Abstract
Summary
The increase in fracture risk associated with a recent fragility fracture is more appropriately captured using a 10-year fracture probability than 2- or 5-year probabilities.
Introduction
The recency of prior fractures affects subsequent fracture risk. The aim of this study was to quantify the effect of a recent sentinel fracture, by site, on the 2-, 5-, and 10-year probability of fracture.
Methods
The study used data from the Reykjavik Study fracture register that documented prospectively all fractures at all skeletal sites in a large sample of the population of Iceland. Fracture probabilities were determined after a sentinel fracture (humeral, clinical vertebral, forearm and hip fracture) occurring within the previous 2 years and probabilities for a prior osteoporotic fracture irrespective of recency. The probability ratios were used to adjust fracture probabilities over a 2-, 5-, and 10-year time horizon.
Results
As expected, probabilities decreased with decreasing time horizon. Probability ratios varied according to age and the site of sentinel fracture. Probability ratios to adjust for a prior fracture within the previous 2 years were higher the shorter the time horizon, but the absolute increases in fracture probabilities were much reduced. Thus, fracture probabilities were substantially lower with time horizons less than 10 years.
Conclusion
The 10-year probability of fractures is the appropriate metric to capture the impact of the recency of sentinel fractures. The probability ratios provide adjustments to conventional FRAX estimates of fracture probability for recent sentinel fractures, adjustments which can readily inform clinical decision-making.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2008, the then World Health Organization (WHO) Collaborating Centre for Metabolic Bone Diseases at Sheffield, UK, released FRAX®, a fracture risk assessment tool for estimating individualized 10-year probability of hip and major osteoporotic fracture (MOF; hip, clinical spine, distal forearm, or proximal humerus) [1]. The FRAX tool integrates seven dichotomous clinical risk factors (CRFs: prior fragility fracture, parental hip fracture, smoking, systemic glucocorticoid use, excess alcohol intake, rheumatoid arthritis, and other causes of secondary osteoporosis) which, in addition to age, sex, and body mass index (BMI), contribute to a 10-year fracture probability estimate independently of bone mineral density (BMD) [1, 2]. BMD at the femoral neck is an optional input variable. FRAX tools are country specific to take account of the heterogeneity of fracture risk and mortality worldwide [3]. Since its release, 71 models have been made available for 66 countries covering more than 80% of the world population [4]. The tool provides metrics which are increasingly used in health technology assessment [5,6,7], regulatory guidance [8], and clinical guidelines [9].
Prior fragility fracture, a well-established risk factor for a future fracture [10,11,12,13,14], is already accommodated within FRAX [1]. The population relative risk of having a hip fracture or other osteoporotic fracture is approximately 2-fold higher for most types of prior fracture. However, the increase in risk is not constant with time or age [13]. Additionally, the risk of a subsequent osteoporotic fracture is particularly acute immediately after an index fracture and wanes progressively with time [15,16,17,18,19,20,21,22]. The immediate risk is high and then wanes over time for approximately 2 years. Thereafter, a nadir is reached but the risk remains higher than that of the general population. The early phase of particularly high risk has been termed imminent risk [22].
This transiency, which is not currently accommodated in the FRAX algorithm, suggests that treatment given to patients immediately after a fracture might avoid a higher number of new fractures compared with treatment given at a later date. Despite limited empirical data [23], this reinforces a rationale for very early intervention immediately after fractures to avoid recurrent fractures. Furthermore, it supports the use of the most effective therapies early in the course of treatment, rather than delaying their use to a time of lower fracture risk. Thus, the quantification of imminent risk enables the targeting of anabolic treatments to individuals identified to be at very high risk [24]. The most recent guidelines of the International Osteoporosis Foundation and European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases provided multipliers to traditional FRAX estimates of fracture probability to account for the imminent risk associated with a recent vertebral fracture [7]. More recently, algorithms have been provided to adjust FRAX probabilities for a recent hip, spine, humerus, and forearm fracture [25].
These adjustments represent multipliers to 10-year fracture probabilities for individuals with a prior fragility fracture. For example, the 10-year probability of major osteoporotic fracture (MOF) in women age 60 from the UK with no clinical risk factors (BMI set at 25 kg/m2) is 5.9%. The FRAX-based probability rises to 12% in the presence of a prior fragility fracture. In the presence of a recent spine fracture (0–2 years), the multiplier of 1.84 is used to uplift the 10-year probability to 22% [25]. It has been argued that shorter-term probabilities would be appropriate for clinical messaging because the multipliers would be greater. The counter argument is that despite higher multipliers, shorter time horizons would reduce the absolute fracture probabilities to an extent greater than the increment provided by higher multipliers. That is, for any given scenario, the final absolute fracture probability will always be greater over a 10-year than over a 2-year time horizon.
The aim of the present study was to compare the impact of recency of index fractures on fracture probability as used by FRAX (i.e., over 10 years) with those calculated over a 5-year or 2-year time horizon.
Methods
Methods have been previously detailed [25]. In brief, the study used data from the Reykjavik Study fracture register that documented prospectively all fractures at all skeletal sites in a large sample of the population of Iceland. Fracture probabilities were determined after a sentinel fracture (humeral, clinical vertebral, forearm, and hip fracture) from the hazards of death and fracture [26, 27]. It is important to note that the probability models used were based on purpose-built models similar, but not identical, to FRAX. Fracture probabilities were computed on the one hand for sentinel fractures occurring within the previous 2 years and on the other hand probabilities for a prior osteoporotic fracture irrespective of its site or recency. Probability ratios for the two estimates were determined for time horizons of 10 years (as for FRAX), 5 years, and 2 years. The probability ratios were used to adjust estimates of fracture probability for recent sentinel fractures by age, sex, site of sentinel fracture, and time horizon.
Probability estimates are presented for each sentinel fracture sustained within the previous 2 years. For brevity, a fracture within the previous 2 years is termed a recent fracture unless otherwise noted.
Results
Follow up data were available for 2074 individuals following a hip fracture, 1365 cases of clinical vertebral fracture, 2364 following a distal forearm fracture, and 1092 cases of fracture at the proximal humerus. Ten-year probabilities of a major osteoporotic fracture and hip fracture in men and women with a prior fragility fracture (any site irrespective of its recency), men and women with a recent sentinel fracture (within 2 years), and the ratio between 10-year probabilities by age are given in the Appendix (Tables 1, 2, 3 and 4).
Ten-year, 5-year, and 2-year probabilities of a major osteoporotic fracture and hip fracture (%) in men and women with a prior fragility fracture (any site irrespective of its recency), probabilities for a recent clinical vertebral fracture (within the previous 2 years), and the ratio between 10-year probabilities by age are provided in the Appendix. We illustrate below the salient features for women from Iceland.
Time horizon
As expected, probabilities decreased with decreasing time horizon. Probabilities of a major osteoporotic fracture (MOF) in women with a prior fracture (of any recency) are shown in Fig. 1. It is important to note that probabilities shorter than 10 years are not a simple fraction of 10-year probabilities, particularly among older women, largely reflecting the effects of competing mortality over the longer time horizon. In the examples in Fig. 1, 5-year probabilities varied from 28% of the 10-year value at the age of 50 years to 79% at the age of 90 years. In the case of 2-year probabilities, the variation with age was from 10 to 43%, respectively.
Similar findings were applied to men and to hip fracture probabilities (see Appendix).
Adjustment ratios
Figure 2 shows adjustment ratios for a recent sentinel spine fracture in women. Adjustment ratios decreased with age but were higher the shorter the time horizon. Of note, the impact of the time horizon on the ratios was most marked at younger ages, and the differences diminished substantially with age. Similar findings applied to men and to hip fracture probabilities (see Appendix).
Probability of MOF
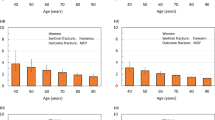
The 10-year probability of major osteoporotic fracture (MOF) in women is shown in Fig. 3 for recent (within previous 2 years) vertebral, hip, humerus, and forearm fracture by age. For each sentinel fracture and each age, fracture probabilities were lowest with a 2-year time horizon, intermediate with a 5-year horizon, and highest for 10-year probabilities. Similar findings were noted in men (Appendix). Probabilities varied according to the site of sentinel fracture with higher ratios for hip and vertebral fracture than for humerus or forearm fracture.
Probability of hip fracture
The 10-year probability of hip fracture in women is shown in Fig. 4 for recent hip fracture by age. At each age, fracture probabilities were lowest with a 2-year time horizon, intermediate with a 5-year horizon, and highest for 10-year probabilities. Similar findings were noted for all sentinel fractures and in men (Appendix).
Discussion
This analysis indicates that although probability adjustment ratios increase with decreasing time horizon, fracture probabilities calculated over a shorter than 10-year horizon yield markedly lower absolute values, as expected. The low absolute risk with the shorter time horizon attenuates markedly the effect of the multiplier. This suggests that 10-year probabilities are the preferred metric to express recent sentinel fractures for at least three reasons. Firstly, management of fracture risk is a long-term strategy, so that short time horizons undermine NNTs and health economic assessment. Secondly, the larger numbers using the 10-year horizon are more readily appreciated by patients and health care professionals. Thirdly, 10-year horizons are accepted worldwide as a risk measurement for many chronic diseases. For fragility fracture, this holds true not only for FRAX but also for national risk engines such as QFracture, the Garvan calculator, and the American Bone Health algorithm [28,29,30]. A counter argument (raised by one of the reviewers of this paper) is that a 2-year probability may be of greater immediate personal significance than a 10-year probability despite the lower probability. The differences are, however, substantial. For example, a woman aged 60 years with a recent vertebral fracture has a 10-year probability of a MOF of 36% and a 2-year probability of 11% (see Table 1 of Appendix).
For the present study, we provided FRAX adjustments for prior fractures within a 2-year interval. The choice of 2 years is somewhat arbitrary but covers the approximate period of imminent risk [22]. Other scenarios are equally possible. For example, the probability ratio for a woman aged 60 years with a sentinel vertebral fracture (that is, at any time in the past 2 years) is 1.84 (Appendix). The probability ratio at the time of fracture (time 0) is 1.96 and at 2 years after the prior fracture is 1.75, differing from the integral value by 5–6% (data not shown). The small differences suggest that the 2-year integral value sacrifices accuracy modestly for a substantial gain in simplicity. Nonetheless, computer-based algorithms will provide a more granular assessment of fracture recency as a continuous variable. An example is shown in Fig. 5 for a sentinel humerus fracture.
The present study also highlights that probability time horizons are non-linear in that, for example, a 5-year probability in individuals is not just half that of a 10-year probability. In large heterogeneous populations, this will be approximately true [31] but falls down in individual estimates. As noted previously, 5-year probabilities varied from 28% of the 10-year value at the age of 50 years to 79% at the age of 90 years in women with a prior fracture (Fig. 1). In the case of 2-year probabilities, the variation with age was from 10 to 43%, respectively. However, at the age of 70 years, the 5-year probability was half that of the 10-year value, and the 2-year probability was one fifth that of the 10-year probability. The differences reflect the changing death and fracture hazards with age. For example, at the age of 50 years, an individual is unlikely to die following say a humeral fracture. In this case, the 2-year probability of a MOF (14.4%) in a woman will be close to one fifth of the 10-year probability (3.18%). At the age of 90 years, the competing risk of death is much higher so that the 2-year probability (12%) approaches more closely the 10-year probability (18%) which, in turn, is almost the same as the 5-year probability (16%). This somewhat complex relationship differs according to the site of sentinel fracture since each has a different impact on subsequent risk of fracture and death. These observations caution the use of short-term probabilities if they do not take these factors into account.
The present results are based on an Icelandic population. There are, however, large differences in age and sex-specific fracture incidence in different countries of the world [3]. Thus, the absolute probability values we observed will not be representative of other populations, but there is no reason to suppose that probability ratios would differ markedly by country. This assumption has not been extensively tested. However, probability ratios following a sentinel vertebral fracture in the present study were very similar to those calculated for the UK [24, 25]. This suggests that the probability ratios derived in the present study can be applied to adjust FRAX estimates of fracture probability in all FRAX models.
References
Kanis JA, on behalf of the World Health Organization Scientific Group (2008a) Assessment of osteoporosis at the primary health-care level. Technical Report. WHO Collaborating Centre, University of Sheffield, UK. Available at http://www.shef.ac.uk/FRAX/index.htm. Accessed 6th Sept 2020
Kanis JA, Johnell O, Oden A, Johansson H, McCloskey EV (2008b) FRAX™ and the assessment of fracture probability in men and women from the UK. Osteoporos Int 19:385–397
Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl D, Cyrus Cooper C, on behalf of the IOF Working Group on Epidemiology and Quality of Life (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23:2239–2256
Kanis JA, Johansson H, Oden A, Cooper C, McCloskey EV, and the Epidemiology and Quality of Life Working Group of IOF (2014) Worldwide uptake of FRAX. Arch Osteoporos 9:166. https://doi.org/10.1007/s11657-013-0166-8
National Institute for Health and Care Excellence (2012) CG146: osteoporosis: fragility fracture risk. Short clinical guideline- evidence and recommendation. National Clinical Guideline Centre, London
National Institute for Health and Care Excellence (2017) TA 464: bisphosphonates for treating osteoporosis. Technology appraisal guidance 464. National Institute for Health and Care Excellence, London. https://nice.org.uk/guidance/ta464. Accessed 8 March 2020
Kanis JA, Cooper C, Rizzoli R, Reginster J-Y, Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis (ESCEO) and the Committees of Scientific Advisors and National Societies of the International Osteoporosis Foundation (IOF) (2019) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 30:3–44
Committee for Medicinal Products for Human Use (CHMP) (2006) Guideline on the evaluation of medicinal products in the treatment of primary osteoporosis. CHMP, London
Kanis JA, Harvey NC, Cyrus Cooper C, Johansson H, Odén A, McCloskey EV, the Advisory Board of the National Osteoporosis Guideline Group (2016) A systematic review of intervention thresholds based on FRAX. A report prepared for the National Osteoporosis Guideline Group and the International Osteoporosis Foundation. Arch Osteoporos 11(1):25. https://doi.org/10.1007/s11657-016-0278-z
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA 3rd, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15:721–739
Haentjens P, Johnell O, Kanis JA, Bouillon R, Cooper C, Lamraski G, Vanderschuren D, Kauffman J-M, Boonen S (2004) Gender-related differences in short and long-term absolute risk of hip fracture after Colles’ or spine fracture: Colles’ fracture as an early and sensitive marker of skeletal fragility in men. J Bone Miner Res 19:1933–1944
Johnell O, Kanis JA, Oden A, Sernbo I, Redlund-Johnell I, Pettersen C, De Laet C, Jonsson B (2004) Fracture risk following an osteoporotic fracture. Osteoporos Int 15:175–179
Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas P, Eisman J, Fujiwara S, Garnero P, Kroger H, McCloskey EV, Mellstrom D, Melton LJ III, Pols H, Reeve J, Silman A, Tenenhouse A (2004) A meta-analysis of previous fracture and subsequent fracture risk. Bone 35:375–382
Hansen L, Petersen KD, Eriksen SA, Langdahl BL, Eiken PA, Brixen K, Abrahamsen B, Jensen JE, Harslof T, Vestergaard P (2015) Subsequent fracture rates in a nationwide population-based cohort study with a 10-year perspective. Osteoporos Int 26:513–519
Johnell O, Oden A, Caulin F, Kanis JA (2001) Acute and long-term increase in fracture risk after hospitalization for vertebral fracture. Osteoporos Int 12:207–214
Giangregorio LM, Leslie WD (2010) Manitoba bone density program. Time since prior fracture is a risk modifier for 10-year osteoporotic fractures. J Bone Miner Res 25:1400–1405
Dretakis KE, Dretakis EK, Papakitsou EF, Psarakis S, Steriopoulos K (1998) Possible predisposing factors for the second hip fracture. Calcif Tissue Int 62:366–369
Nymark T, Lauritsen JM, Ovesen O, Röck ND, Jeune B (2006) Short time-frame from first to second hip fracture in the Funen County hip fracture study. Osteoporos Int 17(9):1353–1357
Lindsay R, Silverman SL, Cooper C, Hanley DA, Barton I, Broy SB, Licata A, Benhamou L, Geusens P, Flowers K, Stracke H, Seeman E (2001) Risk of new vertebral fracture in the year following a fracture. JAMA 285:320–323
Ryg J, Rejnmark L, Overgaard S, Brixen K, Vestergaard P (2009) Hip fracture patients at risk of second hip fracture: a nationwide population-based cohort study of 169,145 cases during 1977-2001. J Bone Miner Res 24:1299–1307
van Geel TACM, van Helden S, Geusens PP, Winkens B, Dinant G-J (2016) Clinical subsequent fractures cluster in time after first fractures. Ann Rheum Dis 68:99–102
Johansson H, Siggeirsdóttir K, Harvey NC, Odén A, Gudnason V, McCloskey E, Sigurdsson G, Kanis JA (2017) Imminent risk of fracture after fracture. Osteoporos Int 28:775–780
Lyles KW, Colon-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C, Hyldstrup L, Recknor C, Nordsletten L, Moore KA, Lavecchia C, Zhang J, Mesenbrink P, Hodgson PK, Abrams K, Orloff JJ, Horowitz Z, Eriksen EF, Boonen S (2007) Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med 357:1–11
Kanis JA, Harvey NC, McCloskey E, Bruyère O, Veronese N, Lorentzon M, Cooper C, Rizzoli R, Adib G, Al-Daghri N, Campusano C, Chandran M, Dawson-Hughes B, Javaid K, Jiwa F, Johansson H, Lee JK, Liu E, Messina D, Mkinsi O, Pinto D, Prieto-Alhambra D, Saag K, Xia W, Zakraoui L, Reginster J-Y (2020) Algorithm for the management of patients at low/middle/high risk of osteoporotic fracture: a global perspective. Osteoporos Int 31:1–12
Kanis JA, Johansson H, Harvey NC, Gudnason V, Sigurdsson G, Siggeirsdottir K, Lorentzon M, Liu M, Vandenput L, McCloskey E (2020) Effects of the recency of sentinel fractures on conventional estimates of fracture probability using FRAX. Osteoporos Int 31, in press:1817–1828
Kanis JA, Johnell O, Oden A, Sernbo I, Redlund-Johnell I, Dawson A, de Laet C, Jonsson B (2000) Long-term risk of osteoporotic fractures in Malmo. Osteoporos Int 11:669–674
Kanis JA, Johnell O, De Laet C, Jonsson B, Oden A, Oglesby A (2002) International variations in hip fracture probabilities: implications for risk assessment. J Bone Miner Res 17:1237–1244
Hippisley-Cox J, Coupland C (2009) Predicting risk of osteoporotic fracture in men and women in England and Wales: prospective derivation and validation of QFracture scores. BMJ 339:b4229
Nguyen ND, Frost SA, Center JR et al (2008) Development of prognostic nomograms for individualizing 5-year and 10-year fracture risks. Osteoporos Int 19:1431–1444
American Bone Health (2020) 10-year fracture risk calculator version 2.1. https://americanbonehealth.org/calculator/. Accessed 23 April 2020
Leslie WD, Majumdar SR, Morin LM, Lix LM, Johansson H, Oden A, McCloskey EV, Kanis JA (2017) FRAX for fracture prediction shorter and longer than 10 years: the Manitoba BMD Registry. Osteoporos Int 28:2557–2564
Acknowledgments
We thank the participants in the Reykjavik Study for their valuable contribution.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the National Bioethics Committee and the Data Protection Authority in Iceland. All the participants gave informed written consent.
Conflicts of interest
W Leslie, E Liu and H Johansson, V Gudnason, G Sigurdsson, and Kristin Siggeirsdottir have no competing interests to declare.
N. Harvey has received consultancy, lecture fees, and honoraria from Alliance for Better Bone Health, AMGEN, MSD, Eli Lilly, Servier, Shire, UCB, Kyowa Kirin, Consilient Healthcare, Radius Health, and Internis Pharma.
EV McCloskey has received consultancy/lecture fees/grant funding/honoraria from AgNovos, Amgen, AstraZeneca, Consilient Healthcare, Fresenius Kabi, Gilead, GSK, Hologic, Internis, Lilly, Merck, Novartis, Pfizer, Radius Health, Redx Oncology, Roche, SanofiAventis, Servier, Synexus, UCB, Viiv, Warner Chilcott, I3 Innovus and Unilever.
JA Kanis reports grants from Amgen, Eli Lilly and Radius Health; consulting fees from Theramex.
M Lorentzon has received lecture fees from Amgen, Lilly, Meda, Renapharma, UCB Pharma, and consulting fees from Amgen, Radius Health, UCB Pharma, Renapharma and Consilient Health, all outside the presented work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Kanis, J., Johansson, H., Harvey, N. et al. The use of 2-, 5-, and 10-year probabilities to characterize fracture risk after a recent sentinel fracture. Osteoporos Int 32, 47–54 (2021). https://doi.org/10.1007/s00198-020-05700-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-020-05700-w