Abstract
The aim of this study was to examine the pattern of fracture risk following a prior fracture at the spine, shoulder or hip. We studied 1918 patients with fractures at these sites identified from the Department of Radiology in Malmo who were followed for 5 years. Poisson regression was used to compute fracture rates immediately after the initial fracture and at 5 years thereafter in men and women aged 60 or 80 years. Immediate fracture risk was higher than that of the general population, more markedly so at the age of 60 than at 80 years. At the age of 60 years, the risk of hip, forearm and spine fractures were significantly increased following a prior spine, hip or shoulder fracture in men. A similar pattern was seen in women, except that the increase in risk of forearm fracture following a spine or hip fracture was not statistically significant. The incidence of further fractures at the shoulder, spine or hip fell with time after the first fracture, a fall that was significant for all fractures after a shoulder fracture, hip fracture after a spine fracture, and hip and spine fractures after a hip fracture. We conclude that the risk of a subsequent fracture immediately after an osteoporotic fracture is highest immediately after the event. This provides a rationale for very early intervention immediately after fractures to avoid recurrent fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many studies have shown that a fragility fracture increases the risk of a further fracture. In a meta-analysis performed by Klotzbuecher et al. [1], the relative risk of having a hip fracture or a vertebral fracture was approximately 2-fold higher for most types of prior fractures. For a prior vertebral fracture, however, the risk of a further vertebral fracture was increased more than 4-fold. The increase in risk may not, however, be constant with time, at least in the case of fractures following a vertebral fracture. We recently showed that, after hospitalisation for a vertebral fracture, there was a greatly increased risk of requiring hospitalisation for a further fracture in the years following the initial hospitalisation [2]. Similar findings were observed for all vertebral fractures by Lindsay et al. [3], who showed that women who had developed a vertebral fracture had a substantial risk of fractures within the next year. The risk appears to decrease over subsequent years, but remains higher than that of the general population. This transient suggests that treatment given to such patients immediately after the vertebral fracture might avoid a high number of new fractures compared with treatment given some time later. The aim of the present study was to determine the pattern of risk of fractures occurring the years after a hip fracture, clinical vertebral fracture or shoulder fracture in both outpatients and hospitalised patients.
Materials and methods
Fractures were identified from the Department of Diagnostic Radiology in Malmö, Sweden [4], where all radiograph referrals are kept from a well-defined catchment area. The catchment identifies 97% of all fractures radiographed, and the remainder are treated privately [5]. X-rays are coded by site and fracture cases were separated from non-fracture cases. All hip fractures were verified against the surgical register in Malmo. Only citizens of Malmo were included in this analysis. Fractures of the hip were those registered in 1990/1991, the proximal humerus in 1987 and clinical vertebral fractures in 1993/1994. Vertebral fractures were included when an X-ray was taken for back pain.
Subsequent fractures sustained later were identified in the year 2000 from the same files and the date of fracture documented. Re-fractures at the same site were excluded by hand reading X-rays. The data on mortality were recorded from EPC (Epidemiological Centre, National Board of Health and Welfare) that records all deaths in Sweden. In order to estimate the accuracy of deaths and fractures, we examined demographic movement patterns in all residents of Malmo aged 70–80 years alive at the end of 1994. Over the subsequent 5 years, 0.5% of men and 0.5% of women had emigrated from Sweden, and mortality statistics were not therefore available. Over the same period, 2.0% of men and 2.2% of women moved from the city, a proportion of whom were lost to radiographic follow-up.
A Poisson model was used to calculate the rate of new fractures after a fracture taking mortality into account. Rates were compared to the incidence of each fracture type in the population of Malmo [4]. A significant increase in fracture rate was determined as a fracture rate where the limits of the 95% confidence interval exceeded the population risk. The rate was calculated as a function of age, sex and time after the fracture. The rate of new fractures was also calculated as a slope between year 0 (the date of fracture) and 5 years to determine whether fractures occurred more frequently at times closer to the original fracture.
Results
We identified 268 patients with fractures of the proximal humerus, 500 with fractures at the spine and 1150 with hip fractures who were followed for the 5-year period. The majority were women (Table 1). During the course of follow-up, 175 hip fractures, 71 forearm fractures, 105 spine fractures and 56 shoulder fractures were identified. The number and site of fractures occurring by year are shown in Table 2. For all fractures, more fractures occurred in the first year after fracture than in subsequent years. In the first year 34% of all subsequent fractures occurred. The number of fractures decreased progressively thereafter with time, so that in the last year of follow-up 90% of all fractures were seen. This general pattern was seen for each fracture type. For any prior fracture, 31–45% of new hip, forearm, spine or shoulder fracture occurred within the first year depending on the site of new fracture (see Table 2).
From the Poisson model, we computed fracture risk in men and women at the age of 60 years and 80 years following a fracture at each specific site (Table 3).
At the age of 60 years, a prior shoulder fracture was associated with an immediate risk of hip, forearm or spine fracture that was significantly higher than that of the age and sex matched population (Table 3). At the age of 80 years, the incidence was increased but significantly higher than the population risk only for subsequent forearm fractures in both men and women (Table 3).
For prior spine fractures, the immediate risk of subsequent fractures of hip, forearm and spine was significantly greater than that of the general population for men aged 60 years or 80 years. A similar pattern was seen in women except for subsequent forearm fractures, where the increase in risk at the age of 60 years (RR=2.3) or 80 years (RR=1.3) was not significantly higher than that of the general population.
A prior hip fracture was a significant risk factor for a further hip fracture in men and women irrespective of age. A prior hip fracture was a significant risk for forearm fracture in men aged 60 and 80 years, but not in women. Subsequent spine fractures were significantly more frequent after hip fracture at the age of 60 years in men and women, but not significantly so at the age of 80 years.
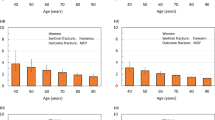
In subsequent years, the risk of fractures fell. Examples are given in Fig. 1. The decrease in incidence was observed for all scenarios (Table 4), but the slope was not significant for forearm or spine fractures following a spine fracture and of borderline significance for a forearm fracture after a hip fracture (P=0.07).
After 5 years, fracture risk remained significantly higher than the population risk for spine fractures after spine fracture (with the exception of men aged 80 years), hip fracture after spine fracture (in men and women aged 60 years), hip fractures after hip fractures (men and women aged 60 years), hip fracture after shoulder fracture (in men and women aged 60 years), spine fracture after shoulder fracture (women aged 60) and forearm fracture after shoulder fracture (for men only).
The difference in fracture rate between men and women was relatively small (see Fig. 2). For example, for new hip fractures the rate was 8–32% higher in women than in men, whereas in the general population, the risk in women aged 70–74 years was approximately 82% higher in women than in men.
Discussion
The principal findings of this study is that fracture rates following an osteoporotic fracture are substantially increased in the immediate post-fracture period. Qualitatively, the data are consistent with a recent meta-analysis and subsequent studies showing the associations between sites of fracture and subsequent fracture risks at other sites [1, 5, 7]. In addition, the present study also shows that a prior hip fracture is a significant risk factor for a forearm fracture (in men at the age of 60 and 80 years). The present study also indicates that quantitatively, the risk of subsequent fractures is much higher than that suggested by longer-term follow-up studies where the pattern of risk with time is not studied. Our findings suggest that, as shown for vertebral fracture [2, 3], the risk is initially high and declines thereafter, though for most fractures, not to the levels of the general population. The present study extends these observations in non-hospitalised patients with vertebral fracture and also suggests that the phenomenon arises following other sites of osteoporotic fracture. The reason for the transient marked increase in risk is not known, but is not due to loss of follow-up, which was near complete. Immobilisation and poor coordination are potential factors [2]. These studies were undertaken before specific treatments for osteoporosis were available in Sweden. A treatment effect of calcium and vitamin D is implausible, given the magnitude of the decrease with time and the poor adherence to chronic therapy [8, 9].
Paradoxically, we showed that fracture rates declined significantly following shoulder and hip fracture, whereas the slope describing decreasing incidence with time was not significant in the case of a prior vertebral fracture and subsequent vertebral fractures. In contrast, this effect was marked for hospitalised vertebral fracture [2]. By including outpatients in the present study, some of whom may have had long-standing fractures not presenting to hospital for some time, the trend with time might have biased against finding an effect. A further limitation of this study is the small number of fractures studied. For this reason, it is not possible to show accurately the exact pattern of incidence with time.
Many randomised studies have shown the effectiveness of pharmaceutical intervention for spine fractures and in some cases for appendicular fractures [10, 11, 12, 13, 14, 15, 16]. The effects on fracture risk are particularly well studied in individuals with a prior vertebral fracture. If the same holds true for appendicular fractures, then our findings suggest that treatment should be targeted immediately after fractures and thereby reduce the very high risk immediately after the fracture event.
References
Klotzbuecher CM, Ross PD, Landsman PB, Abbot III TA, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15:721–739
Johnell O, Odén A, Caulin F, Kanis JA (2001) Acute and long-term increase in fracture risk after hospitalization for vertebral fracture. Osteoporos Int 12:207–214
Lindsay R, Silverman SL, Cooper C, Hanley DA; Barton I, Broy SB, Licata A, Benhamou L, Geusens P, Flowers K, Stracke H, Seeman E (2001) Risk for new vertebral fracture in the year following a fracture. JAMA 285:320–323
Kanis JA, Johnell O, Odén A, Sernbo I, Redlund-Johnell I, Dawson A, De Laet C, Jönsson B (2000) Long-term risk of osteoporotic fracture in Malmö. Osteoporos Int 11:669–674
Jonsson B, Gardsell P, Johnell O, Redlund-Johnell I, Sernbo I (1994) Remembering fractures: fracture registration and proband recall in Southern Sweden. J Epidemiol Comm Health 48:489–490
Van Staa TP, Leufkens HGM, Coopewr C (2002) Does a fracture at one site predict later fractures at other sites? A British cohort study. Osteoporos Int 13:624–629
Hasserius R, Karlsson MK, Nilsson BE, Redlund-Johnell I, Johnell O (2003) Prevalent vertebral deformities predict increased mortality and increased fracture rate in both men and women: a 10 year population-based study of 598 individuals from the Swedish cohort in the European Vertebral Osteoporosis Study. Osteoporos Int 14:61–68
Castel H, Bonneth DY, Sherf M, Liel Y (2001) Awareness of osteoporosis and compliance with management guidelines in patients with newly diagnosed low impact fractures. Osteoporos Int 12:559–564
Torgerson DJ, Dolan P (1998) Prescribing by general practitioners after an osteoporotic fracture. Ann Rheum Dis 57:378–379
Black DM, Cummings SR, Karpf DB et al. (1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fracture. Lancet 348:1535–1541
Cummings SR, Black DM, Thompson DE et al. (1998) Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures. JAMA 280:2077–2082
Harris ST, Watts NB, Genant HK et al. for the VERT Study Group (1999)Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis. A randomized controlled trial. JAMA 282:1344–1352
Reginster J-Y, Minne HW, Sörensen OH et al. (2000) on behalf of the VERT Study Group. Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Osteoporos Int 11:83–91
McClung MR, Geusens P, Miller PD et al. (2001) for the Hip Intervention Program Study Group. Effect of risedronate on the risk of hip fracture in elderly women. N Engl J Med 344:333–340
Ettinger B, Black DM, Mitlak BH et al. (1999) Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene; results from a 3-year randomized clinical trail. Multiple Outcome of Raloxifene Evaluation (MORE) Investigators. JAMA 282:637–645
Neer RM, Arnaud CD, Zanchetta JR et al. (2001) Effect of parathyroid hormone (1–34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med 344:1434–1441
Acknowledgements
We are grateful for the unrestricted support of the Alliance for Better Bone Health, Lilly, Hologic, IGEA, G-E Lunar, Wyeth, Roche and Novartis. These studies were supported by the International Osteoporosis Foundation, the National Osteoporosis Foundation and the International Society for Clinical Densitometry.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Johnell, O., Kanis, J.A., Odén, A. et al. Fracture risk following an osteoporotic fracture. Osteoporos Int 15, 175–179 (2004). https://doi.org/10.1007/s00198-003-1514-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-003-1514-0