Abstract
Summary
The number of individuals aged 50 years or more at high risk of osteoporotic fracture worldwide in 2010 was estimated at 158 million and is set to double by 2040.
Introduction
The aim of this study was to quantify the number of individuals worldwide aged 50 years or more at high risk of osteoporotic fracture in 2010 and 2040.
Methods
A threshold of high fracture probability was set at the age-specific 10-year probability of a major fracture (clinical vertebral, forearm, humeral or hip fracture) which was equivalent to that of a woman with a BMI of 24 kg/m2 and a prior fragility fracture but no other clinical risk factors. The prevalence of high risk was determined worldwide and by continent using all available country-specific FRAX models and applied the population demography for each country.
Results
Twenty-one million men and 137 million women had a fracture probability at or above the threshold in the world for the year 2010. The greatest number of men and women at high risk were from Asia (55 %). Worldwide, the number of high-risk individuals is expected to double over the next 40 years.
Conclusion
We conclude that individuals with high probability of osteoporotic fractures comprise a very significant disease burden to society, particularly in Asia, and that this burden is set to increase markedly in the future. These analyses provide a platform for the evaluation of risk assessment and intervention strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Global Burden of Disease study demonstrated a massive impact of musculoskeletal conditions on populations worldwide [1–3]. The associated expenditure is equivalent to 3 % of gross national product annually [WHO 2003]. Musculoskeletal illness is the second greatest cause of years lived with disability globally [1] and accounts for 6.8 % of total disability-adjusted life years worldwide; this figure has risen by 45 % since 1990, in contrast to the mean rise of 33 % for other disease areas [2]. The contribution of osteoporosis and associated fractures to the burden worldwide has been characterised in terms of specific fracture sites [4–7], bone mineral density [8], life years lost and disability-adjusted life years lost [6, 7]. Although defining osteoporosis burden by the occurrence of hip, or other fractures, or consequent disability has the merit of being based on discreet events, it may be more helpful for disease prevention to consider the burden in terms of those at high risk of a future fracture, that is, the population to whom treatment might be usefully administered [9].
Historically, the World Health Organization’s classification of osteoporosis, based on the measurement of BMD [10], has served as the framework for characterisation of a high fracture risk individual (defined, operationally, as a T-score of −2.5 or below, with BMD at the femoral neck as the international reference standard [11]). Whereas these criteria have commonly provided intervention thresholds for the treatment of osteoporosis, the development of risk assessment algorithms has shown that prevention of fractures is better targeted on the basis of fracture probability using multiple risk factors rather than BMD alone [9, 12]. Probability-based thresholds have been recommended by the Committee for Medicinal Products for Human Use (CHMP) and many assessment guidelines [13–15], with FRAX® being the tool most widely used globally to generate fracture probabilities [16].
The advent of FRAX has permitted intervention thresholds to be based on fracture probability, i.e. the probability above which treatment can be recommended, and in many countries (including North America for spine and hip fracture), the view is taken that treatment can be recommended in women with a prior fragility fracture. Thus, the FRAX probability equivalent to that conferred by a prior fracture may be used to categorise a patient as high fracture risk. Indeed, such approach has been adopted in the UK by the National Osteoporosis Guideline Group (NOGG) [17], and in European Guidance [18, 19], country-specific guidelines [17, 20–27] and in Health Technology Assessment of the burden of disease [15, 28, 29]. Thus, the aim of the present study was, using FRAX, to estimate the burden of disease worldwide in terms of high fracture probability.
Methods
Fracture threshold
We defined the threshold of high fracture probability as the age-specific 10-year probability of a major fracture (clinical vertebral, forearm, humeral and hip fracture) which was equivalent to that of a woman with a prior fragility fracture and no other clinical risk factors. For the purposes of this report, this threshold was termed the ‘fracture threshold’. Probabilities at the fracture threshold were calculated from the age of 50 years in 5-year age intervals without the inclusion of BMD, and body mass index was set to 24 kg/m2. Note that the threshold varies with age. The identical age-specific threshold was used for men. The principal reason for using the same probability thresholds in men as used in women is that men at high risk are categorised in guidelines in this manner. The argument for this position is not only that of equity but also that the cost-effectiveness of intervention at any given probability is very similar in men compared with women [30, 31].
Since the risk of fracture varies from country to country, as does the risk of death [32], fracture probability also varies. For this reason, an age- and sex-specific probability-based definition of high risk was calculated for each country where a FRAX model was available using FRAX (version 3.8).
Disease burden
The proportion of men and women who exceed the probability threshold for fracture was computed from the distribution of the risk score among the cohorts used to develop FRAX. The proportion of men and women in each country who exceeded the probability threshold was derived from the independent correlations (calculated mathematically) of the normalised distributions of the risk scores for hip fracture, other major osteoporotic fractures and death. The number of men and women at or above the fracture threshold was determined from the population demography for each country using UN data for 2010 [33] (medium variant) in 5-year age intervals from the age of 50 years with an upper age category of 95 + years.
Countries where a FRAX model was available were categorised by geographical region (Table 1). Where more than one FRAX model was available for a country (the USA and Singapore), the model representing the largest population was used (Caucasian and Chinese, respectively). FRAX models were available for 53 countries (March 2014) that represented 79 % of the world population aged 50 years or more. The coverage of the regions ranged from 7 % in Africa to 100 % in North America.
To determine the burden of high fracture probability by region, we assumed that the population-weighted proportion of men and women above the fracture threshold in FRAX countries was representative of each region. The number of men and women at or above the fracture threshold was determined from the population demography for each region using UN data for 2010 (medium variant) in 5-year age intervals [33].
Projections beyond 2010
The burden of disease, as measured by the number of men and women at or above the fracture threshold, was estimated from the future population projections up to 2040 in each geographical region using the medium variant of UN projections [33].
Results
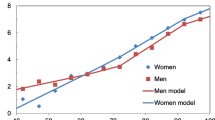
The number of men and women at or above the fracture threshold for each region is given in Table 2. Approximately 21 million men and 137 million women aged 50 years or more across the world had a fracture probability at or above the fracture threshold for the year 2010. The highest number of individuals above the fracture threshold was in Asia with more than 11 million men and 73 million women, respectively, comprising 55 and 54 % of all men and women aged 50 years identified at risk. Men and women in Europe accounted for 17 and 22 % of the global burden, respectively. In each of the other regions, the global burden was less than 10 % of the total. The proportion of the population above the fracture threshold increased with age. The increase with age was not marked in men but rose progressively with age in women. In the age range 50–54 years, 11.9 % exceeded the threshold and this rose progressively with age to 30 % in the age group 80–84 years (Fig. 1).
Over all ages, the female to male ratio was 6.6 worldwide, ranging from 5.1 in Africa to 8.4 in Europe (Table 3). In all regions, the ratio of female to male at risk increased at older ages, reflecting the greater longevity of women compared with men. This was also reflected in lower geographic variation in the female to male ratios at younger ages but a much greater variation in the population aged 85+; here, the ratios ranged from 6.4 in Africa to 18.4 in Europe.
Globally, 3.1 % of men and 18.2 % of women had a fracture probability above the fracture threshold (see Fig. 1). Again, there was some variation by continent with the highest proportion of the female population aged 50 years or more in Oceania and Europe (20.6 and 20.2 %, respectively) and the lowest in Africa and Asia (16.7 and 17.7 %, respectively).
Based on expected demographic changes, the number of men and women exceeding the fracture threshold is expected to increase twofold from 157 million in 2010 to 319 million over a 30-year interval (Fig. 2). Increases were noted for all regions but were particularly marked in Africa and Latin America. The most modest rise (by 30 %) was seen for Europe (Fig. 3). As expected (see Table 2), Asia had the highest proportion of the global burden (59.9 % in women), followed by Europe (14.0 %), Latin America (9.7 %), Africa (9.2 %), North America (6.5 %) and Oceania (0.7 %). The respective share in men was 58.5, 11.2, 10.3, 2.8, 6.3 and 0.8 %.
Discussion
To our knowledge, this is the first attempt to estimate the global burden of disease in terms of fracture probability and complements previous studies which have quantified the burden by hip fracture [4–6], major osteoporotic fracture [7], osteoporosis based on densitometry [8], or disability-adjusted life years and life years lost [6, 7].
We defined the threshold of high fracture probability as the age-specific 10-year probability of a major fracture (clinical vertebral, forearm, humeral or hip fracture), which was equivalent to that of a woman with a BMI of 24 kg/m2 and a prior fragility fracture but no other clinical risk factors. As noted in the introduction, the same threshold is used directly or indirectly in many assessment guidelines. Under the assumptions used for this study, we estimated that there were approximately 21 million men and 137 million women worldwide that had a fracture probability at or above this threshold in 2010 of which a majority (55 %) came from Asia. The high prevalence in Asia is consistent with the preponderance of major fractures that are found in Asia [4, 5]. As might be expected, these figures exceed the 56.2 million major osteoporotic fractures estimated worldwide in 2000 [7] which for the year 2010 may be uplifted to 74.2 million, as judged by the population growth. Given that major fractures account for 60–65 % of all osteoporotic fractures depending on age [34], the number of fragility fractures in 2010 is likely to exceed 120 million. These considerations indicate that a large majority of individuals at high risk (at or above a fracture threshold) have already sustained a fragility fracture. This view is supported by an analysis in the UK where approximately 93 % of women identified in this way had sustained a prior fragility fracture [35]. The changes in population demography suggest that the numbers at high risk will double over the next 40 years.
The present estimates provide a platform on which to evaluate the impact of assessment strategies. For example, screening of women from the age of say 65 years with FRAX (without a BMD test) would identify 72.8 million women (28 % of all women aged 50 years or more) representing 53 % of the postmenopausal population at high risk (see Table 2). Additionally, the methodology could be extended to assessing the potential impact of intervention using a “high-risk” strategy (targeting intervention to those at high risk) or a global strategy to decrease fracture probability in populations such as in postmenopausal women.
The present study relies on a number of assumptions that may affect the reliability of our estimates. The assessment is based on the availability and adequacy of FRAX models and the assumption that in each region, the available models are representative of the region as a whole. Overall, the countries with a FRAX model cover 79 % of the world population but FRAX models in Africa (Morocco and Tunisia) account for only 7 % of the African population. Moreover, the fracture probabilities in North Africa are likely to overestimate those in the rest of the continent. The global impact is likely to be small because of the low fracture probabilities and modest population size. More complete information is available for high-risk countries in the developed world.
A further consideration relates to the construct of the FRAX models. The majority of the FRAX models rely on the assumption that the age- and sex-specific incidence of clinical spine, forearm and proximal humerus fractures can be derived from hip fracture rates [14]. This assumption seems to be reasonable, at least in the Western world, but it may not hold true for morphometric vertebral fractures [36, 37]. With regard to clinical vertebral fracture, there is a high correlation between hip fracture rates and admission to hospital for vertebral fracture such that vertebral fracture discharges are high in those regions where the incidence of hip fracture is also high [38, 39]. A recent long-term prospective study of the incidence of major fractures in Iceland has shown the reliable prediction of other major fractures from hip fracture rates [40]. Similar data have been reported in a North American cohort [41]. These limitations point to the need for more epidemiological information on fracture rates and their inter-relationships worldwide.
The threshold for high risk that we chose for the present study is intuitively appealing, representing the age-specific probability equivalent to a woman with a prior fracture. Many guidelines suggest that women with a prior fracture (limited to hip or spine fractures in some countries) merit intervention on this basis. Notwithstanding, the threshold is arbitrary. In this regard, it is notable that the threshold used for men was the same as that used in women which resulted in a somewhat stable prevalence of the high-risk category. Other thresholds, such as a fracture probability of 5, 10 and 20 %, are alternatives that have been partially explored [28, 42]. Our projection for the doubling of individuals at high risk depends on the adequacy of the future demographic shifts. Although uncertain, it is relevant to note that all individuals who will be aged 50 years or more in 40 years’ time have already been born. Thus, barring major catastrophes, the population projections are relatively robust. We have, however, not factored in secular changes in fracture probability, which may variously increase, decrease or remain stable over this period.
With these caveats, the present data suggest that individuals with high probability of osteoporotic fractures comprise a very significant disease burden to society, particularly in Asia, and are set to increase markedly in the future.
References
Vos T, Flaxman AD, Naghavi M et al (2012) Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study. 2010. Lancet 380(9859):2163–2196
Murray CJ, Vos T, Lozano R et al (2012) Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859):2197–2223
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H et al (2012) A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380:2224–2260
Cooper C, Campion G, Melton LJ III (1992) Hip fractures in the elderly: a world-wide projection. Osteoporos Int 2:285–289
Gullberg B, Johnell O, Kanis JA (1997) World-wide projections for hip fracture. Osteoporos Int 7:407–413
Johnell O, Kanis JA (2004) An estimate of the world-wide prevalence, disability and mortality associated with hip fracture. Osteoporos Int 15:897–902
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733
Odén A, McCloskey EV, Johansson H, Kanis JA (2013) Assessing the impact of osteoporosis on the burden of hip fractures. Calcif Tissue Int 92:42–49
Kanis JA, Oden A, Johnell O, Johansson H, De Laet C, Brown J et al (2007) The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int 18:1033–1046
Kanis JA, Melton LJ 3rd, Christiansen C, Johnston CC, Khaltaev N (1994) The diagnosis of osteoporosis. J Bone Miner Res 9:1137–1141
Kanis JA, McCloskey EV, Johansson H, Oden A, Melton LJ 3rd, Khaltaev N (2008) A reference standard for the description of osteoporosis. Bone 42:467–475
Johansson H, Kanis JA, Oden A, Compston J, McCloskey E (2012) A comparison of case-finding strategies in the UK for the management of hip fractures. Osteoporos Int 23:907–915
Committee for Medicinal Products for Human Use (CHMP) (2006) Guideline on the evaluation of medicinal products in the treatment of primary osteoporosis. Ref CPMP/EWP/552/95Rev.2. London, CHMP. Nov 2006
Kanis JA, Hans D, Cooper C, and the Task Force of the FRAX Initiative et al (2011) Interpretation and use of FRAX in clinical practice. Osteoporos Int 22:395–411
Kanis JA, Borgström F, Compston J, Dreinhöfer K, Nolte E, Jonsson L, Lems WF, McCloskey EV, Rizzoli R, Stenmark J (2013) SCOPE: a scorecard for osteoporosis in Europe. Arch Osteoporos 8:144. doi:10.1007/s11657-013-0144-1
Kanis JA, Johansson H, Oden A, Cooper C, McCloskey EV, and the Epidemiology and Quality of Life Working Group of IOF (2013) Worldwide uptake of FRAX. Arch Osteoporos 8:166. doi:10.1007/s11657-013-0166-8
Compston J, Cooper A, Cooper C, on behalf of the National Osteoporosis Guideline Group (NOGG) et al (2009) Guidelines for the diagnosis and management of osteoporosis in postmenopausal women and men from the age of 50 years in the UK. Maturitas 62:105–108
Lekawasam S, Adachi JD, Agnusdei D, Bilezikian J, Boonen S, Borgström F, for the Joint IOF-ECTS GIO Guidelines Working Group et al (2012) A framework for the development of guidelines for the management of glucocorticoid-induced osteoporosis. Osteoporos Int 23:2257–2276
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster J-Y, on behalf of the Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the Committee of Scientific Advisors of the International Osteoporosis Foundation ( IOF) (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24:23–57
Briot K, Cortet B, Thomas T et al (2012) 2012 update of French guidelines for the pharmacological treatment of postmenopausal osteoporosis. Bone Joint Spine 79:304–313
Grigorie D, Sucaliuc A, Johansson H, Kanis JA, McCloskey E (2013) The application of FRAX® to determine intervention thresholds for osteoporosis in Romania. Arch Osteoporos 8:164
Johansson H, Kanis JA, McCloskey EV, Odén A, Devogelaer J-P, Kaufman J-M, Neuprez A, Hiliigsmann M, Bruyere O, Reginster JY (2010) A FRAX® model for the assessment of fracture probability in Belgium. Osteoporos Int 22:453–461
Kanis JA (2013) Commentary on guidelines on postmenopausal osteoporosis—Indian Menopause Society. J Midlife Health 4:129–131
Lekamwasam S (2013) Sri Lankan FRAX model and country specific intervention thresholds. Arch Osteoporos 8(1-2):148. doi:10.1007/s11657-013-0148-x
Lippuner K, Johansson H, Kanis JA, Rizzoli R (2010) FRAX® assessment of osteoporotic fracture probability in Switzerland. Osteoporos Int 21:381–390
McGowan B, Kanis JA, Johansson H, Silke C, Whelan B (2013) Development and use of FRAX in the management of osteoporosis in Ireland. Arch Osteoporos 8(1-2):146. doi:10.1007/s11657-013-0146-z
Russian Association on Osteoporosis (2013) http://www.osteoporoz.ru/content/view/891/113/
Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J et al (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:136. doi:10.1007/s11657-013-0136-1
Strom O, Borgström F, Kanis JA, Compston JE, Cooper C, McCloskey E et al (2011) Osteoporosis: burden, health care provision and opportunities in the EU. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 6:59–155. doi:10.1007/s11657-011-0060-1
Lippuner K, Johansson H, Borgström F, Kanis JA, Rizzoli R (2012) Cost-effective intervention thresholds against osteoporotic fractures based on FRAX® in Switzerland. Osteoporos Int 23:2579–2589
Kanis JA, Brazier JE, Stevenson M, Calvert NW, Lloyd Jones M (2002) Treatment of established osteoporosis: a systematic review and cost-utility analysis. Health Technol Assess 6(29):1–255
Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl D, Cyrus Cooper C, on behalf of the IOF Working Group on Epidemiology and Quality of Life (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23:2239–2256
United Nations (2010) World Population prospects, the 2010 revision. Department of Economic and Social Affairs, UN (http://esa.un.org/unpd/wpp/unpp/panel_indicators.htm) Accessed Feb 2014
Kanis JA, Oden A, Johnell O, Jonsson B, de Laet C, Dawson A (2001) The burden of osteoporotic fractures: a method for setting intervention thresholds. Osteoporos Int 12:417–427
Johansson H, Kanis JA, Oden A, Compston J, McCloskey E (2012) A comparison of case-finding strategies in the UK for the management of hip fractures. Osteoporos Int 23:907–915
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359:1761–1767
Felsenberg D, Silman AJ, Lunt M et al (2002) Incidence of vertebral fracture in Europe: results from the European Prospective Osteoporosis Study Epos. J Bone Min Res 17:716–724
Johnell O, Gullberg B, Kanis JA (1977) The hospital burden of vertebral fracture in Europe: a study of national register sources. Osteoporos Int 7:138–144
Johnell O, Kanis JA (2005) Epidemiology of osteoporotic fractures. Osteoporos Int 16(suppl 2):S3–S7
Siggeirsdottir K, Aspelund T, Johansson H, Gudmundsson EF, Mogensen B, Jonsson BY et al (2014) The incidence of a first major osteoporotic fracture in Iceland and implications for FRAX. Osteoporos Int 25:2445–2451
Lam A, Leslie WD, Lix LM, Yogendran M, Morin SN, Majumdar SR (2014) Major osteoporotic to hip fracture ratios in Canadian men and women with Swedish comparisons: a population-based analysis. J Bone Miner Res 29:1067–1073
Kanis JA, Johansson H, Odén A, McCloskey EV (2012) The distribution of FRAX® based probabilities in women from Japan. J Bone Miner Metab 30:700–705
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Odén, A., McCloskey, E.V., Kanis, J.A. et al. Burden of high fracture probability worldwide: secular increases 2010–2040. Osteoporos Int 26, 2243–2248 (2015). https://doi.org/10.1007/s00198-015-3154-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3154-6