Abstract
Rational
Atypical antipsychotic drugs (APDs) such as clozapine, olanzapine, quetiapine, risperidone, and ziprasidone are serotonin (5-HT)2A antagonists and relatively weaker dopamine (DA) D2 antagonists, with variable 5-HT2C antagonist properties. The ability of atypical APDs to preferentially increase DA release in the cortex compared to the limbic system is believed to be due in part to their antagonism of 5-HT2A and D2 receptors and believed to contribute to their beneficial effects on cognition, negative, and psychotic symptoms. Previous studies from this laboratory using microdialysis have shown that pretreatment of the 5-HT2A antagonist M100907 with the typical APD and D2 antagonist haloperidol produced an increase in the medial prefrontal cortex (mPFC), but not in the nucleus accumbens (NAC), DA release. However, pretreatment with the 5-HT2A/2C receptor antagonist SR46349-B with haloperidol increased both mPFC and NAC DA release, suggesting that both 5-HT2A and 5-HT2C properties may be important for atypical APD effects.
Objective
The purpose of this study was to examine the effects of a novel putative atypical APD ACP-103 on mPFC and NAC DA release using in vivo microdialysis in freely moving rats that are awake. ACP-103 is an inverse agonist at both 5-HT2A and 5-HT2C receptors and has intermediate affinities for 5-HT2C receptors relative to their affinities for 5-HT2A receptors compared to M100907 and SR46349-B. In addition, the effects of ACP-103 were compared to M100907 and SR46349-B, and ACP-103 was also coadministered with haloperidol.
Results
ACP-103 10.0 mg/kg, but not 3.0 mg/kg, increased DA release in the mPFC, while neither dose increased DA release in the NAC. Like M100907, ACP-103 (3.0 mg/kg) potentiated 0.1 mg/kg haloperidol-induced DA release in the mPFC while inhibiting that in the NAC. However, ACP-103 (3.0 mg/kg), similar to SR46349-B, potentiated a high dose of haloperidol (1.0 mg/kg)-induced DA release in both regions. The potent 5-HT2C antagonist SB242084 1.0 mg/kg significantly potentiated 0.1 mg/kg haloperidol-induced DA release in both the mPFC and NAC. However, SB242084, at 0.2 mg/kg, significantly potentiated DA release only in the NAC. Moreover, SB242084 0.2 mg/kg potentiated DA release in the NAC produced by the combination treatment of 3 mg/kg ACP-103 and 0.1 mg/kg haloperidol.
Conclusion
These data suggest that the relative extent of 5-HT2A and 5-HT2C antagonism, as well as the extent of D2 receptor blockade, has a critical influence on DA release in the mPFC and NAC and may be a determining factor in the action of this class of atypical APDs on these two potentially clinically relevant parameters.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Potent serotonin (5-HT)2A antagonism, in relation to weaker dopamine (DA) D2 receptor antagonism, has been suggested to distinguish atypical antipsychotic drugs (APDs) such as clozapine, quetiapine, olanzapine, risperidone, and ziprasidone from the typical APDs haloperidol or (−)-sulpiride and is a major factor contributing to their antipsychotic action and low extrapyramidal side effect (EPS) (Meltzer et al. 1989; Schotte et al. 1996; Ichikawa and Meltzer 1999). Atypical, but not typical, APDs preferentially increase DA release in the medial prefrontal cortex (mPFC) compared to the limbic system, e.g., the nucleus accumbens (NAC), which is believed to be a potential basis for the ability of the atypical APDs to improve cognition in schizophrenia (Moghaddam and Bunney 1990; Kuroki et al. 1999; Meltzer and McGurk 1999; Ichikawa et al. 2001; Li et al. 2004). The ability of these agents to increase DA release in the mPFC, a region of the brain with a central role in many cognitive functions, has been suggested to be due in part to relatively more potent 5-HT2A receptor than to a D2 receptor blockade. Using in vivo microdialysis in rats, the pretreatment of the selective 5-HT2A receptor antagonist M100907 before administration of the D2 antagonists haloperidol or sulpiride produced an increase in mPFC DA release, which was not observed by these compounds administered alone (Kuroki et al. 1999; Ichikawa et al. 2001; Liégeois et al. 2002). Further, M100907 was able to enhance mPFC DA release in combination with a low dose (0.1 mg/kg) of haloperidol, which, based on D2 receptor occupancy studies, is similar to a subtherapeutic dose in humans. Thus, the ability to maintain antipsychotic effects without high D2 receptor occupancy may also contribute to the lack of EPS produced by atypical APDs.
Many drugs that bind to 5-HT2A receptors with a high affinity also bind, to some extent, to the structurally related 5-HT2C receptors. Some, but not all, typical and atypical APDs have a high affinity for 5-HT2C relative to 5-HT2A receptors (Canton et al. 1990; Roth et al. 1992; Schotte et al. 1996). Quetiapine and risperidone are less potent 5-HT2C than 5-HT2A receptor antagonists, whereas olanzapine and ziprasidone have only slightly weaker affinities for 5-HT2C receptors (Table 1; Roth et al. 1992; Schotte et al. 1996). 5-HT2C antagonism has been postulated to be of therapeutic value for some components of the schizophrenia syndrome, e.g., anxiety, depression, and cognitive deficits. 5-HT2C receptors also exert a preferential control of impulse-flow independent DA release in the NAC and striatum (STR) (Willins and Meltzer 1998; Lucas et al. 2000). 5-HT2C receptors have an important effect on basal DA release in the cortex and NAC. Thus, systemic administration of the selective 5-HT2C antagonist SB242084 by itself increases DA release in the NAC (Di Matteo et al. 1999). Gobert et al. (2000) presented microdialysis and electrophysiologic data which strongly suggested that 5-HT2C receptors exert an inhibitory effect on the burst firing of DA neurons in the ventral tegmental area (VTA) and substantia nigra, and that stimulation of 5-HT2C receptors in the VTA or cortex by the selective 5-HT2C agonist Ro 60-0175 has no effect on cortical DA release under basal conditions (Pozzi et al. 2002). However, blocking these receptors with the 5-HT2C antagonist SB242084 can enhance DA release in the rat cortex (Gobert et al. 2000). They concluded that these tonically active, excitatory 5-HT2C receptors are probably localized on inhibitory gamma-aminobutyric acid (GABA)ergic interneurons on the cell bodies of VTA neurons. The selective 5-HT2C agonist Ro 60-0175 has been shown to inhibit DA release in the cortex, NAC, and STR by Gobert et al. (2000), suggesting that cortical 5-HT2C receptors also tonically inhibit cortical DA release. But Pozzi et al. (2002) were unable to replicate these results in the cortex. In addition, it has been reported that 5-HT2C antagonists potentiate the increase in DA release induced by drugs which increase the activity of DA neuron, e.g., haloperidol, morphine, or phencyclidine (Hutson et al. 2000; Lucas et al. 2000; Porras et al. 2002). Thus, it may be concluded that both 5-HT2A and 5-HT2C receptors, acting at the level of the VTA and the cortex on the perikarya of DA neurons on GABAergic interneurons, respectively, influence cortical DA release. However, the interaction, if any, between 5-HT2A and 5-HT2C receptors, with and without D2 receptor blockade in the mPFC and NAC, is still unclear, as is the significance of this for the clinical effects of atypical APDs which have variable 5-HT2A and 5-HT2C antagonism. Therefore, we hypothesize that addition of 5-HT2C antagonist to the atypical APDs which have low affinities for these receptors may augment their ability to increase cortical DA release which is related to cognitive function.
We have recently reported that another putative APD, SR46349-B, a 5-HT2A/2C antagonist, potentiates both low and high doses of haloperidol-induced DA release in both mPFC and NAC, and this increase in the mPFC, but not NAC, is dependent upon 5-HT1A receptor stimulation (Bonaccorso et al. 2002) as is the case with clozapine and related atypical APDs (Ichikawa et al. 2001). These results suggest that 5-HT2C receptor antagonism may also contribute to the potentiation of DA release produced by haloperidol, and that combined 5-HT2A/2C antagonism may be more advantageous than selective 5-HT2A antagonism as an adjunct to D2 antagonists to improve cognition and negative symptoms in schizophrenia. Indeed, in clinical trials, SR46349-B has been shown to be more effective than placebo in decreasing total psychopathology in newly hospitalized subjects with schizophrenia (Meltzer et al. 2004). M100907 and SR46349-B have been, and still are, of interest as treatments for schizophrenia and l-DOPA-induced psychosis by themselves or as an adjunctive treatment to APDs such as haloperidol. In addition, it has been reported that ritanserin, a mixed 5-HT2A/2C antagonist (Roth et al. 1992), also increases cortical DA release after local administration into the cortex (Pehek 1996). Moreover, it potentiates the D2/3 receptor antagonist raclopride-induced DA release in the mPFC and NAC, but not in the STR (Andersson et al. 1995).
Recently, it has been recognized that most clinically effective APDs are, in fact, inverse agonists at 5-HT2A and 5-HT2C receptors rather than simply neutral antagonists (Weiner et al. 2001; Herrick-Davis et al. 2000). Potency increased as 5-HT2A/2C inverse agonists contribute to the effects of atypical APDs (Herrick-Davis et al. 2000; Weiner et al. 2001; Vanover et al. 2004). The putative atypical APD ACP-103, a 5-HT2A/2C receptor inverse agonist (Vanover et al., unpublished data), which has a high potency for the 5-HT2A receptor (Ki=0.4 nM) and is relatively weak for 5-HT2C receptors (Ki=16 nM), also has been shown to act as a 5-HT2A/2C antagonist. It attenuates (±)−2,5-dimethoxy-4-iodoamphetamine hydrochloride (DOI)-induced head twitches and blocks MK-801 and phencyclidine (PCP)-induced hyperactivity and DOI-induced sensory gating deficits (Investigator's Brochure, Acadia Pharmaceuticals Inc., 2003), which are predictive of antipsychotic- and cognitive-enhancing properties. ACP-103 does not have significant potency for other G-protein-coupled receptors such as muscarinic, histaminergic or adrenergic receptors, or for ion channel receptors. Lately, an ongoing double-blind, placebo-controlled, dose-escalation phase II clinical trial was designed to evaluate the efficacy and tolerability of ACP-103 in 60 Parkinson's disease patients who suffer from treatment-induced psychosis. Results of the interim analysis demonstrated that the ACP-103 treatment group showed a greater reduction in psychotic symptoms on both rating scales [Severity of Illness Scale (CGI-S) and the Scale for the Assessment of Positive Symptoms (SAPS)], relative to the placebo treatment group (Acadia Pharmaceuticals Inc. 2005). Using in vivo microdialysis in moving rats that are awake, the present study determined the effect of ACP-103, alone and together with the D2 antagonist haloperidol and the potent 5-HT2C antagonist SB242084, on DA release in the mPFC and NAC. We compared it with M100907 and SR46349-B on the ability to increase DA release in these two brain regions.
Materials and methods
Animals
Male Sprague–Dawley albino rats (Zivic-Miller Laboratories, Porterville, PA, USA) weighing 250–350 g were housed two per cage and maintained in a controlled 12-h light/12-h dark cycle and under constant temperature at 22°C with free access to food and water.
Surgery and microdialysis
Rats were anesthetized with the modified Equithesin mixture (810 mg pentobarbital, 4.3 g choral hydrate, 2.12 mg MgSO4, 14 ml ethanol, and 29 ml propylene glycol were dissolved in saline, and the final volume was 100 ml) and mounted in a stereotaxic frame (Stoetling, Wood Dale, IL, USA). Two stainless guide cannula (21-gauge) with a dummy probe were placed and fixed by cranioplastic cement (Plastic One, Roanoke, VA, USA) onto the cortex dorsal both to the right mPFC and the left NAC (dual-probe implantation). Stereotaxic coordinates of each probe, when implanted, were A +3.2, L +0.8 (10° inclination), and V −5.5 mm for the mPFC and A +2.0, L +1.5–1.7, and V −7.5 mm for the NAC, respectively, relative to bregma. The incisor bar level was 3.0 mm according to the atlas of Paxinos and Watson (1998).
The microdialysis probes were constructed in our laboratory. A silica–glass capillary tube (150 μm o.d., 75 μm i.d., Polymicro Technologies, Phoenix, AZ, USA) was inserted through the inner bore of a 25-g stainless tube. The stainless tube was inserted into a 28-g Teflon tubing, and then the Teflon tubing was inserted into the inner bore of an 18-g stainless tube. The hollow fiber dialysis membrane (polyacrylonitrile/sodium methalylsulfonate polymer, 310 μm o.d., 220 μm i.d., 40,000 Da cutoff, AN69HF, Hospal; CGH Medical, Lakewood, CO, USA) was fitted over the glass capillary and into the end of the 25-g stainless tube. This junction (0.5 mm) was glued with epoxy (5-Minute Epoxy; Devkon, Danverse, MA, USA) after the length of the hollow dialysis fiber was cut to 3 mm, and the tip of the membrane (0.5 mm) was plugged with epoxy. The length of exposed nonglued surface for dialyzing was 3 mm.
The dialysis probes were implanted into the mPFC and NAC under slight anesthesia with methoxyflurane (Metofane, Pitman-Moore, Mundelein, IL, USA) 3–5 days after cannulation. Rats were then housed individually overnight in a dialysis cage. After the overnight perfusion at 0.4 μl/min of the probe, dialysate samples were collected every 30 min at the rate of 1.5 μl/min. The perfusion medium was Dulbecco's phosphate-buffered saline solution (Sigma, St. Louis, MO, USA), including Ca2+ (138 mM NaCl, 8.1 mM Na2HPO4, 2.7 mM KCl, 1.5 mM KH2PO4, 0.5 mM MgCl, and 1.2 mM CaCl2, pH 7.4). After stable baseline values in the dialysates were obtained, each drug or vehicle was administered to the rats through a catheter that, constructed from microbore Tygon tubing (TGY-010, 0.03′ o.d., 0.01′ i.d.; Small Parts Inc., Miami Lakes, FL, USA), was implanted subcutaneously in the intrascapular space of the rats. The location of the dialysis probes was verified at the end of each experiment by manual brain dissection and with 100-μm brain slices (OTS-4000; FHC, Bowdoinham, ME, USA). The procedures applied in these experiments were approved by the Institute Animal Care and Use Committee of Vanderbilt University in Nashville, TN, USA.
Biochemical assay
Dialysate samples were directly applied onto a high-performance liquid chromatography (HPLC) with electrochemical detection and analyzed with a Millennium chromatogram manager (Waters, Milford, MA, USA). Dopamine was separated (BDS Hypersil 3 μm C18, 1.0×100 mm; Keystone Scientific, Bellefonte, PA, USA) at 35°C maintained by a column heater (LC-22C temperature controller; BAS, West Lafayette, IN, USA). The mobile phase consisted of 48 mM anhydrous citric acid and 24 mM sodium acetate trihydrate containing 0.5 mM EDTA–Na2, 10 mM NaCl, 2 mM dodecyl sulfate sodium salt, and 17% (v/v) acetonitrile, adjusted to pH 4.8 with concentrated NaOH, and was pumped (0.05 ml/min) by an LC-10AD (Shimadzu, Kyoto, Japan). A unijet working electrode (MF-1003, BAS) was set at +0.58 V (LC-4C, BAS) vs an Ag/AgCl reference electrode. Reagents used were analytical or HPLC grade.
Drugs
ACP-103 and SB242084 (Acadia) were dissolved in 45% 2-hydroxypropyl-β-cyclodextrin (Research Biochemical Inc., Natick, MA, USA). Haloperidol (McNeil, Spring House, PA, USA) was dissolved in a small mount of 0.1 M tartaric acid solution and then was adjusted to pH 6–7 with NaOH. Vehicle or drugs in a volume of 1.0 ml/kg were administered subcutaneously to randomly assigned rats.
Data analysis
Mean predrug baseline levels (time −60, time −30, and time 0) were designated as 100%. Following a significant overall repeated-measure analysis of variance (ANOVA), a one-way ANOVA was used to determine group differences (StatView 4.5 for Macintosh). A probability of p<0.05 was considered significant in this study. All results are given as mean±SEM.
Results
Basal extracellular DA levels in the mPFC and the NAC
The baseline samples were collected after a 1-h perfusion, and basal extracellular levels of DA remained stable before the drug injection. Basal extracellular DA levels in the dialysates obtained from all the rats used in this study were 2.25±0.11 (mean±SEM fmol/20 μl; N=46) for the mPFC and 15.26±0.52 (mean±SEM fmol/20 μl; N=39) for the NAC, respectively. There was no significant difference in basal extracellular DA levels between treatment groups in each region.
Effects of ACP-103 on haloperidol-induced extracellular DA levels in the mPFC and the NAC
ACP-103 10.0 mg/kg, but not 3.0 mg/kg, significantly increased DA release in the mPFC [Fig. 1; F(1,11)=9.16, p<0.01 and F(1,11)=2.16, p=0.2, respectively] compared to the vehicle group. However, neither of these doses had any effect on DA levels in the NAC. Consistent with a previous study from our laboratory (Liégeois et al. 2002), 0.1 mg/kg haloperidol produced a slight increase in mPFC and NAC DA release (Fig. 2), while 1.0 mg/kg haloperidol produced a greater increase in DA release in the NAC but not in the mPFC (Fig. 3). The combination of 3.0 mg/kg ACP-103 and 0.1 mg/kg haloperidol significantly increased DA release in the mPFC [Fig. 2; F(1,12)=7.72, p<0.01] but significantly attenuated 0.1 mg/kg haloperidol-induced DA release in the NAC [Fig. 2; F(1,11)=4.96, p<0.05]. In the mPFC, 3.0 mg/kg ACP-103 also significantly potentiated haloperidol (1.0 mg/kg)-induced DA release [Fig. 3; F(1,11)=16.63, p<0.001] as well as the NAC [Fig. 3; F(1,11)=49.1, p<0.001] compared to the effect of 1.0 mg/kg haloperidol alone on DA release in the mPFC or NAC.
The effect of 5-HT2A/2C inverse agonist ACP-103 (3 and 10 mg/kg, s.c.) on extracellular dopamine (DA) levels in the medial prefrontal cortex (mPFC) and nucleus accumbens (NAC). Data are means±SEM of the dialysate DA levels, expressed as a percentage of each predrug baseline DA value (N=5–7). The arrows indicate drug injection times
The effect of 5-HT2A/2C inverse agonist (3 mg/kg, s.c.) on the D2 antagonist haloperidol (0.1 mg/kg, s.c.)-induced extracellular dopamine (DA) levels in the medial prefrontal cortex (mPFC) and nucleus accumbens (NAC). Rats were pretreated with ACP-103 30 min prior to administration of haloperidol. Data are means±SEM of the dialysate DA levels, expressed as a percentage of each predrug baseline DA value (N=5–8). The arrows indicate drug injection times
The effect of the 5-HT2A/2C inverse agonist (3 mg/kg, s.c.) on the D2 antagonist haloperidol (1.0 mg/kg, s.c.)-induced extracellular dopamine (DA) levels in the medial prefrontal cortex (mPFC) and nucleus accumbens (NAC). Rats were pretreated with ACP-103 30 min prior to administration of haloperidol. Data are means±SEM of the dialysate DA levels, expressed as a percentage of each predrug baseline DA value (N=5–7). The arrows indicate drug injection times
Effects of SB242084 on haloperidol-induced extracellular DA levels in the mPFC and the NAC
Both 0.2 and 1.0 mg/kg doses of SB242084 alone had no statistically significant effect on DA release in either the mPFC [F(1,8)=1.75, p=0.87 and F(1,8)=2.25, p=0.21, respectively] or the NAC [F(1,8)=1.05, p=0.91 and F(1,8)=3.25, p=0.22, respectively]. However, the low dose of SB242084 (0.2 mg/kg) significantly potentiated 0.1 mg/kg haloperidol-induced DA release in the NAC [Fig. 4; F(1,9)=38.6, p<0.001] and approached a significant potentiation of haloperidol-induced DA release in the mPFC [Fig. 4; F(1,12)=5.26, p=0.068]. However, the 0.1 mg/kg haloperidol-induced DA release in the mPFC and NAC were significantly potentiated by the 1.0 mg/kg dose of SB242084 [Fig. 5; F(1,8)=38.9, p<0.001 in the mPFC and F(1,7)=52.3, p<0.001 in the NAC].
The effect of the 5-HT2C antagonist SB242084 (0.2 mg/kg, s.c.) on the D2 antagonist haloperidol (0.1 mg/kg, s.c.)-induced extracellular dopamine (DA) levels in the medial prefrontal cortex (mPFC) and nucleus accumbens (NAC). Rats were pretreated with haloperidol 30 min prior to administration of SB242084. Data are means±SEM of the dialysate DA levels, expressed as a percentage of each predrug baseline DA value (N=5–7). The arrows indicate drug injection times
The effect of the 5-HT2C antagonist SB242084 (1.0 mg/kg, s.c.) on the D2 antagonist haloperidol (0.1 mg/kg, s.c.)-induced extracellular dopamine (DA) levels in the medial prefrontal cortex (mPFC) and nucleus accumbens (NAC). Rats were pretreated with haloperidol 30 min prior to administration of SB242084. Data are means±SEM of the dialysate DA levels, expressed as a percentage of each predrug baseline DA value (N=5–7). The arrows indicate drug injection times
Effects of SB242084 on extracellular DA release in the mPFC and the NAC produced by the combination treatment of ACP-103 and haloperidol
As reported above, 3.0 mg/kg ACP-103 potentiated 0.1 mg/kg haloperidol-induced DA release in the mPFC (Fig. 2). To determine the influence of additional 5-HT2C antagonism on this effect of ACP-103, SB242084 (0.2 mg/kg) was injected 30 min after the simultaneous administration of ACP-103 (3.0 mg/kg) and haloperidol (0.1 mg/kg). This combination slightly increased the effect of ACP-103 and haloperidol in the mPFC, but the difference was not significant [Fig. 6; F(1,10)=3.09, p=0.11]. In the NAC, 3.0 mg/kg ACP-103 inhibited 0.1 mg/kg haloperidol-induced DA efflux (Fig. 2). However, the combination of haloperidol (0.1 mg/kg), SB242084 (0.2 mg/kg), and ACP-103 (3 mg/kg) significantly increased DA efflux in the NAC compared to the effect of haloperidol and vehicle injections [Fig. 6; F(1,8)=19.3, p<0.001] or to haloperidol and ACP-103 [F(1,8)=58.6, p<0.001].
The effect of the 5-HT2C antagonist SB242084 (0.2 mg/kg, s.c.) on extracellular dopamine (DA) levels in the medial prefrontal cortex (mPFC) and nucleus accumbens (NAC) produced by the combination treatment of D2 antagonist haloperidol (0.1 mg/kg, s.c.) and 5-HT2A/2C inverse agonist ACP-103 (3 mg/kg, s.c.). Rats were pretreated with ACP-103 and haloperidol 30 min prior to administration of SB242084. Data are means±SEM of the dialysate DA levels, expressed as a percentage of each predrug baseline DA value (N=5–7). The arrows indicate drug injection times
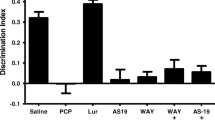
The comparison of the effects of ACP-103, M100907, SB242084, and SR46349-B alone and with low- and high-dose haloperidol on DA release in the mPFC and NAC are provided in Table 1.
Discussion
The main findings of the current study are that ACP-103 (10.0 mg/kg)significantly increased DA release in the mPFC but not in the NAC. Similar to previous studies from this laboratory with the 5-HT2A antagonist M100907 (Liégeois et al. 2002), the lower dose of ACP-103 (3.0 mg/kg) significantly potentiated 0.1 mg/kg haloperidol-induced DA release in the mPFC but inhibited haloperidol-induced DA release in the NAC. However, with the combination of the high dose (1.0 mg/kg) of haloperidol, ACP-103 (3 mg/kg), similar to previous studies using the 5-HT2A/2C antagonist SR46349-B, significantly potentiated haloperidol-induced DA release in both the mPFC and NAC. The effect of ACP-103 alone on DA release in the mPFC and NAC is identical to that of SR46349-B (Bonaccorso et al. 2002). However, SR46349-B also potentiated the effect of low-dose haloperidol-induced DA release in the NAC (Table 1; Bonaccorso et al. 2002). Thus, the effect on cortical and limbic DA release of the combination of ACP-103 and haloperidol is very similar to that of SR46349-B, with the exception of the effect on DA release in the NAC in the presence of a weak blockade of D2 receptors. Increasing DA release in the NAC might be expected to have important effects on reality testing and reward-dependent behavior, while increasing DA release in the cortex might be expected to improve cognition and, possibly, depression and negative symptoms. Thus, ACP-103, like SR46349-B, by itself can enhance DA release in the cortex at high doses and may have some value as monotherapy for some aspects of the schizophrenia syndrome. However, both drugs are more likely to be effective when combined with an APD which has D2 antagonist properties. If it is accepted that enhanced DA release in the NAC is undesirable, the most effective combination from this perspective would be low occupancy of D2 receptors along with ACP-103, which inhibited NAC DA release.
As the principle difference between ACP-103, M100907, and SR46349-B is in their affinities to 5-HT2C receptors relative to 5-HT2A receptors, it is possible to suggest that this ratio influences, to some extent, the interaction with haloperidol and its effect on D2 receptor blockade to affect DA release in the mPFC and NAC. M100907 is 160-fold selective for the 5-HT2A receptor, whereas SR46349-B has the strongest affinity for the 5-HT2C receptor relative to the 5-HT2A, being 8.2-fold more selective for the 5-HT2A receptor (Table 2). ACP-103 is intermediate, being 40-fold more selective for the 5-HT2A than for the 5-HT2C receptor (Table 2). This suggests that stronger 5-HT2C, relative to 5-HT2A, receptor blockade is more likely to enhance DA release in the NAC, and that addition of 5-HT2C receptor blockade can potentiate DA release in the mPFC at both low and high occupancy of D2 receptors. Consistent with this hypothesis, in the present study, we found that 5-HT2C antagonist SB242084 preferentially potentiated NAC DA release produced by haloperidol alone or the combination treatment with ACP-103 and haloperidol. The possible mechanisms that cause these effects are discussed below.
Effect of 5-HT2A/2C antagonists on cortical and NAC DA release
The potent 5-HT2A receptor antagonist M100907 alone, at doses of 0.1, 1.0, and 3.0 mg/kg, which potentiated haloperidol-induced DA release in the mPFC and NAC, did not increase DA release in the cortex or NAC (Bonaccorso et al. 2002). In addition, a very high dose of M100907, 10 mg/kg, also failed to increase DA release in this two regions (unpublished data). The doses of the selective 5-HT2C antagonist SB242084 tested here (0.2 and 1.0 mg/kg) did not increase DA release in either the cortex or the NAC. Spampinato and colleagues reported that SB242084, at doses of 1–10 mg/kg, produced a small, nondose-dependent increase (∼30%) in DA release in the STR and NAC, which were statistically significant in one study (De Deurwaerdere et al. 2004) but not in the other study (Navailles et al. 2004). Gobert et al. (2000) reported that 10 mg/kg SB242084, ten times higher than the doses studied in the present study, increased cortical DA release in the mPFC. However, 10 mg/kg SR46349-B and 10 mg/kg ACP-103, but not 3 mg/kg, alone significantly increased DA efflux in the mPFC but not the NAC. Thus, ACP-103 and SR46349-B increased cortical but not NAC DA efflux, maybe due to the blockade of combination of 5-HT2A and 5-HT2C receptors, which also, in the absence of a D2 receptor blockade, is capable of increasing DA release in the cortex more than the NAC. The basis for the increase in mPFC DA efflux produced in these agents is likely to be direct and indirect inhibition of VTA DA neurons through blockade of 5-HT2A receptors on VTA DA neuron perikarya and 5-HT2C receptors on inhibitory GABAergic interneurons. These effects would be expected on the subgroup of VTA neurons that project to the cortex but not to the limbic system, as neither compound had any effect on DA efflux in the NAC.
5-HT2C receptors are mainly located on GABAergic and glutamatergic neurons in the ventral tegmentum, substantia nigra, and prefrontal cortex (Pompeiano et al. 1994; Abramowski et al. 1995; Eberle-Wang et al. 1997; Clemett et al. 2000). More selective 5-HT2C receptor antagonists such as SB242084 and SB206553 increase the firing rate of DA neurons in the VTA (Prisco et al. 1994; Di Giovanni et al. 1999; Di Matteo et al. 1999) and increase DA overflow in the mPFC (Millan et al. 1998; Gobert et al. 2000). Local administration of the selective 5-HT2C receptor agonist, Ro 60-0175, into the VTA had no effect on basal DA level in the prefrontal cortex but completely antagonized the effect of stress on DA overflow. Administration of this compound directly into the mPFC had no significant effect on basal or stress-induced DA efflux (Pozzi et al. 2002). The 5-HT2C antagonist SB242084, given systemically increased basal extracellular DA, completely prevented the effect of intraventrotegmental Ro 06-0175 to block the effect of stress on cortical DA. These results suggest that stimulation of 5-HT2C receptor in the VTA tonically inhibit basal DA efflux in the mPFC, and that stimulation of 5-HT2C receptors can inhibit stimulated DA efflux. This is consistent with our findings that those drugs such as SR46349-B and ACP-103, which have relatively higher affinities to 5-HT2C receptors, have a greater ability to enhance cortical DA efflux than M100907, which is relatively weak in that regard. A series of studies has shown that SB206553, a selective 5-HT2C/2B receptor antagonist, increases the basal firing rate and the bursting activity of VTA DA-containing neurons (Di Giovanni et al. 1999) and enhances DA efflux in rat NAC and prefrontal cortex (Di Giovanni et al. 1999; Di Matteo et al. 1999; Gobert et al. 2000). Consistent with these findings, SB242084, the most potent and selective 5-HT2C receptor antagonist, selectively enhanced mesocorticolimbic DA function, whereas Ro 600175 and MK212, two 5-HT2C receptor agonists, reduced such activity (Pozzi et al. 2002; Di Matteo et al. 1999; Millan et al. 1998).
Interaction of 5-HT2A antagonists and haloperidol
We have previously reported that low-dose (0.1 mg/kg), but not high-dose (1.0 mg/kg), haloperidol slightly, but significantly, increases DA release in the mPFC, while both doses significantly increased DA release in the NAC (Liégeois et al. 2002), most likely due to its D2 receptor blockade. Like SR46349-B (1 and 3 mg/kg) and M100907 (0.1 mg/kg), ACP-103 (3 mg/kg) potentiated low-dose haloperidol (0.1 mg/kg)-induced DA release in the mPFC. These results suggest that this potentiation may be due to the combined effects of potent 5-HT2A and weak D2 receptor blockade. Many atypical APDs have been shown to have a higher affinity for 5-HT2A than D2 receptors in vitro (Meltzer et al. 1989; Schotte et al. 1996) and in vivo (Schotte et al. 1996; Stockmeier et al. 1993; Zhang and Bymaster 1999). This has been suggested to be a major factor in the ability of the atypical APDs to increase DA release in the mPFC and improve cognition (Meltzer and McGurk 1999). However, typical APDs, which are potent D2 receptor antagonists, do not, by themselves, increase DA release in the mPFC and also a have minor effect on negative symptom and cognition. The combination of any of the three 5-HT agents discussed here with low-dose haloperidol, which weakly occupies D2 receptors, potentiated DA release in the mPFC to a similar extent, suggesting that addition of 5-HT2A/2C receptor antagonism to typical neuroleptic drugs such as haloperidol or fluphenazine, which are relatively devoid of 5-HT2A receptor antagonism, may achieve at least some of the benefits of the atypical APDs on cognition. However, the dose of the typical neuroleptic drugs and the extent of D2 receptor blockade achieved can be critical since the data reported here indicates that in the mPFC, blockade of 5-HT2A receptors can lead to DA release, at least acutely, regardless of the extent of 5-HT2C receptor antagonism, only when D2 receptor occupancy is low. This was not found to be so when DA receptor blockade was more extensive, as is the case with current clinical practice with typical neuroleptic drugs (Farde et al. 1992).
Interaction of 5-HT2A/2C antagonists and haloperidol
Like M100907, but unlike SR46349-B, ACP-103 inhibited low-dose haloperidol-induced DA release in the NAC, which can be due to the greater selectivity of M100907 and ACP-103 for 5-HT2A receptors than for SR46349-B. The more potent 5-HT2C antagonism of SR46349-B may attribute greatly to the DA release in the NAC. Ritanserin, a 5-HT2A/2C antagonist with a potent affinity for 5-HT2C (Ki=2.7 nM) (Table 1), has also been reported to potentiate the ability of the D2/3 receptor antagonist raclopride to increase DA release in both the mPFC and NAC (Andersson et al. 1995). In the present study, 0.2 and 1.0 mg/kg SB242084 significantly potentiated haloperidol-induced DA release in the NAC, while only 1.0 mg/kg SB242084 potentiated DA release in the mPFC. In addition, 0.2 mg/kg SB242084 also reversed the inhibition of NAC DA release produced by the combination of 0.1 mg/kg haloperidol and ACP-103. However, adding additional 5-HT2C antagonism with SB242084 did not modify the potentiation of cortical DA release produced by haloperidol and ACP-103. Therefore, this may suggest that, in the presence of weak D2 blockade, 5-HT2A antagonism preferentially modify DA release in the mPFC, and 5-HT2C antagonism preferentially modify DA release in the NAC. These results also indicated that the effect of the combination of SB242084 with ACP-103, when combined to haloperidol, produced identical effects of SR46349-B. This further confirmed that the different effects produced by ACP-103 are due to its intermediate affinities for 5-HT2C receptors compared to M100907 and SR46349-B.
In conclusion, ACP-103 potentiated DA release in the mPFC and inhibited DA release in the NAC of haloperidol. It remains to be determined if ACP-103 and M100907 can be effective as monotherapy in some patients with psychosis or whether they can potentiate the effect of selective D2 antagonists, or even subtherapeutic doses of atypical APDs, especially those like risperidone and olanzapine which have high affinities for the D2 receptor. Overall, ACP-103 would appear to have a more desirable effect on DA release in the mPFC than SR46349-B or M100907 does either by itself or in combination with low or high doses of D2 antagonist.
References
Abramowski D, Rigo M, Duc D, Hoyer D, Staufenbiel M (1995) Localization of the 5-hydroxytryptamine2C receptor protein in human and rat brain using specific antisera. Neuropharmacology 34:1635–1645
Acadia Pharmaceuticals Inc. (2005) Acadia Pharmaceuticals announces encouraging interim results from ongoing phase II trial of ACP-103 for treatment-induced psychosis in patients with Parkinson's disease. PRNewswire-FirstCall, NY
Andersson JL, Nomikos GG, Marcus M, Hertel P, Mathe JM, Svensson TH (1995) Ritanserin potentiates the stimulatory effects of raclopride on neuronal activity and dopamine release selectivity in the mesolimbic dopaminergic system. Naunyn-Schmiedeberg's Arch Pharmacol 352:374–385
Bonaccorso S, Meltzer H, Li Z, Dai J, Alboszta A, Ichikawa J (2002) SR46349-B, a 5-HT(2A/2C) receptor antagonist, potentiates haloperidol-induced dopamine release in rat medial prefrontal cortex and nucleus accumbens. Neuropsychopharmacology 27:430–441
Canton H, Verriele L, Colpaert FC (1990) Binding of typical and atypical antipsychotics to 5-HT1C and 5-HT2 sites—clozapine potently interacts with 5-HT1C sites. Eur J Pharmacol 191:93–96
Clemett DA, Punhani T, Duxon MS, Blackburn TP, Fone KCF (2000) Immunohistochemical localisation of the 5-HT2C receptor protein in the rat CNS. Neuropharmacology 39:123–132
De Deurwaerdere P, Navailles S, Berg KA, Clarke WP, Spampinato U (2004) Constitutive activity of the serotonin2C receptor inhibits in vivo dopamine release in the rat striatum and nucleus accumbens. J Neurosci 24:3235–3241
Di Giovanni G, De Deurwaerdere P, Di Mascio M, Di Matteo V, Esposito E, Spampinato U (1999) Selective blockade of serotonin2C/2B receptors enhances mesolimbic and mesostriatal dopaminergic function: a combined in vivo electrophysiological and microdialysis study. Neuroscience 91:587–597
Di Matteo V, Di Giovanni G, Di Mascio M, Esposito E (1999) SB242084, a selective serotonin2C receptor antagonist, increases dopaminergic transmission in the mesolimbic system. Neuropharmacology 38:1195–1205
Eberle-Wang K, Mikeladze Z, Uryu K, Chesselet MF (1997) Pattern of expression of the serotonin2C receptor messenger RNA in the basal ganglia of adult rats. J Comp Neurol 384:233–247
Farde L, Nordstrom AL, Wiesel FA, Pauli S, Halldin C, Sedvall G (1992) Positron emission tomographic analysis of central D1 and D2 dopamine receptor occupancy in patients treated with classical neuroleptics and clozapine. Relation to extrapyramidal side effects. Arch Gen Psychiatry 49:538–544
Gobert A, Rivet JM, Lejeune F, Newman-Tancredi A, Adhumeau-Auclair A, Nicolas J, Cistarelli L, Melon C, Millan MJ (2000) Serotonin2C receptors tonically suppress the activity of mesocortical dopaminergic and adrenergic, but not serotonergic, pathways: a combined dialysis and electrophysiological analysis in the rat. Synapse 36:205–221
Herrick-Davis K, Grinde E, Teitler M (2000) Inverse agonist activity of atypical antipsychotic drugs at human 5-hydroxytryptamine2C receptors. J Pharmacol Exp Ther 295:226–232
Hutson PH, Barton CL, Jay M, Blurton P, Burkamp F, Clarkson R, Bristow LJ (2000) Activation of mesolimbic dopamine function by phencyclidine is enhanced by 5-HT2C/2B receptor antagonists: neurochemical and behavioural studies. Neuropharmacology 39:2318–2328
Ichikawa J, Meltzer HY (1999) Relationship between dopaminergic and serotonergic neuronal activity in the frontal cortex and the action of typical and atypical antipsychotic drugs. Eur Arch Psychiatry Clin Neurosci 249(Suppl 4):90–98
Ichikawa J, Ishii H, Bonaccorso S, Fowler WL, O'Laughlin IA, Meltzer HY (2001) 5-HT(2A) and D(2) receptor blockade increases cortical DA release via 5-HT(1A) receptor activation: a possible mechanism of atypical antipsychotic-induced cortical dopamine release. J Neurochem 76:1521–1531
Kennett GA, Wood MD, Bright F, Trail B, Riley G, Holland V, Avenell KY, Stean T, Upton N, Bromidge S, Forbes IT, Brown AM, Middlemiss DN, Blackburn TP (1997) SB 242084, a selective and brain penetrant 5-HT2C receptor antagonist. Neuropharmacology 36:609–620
Kuroki T, Meltzer HY, Icikawa J (1999) Effects of antipsychotic drugs on extracellular dopamine levels in rat medial prefrontal cortex and nucleus accumbens. J Pharmacol Exp Ther 288:774–781
Li Z, Ichikawa J, Dai J, Meltzer HY (2004) Aripiprazole, a novel antipsychotic drug, preferentially increases dopamine release in the prefrontal cortex and hippocampus in rat brain. Eur J Pharmacol 493:75–83
Liégeois JF, Ichikawa J, Meltzer HY (2002) 5-HT2A receptor antagonism potentates haloperidol-induced dopamine release in rat medial prefrontal cortex and inhibits that in the nucleus accumbens in a dose-dependent manner. Brain Res 947:157–162
Lucas G, De Deurwaerdere P, Caccia S, Spampinato U (2000) The effect of serotonergic agents on haloperidol-induced striatal dopamine release in vivo: opposite role of 5-HT(2A) and 5-HT(2C) receptor subtypes and significance of the haloperidol dose used. Neuropharmacology 39:1053–1063
Meltzer HY, McGurk SR (1999) The effects of clozapine, risperidone, and olanzapine on cognition in schizophrenia. Schizophr Bull 25:233–256
Meltzer HY, Matsubara S, Lee JC (1989) Classification of typical and atypical antipsychotic drugs on the basis of dopamine D-1, D-2 and serotonin2 pKi values. J Pharmacol Exp Ther 251:238–246
Meltzer HY, Arvanitis L, Bauer D, Rein W, Meta-Trial Study Group (2004) Placebo-controlled evaluation of four novel compounds for the treatment of schizophrenia and schizoaffective disorder. Am J Psychiatry 161:975–984
Millan MJ, Dekeyne A, Gobert A (1998) Serotonin (5-HT)2C receptors tonically inhibit dopamine (DA) and noradrenaline (NA), but not 5-HT, release in the frontal cortex in vivo. Neuropharmacology 37:953–955
Moghaddam B, Bunney BS (1990) Acute effects of typical and atypical antipsychotic drugs on the release of dopamine from prefrontal cortex, nucleus accumbens, and striatum of the rat: an in vivo microdialysis study. J Neurochem 54:1755–1760
Navailles S, De Deurwaerdere P, Porras G, Spampinato U (2004) In vivo evidence that 5-HT2C receptor antagonist but not agonist modulates cocaine-induced dopamine outflow in the rat nucleus accumbens and striatum. Neuropsychopharmacology 29:319–326
Paxinos G, Watson C (1998) The rat brain in stereotaxic coordinates. Academic, New York
Pehek EA (1996) Local infusion of the serotonin antagonists ritanserin or ICS 205,930 increases in vivo dopamine release in the rat medial prefrontal cortex. Synapse 24:12–18
Pompeiano M, Palacios JM, Mengod G (1994) Distribution of the serotonin 5-HT2 receptor family mRNAs: comparison between 5-HT2A and 5-HT2C receptors. Brain Res Mol Brain Res 23:163–178
Porras G, Di Matteo V, Fracasso C, Lucas G, De Deurwaerdere P, Caccia S, Esposito E, Spampinato U (2002) 5-HT2A and 5-HT2C/2B receptor subtypes modulate dopamine release induced in vivo by amphetamine and morphine in both the rat nucleus accumbens and striatum. Neuropsychopharmacology 26:311–324
Pozzi L, Acconcia S, Ceglia I, Invernizzi RW, Samanin R (2002) Stimulation of 5-hydroxytryptamine (5-HT(2C)) receptors in the ventrotegmental area inhibits stress-induced but not basal dopamine release in the rat prefrontal cortex. J Neurochem 82:93–100
Prisco S, Pagannone S, Esposito E (1994) Serotonin–dopamine interaction in the rat ventral tegmental area: an electrophysiological study in vivo. J Pharmacol Exp Ther 271:83–90
Roth BL, Ciaranello RD, Meltzer HY (1992) Binding of typical and atypical antipsychotic agents to transiently expressed 5-HT1C receptors. J Pharmacol Exp Ther 260:1361–1365
Schotte A, Janssen PF, Gommeren W, Luyten WH, Van Gompel P, Lesage AS, De Loore K, Leysen JE (1996) Risperidone compared with new and reference antipsychotic drugs: in vitro and in vivo receptor binding. Psychopharmacology (Berl) 124:57–73
Stockmeier CA, DiCarlo JJ, Zhang Y, Thompson P, Meltzer HY (1993) Characterization of typical and atypical antipsychotic drugs based on in vivo occupancy of serotonin2 and dopamine2 receptors. J Pharmacol Exp Ther 266:1374–1384
Vanover KE, Harvey SC, Son T, Bradley SR, Kold H, Makhay M, Veinbergs I, Spalding TA, Weiner DM, Andersson CM, Tolf BR, Brann MR, Hacksell U, Davis RE (2004) Pharmacological characterization of AC-90179 [2-(4-methoxyphenyl)-N-(4-methyl-benzyl)-N-(1-methyl-piperidin-4-yl)-acetamide hydrochloride]: a selective serotonin 2A receptor inverse agonist. J Pharmacol Exp Ther 310(3):943–951. DOI 10.1124/jpet.104.066688
Weiner DM, Burstein ES, Nash N, Croston GE, Currier EA, Vanover KE, Harvey SC, Donohue E, Hansen HC, Andersson CM, Spalding TA, Gibson DF, Krebs-Thomson K, Powell SB, Geyer MA, Hacksell U, Brann MR (2001) 5-hydroxytryptamine2A receptor inverse agonists as antipsychotics. J Pharmacol Exp Ther 299:268–276
Willins DL, Meltzer HY (1998) Serotonin 5-HT2C agonists selectively inhibit morphine-induced dopamine efflux in the nucleus accumbens. Brain Res 781:291–299
Zhang W, Bymaster FP (1999) The in vivo effects of olanzapine and other antipsychotic agents on receptor occupancy and antagonism of dopamine D1, D2, D3, 5HT2A and muscarinic receptors. Psychopharmacology (Berl) 141:267–278
Acknowledgements
Supported in part by a grant from Acadia Pharmaceuticals Inc.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, Z., Ichikawa, J., Huang, M. et al. ACP-103, a 5-HT2A/2C inverse agonist, potentiates haloperidol-induced dopamine release in rat medial prefrontal cortex and nucleus accumbens. Psychopharmacology 183, 144–153 (2005). https://doi.org/10.1007/s00213-005-0170-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-005-0170-9