like the amphetamine- (Arnt 1995) and PCP-induced hyperactivity models (Gleason and Shannon 1997).
The reversal of the PCP-induced deficits are not mediated by DA D2 receptor blockade, as haloperidol had no effect while being the most specific DA D2 antagonist among the drugs tested. Besides having DA D2 antagonist properties, the second-generation antipsychotics also act on a number of other neurotransmitter receptors (Arnt and Skarsfeldt 1998; Leysen 2000). Effects on several of these receptors, and in particular the balance between these, may be involved in the reversal of the impaired cognitive performance induced by the PCP treatment.
All second-generation compounds in this study share potent antagonistic effects at 5-HT2A, 5-HT2C, and α1-adrenergic receptors, with effects at these targets often occurring with higher potencies than the effects at DA D2 receptors. It is known that selective ligands at these targets [e.g., M100907 (5-HT2A) and prazosin (α1), respectively] can inhibit locomotor hyperactivity induced by PCP or by the other prototype NMDA antagonist MK-801 (Gleason and Shannon 1997; Mathé et al. 1996). Antipsychotics with potent 5-HT2A and α1-adrenergic antagonistic activity also readily block PCP- or MK-801-induced hyperactivity (Gleason and Shannon 1997). Furthermore, prazosin and M100907 reverse MK-801- or PCP-disrupted prepulse inhibition of startle response (Bakshi and Geyer 1997; Varty et al. 1999). Other actions of PCP/MK-801 show variable sensitivity to reversal by second-generation antipsychotics, 5-HT2A, and α1-adrenergic modulation, e.g., in a model of social interaction (Sams-Dodd 1997) and in various cognitive models after acute or repeated administration of PCP or MK-801 (Boast et al. 1999; Hashimoto et al. 2005; Idris et al. 2005; Abdul et al. 2006).
Risperidone, clozapine, and sertindole have several other receptor activities in addition to the above mentioned but otherwise differ markedly in their profiles: Sertindole has very high affinity for 5-HT6 receptors but lack affinity for α2-adrenergic, histaminergic, and muscarinic receptors (Arnt and Skarsfeldt 1998; Leysen 2000). Risperidone has low 5-HT6 and muscarinic receptor affinity but has higher affinity for α2-adrenergic and histamine H1 receptors (ibid).
The 5-HT6 receptor is a candidate for cognition-enhancing effects based on studies of selective 5-HT6 antagonists. The 5-HT6 receptor is highly expressed in the hippocampus and cortex, shows interactions with cholinergic and glutamatergic mechanisms, and blockade of the receptor has procognitive effects and is followed by increases in DA, glutamate, and acetylcholine in the frontal cortex (review by Woolley et al. 2004; Hatcher et al. 2005; Rodefer et al. 2006; Lacroix et al. 2004; Dawson et al. 2001; Hirst et al. 2006). Thus, 5-HT6 receptor antagonism may rationalize the marked efficacy demonstrated with sertindole. Risperidone, as mentioned, has low 5-HT6 affinity, but its α2-adrenoceptor antagonist activity in combination with D2/D3 DA antagonism may contribute to the improvement of cognition in the present study. This is supported by studies showing that the cognitive deficits induced by MK-801 can be reversed by combined idazoxan and raclopride administration in parallel with an increase in extracellular DA in frontal cortex (Hertel et al. 1999; Marcus et al. 2005). However, the involvement of α2-adrenoceptors in cognition is not clear. The α2-adrenoceptor agonist clonidine reversed working memory deficits induced by subchronic PCP administration, and the disruptive effect of PCP was further enhanced by α2-antagonism (Marrs et al. 2005). Thus, the role of α2-adrenoceptors needs further clarification and may be task-dependent.
Finally, clozapine has a very broad profile, including significant activity at all the receptors discussed above (Arnt and Skarsfeldt 1998; Leysen 2000), making interpretation of mechanism of action of the observed effects very complex. Clozapine has weak partial agonist/antagonist effects on separate subtypes of muscarinic receptors (Zorn et al. 1994; Weiner et al. 2004). This is further complicated by the higher muscarinic M1 agonist efficacy of the main metabolite, desmethyl-clozapine, which occur in significant amounts in clozapine-treated patients (Weiner et al. 2004). As muscarinic M1 agonism may improve cognition (ibid), while antimuscarinic activity potentially worsens cognitive function (Riekkinen et al. 1990), the outcome of clozapine administration is rather unpredictable. It will likely depend on a balance between plasma and brain levels of the parent compound vs the metabolite, as suggested by Weiner et al. (2004). The metabolite ratio is influenced by metabolic activity and will be dependent on species studied, treatment regimen, and route of administration used in the experimental design.
In addition to the muscarinic effects, activities of clozapine and its metabolite on other receptors may influence the outcome of the cognition experiments, most notably the 5-HT and α-adrenergic receptor subtypes discussed earlier. Furthermore, the potent histamine H1 antagonist effect of clozapine (Arnt and Skarsfeldt 1998; Leysen 2000) may limit the cognitive improvement. In human studies combining functional neuroimaging and cognitive tasks, a strong correlation between increased histamine H1 occupancy and decreased cognitive performance was found (Okamura et al. 2000; Tashiro et al. 2002). Finally, clozapine-induced sedation which occurs at slightly higher doses than used in the present study may be attributable to the potent histamine H1 antagonism, although tolerance does develop after repeated treatment (Chesler and Salamone 1996). Taken together, many variables determine the efficacy of clozapine. The net outcome from the present study, indeed, was a limited reversal of the impairment induced by PCP in doses that does not affect water maze performance per se. Results of other studies vary considerably from full reversal (e.g. Marcus et al. 2005; Idris et al. 2005; Abdul et al. 2006) to no reversal (Rodefer et al. 2006) of PCP’s effects, most likely also depending on the specific task studied.
In conclusion, our data show that second-generation antipsychotics, but not haloperidol, can reverse PCP-induced cognitive impairment in rats in the Morris’ water maze. However, the effects of clozapine and risperidone are seen only in a narrow dose range, while the effect of sertindole is more robust across three dose levels. Several mechanisms may be involved in the PCP reversal, either alone or in combination; for sertindole particularly 5-HT6 receptor antagonism appears to be of importance and merits further investigation.
References
Abdul M, Reynolds GP, Neill JC (2006) The effect of atypical and classical antipsychotics on sub-chronic PCP-induced cognitive deficits in a reversal-learning paradigm. Behav Brain Res 169:263–273
Addington J, Addington D (1999) Neurocognitive and social functioning in schizophrenia. Schizophr Bull 25:173–182
Arnt J (1995) Differential effects of classical and newer antipsychotics on the hypermotility induced by two dose levels of d-amphetamine. Eur J Pharmacol 283:55–62
Arnt J, Skarsfeldt T (1998) Do novel antipsychotics have similar pharmacological characteristics? A review of the evidence. Neuropsychopharmacology 18:63–101
Bakshi VP, Geyer MA (1997) Phencyclidine-induced deficits in prepulse inhibition of startle are blocked by prazosin, an alpha-1 noradrenergic antagonist. J Pharmacol Exp Ther 283:666–674
Boast C, Bartolomeo AC, Morris H, Moyer JA (1999) 5HT antagonists attenuate MK801-impaired radial arm maze performance in rats. Neurobiol Learn Mem 71:259–271
Brewer W, Wood S, Phillips L, Francey S, Pantelis C, Yung A, Cornblatt B, McGorry P (2006) Generalized and specific cognitive performance in clinical high-risk cohorts: a review highlighting potential vulnerability markers for psychosis. Schizophr Bull 32:538–555
Chesler EJ, Salamone JD (1996) Effects of acute and repeated clozapine injections on cholinomimetic-induced vacuous jaw movements. Pharmacol Biochem Behav 54:619–624
Cleghorn JM, Kaplan RD, Szechtman B, Szechtman H, Brown GM (1990) Neuroleptic drug effects on cognitive function in schizophrenia. Schizophr Res 3:211–219
Cutmore TRH, Beninger RJ (1990) Do neuroleptics impair learning in schizophrenic patients. Schizophr Res 3:173–186
D’Hooge R, De-Deyn PP (2001) Applications of the Morris water maze in the study of learning and memory. Brain Res Brain Res Rev 36:60–90
Dawson LA, Nguyen HQ, Li P (2001) The 5-HT(6) receptor antagonist SB-271046 selectively enhances excitatory neurotransmission in the rat frontal cortex and hippocampus. Neuropsychopharmacology 25:662–668
Didriksen M (1995) Effects of antipsychotics on cognitive behaviour in rats using the delayed non-match to position paradigm. Eur J Pharmacol 281:241–250
Didriksen M, Kreilgaard M, Arnt J (2006) Sertindole, in contrast to clozapine and olanzapine, does not disrupt water maze performance after acute or chronic treatment. Eur J Pharmacol 542:108–115
Diehl K-H, Hull R, Morton D, Pfister R, Rabemampianina Y, Smith S, Vidal J-M, Van De Vorstenbosch C (2001) A good practice guide to the administration of substances and removal of blood, including routes and volumes. J Appl Toxicol 21:15–23
Fitton A, Heel RC (1990) Clozapine. A review of its pharmacological properties, and therapeutic use in schizophrenia. Drugs 40:722–747
Fulton B, Goa KL (1997) Olanzapine, a review of its pharmacological properties and therapeutic efficacy in the management of schizophrenia and related psychoses. Drugs 53:281–298
Gleason SD, Shannon HE (1997) Blockade of phencyclidine-induced hyperlocomotion by olanzapine, clozapine and serotonin receptor subtype selective antagonists in mice. Psychopharmacology 129:79–84
Goldberg TE, Ragland D, Torrey EF, Gold JM, Bigelow LB, Weinberger DR (1990) Neuropsychological assessment of monozygotic twins discordant for schizophrenia. Arch Gen Psychiatry 47:1066–1072
Goldberg TE, Greenberg RD, Griffin SJ, Gold JM, Kleinman JE, Pickar D, Schulz SC, Weinberger DR (1993) The effect of clozapine on cognition and psychiatric symptoms in patients with schizophrenia. Br J Psychiatry 162:43–48
Green MF (1996) What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry 153:321–330
Green MF, Kern RS, Braff DL, Mintz J (2000) Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull 26:119–136
Harvey PD, Parrella M, White L, Mohs RC, Davidson M, Davis KL (1999) Convergence of cognitive and adaptive decline in late-life schizophrenia. Schizophr Res 35:77–84
Hashimoto K, Fujita Y, Shimizu E, Iyo M (2005) Phencyclidine-induced cognitive deficits in mice are improved by subsequent subchronic administration of clozapine, but not haloperidol. Eur J Pharmacol 519:114–117
Hatcher P, Brown V, Tait D, Bate S, Overend P, Hagan J, Jones D (2005) 5-HT6 receptor antagonists improve performance in an attentional set shifting task in rats. Psychopharmacology 181:253–259
Hertel P, Fagerquist MV, Svensson TH (1999) Enhanced cortical dopamine output and antipsychotic-like effects of raclopride by alpha2 adrenoceptor blockade. Science 286:105–107
Hirst W, Stean T, Rogers D, Sunter D, Pugh P, Moss S, Bromidge S, Riley G, Smith D, Bartlett S, Heidbreder C, Atkins A, Lacroix L, Dawson L, Foley A, Regan C, Upton N (2006) SB-399885 is a potent, selective 5-HT6 receptor antagonist with cognitive enhancing properties in aged rat water maze and novel object recognition models. Eur J Pharmacol 553:109–119
Hoff AL, Faustman WO, Wieneke M, Espinoza S, Costa M, Wilkowitz O, Csernansky JG (1996) The effect of clozapine on symptom reduction, neurocognitive function, and clinical management in treatment-refractory state hospital schizophrenic inpatients. Neuropsychopharmacology 15:361–369
Idris NF, Repeto P, Neill JC, Large CH (2005) Investigation of the effects of lamotrigine and clozapine in improving reversal-learning impairments induced by acute phencyclidine and d-amphetamine in the rat. Psychopharmacology 179:336–348
Javitt DC, Zukin SR (1991) Recent advances in the phencyclidine model of schizophrenia. Am J Psychiatry 148:1301–1308
Jentsch JD, Roth RH (1999) The neuropsychopharmacology of phencyclidine: from NMDA receptor hypofunction to the dopamine hypothesis of schizophrenia. Neuropsychopharmacology 20:201–225
Kane JM, Tamminga CA (1997) Sertindole (serdolect): preclinical and clinical findings of a new atypical antipsychotic. Expert Opin Investig Drugs 6:1729–1741
Kapur S, Zipursky RB, Remington G (1999) Clinical and theoretical implications of 5-HT2 and D2 receptor occupancy of clozapine, risperidone, and olanzapine in schizophrenia. Am J Psychiatry 156:286–293
Lacroix L, Dawson L, Hagan J, Heidbreder C (2004) 5-HT6 receptor antagonist SB-271046 enhances extracellular levels of monoamines in the rat medial prefrontal cortex. Synapse 51:158–164
Leysen JE (2000) Receptor profile of antipsychotics. In: Ellenbroek BA, Cools AR (eds) Atypical antipsychotics. Milestones in drug therapy. Birkhäuser Verlag, Basel, pp 57–81
Lis S, Krieger S, Gallhofer B, Torre P, Mittoux A, Menard F (2003) Sertindole is superior to haloperidol in cognitive performance in patients with schizophrenia: a comparative study. Eur Neuropsychopharmacol 13:S323–S324
Marcus M, Jardemark K, Wadenberg M, Langlois X, Hertel P, Svensson T (2005) Combined alpha2 and D2/3 receptor blockade enhances cortical glutamatergic transmission and reverses cognitive impairment in the rat. Int J Neuropsychopharmacol 8:315–327
Marrs W, Kuperman J, Avedian T, Roth R, Jentsch J (2005) Alpha-2 adrenoceptor activation inhibits phencyclidine-induced deficits of spatial working memory in rats. Neuropsychopharmacology 30:1500–1510
Mathé JM, Nomikos GG, Hildebrand BE, Hertel P, Svensson TH (1996) Prazosin inhibits MK-801-induced hyperlocomotion and dopamine release in the nucleus accumbens. Eur J Pharmacol 309:1–11
Meltzer HY, McGurk SR (1999) The effects of clozapine, risperidone, and olanzapine on cognitive function in schizophrenia. Schizophr Bull 25:233–255
Morris RGM (1984) Developments of a water-maze procedure for studying spatial learning in the rat. J Neurosci Methods 11:47–60
Mortimer AM (1997) Cognitive function in schizophrenia—do neuroleptics make a difference? Pharmacol Biochem Behav 56:789–795
Natesan S, Reckless G, Nobrega J, Fletcher P, Kapur S (2006) Dissociation between in vivo occupancy and functional antagonism of dopamine D2 receptors: comparing aripiprazole to other antipsychotics in animal models. Neuropsychopharmacology 31:1854–1863
Nuechterlein KH, Robbins TW, Einat H (2005) Distinguishing separable domains of cognition in human and animal studies: what separations are optimal for targeting interventions? A summary of recommendations from breakout group 2 at the measurement and treatment research to improve cognition in schizophrenia new approaches conference. Schizophr Bull 31:870–874
Okamura N, Yanai K, Higuchi M, Sakai J, Iwata R, Ido T, Sasaki H, Watanabe T, Itoh M (2000) Functional neuroimaging of cognition impaired by a classical antihistamine, d-chlorpheniramine. Br J Pharmacol 129:115–123
Podhorna J, Didriksen M (2005) Performance of male C57BL/6J mice and Wistar rats in the water maze following various schedules of phencyclidine treatment. Behav Pharmacol 16:25–34
Riekkinen P Jr, Sirviö J, Aaltonen M, Riekkinen P (1990) Effects of concurrent manipulations of nicotinic and muscarinic receptors on spatial and passive avoidance learning. Pharmacol Biochem Behav 37:405–410
Rodefer JS, Nguyen TN, Arnt J (2006) The effects of antipsychotics on cognitive deficits produced by subchronic PCP administration in a rodent attentional ED/ID set-shifting task. Int J Neuropsychopharmacol 9(S1):S140
Sams-Dodd F (1997) Effect of novel antipsychotic drugs on phencyclidine-induced stereotyped behaviour and social isolation in the rat social interaction test. Behav Pharmacol 8:196–215
Sevy S, Davidson M (1995) The costs of cognitive impairment in schizophrenia. Schizophr Res 17:1–3
Siegel S (1956) Nonparametric statistics for the behavioral sciences. McGraw-Hill, New York
Skarsfeldt T (1996) Differential effect of antipsychotics on place navigation of rats in the Morris water maze. Psychopharmacology 124:126–133
Tamminga CA, Mack RJ, Granneman GR, Silber CJ, Kashkin KB (1997) Sertindole in the treatment of psychosis in schizophrenia: efficacy and safety. Int Clin Psychopharmacol 12(Suppl 1):S29–S35
Tashiro M, Mochizuki H, Iwabuchi K, Sakurada Y, Itoh M, Watanabe T, Yanai K (2002) Roles of histamine in regulation of arousal and cognition: functional neuroimaging of histamine H1 receptors in human brain. Life Sci 72:409–414
Tollefson GD (1996) Cognitive function in schizophrenic patients. J Clin Psychiatry 57:31–39
Varty GB, Bakshi VP, Geyer MA (1999) M100907, a serotonin 5-HT2A receptor antagonist and putative antipsychotic, blocks dizocilpine-induced prepulse inhibition deficits in Sprague–Dawley and Wistar rats. Neuropsychopharmacology 20:311–321
Velling DI, Mahurin RK, Diamond PL, Hazleton BC, Eckert SL, Miller AL (1997) The functional significance of symptomatology and cognitive function in schizophrenia. Schizophr Res 25:21–31
Weinberger DR, Gallhofer B (1997) Cognitive function in schizophrenia. Int Clin Psychopharmacol 12:S29–S36
Weiner DM, Meltzer HY, Veinbergs I, Donohue EM, Spalding TA, Smith TT, Mohell N, Harvey SC, Lameh J, Nash N, Vanover KE, Olsson R, Jayathilake K, Lee M, Levey AI, Hacksell U, Burstein ES, Davis RE, Brann MR (2004) The role of M1 muscarinic receptor agonism of N-desmethylclozapine in the unique clinical effects of clozapine. Psychopharmacology 177:207–216
Woolley ML, Marsden CA, Fone KCF (2004) 5-HT(6) receptors. Curr Drug Targets CNS Neurol Dis 3:59–79
Zorn SH, Jones SB, Ward KM, Liston DR (1994) Clozapine is a potent and selective muscarinic M4 receptor agonist. Eur J Pharmacol 269:R1–R2
Acknowledgement
The authors would like to thank Birgitte Bjørkenberg, Marlene Quvang Jørgensen, and Maj-Britt Filsø Mathiassen for their excellent technical assistance in conducting these experiments.
All experiments were conducted in accordance with the Danish animal protection law.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Didriksen, M., Skarsfeldt, T. & Arnt, J. Reversal of PCP-induced learning and memory deficits in the Morris’ water maze by sertindole and other antipsychotics. Psychopharmacology 193, 225–233 (2007). https://doi.org/10.1007/s00213-007-0774-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-007-0774-3