Abstract
Summary
Decreasing the daily dose of glucocorticoids improved bone metabolic marker levels in patients with rheumatoid arthritis. However, changes in disease activity did not influence bone metabolism. Bone metabolism might thus remain uncontrolled even if disease activity is under good control. Decreasing glucocorticoid dosage appears important for improving bone metabolism.
Introduction
Patients with rheumatoid arthritis (RA) develop osteoporosis more frequently than healthy individuals. Bone resorption is increased and bone formation is inhibited in patients with RA, and glucocorticoid negatively affects bone metabolism. We aimed to investigate factors influencing bone metabolic markers in patients with RA.
Methods
We started the 10-year prospective cohort Total Management of Risk Factors in Rheumatoid Arthritis Patients to Lower Morbidity and Mortality (TOMORROW) study in 2010. We compared changes in urinary cross-linked N-telopeptide of type I collagen (uNTx) and serum osteocalcin (OC), as markers of bone resorption and formation, respectively, in 202 RA patients and age- and sex-matched volunteers between 2010 and 2011. We also investigated factors influencing ΔuNTx and ΔOC in the RA group using multivariate analysis.
Results
Values of ΔuNTx were significantly lower in patients with RA than in healthy controls (−0.51 vs. 7.41 nmol bone collagen equivalents (BCE)/mmol creatinine (Cr); p = 0.0013), whereas ΔOC values were significantly higher in RA patients (0.94 vs. 0.37 ng/ml; p = 0.0065). Changes in prednisolone dosage correlated negatively with ΔOC (β = −0.229, p = 0.001), whereas changes in disease activity score, bisphosphonate therapy, and period of biologics therapy did not correlate significantly with ΔOC. No significant correlation was seen between ΔuNTx and change in prednisolone dosage.
Conclusions
Decreased glucocorticoid dosage improved bone metabolic markers in RA, but disease activity, bisphosphonate therapy, and period of biologics therapy did not influence levels of bone metabolic markers. Decreasing glucocorticoid dosage appears important for improving bone metabolic marker profiles in patients with RA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is one of the most important complications in patients with rheumatoid arthritis (RA) [1], increasing the risk of hip and vertebral fractures by about twofold to sixfold in patients with RA compared to controls [2–4]. Hip and vertebral fracture leads to decreased activities of daily living, particularly in elderly patients [5]. Previous studies have shown that the frequency of osteoporosis is 15–20 % at the hip and spine in patients with RA [6, 7].
Bone metabolism in patients with RA is exposed to some unexpected influences. Pro-inflammatory cytokines, such as tumor necrosis factor (TNF)-α, interleukin (IL)-1, IL-6, and IL-17, correlate strongly with bone loss induced by osteoclastogenesis and bring about peri-articular osteoporosis [8]. Disuse following joint destruction leads to systemic osteoporosis. Oral glucocorticoids are known to exert harmful effects on bone [9, 10] but are frequently used in the treatment of RA to suppress inflammation. It is also necessary to consider osteoporosis with increasing age. In particular, use of glucocorticoids has been reported to increase the risk of fractures through secondary osteoporosis [9]. In the case of using or planning to use oral glucocorticoids (prednisolone (PSL) equivalents ≥5 mg/day) for 3 months or longer, general guidance and drug treatment have been recommended [11, 12]. Conversely, biological disease-modifying anti-rheumatic-drugs (bDMARDs) not only decrease disease activity and protect against joint destruction but also improve bone metabolic marker profiles [13].
We have started a prospective cohort study to examine the risk factors affecting osteoporosis in patients with RA. The aim of this study was to investigate changes in bone metabolic marker levels among patients with RA by comparison with those in age- and sex-matched controls. We also clarified factors influencing bone metabolic markers in patients with RA.
Materials and methods
Study design and subjects
The current analysis is a part of a prospective 10-year cohort study (Total Management of Risk Factors in Rheumatoid Arthritis Patients to Lower Morbidity and Mortality, TOMORROW study) being conducted from 2010 to 2020. The study was registered with the UMIN Clinical Trials Registry [http://www.umin.ac.jp/ctr/] (UMIN000003876). The TOMORROW study is designed to evaluate risk factors associated with osteoporosis and metabolic syndrome in patients with RA.
This study included 208 patients with RA (177 women, 31 men) at the Osaka City University Hospital and 205 age- and sex-matched healthy volunteers (172 women, 33 men) recruited through mass media (total, 413 subjects). All patients with RA were between 20 and 79 years old and fulfilled the American College of Rheumatology (ACR) criteria (1987) for RA [14]. Distributions of age and sex were matched with general clinical practice. The ethics committee of Osaka City University Medical School approved the study protocol. Written informed consent was obtained from all patients and volunteers in accordance with the Declaration of Helsinki.
Clinical assessment
Clinical and laboratory data were collected in January to March of 2010 at the first visit and in January to March of 2011 as the second visit. During the observation period, patients were treated according to clinical disease activity by their rheumatologist. All participants completed a self-administered questionnaire on general health status, all past history of comorbidities, and present and past medications. RA activity was measured using the disease activity score (DAS) composite index using erythrocyte sedimentation rate (ESR), applying a 28-joint score (DAS28-ESR) [15]. This index included the number of swollen and tender joints, patient’s global assessment of disease activity by visual analogue scale, and ESR. Functional status was also measured using the modified health assessment questionnaire (mHAQ) scores in patients with RA [16].
Bone metabolic markers
Levels of bone metabolic markers were measured in serum and urine obtained from each participant at approximately the same time in the morning after overnight fasting. We evaluated serum osteocalcin (OC) as the bone formation marker and urinary cross-linked N-telopeptide of type I collagen (uNTx) as the bone resorption marker. We compared data from patients with RA and healthy volunteers between 2010 and 2011 and defined the change in uNTx (ΔuNTx) as ΔuNTx = uNTx value in 2011 − uNTx value in 2010, and the change in OC (ΔOC) as ΔOC = OC value in 2011 − OC value in 2010.
Statistical analysis
Differences in demographic variables, clinical variables, OC, and uNTx between patients with RA and healthy volunteers were analyzed by applying the unpaired Student’s t test for continuous variables or the chi-square test for categorical variables. Values of ΔuNTx and ΔOC in patients with RA and healthy volunteers were compared using the unpaired Student’s t test. In RA patients, the changes in DAS28-ESR, C-reactive protein (CRP), PSL usage rate, and PSL dosage were compared using the paired Student’s t test. For patients with RA, the influences of changes in PSL dosage (ΔPSL), disease activity (ΔDAS28-ESR), use of bisphosphonates, and period of bDMARDs on bone metabolic markers were examined using Spearman correlation coefficients. Multivariate linear regression analysis was used to investigate factors influencing ΔuNTx and ΔOC. Variables entered comprised ΔPSL, ΔDAS28-ESR, use of bisphosphonates, period of bDMARDs, age, sex, disease duration, and Steinbrocker class, as factors that might affect levels of bone metabolic markers. All data are presented as mean ± standard deviation (SD). A value of p < 0.05 was considered significant. All statistical analyses were performed using the StatView version 5.0 software package (SAS Institute Japan, Tokyo, Japan).
Results
Among all subjects, six patients with RA dropped out based on the wishes of the patient (four females) or due to a change in hospitals (two females), and three healthy volunteers also chose to drop out (one female, two males). This study included 202 patients with RA (171 females, 31 males) and 202 healthy volunteers (170 females, 32 males). Baseline demographics and clinical characteristics of this study are shown in Table 1. Demographic characteristics in the two study groups were similar, because the control group subjects were recruited to match the age and sex of the RA group subjects. No significant differences in bone mineral density (BMD) using dual-energy X-ray absorptiometry were identified between the RA and control groups. However, uNTx level was significantly higher in the RA group than in the control group. The prevalence of osteoporosis (defined as BMD <0.7 g/cm2 at the lumbar spine) [17] was 10.9 % in the RA and 7.4 % in the control group. No significant differences were apparent between groups (p = 0.301, Fisher’s exact test). Bisphosphonate and oral prednisolone were more frequently used for the RA group. As characteristics of patients with RA, mean disease duration was 14.1 ± 11.8 years, mean DAS28-ESR score was 3.47 ± 1.33, and mean mHAQ score was 0.46 ± 0.44. The use rate of biologic agents was 54.5 %, because we recruited patients with RA using bDMARD treatment as half of the RA subjects, to detect long-term effects of bDMARDs on bone and lipid metabolism. Changes to disease activity and PSL dosage in patients with RA are shown in Table 2. After 1 year, DAS28-ESR and CRP were almost the same. On the other hand, the rate of PSL use had decreased to 26.7 % and the mean dosage of PSL was significantly less in 2011 than in 2010. The frequency of past fractures including fragile fracture was significantly higher in the RA group than in the control group at baseline (RA group, 40 %; control group, 24 %; p < 0.001), whereas new fractures at 1 year were seen in nine cases in the RA group (4.5 %) and in four cases in the control group (2.0 %). The frequency of new fractures was similar between groups (p = 0.259, Fisher’s exact test).
The factors influencing bone metabolic markers were detected by univariate analysis and multivariate regression analysis with a forward stepwise procedure. The factors influencing ΔuNTx were ΔOC and RA (ΔOC, β = 0.328, p < 0.0001; RA, β = −0.203, p < 0.0001), and those for ΔOC were ΔuNTx and RA (ΔuNTx, β = 0.328, p < 0.0001; RA, β = 0.191, p < 0.0001). RA was thus revealed as an independent factor influencing bone formation markers.
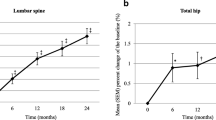
Changes in levels of bone formation markers are shown in Fig. 1. The ΔuNTx was significantly lower in the RA group than in the control group (−0.51 ± 29.4 vs. 7.41 ± 18.7 nmol bone collagen equivalents (BCE)/mmol creatinine (Cr); p = 0.0013; Fig. 1a). Values of ΔOC increased in both groups (RA, 0.94 ± 2.47 ng/ml; control, 0.37 ± 1.62 ng/ml). However, ΔOC was significantly higher in the RA group than in the control group (p = 0.0065, Fig. 1b).
In patients with RA, ΔPSL did not correlate with ΔuNTx (r = 0.07, p = 0.323, Fig. 2a) but showed a significant negative correlation with ΔOC (r = −0.227, p = 0.011, Fig. 2b). Conversely, ΔDAS28-ESR did not correlate with ΔuNTx (r = 0.099, p = 0.161, Fig 2c) and ΔOC (r = 0.033, p = 0.644, Fig. 2d) using Spearman correlation coefficients. Finally, multivariate linear regression analysis showed that ΔPSL dosage correlated negatively with ΔOC (β = −0.229, p = 0.001), whereas change of disease activity score (ΔDAS28-ESR), bisphosphonate therapy, and period of biologics therapy did not significantly correlate with ΔOC (Table 3). The analysis of factors influencing ΔuNTx found no significant correlation between ΔuNTx and any of ΔPSL dosage (r = 0.073, p = 0.312), ΔDAS28-ESR (r = −0.105, p = 0.144), bisphosphonate therapy (r = −0.035, p = 0.645), or period of biologics therapy (r = −0.064, p = 0.381).
Scatter plots for change in PSL (ΔPSL) (a, b) and DAS28-ESR (ΔDAS28-ESR) (c, d) against changes in uNTx (ΔuNTx) (a, c) and OC (ΔOC) (b, d) among patients with RA using Spearman correlation coefficients. PSL prednisolone, DAS disease activity score, ESR erythrocyte sedimentation rate, uNTx urinary cross-linked N-telopeptide of type I collagen, OC serum osteocalcin
Discussion
This study demonstrated that bone metabolic markers (uNTx as a bone resorption marker and OC as a bone formation marker) in patients with RA were improved more than those of age- and sex-matched healthy volunteers. In addition, a decrease in PSL dosage decreased markers of bone resorption and increased markers of bone formation among patients with RA. However, disease activity, bisphosphonate therapy, and period of biologics therapy did not influence bone metabolic markers.
Causes of osteoporosis in patients with RA are multifactorial and could be associated with the disease itself or decreases in physical activity [18], treatment with glucocorticoids [19], or even common postmenopausal osteoporosis [18–20]. ACR recommended bisphosphonate or teriparatide therapy and monitoring for patients with glucocorticoid-induced osteoporosis after taking glucocorticoids for over 3 months [11]. However, the effects of decreasing glucocorticoid dosage on osteoporosis in patients with RA remain unclear.
Disease activity is important for improving osteoporosis in patients with RA. Vis et al. reported that patients with good response (low disease activity) showed a slight gain in BMD of the lumbar spine and hips, whereas patients with poor response (moderate or high disease activity) showed a loss of BMD [21]. However, no significant correlation was apparent between bone metabolic markers and change in disease activity score in the present study. Baseline disease activity scores of patients with RA were relatively low (mean DAS28-ESR, 3.47) and the change of disease activity score during 1 year was small (mean ΔDAS28-ESR, 0.04), probably due to the stability of disease activity in our cohort. Bone metabolic markers have been reported to improve with bDMARDs. A previous report demonstrated that infliximab therapy increased serum osteocalcin levels [22], and tocilizumab also increased serum levels of N-terminal type I procollagen propeptide as a marker of bone formation in RA patients [23]. However, our results failed to show significant positive correlation with increases of OC and uNTx, which may be explained by the high rate of bDMARD usage (50 %) in this study. No significant difference in ΔuNTx was seen between bDMARD users (0.51 ± 29.7 nmol BCE/mmol Cr) and non-users (−1.7 ± 29.0 nmol BCE/mmol Cr; p = 0.491). The same tendency was seen for ΔOC (bDMARD users, 1.05 ± 2.43 ng/ml; non-bDMARD users, 0.81 ± 2.51 ng/ml; p = 0.591). The use of bisphosphonates might be important for osteoporosis treatment and prevention of fracture in patients with RA [24]. The rate of oral bisphosphonate use remained low in the TOMORROW study (RA, 31 %; healthy volunteers, 5 %; p < 0.001). As a result, the present study could not evaluate the efficacy of bisphosphonates in terms of bone metabolic markers in patients with RA. Glucocorticoids have been reported to inhibit the differentiation of osteoblasts, while also inducing osteoblast and osteocyte apoptosis [25, 26]. In this study, the control of disease activity in patients with RA was good and the dosage of PSL was able to be decreased over the course of a year. This allowed an increase in OC levels and improved bone metabolism in patients with RA.
In patients with RA, only ΔPSL dosage was detected as a factor influencing changes in serum OC by multivariate linear regression analysis. However, changes in disease activity score, bisphosphonate therapy, and period of biologics therapy did not significantly correlate with changes in serum levels of OC. Van Staa et al. reported osteoporotic fracture risk in RA as attributable to a combination of disease activity and use of oral glucocorticoids [3]. In our study, bDMARD treatment was used for about half of patients with RA and allowed good control of disease activity in almost all patients during the study period.
Patients in whom the PSL dosage could be decreased might have achieved good control and showed improved disease activity in 1 year. We therefore investigated the correlation between ΔPSL dosage and ΔDAS28-ESR but found no relationship (r = 0.001, p = 0.983). We reported that reducing the glucocorticoid dosage and adding bisphosphonate was important for osteoporosis in patients with RA, even if they had been well controlled by biologic agents [17]. The results of a previous report support the results of this study.
Some limitations to the present study must be considered. First, the baseline disease activity score of patients with RA was relatively low (mean DAS28-ESR, 3.47), and the usage rate of bDMARDs in this study was 50 %. This rate is higher than the general average use in the real world [27, 28] because of our protocol. Second, the change in disease activity from baseline to 1 year was small, so influences on bone metabolic markers might have been underestimated. Third, the usage rate and dosage of glucocorticoids were both relatively low compared to the general situation [28]. However, precisely because disease activity was under good control, the decrease in glucocorticoids was important for improving bone metabolic markers. Third, we did not perform DXA after 1 year in this study according to the original protocol and could not analyze the influence of reducing glucocorticoid dosage on lumbar or hip BMD in patients with RA. We also used whole-body mode for DXA, allowing the simultaneous analysis of BMD, lean body mass, and fat mass. The whole-body mode of DXA did not provide data that could be used to determine hip BMD. This study was not able to reveal whether the decrease in glucocorticoids correlated with risk of fragile fracture or bone density of the hip and spine. With the full data from the 10-year TOMORROW study, we believe that we will be able to better evaluate those endpoints.
In conclusion, our study indicated that decreasing glucocorticoids increased bone formation markers among patients with RA. That is, bone metabolic markers were improved. However, disease activity did not influence bone metabolic markers, which might thus degenerate even when disease activity is under good control. Decreasing the dose of glucocorticoids is important for improving bone metabolic markers in patients with RA.
References
Deodhar AA, Woolf AD (1996) Bone mass measurement and bone metabolism in rheumatoid arthritis: a review. Br J Rheumatol 35:309–322
Peel NF, Moore DJ, Barrington NA, Bax DE, Eastell R (1995) Risk of vertebral fracture and relationship to bone mineral density in steroid treated rheumatoid arthritis. Ann Rheum Dis 54:801–806
van Staa TP, Geusens P, Bijlsma JW, Leufkens HG, Cooper C (2006) Clinical assessment of the long-term risk of fracture in patients with rheumatoid arthritis. Arthritis Rheum 54:3104–3112
Wright NC, Lisse JR, Walitt BT, Eaton CB, Chen Z (2011) Arthritis increases the risk for fractures—results from the women’s health initiative. J Rheumatol 38:1680–1688
Kannus P, Sievanen H, Palvanen M, Jarvinen T, Parkkari J (2005) Prevention of falls and consequent injuries in elderly people. Lancet 366:1885–1893
Haugeberg G, Uhlig T, Falch JA, Halse JI, Kvien TK (2000) Bone mineral density and frequency of osteoporosis in female patients with rheumatoid arthritis: results from 394 patients in the Oslo County Rheumatoid Arthritis register. Arthritis Rheum 43:522–530
Lodder MC, Haugeberg G, Lems WF, Uhlig T, Orstavik RE, Kostense PJ, Dijkmans BA, Kvien TK, Woolf AD (2003) Radiographic damage associated with low bone mineral density and vertebral deformities in rheumatoid arthritis: the Oslo-Truro-Amsterdam (OSTRA) collaborative study. Arthritis Rheum 49:209–215
Braun T, Schett G (2012) Pathways for bone loss in inflammatory disease. Curr Osteoporos Rep 10:101–108
Van Staa TP, Leufkens HG, Abenhaim L, Zhang B, Cooper C (2000) Use of oral corticosteroids and risk of fractures. J Bone Miner Res 15:993–1000
van Staa TP, Leufkens HG, Cooper C (2002) The epidemiology of corticosteroid-induced osteoporosis: a meta-analysis. Osteoporos Int 13:777–787
Grossman JM, Gordon R, Ranganath VK, Deal C, Caplan L, Chen W, Curtis JR, Furst DE, McMahon M, Patkar NM, Volkmann E, Saag KG (2010) American College of Rheumatology 2010 recommendations for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Care Res 62:1515–1526
Nawata H, Soen S, Takayanagi R, Tanaka I, Takaoka K, Fukunaga M, Matsumoto T, Suzuki Y, Tanaka H, Fujiwara S, Miki T, Sagawa A, Nishizawa Y, Seino Y (2005) Guidelines on the management and treatment of glucocorticoid-induced osteoporosis of the Japanese Society for Bone and Mineral Research (2004). J Bone Miner Metab 23:105–109
Vis M, Havaardsholm EA, Haugeberg G, Uhlig T, Voskuyl AE, van de Stadt RJ, Dijkmans BA, Woolf AD, Kvien TK, Lems WF (2006) Evaluation of bone mineral density, bone metabolism, osteoprotegerin and receptor activator of the NFkappaB ligand serum levels during treatment with infliximab in patients with rheumatoid arthritis. Ann Rheum Dis 65:1495–1499
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, Healey LA, Kaplan SR, Liang MH, Luthra HS et al (1988) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31:315–324
Prevoo ML, van’t Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL (1995) Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum 38:44–48
Pincus T, Summey JA, Soraci SA Jr, Wallston KA, Hummon NP (1983) Assessment of patient satisfaction in activities of daily living using a modified Stanford Health Assessment Questionnaire. Arthritis Rheum 26:1346–1353
Okano T, Koike T, Tada M, Sugioka Y, Mamoto K, Wakitani S, Nakamura H (2014) The limited effects of anti-tumor necrosis factor blockade on bone health in patients with rheumatoid arthritis under the use of glucocorticoid. J Bone Miner Metab 32:593–600
Laan RF, Buijs WC, Verbeek AL, Draad MP, Corstens FH, van de Putte LB, van Riel PL (1993) Bone mineral density in patients with recent onset rheumatoid arthritis: influence of disease activity and functional capacity. Ann Rheum Dis 52:21–26
Hall GM, Spector TD, Griffin AJ, Jawad AS, Hall ML, Doyle DV (1993) The effect of rheumatoid arthritis and steroid therapy on bone density in postmenopausal women. Arthritis Rheum 36:1510–1516
Haugeberg G, Ørstavik RE, Uhlig T, Falch JA, Halse JI, Kvien TK (2002) Bone loss in patients with rheumatoid arthritis: results from a population-based cohort of 366 patients followed up for two years. Arthritis Rheum 46:1720–1728
Vis M, Guler-Yuksel M, Lems WF (2013) Can bone loss in rheumatoid arthritis be prevented? Osteoporos Int 24:2541–2553
Lange U, Teichmann J, Muller-Ladner U, Strunk J (2005) Increase in bone mineral density of patients with rheumatoid arthritis treated with anti-TNF-alpha antibody: a prospective open-label pilot study. Rheumatology (Oxford) 44:1546–1548
Garnero P, Thompson E, Woodworth T, Smolen JS (2010) Rapid and sustained improvement in bone and cartilage turnover markers with the anti-interleukin-6 receptor inhibitor tocilizumab plus methotrexate in rheumatoid arthritis patients with an inadequate response to methotrexate: results from a substudy of the multicenter double-blind, placebo-controlled trial of tocilizumab in inadequate responders to methotrexate alone. Arthritis Rheum 62:33–43
Lane NE, Kelman A (2003) A review of anabolic therapies for osteoporosis. Arthritis Res Ther 5:214–222
O’Brien CA, Jia D, Plotkin LI, Bellido T, Powers CC, Stewart SA, Manolagas SC, Weinstein RS (2004) Glucocorticoids act directly on osteoblasts and osteocytes to induce their apoptosis and reduce bone formation and strength. Endocrinology 145:1835–1841
Weinstein RS, Jilka RL, Parfitt AM, Manolagas SC (1998) Inhibition of osteoblastogenesis and promotion of apoptosis of osteoblasts and osteocytes by glucocorticoids. Potential mechanisms of their deleterious effects on bone. J Clin Invest 102:274–282
Neovius M, Sundstrom A, Simard J, Wettermark B, Cars T, Feltelius N, Askling J, Klareskog L (2011) Small-area variations in sales of TNF inhibitors in Sweden between 2000 and 2009. Scand J Rheumatol 40:8–15
Yamanaka H, Seto Y, Tanaka E, Furuya T, Nakajima A, Ikari K, Taniguchi A, Momohara S (2013) Management of rheumatoid arthritis: the 2012 perspective. Mod Rheumatol 23:1–7
Acknowledgments
We wish to thank Atsuko Kamiyama, Tomoko Nakatsuka, and the Center for Drug & Food Clinical Evaluation, Department of Radiology, and Department of Central Clinical Laboratory in Osaka City University Hospital for their special efforts as research coordinators in recruiting subjects, collecting data, and managing the quality of data. We greatly appreciate the cooperation of the patients with RA and volunteers who participated in this study.
Conflicts of interest
Dr. Koike has received grant fees, research fees, consulting fees, or other remuneration from AbbVie, Astellas Pharma Inc., Bristol-Myers Squibb, Chugai Pharmaceutical, Eisai, Janssen, Lilly, Mitsubishi Tanabe Pharma Corporation, MSD, Ono Pharmaceutical, Pfizer, Roche, Takeda Pharmaceutical, Teijin Pharma, and UCB. Dr. Nakamura has received research grants and/or speaking fees from Chugai Pharmaceutical, Astellas Pharma, Janssen Pharmaceutica, GlaxoSmithKline, Pfizer, Daiichi Sankyo, and Ono Pharmaceutical. Dr. Tada, Dr. Inui, Dr. Sugioka, Dr. Mamoto, and Dr. Okano do not have any conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tada, M., Inui, K., Sugioka, Y. et al. Reducing glucocorticoid dosage improves serum osteocalcin in patients with rheumatoid arthritis—results from the TOMORROW study. Osteoporos Int 27, 729–735 (2016). https://doi.org/10.1007/s00198-015-3291-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3291-y