Abstract
The effects of exercise in conjunction with weight-loss diets on bone health are mixed. Our objective was to systematically review and meta-analyze controlled clinical trials in adults investigating the addition of exercise to a weight-loss diet compared with a calorie-matched weight-loss diet without exercise on bone measures. Online databases including PubMed/MEDLINE, EMBASE, ISI (Web of Science), Scopus, and Google Scholar were searched up to April 2021 with no restriction. A random effects model was used to calculate the overall estimates. Quality of evidence was assessed using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology. Fourteen eligible controlled clinical trials were included in the systematic review. The meta-analysis revealed that, compared to weight-loss diets alone, the addition of exercise did not improve total body bone mineral density (BMD) [weighted mean difference (WMD) = 0.002 g/cm2, P = 0.62, n = 8], lumbar BMD (WMD = 0.007 g/cm2, P = 0.44, n = 9), total hip BMD (WMD = 0.015 g/cm2, P = 0.14, n = 4) and total bone mineral content (BMC) (WMD = − 11.97 g, P = 0.29, n = 7). Subgroup analysis revealed that resistance exercise in conjunction with hypocaloric diets positively affects total BMD compared to an energy restrictive diet alone (WMD = 0.01 g/cm2, P = 0.003, n = 3). Overall, it appears that only resistance exercise beneficially affects total BMD during a calorie-restricted diet in adults. Further well-controlled and long-term clinical trials are still needed to confirm these results. PROSPERO registration number: CRD42020173434.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The global prevalence of overweight and obesity is on a constant rise. Epidemiological studies have demonstrated that obesity increases the risk of metabolic, cardiovascular, and musculoskeletal diseases, considerably. Moreover, obesity has also been associated with decreased life expectancy and quality of life [1]. A calorie-restricted diet is the most commonly prescribed lifestyle intervention for weight loss in adults. Dietary calorie restriction reduces body weight as well as the risk of several chronic diseases. Nevertheless, the catabolic state caused by calorie restriction could have functional and physiological effects via changes in the metabolism of fat and other tissues such as the skeletal muscle, liver, and heart [2]. Skeletal muscle mass might be reduced during a calorie-restricted diet which in turn decreases muscle strength and bone mass [3]. Although weight-loss diets might improve metabolic health in obese adults, it can be accompanied by a loss in bone mineral density (BMD) [4].
In general, diet and exercise are known to alter body composition and bone mineral density. Previous investigations reported that the addition of exercise to a weight-loss diet can attenuate the effects of BMD loss due to weight loss [5, 6]. Some studies revealed that exercise training may prevent bone loss during weight loss in older adults [7, 8]. Moreover, several studies reported that regular weight-bearing or/and resistance training can preserve bone during calorie-restricted weight loss [9, 10]. In this line, Serra et al. [11] showed that the addition of aerobic exercise to weight loss tends to attenuate the reductions in femoral neck BMD in African American and Caucasian postmenopausal women. In addition, Villareal et al. [6] suggested that BMD of the hip might be attenuated in a weight-loss diet plus exercise group than in the weight-loss diet alone group. In contrast, Beavers et al. [12] reported that exercise training did not attenuate weight loss-associated reductions in BMD in overweight and obese older adults with osteoarthritis. We are aware of a systematic review and meta-analysis performed by Yarizadeh et al. [13], which compared the effect of exercise plus low-calorie diets with low-calorie diets alone on bone status. However, they included studies in which caloric restriction was different between intervention and control groups [14, 15]. They also failed to include several relevant randomized controlled trials (RCTs) [11, 16,17,18,19,20,21]; therefore, their results might be biased.
Given that there is a concern regarding the unfavorable effects of adherence to a calorie-restricted diet alone on bone health measures and the contradictory results of previous studies regarding the effects of adding exercise to weight-loss diets, we conducted a systematic review and meta-analysis determining the effect of weight-loss diet plus exercise on bone mass in overweight and obese adults.
Methods
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement was followed for reporting this systematic review and meta-analysis. The study protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) database in April 2020, with the registration code CRD42020173434 and also reported in detail elsewhere [22].
Search strategy
A systematic literature search was conducted in PubMed/MEDLINE, EMBASE, ISI (Web of Science), Scopus, and Google Scholar up to April 2021, using the following Medical Subject Headings (MeSH) and non-MeSH keywords: (1) nutrition, nutrition therapy, caloric restriction, weight-reducing, diet*, hypo-caloric; (2) exercise, physical activity, training, physical fitness; (3) intervention, controlled trial, randomized, random*, randomly, placebo, assignment, clinical trial, trial. The full list of keywords and search strategies for each database are provided in Supplementary Table 1. No language, publication date, or any other restrictions were applied while searching databases. To locate unpublished studies, pre-print indexing websites (e.g., https://www.researchsquare.com/) and the registered clinical trials approved by the World Health Organization (WHO) were investigated.
Eligibility criteria
Studies with the following criteria were included in this review: original articles (1) with a controlled clinical trial design (either parallel or cross-over); (2) conducted on overweight or obese adults (≥ 18 years of age, and BMI ≥ 25 kg/m2); (3) assessed the effect of a weight-loss diet combined with exercise in comparison with a weight-loss diet alone on bone mass, while the energy restriction of diets was the same in both groups. Studies were excluded if (1) they were conducted in pregnant or lactating women, (2) their intervention period was short (< 2 weeks), or (3) reported duplicate data.
Data extraction
Six researchers (Z.Y, S.S, S.B, SH.R, S.MT, and T.Z) independently screened and cross-checked the titles and abstracts as well as final full-text screening to find the relevant articles based on the inclusion and exclusion criteria. Data were extracted independently by 2 investigators (ZY and SB) from eligible studies: publication details (first author’s last name, publication year, and country), participants’ characteristics (number, age, gender, and health status), study characteristics (number of study arms, duration of intervention, type of the weight-loss diet, the amount of calorie restriction, and exercise plan), and mean and standard deviation (SD) of desired outcomes. These included total, lumbar and hip BMD, total BMC obtained at baseline, post-intervention, and their change from the baseline, including where possible, P-values for within-group and between-group comparison. Discrepancies were resolved by discussion and consensus with the senior author (ASA).
Quality assessment
The Cochrane collaboration’s tool was used to examine the quality of the eligible studies based on 7 domains: (1) random sequence generation (selection bias), (2) allocation concealment (selection bias), (3) blinding of participants and personnel (performance bias), (4) blinding of outcome assessment (detection bias), (5) incomplete outcome data (attrition bias), (6) selective outcome reporting (reporting bias), and (7) compliance to the diet as another possible source of bias. Each domain was judged as “low risk of bias,” “high risk of bias,” or “unclear risk of bias.” Since blindness is not possible for studies that examine the effects of diet and exercise, the blinding of participants, personnel, and reviewers was not considered as a major factor in assessing the risk of bias. Finally, the overall quality of each eligible trial was categorized as “low risk” (“low risk” for all key domains), “unclear risk” (“unclear risk of bias” in 1 or more domains), and “high risk” (“high risk” for 1 or more domains). Furthermore, the non-randomized trials were evaluated using risk of bias in non-randomized studies of interventions (ROBINS-I) tool [23]. The factors contributing to study quality were 7 domains ( confounding factors, selection of participants, interventions classification, deviations from intended interventions, missing data, outcomes measurement, and selective reporting) and overall risk of bias was reported as low, moderate, serious, critical, or no information.
Quality of evidence
The quality assessment of evidence for each outcome was assessed by the GRADE (Grading of Recommendations Assessment, Development, and Evaluation) approach, based on the following domains: risk of bias, publication bias, imprecision of results, heterogeneity, and indirectness of evidence [24]. Eventually, quality of evidence was classified as high, moderate, low, and very low.
Statistical analysis
The mean change in outcome variables and their corresponding standard deviations (SDs) were extracted from each study arm to calculate the mean difference of changes and its standard error (SE) to be used as effect size for meta-analyses. Since, change values were not reported in eligible studies, they were calculated by using 0.5 as the correlation coefficient between baseline and follow-up values. To ensure the meta-analysis was not sensitive to the selected correlation coefficient, all analysis were repeated using correlation coefficients of 0.2 and 0.8. The DerSimonian and Laird random‐effects model, which considers the between-study variability, was used to calculate the weighted mean difference (WMD) and its corresponding 95% CIs (confidence intervals). The heterogeneity between studies was assessed using Cochran’s Q test and the I-squared (I2) statistic. To explore the potential sources of heterogeneity, several subgroup analyses were performed based on gender (female/both), menopausal status (both men and women/postmenopausal /premenopausal), exercise type (aerobic/resistance/both), ingestion of vitamins or mineral supplements (yes/no), and diet type [low calorie (800–1200)/moderate low calorie (≥ 1200)]. As a complete bone remodeling cycle takes 3–4 months to occur [25], the study duration of ≤ 16–weeks and > 16 weeks was defined as short and long term, respectively for subgroup analysis. Sensitivity analysis was conducted to explore whether the overall effects depended on a specific study. In addition, sensitivity analyses were carried out by excluding the studies with ≤ 16 weeks to further confirm the robustness of the findings. Publication bias was assessed by visual inspection for asymmetry of the funnel plot since there were fewer than 10 studies in the meta-analysis. All analyses were performed using STATA, version 11.2 (Stata Corp, College Station, TX, USA), and P < 0.05 was considered statistically significant.
Results
Study selection and characteristics
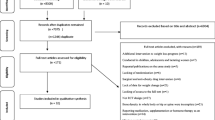
As shown in Fig. 1, 42,189 publications were retrieved by searching the electronic databases and 36,582 articles remained following the removal of duplicates. The screening of titles/abstracts resulted in 469 papers that had full texts assessed for further consideration. Of these, 455 articles were excluded because of the following reasons: (1) 119 articles were repeated publications on the same study population, (2) we could not access the full text of 17 studies even after contacting the authors, (3) 31 studies did not provide an equal calorie restriction in diet alone and diet plus exercise groups, (4) 155 studies did not consider the selected outcome variable, (5) 1 study presented data after a follow-up period and another study did not have adequate data to calculate changes. Seventy-six trials did not report any weight-loss program and 55 other articles were excluded due other reasons (letters to the editor, conducted in pregnant and lactating women, participants < 18 years old). Finally, fourteen eligible controlled clinical trials were included in the current systematic review and meta-analysis [6, 9,10,11, 16,17,18,19,20,21, 26,27,28,29].
Study and participant characteristics
The included investigations were published between 1997 and 2018. Eight eligible articles were published in the USA [6, 11, 17, 21, 26,27,28,29], one in Canada [20], Egypt [10], Brazil [16], and three in Asian countries [9, 18, 19]. All studies used a parallel design and the intervention duration ranged from 12 to 36 weeks. Most studies were conducted on females, except 3 studies which included both genders [6, 16, 29], and the participants were aged 30–80 years. Eight trials were conducted among postmenopausal women [6, 11, 16, 20, 21, 27,28,29], 3 trials included premenopausal participants [9, 10, 17] and pre-and post-menopausal women [18, 19, 26]. Moreover, the health status of participants was as follows: healthy overweight and/or obese individuals [9, 10, 17,18,19,20,21, 26, 27], patients with T2DM [16], healthy and individuals with stable hyperlipidemia and hypertension [11, 28], healthy and subjects with stable medication [6], and overweight/obese with cardiometabolic disease or metabolic syndrome [29]. With regard to the exercise protocol, 7 studies utilized aerobic exercise [10, 11, 16, 19, 27,28,29], 6 investigations assessed the effects of resistance exercise [9, 17, 19, 20, 26, 29], and 3 studies examined the effects of aerobic and resistance exercise together [6, 18, 21]. Low-calorie diets (800–1200 kcal/day) were presented as the intervention in 3 studies [9, 18, 26], and the other included studies recommended moderate low-calorie diets (≥ 1200 kcal/day) [6, 10, 11, 16, 17, 19,20,21, 27,28,29]. The characteristics of the included studies are listed in Table 1.
Risk of bias assessment and the quality of evidence
A summary of the risk of bias assessment for included studies is reported in Table 2. All studies except one (Silverman et al. [28]) expressed that the participants were randomized, but a number of studies mentioned the usage of the random sequence generation method [6, 17, 29]. There was no report of allocation concealment except in one study [6], and 4 studies were considered to be at low risk of bias for blinding of outcome assessment [6, 26, 27, 29]. None of the included trials described a method for blinding participants or personnel. No indication of selective reporting and incomplete outcome data [apart from the study of Serra et al. [11]] was observed in all the included studies. The majority of included trials described the methods that were used for dietary compliance assessment, so they were regarded as low risk [6, 9, 11, 17,18,19,20,21, 26,27,28,29]. According to the Robins-I tool, the study done by Silverman et al. [28] was considered as low risk of bias in all domains.
Moreover, with regard to the quality of evidence, the application of the GRADE system showed a low certainty for total BMD, hip BMD, total BMC, and a moderate level of certainty for lumbar BMD (Supplemental Table 2).
Meta-analysis
Total bone mineral density
The analysis of 8 controlled clinical trials with 9 treatment arms (n = 328) [6, 9, 16, 18, 19, 21, 26, 27] revealed that low calorie diets plus exercise had no significant additive effect on total bone mineral density (total BMD) (WMD = 0.002 g/cm2, 95% CI − 0.007, 0.012, P = 0.62) compared to diet-induced weight loss alone. The between-study heterogeneity was shown to be moderate (Cochran’s Q test, Q statistic = 15.75, P = 0.046, I2 = 49.20%).
As illustrated in Table 3, the subgroup analysis revealed that total BMD was significantly improved in participants who had resistance exercise during diet-induced weight loss when compared to those who went on an energy-restrictive diet without exercise (WMD = 0.01 g/cm2, 95% CI 0.003, 0.016, P = 0.003) and no heterogeneity was seen between included studies (Cochran’s Q test, Q statistic = 0.23, P = 0.88, I2 = 0%). The subgroup analysis showed that study duration, diet type, and taking vitamin or mineral supplements were potential sources of heterogeneity. In addition, significant alterations were not observed in the analysis for studies with vitamin or mineral supplement intake (WMD = 0.003 g/cm2, 95% CI − 0.009, 0.015, P = 0.64). Moreover, no significant effect on total BMD was observed in both subgroups of duration.
Lumbar bone mineral density
Nine studies [6, 9,10,11, 19, 26,27,28,29] assessed the effects of exercise and low-calorie diets compared with low-calorie diets alone on lumbar bone mineral density (lumbar BMD) (562 participants). According to the pooled analysis, weight-loss diets in conjunction with exercise had no significant positive effect on lumbar BMD in comparison with weight-loss diets alone (WMD = 0.007; 95% CI − 0.011, 0.025 g/cm2, P = 0.44) and the between-study heterogeneity was high (Q statistic = 24.86, P = 0.002, I2 = 67.80%, Table 3). Similar results were obtained when studies with a duration of ≤ 16 weeks [9, 10] were removed. After performing subgroup analysis, no significant relationship was detected based on any of the variables. However, the heterogeneity between studies was explained by the subgroup analysis according to menopausal status, diet, and exercise type.
Hip bone mineral density
Meta-analysis of 4 trials (n = 295) [6, 10, 19, 29] reported that a combination of calorie restriction and exercise did not significantly affect hip bone mineral density (hip BMD) (WMD = 0.015 g/cm2, 95% CI − 0.005, 0.036, P = 0.14), with high between-study heterogeneity (Q statistic = 12.50, P = 0.006, I2 = 76.00%, Table 3). The exclusion of a study with a duration of ≤ 16 weeks [10] did not significantly alter the result.
Total bone mineral content
Seven trials with 8 treatment arms (n = 320) provided information on changes in total bone mineral content (total BMC) following exercise and calorie restriction and calorie restriction alone [9, 17,18,19,20, 26, 27]. As shown in Table 3, the addition of exercise to a weight-loss program does not significantly affect BMC (WMD = − 11.97 g, 95% CI − 34.21, 10.27, P = 0.29). It is also worth pointing out that no evidence of between-study heterogeneity was detected (Q statistic = 4.02, P = 0.77, I2 = 0%). Subgroup analysis was performed based on the studies’ duration and menopausal status so that the intervention period and menopausal status did not modify the effects of exercise in conjunction with weight-loss diets.
Sensitivity analysis and publication bias
Sensitivity analysis indicated that omitting a study done by Nakata et al. [18] changed the overall effect of low calorie diet plus exercise on total BMD to a statistically significant increase (WMD = 0.008 g/cm2, 95% CI 0.002, 0.013). None of the other pooled effects were sensitive to the included studies.
There was no evidence of publication bias in the meta-analysis of low-calorie diet plus exercise on bone mineral density and content according to visual inspection for asymmetry of the funnel plots (Fig. 2).
Begg’s funnel plots (with pseudo 95% CIs) depicting the effect sizes (difference in means) versus their standard errors (SEs) for controlled trials that assessed the effects of exercise plus a weight-loss diet compared with a weight-loss diet alone on total BMD (A), lumbar BMD (B), hip BMD (C), and total BMC (D)
Discussion
The findings of the current systematic review and meta-analysis revealed that BMD of the total body, lumbar, and hip did not significantly change following exercise plus caloric restriction compared to an iso-energetic hypocaloric diet alone. However, total BMD was greater following the addition of resistance exercise to a calorie-restriction program compared with those who were under conditions of similar calorie restriction without exercise. Low-calorie diets plus exercise failed to generate significant changes in total BMC when compared with the same hypocaloric diets.
A previously published meta-analysis demonstrated that diet-induced weight loss might not significantly affect the lumbar spine and whole-body BMD, while total hip BMD was decreased [30]. The results of a further meta-analysis showed that exercise combined with calorie restriction led to a reduction in hip and an increased total BMD but not in lumbar BMD, compared with a control group [31]. Also, the results of a systematic review and meta-analysis revealed that different types of exercise have a favorable effect on BMD in postmenopausal women [32]. In addition, a meta-analysis conducted by Soltani et al. reported that exercise-induced weight loss in adults had an increasing effect on hip and lumbar spine BMD without affecting total BMD [31] compared to a control group (without any intervention). The mechanisms underlying the alteration in bone mass during weight loss have not been fully elucidated. Some evidence has shown that weight reduction might improve bone mass through increasing serum 25(OH) D and this may be due to its release from adipose tissue [33]. Moreover, ghrelin, a major regulator of appetite, increases in response to weight loss and modulates the proliferation and differentiation of osteoblasts [34]. The incretin hormones, GLP-1 (glucagon-like peptide-1), and gastric inhibitory polypeptide appear to have an anabolic effect on bone which are increased with weight loss [35]. Additionally, elevated adiponectin with weight loss, might lead to suppressing the osteoclast number and activating the osteoblastogenesis [36]. In general, there is no obvious link between the changes in gut peptides during caloric restriction and its effects on bone metabolism and its loss [37]. In contrast, some studies have proposed that reducing adiposity during weight loss could lead to a decreased circulating estrogen and other sex hormones [38]. These changes negatively influence bone osteoblasts [39], and in addition, calorie restriction may diminish calcium absorption efficiency [40]. This could occur in several ways, for example, through reducing estrogen levels, a rise in cortisol levels, and/or high serum PTH following weight reduction [41]. Overall, the interplay between hormones, cytokines, and growth factors and their influences on calcium absorption and bone during calorie restriction are multifaceted, and this can be affected by other factors including the diet duration, amount of weight loss, ethnicity, age, and gender [37].
Exercise is recognized as having favorable effects on bone mineral composition [31, 32]; however, findings are contradictory regarding whether exercise incorporated into a hypocaloric diet can be more beneficial against bone loss. The conclusion of the present study indicated that adding resistance exercise to an energy-restricted diet has a positive effect on total BMD. Since increasing muscle strength is related to enhancement of bone mass, it is proposed that osteogenesis is stimulated in response to muscle contraction. Thus, the main mechanism facilitating resistance training and effects on osteogenic development is the action of muscle via the force of muscular contraction at the site of attachment of the tendon area on the bone [42]. Another mechanism that might explain the positive effects of the addition of resistance exercise to weight loss on BMD is the increment in lean mass which increases growth factors levels such as IGF-1 [43]. Exercise seems to establish a further stimulus for decreasing fat mass when incorporated with the dietary intervention [19]. It is postulated that weight-loss diets combined with exercise may help attenuate some of the factors involved in bone loss inclusive of increments in IGF-1, and a decline in systemic inflammation [28]. Exercise during weight loss could improve physical function that is just as important as increasing BMD to prevent fractures [6, 37]. Nevertheless, we observed that the overall mean difference for BMD and BMC between dietary restriction incorporated with exercise and dietary restriction alone were non-significant. Our meta-analysis found no obvious differences in effectiveness between low-calorie diets in conjunction with exercise and low-calorie diets alone. This may reflect that a number of factors such as the difference in the types of exercise programs, duration and intensity of exercise, type of diet, and the amount of calorie restriction were heterogeneous between studies. It is noteworthy that, there were discrepancies regarding the compliance and dropout rates between studies. In addition, it is suggested that an exercise program may have different effects on individuals with diverse physical activity levels. It is also conceivable that the influence of exercise on bone mass differs between races [44]. Considering the factors mentioned previously, it seems that more studies are needed to arrive at a firm conclusion. It is worth noting that exercise and weight loss are low-cost non-pharmacological approaches that are available to the public. Exercise and weight loss can improve obesity-related medical complications, physiological and psychological performance [6] and this approach has health benefits beyond the skeleton.
It appears that a very low or low-calorie diet versus moderate energy restriction causes more reductions in BMD and increases in bone turnover. This is because severe energy restriction results in greater weight-loss diets than moderate energy restriction, which might cause more mechanical unloading of bone and thus greater bone loss [45, 46]. However, our subgroup analysis (based on the amount of calorie restriction) did not provide any difference regarding the effect of exercise when added to low-calorie or very-low-calorie diets. This highlights the need for further investigation into the role of various diet types on the bone at different ages, as well as the interaction of different types of exercise with them.
A systematic review by Yarizadeh et al. [13] concluded that physical training significantly affects total BMC, hip BMD during weight reduction, whereas our study could not confirm these findings. Two duplicated studies [Shah et al. [5] and Villareal et al. [6], and several publications with the same data] were included in the meta-analysis done by Yarizadeh et al. [13]; furthermore, they included a study completed by Daly et al. [47] in which the weight-loss group participated in stationary cycling and a series of static stretching exercises. Additionally, follow-up data of Shah et al. [5], Villareal et al. [6], and Beavers et al. [12] including the weight maintenance phase of the studies had been considered in the mentioned meta-analysis, while the aim of the study was to assess the effect of exercise-calorie restriction compared to energy restriction and only before and after intervention period data should be extracted. It should be noted that Svendsen et al. [48] expressed their results as percentages and could not be entered into the meta-analysis. The previous meta-analysis also included 2 studies [14, 15] in which energy restriction was not the same in the 2 intervention groups. Furthermore, they listed non-randomized controlled trials as exclusion criteria, whereas the study done by Silverman et al. [28] did not meet this condition and was included in their meta-analysis. These may explain the differences in our findings. It is important to note that a number of controlled clinical trials [11, 16,17,18,19,20,21] were not considered in the previous review. Therefore, their results might be biased. The present systematic review was undertaken to detect the maximum number of controlled clinical trials. The current study provides evidence that adding exercise to a weight-loss regimen does not positively affect total and lumbar BMD, which is in agreement with the results of the recent meta‐analysis done by Yarizadeh et al. [13].
All included studies used dual-energy X-ray absorptiometry (DXA) to measure bone mass. DXA (a two-dimensional technique) has some inherent limitations. This method cannot distinguish between cortical and trabecular bone and also between changes that are caused owing to bone geometry and those actually due to BMD alterations. Moreover, it cannot provide information on microstructural characteristics, which is the main determinant of bone strength. It is likely that excess fat tissue surrounding the bone in subjects with obesity could lead to DXA measurement errors for BMD [49, 50]. In addition to DXA, there are three-dimensional image processing such as peripheral quantitative computed tomography (pQCT), high-resolution pQCT (HR-pQCT), and magnetic resonance imaging (MRI) that can be used to characterize bone quality and strength The peripheral quantitative computed tomography has been applied to assess BMD, bone strength (along the length of long bones), bone cross-sectional geometry, and to provide insight into muscle and fat parameters; however, its resolution does not provide quantification of bone microarchitecture. The dominant advantage of the HR-pQCT technique is the possibility of examining cancellous bone from cortical bone separately and estimating bone strength through finite element analysis [51]. As compared to the aforementioned methods, MRI presents a feasible technique for assessing bone quality; however, less precision and reproducibility limit its potential to be used as a valid diagnostic technique [52]. Recently, it has been reported that elevated bone marrow adipose tissue and fatty infiltration of muscular tissue might play a role in the pathogenesis of osteoporosis or sarcopenia. They are related to age and body composition. These novel imaging biomarkers can be measured by regional magnetic resonance spectroscopy (MRS). There is evidence that physical activity can control the extent of bone marrow adipose tissue [53,54,55]. Therefore, it is suggested that future RCTs use advanced imaging modalities to investigate the role of resistance/impact exercise in preserving bone/muscle structure and bone marrow/muscle fat during a hypocaloric diet.
The present study has several strengths. It was undertaken based on a comprehensive search to identify all relevant literature and no evidence of publication bias was detected. Moreover, the degree of adherence to the intervention has been considered in most included studies with the exception of 2 studies [10, 16]. The exercise training was supervised in all studies except Silverman et al. [28]. Furthermore, the overall quality of evidence of every outcome was evaluated using the GRADE system. All studies reported menopausal status; therefore, we assessed the effect on BMD based on menopause status but the number of articles in this field was limited. Our findings have several limitations that are worthy of consideration: (i) as hormone therapy could attenuate bone loss, some included studies did not take this variable into account as an exclusion criterion and the duration of some included studies was short that may underestimate the effect of the treatment, (ii) there is heterogeneity between the included studies which assessed the effect on BMD that may have been affected by the variations in exercise intensity and program, amount of calorie restriction, and the composition of the diet, (iii) a limited number of studies were conducted on some of the bone outcomes such as hip BMD which led to inconclusive results; thus, more high-quality clinical studies are required to reach a more reliable result regarding the effect of a hypocaloric diet with and without exercise on bone mass, (iv) studies done by Miller et al. and St-Onge et al. [17, 20] examined only BMC while BMD measurement is useful for predicting fracture risk in adults [56]. All relevant studies except the one conducted by Silverman et al. [28] were RCTs; however, based on the risk of bias assessment, all of them except two [6, 28] were judged to be “unclear,” which means that additional studies are still needed to increase the confidence in the estimated effects. In addition, since blinding is not feasible for the trials which assess the effect of dietary and exercise interventions, it is possible that this may have influenced the quality of the studies. It is worth noting that lumbar spine BMD is not a reliable marker compared to the hip or femoral neck BMD due to scoliosis/stenosis, especially in older populations [57].
Regarding the limitations mentioned above, the interpretation of results should be viewed with caution and more high-quality RCTs are recommended to help inform evidence-based decisions.
Conclusion
In summary, the findings of the present systematic review and meta-analysis showed that adding exercise to a weight-loss regimen does not have a positive effect on bone mineral density and content in comparison to a weight-loss diet alone. However, the addition of resistance exercise to a weight-loss diet led to an improved total BMD. Further high-quality controlled clinical trials are still needed to confirm the findings presented here.
Data availability
All generated or analyzed data are included in this article, its supplementary file, and protocol [22].
Abbreviations
- BMD:
-
Bone mineral density
- BMC:
-
Bone mineral content
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROSPERO:
-
Prospective Register of Systematic Reviews
- MeSH:
-
Medical Subject Headings
- WHO:
-
World Health Organization
- BMI:
-
Body mass index
- SD:
-
Standard deviation
- GRADE:
-
Grading of Recommendations Assessment, Development and Evaluation
- SE:
-
Standard error
- WMD:
-
Weighted mean difference
- CIs:
-
Confidence intervals
- I2 :
-
I-squared
References
Bray G, Kim K, Wilding J, Federation WO (2017) Obesity: a chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obes Rev 18:715–723
Bosy-Westphal A, Kossel E, Goele K, Later W, Hitze B, Settler U, Heller M, Glüer C-C, Heymsfield SB, Müller MJ (2009) Contribution of individual organ mass loss to weight loss–associated decline in resting energy expenditure. Am J Clin Nutr 90:993–1001
Compston J, Laskey M, Croucher P, Coxon A, Kreitzman S (1992) Effect of diet-induced weight loss on total body bone mass. Clin Sci 82:429–432
Villareal DT, Apovian CM, Kushner RF, Klein S (2005) Obesity in older adults: technical review and position statement of the American Society for Nutrition and NAASO, The Obesity Society. Am J Clin Nutr 82:923–934
Shah K, Armamento-Villareal R, Parimi N, Chode S, Sinacore DR, Hilton TN, Napoli N, Qualls C, Villareal DT (2011) Exercise training in obese older adults prevents increase in bone turnover and attenuates decrease in hip bone mineral density induced by weight loss despite decline in bone-active hormones. J Bone Miner Res 26:2851–2859
Villareal DT, Chode S, Parimi N, Sinacore DR, Hilton T, Armamento-Villareal R, Napoli N, Qualls C, Shah K (2011) Weight loss, exercise, or both and physical function in obese older adults. N Engl J Med 364:1218–1229
Bolam KA, van Uffelen JG, Taaffe DR (2013) The effect of physical exercise on bone density in middle-aged and older men: a systematic review. Osteoporos Int 24:2749–2762
Martyn-St James M, Carroll S (2006) High-intensity resistance training and postmenopausal bone loss: a meta-analysis. Osteoporos Int 17:1225–1240
Nakata Y, Ohkawara K, Lee DJ, Okura T, Tanaka K (2008) Effects of additional resistance training during diet-induced weight loss on bone mineral density in overweight premenopausal women. J Bone Miner Metab 26:172–177
Hosny IA, Elghawabi HS, Younan WBF, Sabbour AA, Gobrial MAM (2012) Beneficial impact of aerobic exercises on bone mineral density in obese premenopausal women under caloric restriction. Skeletal Radiol 41:423–427
Serra M, Blumenthal J, Ryan A (2013) Impact of weight loss and aerobic exercise on nutrition and bone mineral density in African American and Caucasian postmenopausal women. J Aging Res Clin Pract 2:11–16
Beavers DP, Beavers KM, Loeser RF, Walton NR, Lyles MF, Nicklas BJ, Shapses SA, Newman JJ, Messier SP (2014) The independent and combined effects of intensive weight loss and exercise training on bone mineral density in overweight and obese older adults with osteoarthritis. Osteoarthritis Cartilage 22:726–733
Yarizadeh H, Asadi S, Baharlooi H, Setayesh L, Kakavandi NR, Hambly C, Djafarian K, Mirzaei K (2020) Beneficial impact of exercise on bone mass in individuals under calorie restriction: a systematic review and meta-analysis of randomized clinical trials. Crit Rev Food Sci Nutr 61:553–565
Weiss EP, Jordan RC, Frese EM, Albert SG, Villareal DT (2017) Effects of weight loss on lean mass, strength, bone, and aerobic capacity. Med Sci Sports Exerc 49:206–217
Redman LM, Rood J, Anton SD, Champagne C, Smith SR, Ravussin E (2008) Calorie restriction and bone health in young, overweight individuals. Arch Intern Med 168:1859–1866
de Sousa MV, Fukui R, Krustrup P, Pereira R, Silva P, Rodrigues A, de Andrade J, Hernandez A, da Silva MR (2014) Positive effects of football on fitness, lipid profile, and insulin resistance in B razilian patients with type 2 diabetes. Scand J Med Sci Sports 24:57–65
Miller T, Mull S, Aragon AA, Krieger J, Schoenfeld BJ (2018) Resistance training combined with diet decreases body fat while preserving lean mass independent of resting metabolic rate: a randomized trial. Int J Sport Nutr Exerc Metab 28:46–54
Nakata Y, Tanaka K, Shigematsu R, Amagai H, Suzuki T (2002) Effects of change in body mass and body composition during body mass reduction on bone mass in obese middle-aged women. Jpn J Phys Fitness Sports Med 51:129–137
Nam S-s, Sunoo S, Park H-y, Moon H-w (2016) The effects of long-term whole-body vibration and aerobic exercise on body composition and bone mineral density in obese middle-aged women. J Exerc Nutr Biochem 20:19–27
St-Onge M, Rabasa-Lhoret R, Strychar I, Faraj M, Doucet É, Lavoie J-M (2013) Impact of energy restriction with or without resistance training on energy metabolism in overweight and obese postmenopausal women: a Montreal Ottawa New Emerging Team group study. Menopause 20:194–201
Thompson JL, Gylfadottir UK, Moynihan S, Jensen CD, Butterfield GE (1997) Effects of diet and exercise on energy expenditure in postmenopausal women. Am J Clin Nutr 66:867–873
Beigrezaei S, Yazdanpanah Z, Soltani S, Rajaie SH, Mohseni-Takalloo S, Zohrabi T, Kaviani M, Forbes SC, Baker JS, Salehi-Abargouei A (2021) The effects of exercise and low-calorie diets compared with low-calorie diets alone on health: a protocol for systematic reviews and meta-analyses of controlled clinical trials. Syst Rev 10:1–6
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:1–7
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H (2011) GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 64:383–394
MUNDY GR, (1999) Bone remodeling. In: Favus MJ (ed) Primer on the metabolic bone diseases and disorders of mineral metabolism. Lippincott Williams & Wilkins, Philadelphia, pp 30–38
Andersen RE, Wadden TA, Herzog RJ (1997) Changes in bone mineral content in obese dieting women. Met Clin and Exp 46:857–861
Ryan AS, Nicklas BJ, Dennis KE (1998) Aerobic exercise maintains regional bone mineral density during weight loss in postmenopausal women. J Appl Physiol 84:1305–1310
Silverman NE, Nicklas BJ, Ryan AS (2009) Addition of aerobic exercise to a weight loss program increases BMD, with an associated reduction in inflammation in overweight postmenopausal women. Calcif Tissue Int 84:257–265
Beavers KM, Walkup MP, Weaver AA, Lenchik L, Kritchevsky SB, Nicklas BJ, Ambrosius WT, Stitzel JD, Register TC, Shapses SA (2018) Effect of exercise modality during weight loss on bone health in older adults with obesity and cardiovascular disease or metabolic syndrome: a randomized controlled trial. J Bone Miner Res 33:2140–2149
Zibellini J, Seimon RV, Lee CM, Gibson AA, Hsu MS, Shapses SA, Nguyen TV, Sainsbury A (2015) Does diet-induced weight loss lead to bone loss in overweight or obese adults? A systematic review and meta-analysis of clinical trials. J Bone Miner Res 30:2168–2178
Soltani S, Hunter G, Kazemi A, Shab-Bidar S (2016) The effects of weight loss approaches on bone mineral density in adults: a systematic review and meta-analysis of randomized controlled trials. Osteoporos Int 27:2655–2671
Kemmler W, Shojaa M, Kohl M, von Stengel S (2020) Effects of different types of exercise on bone mineral density in postmenopausal women: a systematic review and meta-analysis. Calcif Tissue Int 107:409–439
Mason C, Xiao L, Imayama I, Duggan CR, Bain C, Foster-Schubert KE, Kong A, Campbell KL, Wang C-Y, Neuhouser ML (2011) Effects of weight loss on serum vitamin D in postmenopausal women. Am J Clin Nutr 94:95–103
Fukushima N, Hanada R, Teranishi H, Fukue Y, Tachibana T, Ishikawa H, Takeda S, Takeuchi Y, Fukumoto S, Kangawa K (2005) Ghrelin directly regulates bone formation. J Bone Miner Res 20:790–798
Sumithran P, Prendergast LA, Delbridge E, Purcell K, Shulkes A, Kriketos A, Proietto J (2011) Long-term persistence of hormonal adaptations to weight loss. N Engl J Med 365:1597–1604
Oshima K, Nampei A, Matsuda M, Iwaki M, Fukuhara A, Hashimoto J, Yoshikawa H, Shimomura I (2005) Adiponectin increases bone mass by suppressing osteoclast and activating osteoblast. Biochem Biophys Res Commun 331:520–526
Shapses SA, Sukumar D (2012) Bone metabolism in obesity and weight loss. Annu Rev Nutr 32:287–309
O’dea JP, Wieland RG, Hallberg MC, Llerena LA, Zorn EM, Genuth SM (1979) Effect of dietary weight loss on sex steroid binding, sex steroids, and gonadotropins in obese postmenopausal women. J Lab Clin Med 93:1004–1008
Eriksen EF, Colvard DS, Berg NJ, Graham ML, Mann KG, Spelsberg TC, Riggs BL (1988) Evidence of estrogen receptors in normal human osteoblast-like cells. Science 241:84–86
Cifuentes M, Riedt CS, Brolin RE, Field MP, Sherrell RM, Shapses SA (2004) Weight loss and calcium intake influence calcium absorption in overweight postmenopausal women. Am J Clin Nutr 80:123–130
Shapses SA, Riedt CS (2006) Bone, body weight, and weight reduction: what are the concerns? J Nutr 136:1453–1456
Kerr D, Morton A, Dick I, Prince R (1996) Exercise effects on bone mass in postmenopausal women are site-specific and load-dependent. J Bone Miner Res 11:218–225
Maddalozzo G, Snow C (2000) High intensity resistance training: effects on bone in older men and women. Calcif Tissue Int 66:399–404
Wallace B, Cumming R (2000) Systematic review of randomized trials of the effect of exercise on bone mass in pre-and postmenopausal women. Calcif Tissue Int 67:10–18
Williams NI, Leidy HJ, Hill BR, Lieberman JL, Legro RS, Souza MJD (2015) Magnitude of daily energy deficit predicts frequency but not severity of menstrual disturbances associated with exercise and caloric restriction. Am J Physiol Endocrinol Metab 308:E29–E39
Anderson JW, Konz EC, Frederich RC, Wood CL (2001) Long-term weight-loss maintenance: a meta-analysis of US studies. Am J Clin Nutr 74:579–584
Daly RM, Dunstan DW, Owen N, Jolley D, Shaw JE, Zimmet PZ (2005) Does high-intensity resistance training maintain bone mass during moderate weight loss in older overweight adults with type 2 diabetes? Osteoporos Int 16:1703–1712
Svendsen OL, Hassager C, Christiansen C (1993) Effect of an energy-restrictive diet, with or without exercise, on lean tissue mass, resting metabolic rate, cardiovascular risk factors, and bone in overweight postmenopausal women. Am J Med 95:131–140
Kanis JA (2002) Diagnosis of osteoporosis and assessment of fracture risk. Lancet (London, England) 359:1929–1936
Brownbill RA, Ilich JZ (2005) Measuring body composition in overweight individuals by dual energy x-ray absorptiometry. BMC Med Imaging 5:1–7
Pisani P, Renna MD, Conversano F, Casciaro E, Muratore M, Quarta E, Di Paola M, Casciaro S (2013) Screening and early diagnosis of osteoporosis through X-ray and ultrasound based techniques. World J Radiol 5:398
Mckee H, Beattie K, Lau A, Wong A, Adachi R (2017) Novel imaging modalities in the diagnosis and risk stratification of osteoporosis. J Orthop Ther 2017:1–9
Burian E, Syväri J, Dieckmeyer M, Holzapfel C, Drabsch T, Sollmann N, Kirschke JS, Rummeny EJ, Zimmer C, Hauner H (2020) Age-and BMI-related variations of fat distribution in sacral and lumbar bone marrow and their association with local muscle fat content. Sci Rep 10:1–8
Wehrli FW, Hopkins JA, Hwang SN, Song HK, Snyder PJ, Haddad JG (2000) Cross-sectional study of osteopenia with quantitative MR imaging and bone densitometry. Radiology 217:527–538
Rantalainen T, Nikander R, Heinonen A, Cervinka T, Sievänen H, Daly RM (2013) Differential effects of exercise on tibial shaft marrow density in young female athletes. J Clin Endocrinol Metab 98:2037–2044
Chandran M, Hough F, Lee K (2010) Is BMD measurement still useful with the advent of the FRAX fracture risk assessment tool. Medicographia 32:49–58
Pappou IP, Girardi FP, Sandhu HS, Parvataneni HK, Cammisa FP Jr, Schneider R, Frelinghuysen P, Lane JM (2006) Discordantly high spinal bone mineral density values in patients with adult lumbar scoliosis. Spine 31:1614–1620
Acknowledgements
The authors would like to thank the research council of Nutrition and Food Security Research Center, Shahid Sadoughi University of Medical Sciences for scientific support of the present study.
Funding
The present systematic review was financially supported by Nutrition and Food Security research center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yazdanpanah, Z., Beigrezaei, S., Mohseni-Takalloo, S. et al. Does exercise affect bone mineral density and content when added to a calorie-restricted diet? A systematic review and meta-analysis of controlled clinical trials. Osteoporos Int 33, 339–354 (2022). https://doi.org/10.1007/s00198-021-06187-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-021-06187-9