Abstract
Summary
A simple question construct regarding number of falls in the previous year, ascertained by a single question, was strongly associated with incident fractures in routine clinical practice using a population-based dual-energy X-ray absorptiometry (DXA) registry.
Introduction
There is conflicting evidence from research cohorts that falls independently increase fracture risk. We examined the independent effects of falls on subsequent fractures in a large clinical registry of bone mineral density (BMD) results for the Province of Manitoba, Canada that has been systematically collecting self-reported falls information since September 1, 2012.
Methods
The study population consisted of 24,943 women and men aged 40 years and older (mean age 65.5 ± 10.2 years) with fracture probability assessment (FRAX), self-reported falls for the previous year (categorized as none, 1, 2, or > 3) and fracture outcomes. Adjusted hazard ratios (HR) with 95 confidence intervals (CI) for time to fracture were estimated using Cox proportional hazards models.
Results
During mean observation time of 2.7 ± 1.0 years, 863 (3.5%) sustained one or more major osteoporotic fractures (MOF), 212 (0.8%) sustained a hip fracture, and 1210 (4.9%) sustained any incident fracture. Compared with no falls in the previous year (referent), there was a gradient of increasing risk for fracture with increasing number of falls (all P < 0.001). Results showed minimal attenuation with covariate adjustment. When adjusted for baseline fracture probability (FRAX score with BMD) the HR for MOF increased from 1.49 (95% CI 1.25–1.78) for one fall to 1.74 (1.33–2.27) for two falls to 2.62 (2.06–3.34) for ≥ 3 falls. HRs were similar for any incident fracture and slightly greater for prediction of hip fracture, reaching 3.41 (95% CI 2.19–5.31) for ≥ 3 previous falls.
Conclusions
Self-report number of falls in the previous year is strongly associated with incident fracture risk in the routine clinical practice setting, and this risk is independent of age, sex, BMD, and baseline fracture probability. Moreover, there is dose–response with multiple falls (up to a maximum of 3) conferring greater risk than a single fall.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is characterized by low bone mass and deterioration of bone tissue, leading to an increase in bone fragility and susceptibility to fracture, with substantial health consequences for the individual and society [1]. Fracture risk algorithms that combine clinical risk factors and bone mineral density (BMD) are now widely used in clinical practice to target high-risk individuals for treatment [2]. The fracture risk assessment tool (FRAX®) was developed to predict an individual’s 10-year probability of major osteoporotic fracture (MOF; a composite of the hip, humerus, forearm, and clinical vertebral fractures) and hip fracture from readily assessed clinical risk factors [3], with over 100 clinical practice guidelines including FRAX in their recommendations [2].
A frequent criticism of the FRAX model has been the lack of inclusion of falls or fall risk in predicting fractures [4, 5]. In contrast, fall history is an input variable to other risk calculators. For example, the Garvan fracture risk calculator considers number of falls in the previous year, from 0 to maximum 3 [6, 7]. The QFracture calculator considers prior falls, without a defined time frame, as a dichotomized measure [8, 9]. Recent evidence derived from carefully conducted research cohort studies in men found that falls increase fracture risk independent of FRAX probability [10]. However, data are inconsistent with a paucity of evidence demonstrating usefulness of self-reported fall data as collected in routine clinical practice. Falls in the previous year did not contribute to MOF risk assessment in a small cohort from Rochester, Minnesota (250 women and 249 men), or a large cohort of 2000 older Chinese women, and was excluded from the Fracture INDEX tool based upon the Study of Osteoporotic Fractures (SOF) [11,12,13]. Since risk from falls may be responsive to pharmacologic and non-pharmacologic interventions, it is important to determine if falls predict fractures independently of currently accepted risk factors [14, 15].
Given uncertainty regarding the usefulness of fall information collected in routine clinical practice, we examined the independent effects of falls and FRAX for predicting fracture outcomes in a large clinical registry of patients with BMD data for the Province of Manitoba, Canada. This registry has been systematically collecting self-reported fall information since September 1, 2012.
Methods
Study population
In the Canadian Province of Manitoba (population 1.3 million in 2017), health services are provided to virtually all residents through a public healthcare system. Dual-energy X-ray absorptiometry (DXA)-based BMD testing has been managed as an integrated clinical program since 1997; criteria for testing have been published and include screening at age 65 years for women and in men and younger women with additional risk factors [16]. The program maintains a database of all DXA results which can be linked with other provincial population-based computerized health databases through an anonymous personal identifier. The DXA database has completeness and accuracy in excess of 99% [17].
The study population consisted of all women and men aged 40 years and older with self-reported fall information and DXA scans from September 1, 2012 and March 31, 2016. We excluded those not registered for health care in Manitoba, without coverage after the baseline BMD, or with missing baseline measurements required for FRAX. For those with more than one qualifying examination, only the first was included. The study was approved by the Health Research Ethics Board for the University of Manitoba.
Self-reported falls
All patients receive an intake questionnaire by mail approximately 2–4 weeks prior to their BMD appointment. The questionnaire collects important information required for reporting, including FRAX risk factors. Since September 1, 2012, it has included a fall question. There is no uniform question construct regarding fall history; therefore, we asked about number of falls in the preceding year. We adapted language from previous studies, particularly the baseline questionnaire for the Canadian Multicentre Osteoporosis Study (CaMos) [18], with language adapted for ease of understanding and self-reporting. The final wording was “Have you fallen in the last year? (Do NOT include minor slips or from sports.) If Yes, how many times? ○ No ○ Don’t know.” Completeness of the information was reviewed by the BMD technologist at the time of BMD testing and there were no missing data. Responses were captured in a web-based BMD reporting tool, with uncertain coded as no falls.
Bone mineral density measurements and fracture probability
Hip DXA scans were performed and analyzed in accordance with manufacturer’s recommendations. Femoral neck T-scores (number of SDs above or below young adult mean BMD) were calculated from NHANES III white female reference values [19]. The program’s quality assurance is under strict supervision by a medical physicist [16]. The six cross-calibrated instruments used for this study (3 Prodigy and 3 iDXA, GE/Lunar Healthcare, Madison WI; between-scanner differences < 0.1 T-score) exhibited stable long-term performance (coefficient of variation < 0.5%). All reporting physicians and supervising technologists are required to maintain DXA certification with the International Society for Clinical Densitometry (ISCD).
Ten-year probability of a major osteoporotic fracture risk was calculated using the World Health Organization fracture risk assessment tool, Canadian version (FRAX® Desktop Multi-Patient Entry, version 3.7) [20, 21]. Briefly, age, body mass index (BMI), femoral neck BMD, and other data required for calculating fracture probability with FRAX were assessed from measurements (height and weight) and information collected directly from subjects through the intake questionnaire which was reviewed at the time of DXA scanning [22]. Questionnaire information was supplemented with population-based healthcare data (hospital discharge abstracts, medical claims diagnoses, province-wide retail pharmacy database) as previously described, thereby ensuring complete information in virtually all subjects [23,24,25]. The Canadian FRAX tool was calibrated using nationwide hip fracture and mortality data as previously described [21]. Predictions agree closely with observed fracture risk in our population [26, 27].
Fractures outcomes
Manitoba Health records were assessed for the presence of fracture diagnostic codes following the BMD assessment. Fractures that were not associated with trauma codes were assessed through a combination of hospital discharge abstracts (diagnoses and procedures coded using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) prior to 2004 and International Classification of Diseases, Tenth Revision, Canadian Enhancements (ICD-10-CA) thereafter) and physician billing claims (coded using ICD-9-CM). The primary analysis was based upon incident non-traumatic hip, clinical vertebral, forearm, and humerus fracture diagnostic codes (collectively designated “major osteoporotic” fractures) using previously validated algorithms [28, 29]. We required that hip and forearm fracture codes be associated with site-specific fracture reduction, fixation, or casting codes to enhance specificity for an acute fracture event. Secondary analyses examine hip fracture alone or any incident fracture (excluding head/neck, hands, feet, and ankle). To minimize potential misclassification of prior incident fractures, we conservatively required that there be no hospitalization or physician visit(s) with the same fracture type in the 6 months preceding an incident fracture diagnosis. Administrative fracture data is collected independent from and after the collection of falls data, thereby avoiding ascertainment bias.
Statistical analysis
Statistical analyses were performed with Statistica (Version 13.0, StatSoft Inc., Tulsa, OK). Descriptive statistics for demographic and baseline characteristics are presented as mean ± SD for continuous variables or number (%) for categorical variables. We estimated Spearman’s correlations between number of falls and baseline characteristics. Time to incident fracture following the DXA scan (index date) was studied using Cox proportional hazards regression. Observations were censored for death (vital statistics), migration out of province (Manitoba Health registry file), or end of follow-up (March 31, 2017). The primary analysis examined incident MOF as the outcome of interest with numbers of falls in the previous year as a categorical measure (levels 1 fall, 2 falls, ≥ 3 falls; referent no falls). We reported hazard ratios (HRs) with 95% confidence intervals (CIs) adjusted for age and sex (Model 1); age, sex, BMI, and femoral neck BMD (Model 2); or baseline fracture probability (MOF fracture probability for incident MOF or any fracture, hip fracture probability for incident hip fracture) using the FRAX score with BMD (Model 3), log-transformed to correct for a skewed distribution. Proportionality of hazards was confirmed by testing scaled Schoenfeld residuals versus time. As supplementary analyses, we stratified by sex and age (< 65 years vs ≥ 65 years, < 65 years vs 65–79 years vs > 80 years) and examined previous falls as a risk factor for mortality, and tested for two-way interactions with falls. Furthermore, we tested for two-way interactions between age and sex with number of falls and we also categorized number of falls in the previous year from 1 through ≥ 5 as a previous report has proposed an adjustment of FRAX output based upon number of falls to a maximum of five [5].
Results
Figure 1 summarizes the population selection process. In the period 2012–2016 when previous falls information was collected, there were 27,544 individual visits for BMD assessment. After exclusions (2601, 9.4%), the analytic cohort consisted of 24,943 individuals with complete information regarding falls, FRAX risk factors, and fracture follow-up. One or more falls was reported by 20.6% of the study cohort (12.4% one fall, 4.3% two falls, 3.9% ≥ 3 falls in the previous year). Mean age of the cohort was 65.5 ± 10.2 years with a large majority of females (89.7%), typical for the population undergoing BMD screening. Average BMI, femoral neck T-score, and fracture probability are summarized in Table 1.
The association between number of falls in the previous year and age, sex, BMI, femoral neck T-score, and fracture probability are summarized in Table 2. In general, these associations were very weak and number of falls explained < 1% of the variance.
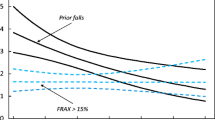
During mean observation time of 2.7 ± 1.0 years, 863 (3.5%) sustained one or more MOF, 212 (0.8%) sustained a hip fracture, and 1210 (4.9%) sustained any incident fracture. Figure 2 shows the unadjusted fracture-free Kaplan–Meier’s survival curve according to number of self-reported falls in the previous year. There was a significant divergence in the curves (log-rank P < 0.001) regardless of whether the outcome was incident MOF, hip fracture, or any incident fracture. Individuals with no previous falls were consistently at lower risk than individuals with falls, with individuals experiencing ≥ 3 falls consistently at greatest risk.
Incident fracture prediction assessed from Cox proportional hazards models with adjustment for baseline covariates is summarized in Table 3. Compared with no falls in the previous year (referent), there was a gradient of increasing risk for fracture with increasing number of falls (all P < 0.001). Results showed minimal attenuation with covariate adjustment. When adjusted for baseline fracture probability (FRAX score with BMD), the HR for MOF increased from 1.49 (95% CI 1.25–1.78) for one fall to 1.74 (1.33–2.27) for two falls to 2.62 (2.06–3.34) for ≥ 3 falls. HRs were similar for any incident fracture and slightly greater for prediction of hip fracture, reaching 3.41 (95% CI 2.19–5.31) for ≥ 3 falls. In supplementary analyses, we tested for linear trend related to number of previous falls and this was significant in all models (P < 0.005). Mortality also showed a gradient increase in risk with increasing number of falls, though the HRs for death were lower than the HRs for fracture.
Sex and age stratified analyses are provided in Supplementary Table 1. Tests for interactions between age (stratified as < 65 years vs ≥ 65 years and as < 65 years vs 65–79 years vs ≥ 80 years) and sex with number of falls and were non-significant (all P interaction > 0.1). Supplementary analysis according to number of previous falls up to a maximum of 5 did not show any further increase in risk after three 3 falls (Supplementary Table 2).
Discussion
We documented that a simple question regarding self-reported falls in the previous year could be easily collected during routine clinical practice and that this information was strongly predictive of short-term fracture risk independent of multiple clinical risk factors including fracture probability using the FRAX tool with BMD. Moreover, there was evidence of dose–response with increasing risk as a function of the number of previous falls. One in five individuals reported a fall in the previous year, with one in twelve reporting multiple falls. This prevalence of falls is within the range of previous reports, providing face validity for the information collected [6, 10, 18, 30]. There was very low correlation between number of previous falls and other baseline characteristics, including age, sex, BMI, femoral neck T-score, and fracture probability. This is consistent with the minimal attenuation observed in the covariate-adjusted models and independent information provided by falls history.
It is noteworthy that other cohorts, including the original Dubbo cohort used for developing the Garvan algorithm and the validation study using the CaMos cohort, modeled fracture risk per fall [18]. Neither of these studies had sufficient statistical power to examine numbers of falls as discrete categories (1, 2, 3, or more). Assumptions that falls risk would be additive in the model are confirmed in the current analysis where there is clear evidence of dose–response. Our findings also complement data from the Norwegian Nord-Trondelag Health Study (HUNT 3) which included 3687 women and 3025 men age 70–90 years [30]. This study confirmed that self-reported falls were an independent risk factor for fracture in women (HR 1.64, 95% CI 1.20–2.24) but not among men (HR 1.09, CI 0.65–1.83). Falls prevalence in this study (22.1% among women, 17.5% among men) was similar to our study. However, the HUNT3 study did not have information regarding BMD or non-hip fractures and did not collect fall information in individuals aged < 70 years. Our findings expand the age range over which falls history is useful and did not identify significant interaction with age or sex.
A previous report from the International Society for Clinical Densitometry/International Osteoporosis Foundation Task Force suggested that FRAX probability could be modified to account for falls history using a multiplication factor of 1.3 for each past fall (up to 5 falls) [5]. This would imply risk adjustments of 1.3 for a single fall, 1.7 for two falls, and 2.2 for three falls, values that are within the confidence limits of our study (Table 3). The multiplication factor of 1.3 was based upon the univariate HR for incident hip fracture in White women with a past fall derived from the Study of Osteoporotic Fractures, which had a wide confidence interval (1.1–1.5), and became statistically non-significant after adjustment for poor health and markers of poor mobility [31]. Our data show a gradient of risk up to 3 previous falls but not beyond that, suggesting that this adjustment should be limited to a maximum of 3 falls. This may be a reflection of a small number of individuals with 4 and 5 or more falls, or an individual’s difficulty to precisely recall numbers of fall events in the prior year after they exceed 3.
Strengths of our study include broad inclusion criteria, which are representative of women and men seen in routine clinical practice for assessment of bone health [17]. Our results are therefore likely to be of direct applicability to clinical practice and complement existing data from prospective research cohorts and clinical trials. We also acknowledge several limitations. Falls information is intrinsically dynamic, and we do not have information on falls that occurred more than 1 year before BMD testing or during follow-up. Previous studies have suggested that there is a significant interaction between previous falls and observation time for both prediction of incident falls and prediction of incident fracture, such that this risk diminishes over time [10, 32]. Since the mean follow-up in our cohort was relatively brief (2.7 years), it was not possible to assess this interaction. Similarly, previous falls are associated with increased mortality which may attenuate long-term risk; this is an important consideration in modeling 10-year fracture probability in the presence of competing mortality. Our assessment of falls was based upon a relatively simple question construct, and it is possible that more detailed questioning within the framework of a research protocol might have extracted more detailed information such as the mechanism and severity of the fall or fall-related injuries [33]. However, inaccurate recording of falls would likely bias our results towards the null, which are therefore conservative. Moreover, the question construct is likely to be of greater relevance for routine clinical practice where data collection processes must be simple. The frequency of self-reported falls that we observed is comparable to many other cohorts, providing face validity for the measurement [6, 10, 18, 30]. We did not detect significant interactions between sex and age, but power to detect weaker interactions may be limited by the small number of men and individuals aged > 85 years. Finally, fracture outcomes were assessed through population-based healthcare data sources rather than X-ray review. However, we have previously shown that the definitions used have high validity when compared with X-ray [28, 29].
In summary, a simple question construct regarding number of falls in the previous year is strongly associated with incident fracture risk in routine clinical practice. This risk is independent of age, sex, BMD, and baseline fracture probability. Moreover, there is dose–response with multiple falls (up to a maximum of 3) conferring greater risk than a single fall. These data provide further impetus to incorporate fall history into future iterations of FRAX so that this information can guide clinical management of patients at high risk for incident fracture.
References
Compston JE, McClung MR, Leslie WD (2019) Osteoporosis. Lancet 393(10169):364–376
Kanis JA, Harvey NC, Cooper C, Johansson H, Oden A, McCloskey EV et al (2016) A systematic review of intervention thresholds based on FRAX: a report prepared for the National Osteoporosis Guideline Group and the International Osteoporosis Foundation. Arch Osteoporos 11(1):25
Kanis JA.2007 Assessment of osteoporosis at the primary health-care level. Technical Report. Accessible at http://www.shef.ac.uk/FRAX/pdfs/WHO_Technical_Report.pdf.: Published by the University of Sheffield
Kanis JA, Hans D, Cooper C, Baim S, Bilezikian JP, Binkley N et al (2011) Interpretation and use of FRAX in clinical practice. Osteoporos Int 22(9):2395–2411
Masud T, Binkley N, Boonen S, Hannan MT, Members FPDC (2011) Official positions for FRAX(R) clinical regarding falls and frailty: can falls and frailty be used in FRAX(R)? From Joint Official Positions Development Conference of the International Society for Clinical Densitometry and International Osteoporosis Foundation on FRAX(R). J Clin Densitom 14(3):194–204
Nguyen ND, Frost SA, Center JR, Eisman JA, Nguyen TV (2008) Development of prognostic nomograms for individualizing 5-year and 10-year fracture risks. Osteoporos Int 19(10):1431–1444
Nguyen ND, Frost SA, Center JR, Eisman JA, Nguyen TV (2007) Development of a nomogram for individualizing hip fracture risk in men and women. Osteoporos Int 18(8):1109–1117
Hippisley-Cox J, Coupland C.2011 Validation of QFracture compared with FRAX: analysis prepared for NICE 2011.
Hippisley-Cox J, Coupland C (2012) Derivation and validation of updated QFracture algorithm to predict risk of osteoporotic fracture in primary care in the United Kingdom: prospective open cohort study. BMJ. 344:e3427
Harvey NC, Oden A, Orwoll E, Lapidus J, Kwok T, Karlsson MK et al (2017) Falls predict fractures independently of FRAX probability: a meta-analysis of the osteoporotic fractures in men (MrOS) study. J Bone Miner Res
Su Y, Leung J, Kwok T.2017 The role of previous falls in major osteoporotic fracture prediction in conjunction with FRAX in older Chinese men and women: the Mr. OS and Ms. OS cohort study in Hong Kong. Osteoporos Int.
Melton LJ 3rd, Atkinson EJ, Achenbach SJ, Kanis JA, Therneau TM, Johansson H et al (2012) Potential extensions of the US FRAX algorithm. J Osteoporos 2012:528790
Black DM, Steinbuch M, Palermo L, Dargent-Molina P, Lindsay R, Hoseyni MS, Johnell O (2001) An assessment tool for predicting fracture risk in postmenopausal women. Osteoporos Int 12(7):519–528
Kayan K, Johansson H, Oden A, Vasireddy S, Pande K, Orgee J, Kanis JA, McCloskey EV (2009) Can fall risk be incorporated into fracture risk assessment algorithms: a pilot study of responsiveness to clodronate. Osteoporos Int 20(12):2055–2061
Zhao R, Feng F, Wang X (2017) Exercise interventions and prevention of fall-related fractures in older people: a meta-analysis of randomized controlled trials. Int J Epidemiol 46(1):149–161
Leslie WD, Metge C (2003) Establishing a regional bone density program: lessons from the Manitoba experience. J Clin Densitom 6(3):275–282
Leslie WD, Caetano PA, Macwilliam LR, Finlayson GS (2005) Construction and validation of a population-based bone densitometry database. J Clin Densitom 8(1):25–30
Langsetmo L, Nguyen TV, Nguyen ND, Kovacs CS, Prior JC, Center JR, Morin S, Josse RG, Adachi JD, Hanley DA, Eisman JA, the Canadian Multicentre Osteoporosis Study Research Group (2011) Independent external validation of nomograms for predicting risk of low-trauma fracture and hip fracture. CMAJ. 183(2):E107–E114
Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston Jr CC, Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8(5):468–489
Kanis JA, Oden A, Johansson H, Borgstrom F, Strom O, McCloskey E (2009) FRAX and its applications to clinical practice. Bone. 44(5):734–743
Leslie WD, Lix LM, Langsetmo L, Berger C, Goltzman D, Hanley DA, Adachi JD, Johansson H, Oden A, McCloskey E, Kanis JA (2011) Construction of a FRAX(R) model for the assessment of fracture probability in Canada and implications for treatment. Osteoporos Int 22(3):817–827
Bisson EJ, Finlayson ML, Ekuma O, Marrie RA, Leslie WD (2019) Accuracy of FRAX(R) in people with multiple sclerosis. J Bone Miner Res
Leslie WD, Morin SN, Lix LM, Niraula S, McCloskey EV, Johansson H et al (2019) Performance of FRAX in women with breast cancer initiating aromatase inhibitor therapy: a registry-based cohort study. J Bone Miner Res
Peschken CA, Hitchon CA, Garland A, Bernstein CN, Chen H, Fransoo R, Marrie RA (2016) A population-based study of intensive care unit admissions in rheumatoid arthritis. J Rheumatol 43(1):26–33
Yang S, Leslie WD, Yan L, Walld R, Roos LL, Morin SN, Majumdar SR, Lix LM (2016) Objectively verified parental hip fracture is an independent risk factor for fracture: a linkage analysis of 478,792 parents and 261,705 offspring. J Bone Miner Res 31(9):1753–1759
Leslie WD, Lix LM, Johansson H, Oden A, McCloskey E, Kanis JA, Manitoba Bone Density Program (2010) Independent clinical validation of a Canadian FRAX tool: fracture prediction and model calibration. J Bone Miner Res 25(11):2350–2358
Fraser LA, Langsetmo L, Berger C, Ioannidis G, Goltzman D, Adachi JD et al (2011) Fracture prediction and calibration of a Canadian FRAX(R) tool: a population-based report from CaMos. Osteoporos Int 22(3):829–837
Lix LM, Azimaee M, Osman BA, Caetano P, Morin S, Metge C, Goltzman D, Kreiger N, Prior J, Leslie WD (2012) Osteoporosis-related fracture case definitions for population-based administrative data. BMC Public Health 12:301
Epp R, Alhrbi M, Ward L, Leslie WD (2018) Radiological validation of fracture definitions from administrative data. J Bone Miner Res 33(Supp 1):S275
Hoff M, Meyer HE, Skurtveit S, Langhammer A, Sogaard AJ, Syversen U, et al.2017 Validation of FRAX and the impact of self-reported falls among elderly in a general population: the HUNT study, Norway. Osteoporos Int.
Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM (1995) Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med 332(12):767–773
Harvey NC, Johansson H, Oden A, Karlsson MK, Rosengren BE, Ljunggren O et al (2016) FRAX predicts incident falls in elderly men: findings from MrOs Sweden. Osteoporos Int 27(1):267–274
Teister CJ, Chocano-Bedoya PO, Orav EJ, Dawson-Hughes B, Meyer U, Meyer OW, Freystaetter G, Gagesch M, Rizzoli R, Egli A, Theiler R, Kanis JA, Bischoff-Ferrari HA (2018) Which method of fall ascertainment captures the most falls in prefrail and frail seniors? Am J Epidemiol 187(10):2243–2251
Acknowledgments
The authors acknowledge the Manitoba Centre for Health Policy for use of data contained in the Population Health Research Data Repository (HIPC 2016/2017-29). SNM is chercheur-boursier des Fonds de Recherche du Québec en Santé. LML is supported by a Tier I Canada Research Chair.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Health Research Ethics Board for the University of Manitoba.
Conflicts of interest
Suzanne Morin: Nothing to declare for the context of this paper, but has received research grants from Amgen, Merck.
Eugene McCloskey: Nothing to declare for the context of this paper, but numerous ad hoc consultancies/speaking honoraria and/or research funding from Amgen, Bayer, General Electric, GSK, Hologic, Lilly, Merck Research Labs, Novartis, Novo Nordisk, Nycomed, Ono, Pfizer, ProStrakan, Roche, Sanofi-Aventis, Servier, Tethys, UBS, and Warner Chilcott.
Nicholas Harvey: Nothing to declare for the context of this paper, but has received consultancy/ lecture fees/honoraria/ grant funding from Alliance for Better Bone Health, Amgen, MSD, Eli Lilly, Servier, Shire, Consilient Healthcare, and Internis Pharma.
John A. Kanis: Grants from Amgen, Lilly, Radius Health and non-financial support from Medimaps outside the submitted work.
William Leslie, Patrick Martineau, Mark Bryanton, Lisa Lix, Helena Johansson: No conflicts of interest.
Disclaimer
The results and conclusions are those of the authors and no official endorsement by the Manitoba Centre for Health Policy, Manitoba Health, Seniors and Active Living, or other data providers is intended or should be inferred. This article has been reviewed and approved by the members of the Manitoba Bone Density Program Committee.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOC 49 kb)
Rights and permissions
About this article
Cite this article
Leslie, W., Morin, S., Lix, L. et al. Fracture prediction from self-reported falls in routine clinical practice: a registry-based cohort study. Osteoporos Int 30, 2195–2203 (2019). https://doi.org/10.1007/s00198-019-05106-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-019-05106-3