Abstract
Chronic inflammation including autoimmune disease is an important risk factor for the development of osteoporosis. Receptor activator of nuclear factor-κB ligand (RANKL) and macrophage colony-stimulating factor (M-CSF) play a central role in osteoclast differentiation and function, and the molecular pathways by which M-CSF and RANKL induce osteoclast differentiation have been analyzed in detail. Proinflammatory cytokines directly or indirectly regulate osteoclastogenesis and bone resorption providing a link between inflammation and osteoporosis. Tumor necrosis factor-α, interleukin (IL)-1, IL-6, and IL-17 are the most important proinflammatory cytokines triggering inflammatory bone loss. Inhibition of these cytokines has provided potent therapeutic effects in the treatment of diseases such as rheumatoid arthritis. Further investigation is needed to understand the pathophysiology and to develop new strategies to treat inflammatory bone loss. This review summarizes new data on inflammatory bone loss obtained in 2011.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
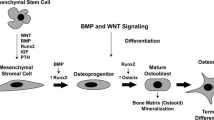
Chronic inflammation is a strong trigger of bone loss. Thus, increased level of C-reactive protein as a measure for inflammation is associated with increased risk for osteoporotic fractures. Chronic inflammatory diseases such as rheumatoid arthritis (RA), ankylosing spondylitis, and inflammatory bowel disease are frequently accompanied by osteoporosis [1]. RA additionally leads to local bone erosion. These clinical findings are confirmed by animal models of arthritis and other autoimmune disease [1]. Decreased bone mineral density is mainly due to increased bone resorption. The sole bone-resorbing cells are osteoclasts. Receptor activator of nuclear factor-κB ligand (RANKL) was discovered in 1998 and plays a key role in osteoclast differentiation and function [1]. Today RANKL signaling has been analyzed in detail and several other cytokines or factors have been discovered that directly or indirectly regulate osteoclast differentiation and function. Proinflammatory cytokines positively regulate osteoclastogenesis and bone resorption showing a link between inflammation and bone loss. New data on inflammatory bone loss obtained in 2011 are summarized in this review article.
Novel Insights Into the Role of RANKL in Bone Homeostasis
RANKL is a member of the tumor necrosis factor (TNF) family of cytokines and plays a key role in osteoclastogenesis and thus inflammatory bone loss [1]. A recent publication has demonstrated that RANKL expression in osteocytes is more important than RANKL expression in osteoblasts in vitro and in vivo [2•]. A smaller amount of RANKL is expressed in synovial cells, activated T cells, B cells, and natural killer cells [1]. Yeo et al. [3] analyzed cytokine mRNA expression in peripheral blood mononuclear cells (PBMCs) and synovial fluid cells of RA patients and have shown that B cells are a source of RANKL. These results were confirmed with flow cytometry and immunofluorescence staining of the synovial tissue. However, osteocytes and osteoblasts are not considered in this study. Synovial fluid but not serum level of RANKL has been correlated with disease activity in RA patients [4].
Boumans et al. [5] showed that rituximab (anti-CD20 antibody) treatment of RA patients is associated with decreased synovial osteoclast precursors and RANKL expression and increased osteoprotegerin (OPG)/RANKL ratio in serum. Further investigation should clarify the role of B cells in RANKL secretion and inflammatory bone loss.
In vitro, members of the TNF family other than RANKL also support osteoclastogenesis. Mabilleau et al. [6] generated human osteoclast using RANKL, TNF-α/interleukin (IL)-1, or LIGHT. Bone resorption is enhanced in the presence of LIGHT but still much lower than with RANKL, showing that RANKL supports osteoclastogenesis more efficiently. Jang et al. [7•] showed that Foxp3 + regulatory T-cell–deficient mice develop more severe arthritis and bone destruction than wild-type mice. This is due to the influx of numerous RANKL-positive cells into synovia. These data suggest that regulatory T cells prevent inflammatory bone loss by reducing the number of RANKL expressing cells, as previously reported by other groups. Staphylococcus aureus protein A (SPA) contributes to loss of bone mineral density in patients with osteomyelitis. On the one hand, SPA binds to osteoblasts in vitro and prevents proliferation, induces apoptosis, and inhibits mineralization, and on the other hand, infected osteoblasts show increased RANKL expression [8].
Recent data demonstrate that RANKL contributes to pathogenesis of gouty arthritis. Osteoclasts are present around tophi and in osteolytic lesions of patients with gout. RANKL is highly expressed in T cells while OPG was not or weakly expressed in tophus tissue. Stimulation of PBMCs with monosodium urate monohydrate crystals induces expression of proinflammatory cytokines and RANKL but inhibited OPG expression. Furthermore, synovial mononuclear cells in gouty arthritis express proinflammatory cytokines and RANKL [9•]. Moreover, serum level of OPG and soluble IL-6 receptor (IL-6R) is negatively associated with radiographic damage in patients with gouty arthritis [10].
Shared Signaling Pathways of Bone and Immune Cells
RANKL activates the key transcription factor NFATc1 (nuclear factor of activated T cells, cytoplasmic 1) that regulates the expression of osteoclast-specific genes. NFATc1 is regulated by RANKL in two different ways: nuclear factor-κB (NF-κB)/AP-1/c-Fos pathway and calcium signaling [1]. RANKL increases intracellular calcium concentration and activates NFATc1 via calcineurin. There are two sources of calcium: extracellular space and intracellular stores [1]. Orai 1 is a store-operated calcium entry channel. Silencing the Orai 1 gene in a murine monocyte cell line inhibits RANKL-induced osteoclastogenesis by suppressing the induction of NFATc1 and cell fusion by inhibition of the induction of the d2 isoform of vacuolar ATPase Vo. In consequence, bone resorption is impaired. These in vitro data suggest an important role of Orai 1 in calcium signaling in osteoclasts [11]. L-type calcium channels mediate the influx of extracellular calcium and thus increase intracellular calcium concentration. An L-type calcium channel agonist increases intracellular calcium concentration and inhibited osteoclastogenesis by blocking IκB degradation and NFATc1 activation. Possibly this L-type calcium channel agonist increases the calcium threshold for effective activation of NFATc1 and thus inhibits RANKL-induced osteoclastogenesis [12].
Both classical and alternative NF-κB signaling pathways contribute to NFATc1 activation in osteoclasts [1]. Regucalcin is a calcium-binding protein known to promote osteoclastogenesis in vivo and in vitro. Recent in vitro data have shown that this promotion of osteoclastogenesis is due to increased basal and RANKL-induced activation of NF-κB signaling [13]. The NF-κB inhibitor SPA0355 inhibits osteoclastogenesis in vitro and reduces disease activity in mice with collagen-induced arthritis [14]. NF-κB–inducing kinase (NIK) is part of the alternative NF-κB signaling pathway. Soysa et al. [15] have shown that NIK defective mice have reduced bone mineral density due to impaired osteoclastogenesis and are protected from lipopolysaccharide (LPS)-induced inflammatory bone loss.
The large zinc finger protein ZAS3 promotes osteoclastogenesis. Cytoplasmic ZAS3 associates with TRAF6 and controls NF-κB signaling. Nuclear ZAS3 acts as a transcriptional regulator for osteoclast-associated genes and ZAS3 directly activates NFATc1 [16]. LPS induces formation of osteoclasts in vitro, but these osteoclasts do not resorb bone. This is possibly due to LPS-induced expression of A20 that leads to TRAF6 degradation and NF-κB inhibition [17]. Bishop et al. [18] studied RANKL expression in T cells in detail. RANKL expression is regulated by the enhancers mRL-D5 and T-cell control region and the transcription factors c-Fos, NF-κB, and Nfat.
Bruton’s tyrosine kinase (Btk) plays an important role in B cells; beyond that it is also involved in RANKL signaling. Btk inhibitors protect mice from inflammatory arthritis and are now analyzed in clinical trials in RA patients. Danks et al. [19] have shown impaired in vitro osteoclastogenesis of monocytes isolated from patients with mutations in Btk. However, these patients have no higher bone mass, which may be due to elevated serum levels of inflammatory cytokines that support osteoclastogenesis [19]. Recent data suggest that the Btk inhibitor PCI-32765 may target B cells, monocytes, macrophages, and mast cells in murine arthritis [20].
Yoon et al. [21] analyzed the role of cAMP signaling in osteoclastogenesis. RANKL increases expression of adenylate cyclase 3, which increases cyclic AMP (cAMP) level leading to reduced osteoclastogenesis in vitro and in vivo through NFATc1. On the other hand, RANKL activates calcium/calmodulin-dependent protein kinase that decreases cAMP, thus promoting osteoclastogenesis. Osteoclastogenesis may be fine-tuned by the balance of these two contrary mechanisms [21]. Bao et al. [22] have shown that acid sphingomyelinase regulates osteoclastogenesis by modulating sphingosine kinases downstream of RANKL. Recent data suggest that extracellular signal-regulated kinase 1 (ERK1) and the transcription factor FBI-1/OCZF/LRF positively regulate osteoclastogenesis [23, 24]. Osteoclasts produce TSG-6 in response to TNF-α, IL-1, and IL-6. TSG-6 inhibits the activation of osteoclasts and may represent an autocrine mechanism to limit inflammatory bone loss [25].
Recent studies have shown that epigenetic mechanisms such as histone methylation and acetylation control gene expression. Yasui et al. [26] have observed the histone H3 lysin 27 (H3K27) in the NFATc1 gene in bone marrow–derived macrophages and markedly reduced in mature osteoclasts. Jumonji domain containing-3 (Jmjd3), a H3K27 demethylase, is induced by RANKL and silencing of Jmjd3 suppresses RANKL-induced osteoclastogenesis. These data suggest a critical role of Jmjd3 in osteoclastogenesis [26]. Inhibition of histone deacetylase class I and II suppresses human osteoclastogenesis in vitro [27]. Kim et al. [28] have shown that RANKL stimulates NFATc1 acetylation and thus increases NFATc1 transcriptional activity by increasing protein level by post-translational modification. Further research is needed to characterize these epigenetic mechanisms in detail.
The Teamwork of M-CSF and IL-34
M-CSF is a key mediator of osteoclast differentiation and enhances survival and motility of mature osteoclasts. Hodge et al. [29] have shown that M-CSF augmented RANKL-induced bone resorption without increasing the number of osteoclasts. M-CSF pretreatment facilitates RANKL-induced activation of c-Fos and ERK, but not NF-κB and NFATc1 [29]. The receptor of M-CSF is c-Fms. Kimura et al. [30] have shown that local administration of anti-c-Fms antibody inhibits LPS-induced osteoclast formation. The new cytokine IL-34 also binds to c-Fms and induces osteoclastogenesis together with RANKL independent of M-CSF. Systemic application of IL-34 to mice reduces trabecular bone mass [31]. Chemel et al. [32] have shown IL-34 expression in synovial biopsies from RA patients. IL-34 is expressed in macrophages, endothelial cells, fibroblasts, leukocytes, and multinucleated giant cells, and IL-34 expression correlates with the clinical synovitis score, hyperplasia of the synovial lining layer, and total leukocyte counts in the synovial fluids. IL-34 expression in synovial fibroblasts increases after stimulation with TNF-α and IL-1β dependent on JNK and NF-κB [32]. Further investigation should clarify the potential of IL-34 as a new target for the treatment of inflammatory bone loss.
Effects of IL-1 Family Members on the Bone
IL-1 plays an important proinflammatory and pro-osteoclastogenic role in animal models of RA, but targeting IL-1 has not yet provided strong effect in the treatment of RA [1]. Lee et al. [33] have shown that IL-1β directly inhibits early human osteoclastogenesis by downregulation of RANK and the costimulatory triggering receptor expressed on myeloid cells 2 (TREM2) receptor. IL-1β inhibits M-CSF-induced expression of RANK by decreasing the M-CSF receptor c-Fms at the surface of osteoclast precursors [33]. This effect may be a possible explanation for the limited success of targeting IL-1 in RA patients. However, few data exist that demonstrate a bone protective effect of anti-IL-1 therapy in RA [1]. Ignatius et al. [34] have shown that IL-1β only together with complement C3a or C5a increases the secretion of the pro-osteoclastogenic cytokine IL-6 by human osteoblasts. C3a and C5a directly induce the formation of human TRAP-positive multinuclear cells independent of RANKL, but these cells do not show resorptive activity [34]. The most important source of IL-1β is macrophages. Bone morphogenetic protein 6 induces IL-1β expression in murine macrophages dependent on the transcription factors PU.1 and Smad1 [35].
IL-33 is the most recently identified member of the IL-1 family. IL-33 receptor (ST2)-deficient mice showed reduced bone mass. In vitro IL-33 inhibits RANKL and M-CSF mediated differentiation of murine bone marrow cells to osteoclasts [36]. This inhibition depends on the presence of osteoblasts. IL-33 induces the expression of granulocyte-macrophage (GM)-CSF, IL-4, IL-13, and IL-10 in osteoblasts and the inhibitory effect of IL-33 is reduced only by depletion of all of these cytokines [37]. IL-33 is expressed in osteoblasts in murine bone [37]. Overexpression of IL-33 in osteoblasts reduces trabecular volume and the number of osteoclasts in vivo. There are no quantitative differences of leukocyte subpopulation in this model, suggesting that inhibition of osteoclastogenesis is one of the major physiological functions of IL-33 [38•].
Zaiss et al. [39•] analyzed TNF transgenic mice to determine the role of IL-33 in arthritis. Administration of IL-33 reduces systemic bone loss and the number of osteoclasts in these mice. IL-33 increases serum levels of IL-4 and IL-13 and shifts the balance from osteoclast to alternatively activated macrophage differentiation. IL-33 protects from TNF-α–mediated bone loss [39•]. IL-33 induces NF-κB activation; this is dependent on Janus kinase 2 [40]. Ali et al. [41] have shown that IL-33 directly binds intracellular NF-κB and reduces NF-κB–induced gene expression, thus showing an inhibitory effect of IL-33 on NF-κB–triggered gene expression.
IL-33 is expressed in osteocytes in human bone. Zaiss et al. [39•] have shown that IL-33 inhibits human osteoclastogenesis in vitro, but Saidi et al. [42] have detected no inhibitory effect of IL-33 in vitro. Serum level of IL-33 is elevated in RA patients and correlates with disease activity. The data concerning IL-33 in synovial fluid of RA patients are contradictory [43–45]. These recent data show that IL-33 plays an important role as anti-osteoclastogenic cytokine in animal models, but further investigation should characterize the exact role of IL-33 in inflammatory bone loss in humans.
News on the Skeletal Effects of TNF-α and IL-6
TNF-α is an important pro-resorptive cytokine, but recent data suggest an additional protective role of TNF-α in a mouse model. Nagano et al. [46] have demonstrated a protective effect of TNF type 2 receptor. Atanga et al. [47] have shown that TNF and vitamin D inhibit osteoclastogenesis in vitro by increasing GM-CSF secretion of osteoblasts. These protective effects of TNF-α may fine-tune TNF-α–mediated inflammatory bone loss. Human in vitro data highlight new aspects of the proresorptive cytokine TNF-α. TNF-α increases expression of RANKL in human bone marrow adipocytes and induces the formation of osteoclasts in co-culture experiments with osteoclast precursors and bone marrow adipocytes [48]. Yarilina et al. [49] have shown that TNF-α activates c-Jun, NF-κB, and calcium signaling leading to NFATc1 activation and thus osteoclast differentiation independent of RANKL in human macrophages. Finzel et al. [50] detected bone erosions of RA patients by μCT. Patients receiving a TNF inhibitor in combination with methotrexate have shown a decrease of mean depth of the erosions in contrast to the methotrexate-treated control group. These data suggest repair of bone erosions using TNF inhibitors [50]. In vitro data demonstrate an effect of TNF-α not only on osteoclasts but also on osteoblasts. TNF-α inhibits osteoblast differentiation and bone nodule formation [51]. A possible mechanism is the downregulation of POEM by TNF dependent on NF-κB [52]. This inhibitory effect of TNF-α on osteoblasts could possibly explain the repair of bone erosions using TNF-α inhibitors in RA patients. However, further investigation is needed to verify this hypothesis.
The majority of the in vivo data show a pro-osteoclastogenic effect of IL-6. However, in vitro data have demonstrated enhanced as well as reduced osteoclastogenesis [1]. Suzuki et al. [53] showed that RANKL-mediated osteoclast differentiation is decreased by IL-6 in cultures of an osteoclast precursor cell line. The addition of a synovial cell line increases the number of osteoclasts dependent on intercellular adhesion molecule-1 (ICAM-1). Cheung et al. [54] have demonstrated that IL-6–elevated ICAM-1 expression on endothelial cells leads to increased adhesion of osteoclast precursor cells. These data emphasize that IL-6 has an indirect effect on osteoclastogenesis mediated through other cell types. In vitro data suggest a central role of ICAM-1; this should to be confirmed by in vivo experiments. Chondrocyte media stimulated with IL-6 and soluble IL-6R contain a high level of prostaglandin E2 and suppresses osteoclastogenesis in vitro [55], suggesting an inhibitory effect of chondrocytes. Cell-cell contact was not investigated and the in vivo relevance remains unclear. The IL-6R–specific antibody tocilizumab efficiently reduces disease activity and radiographic progression in RA patients [1]. Current data demonstrate increased OPG/RANKL ratio in RA patients treated with tocilizumab [56]. Immunohistochemical examination of bone marrow has shown significantly higher expression of OPG in tocilizumab-treated RA patients compared to controls [57].
Osteoblasts are an important source of IL-6. Wnt3a reduces TNF-α–stimulated IL-6 secretion though the canonical Wnt pathway in osteoblasts [58]. Platelet-derived growth factor–induced IL-6 production by osteoblasts is mediated by AMP-activated protein kinase [59]. Furthermore, angiotensin II induces IL-6 synthesis in osteoblasts through the ERL 1/2 pathway [60]. Rego et al. [61] showed that IL-6 production in LPS-stimulated macrophages is positively regulated by Src homology domain 2-containing tyrosine phosphatase-1 (SHP-1) dependent on C/EBPβ and NF-κB pathways and SHP-1 independent NF-κB pathway. IL-27 is a member of the IL-6/IL-12 family. Recent data demonstrate that IL-27 inhibits RANKL expression in T cells mediated in part through STAT3 and thus suggesting a protective effect of IL-27 [62].
IL-17: Bridging T Cells and Bone
TH17 cells represent an osteoclastogenic T-cell subset. Thus, a lot of new work concerning Th17 cells and IL-17 was published last year. Halvorsen et al. [63] focused on Th17 cells located within the synovial tissue of RA patients. They isolated an IL-17–producing polyclonal T-cell line. These cells are CCR6 positive and secreted IL-6, IL-10, TNF-α, and interferon-γ (IFN-γ) besides IL-17 in vitro. Exogenous IL-15 increases IL-17 production. These data show that Th17 cells are present in the synovial tissue of RA patients; however, Hueber et al. [64] have shown that mast cells may be a more important source of IL-17. Pöllinger et al. [65•] analyzed whether Th17 cells and IL-17+γδ T cells mediate arthritic bone loss. Depletion experiments have shown that Th17 cells are more important concerning bone loss in collagen-induced arthritis in vivo. Th17 cells are localized in the vicinity of osteoclasts in subchondral areas. Examination of synovia from RA patients has shown a similar contribution of these T cells [65•].
Toll-like receptor signaling is critical for IL-17 production and the development of bone erosions in a mouse model of chronic arthritis due to intra-articular injections of streptococcal cell wall fragments. This study demonstrates a pro-resorptive role of myeloid differentiation factor 88 (MyD88) and protective role of Toll/IL-1 receptor domain-containing adapter-inducing interferon β (TRIF) in this T-cell–driven arthritis model [66]. Oostlander et al. [67] have shown in vitro osteoclast formation of T-cell and B-cell–depleted human PBMCs in co-culture with T cells without supplementation of the osteoclastogenic factors RANKL and M-CSF. Osteoclast formation is related to IL-17 levels in vitro and is significantly higher using PBMCs of patients with Crohn’s disease than healthy controls [67]. The exact mechanism how IL-17 induces osteoclast formation remains unclear. Intra-articular injection of IL-17 aggravates inflammation and bone destruction in mice collagen-induced arthritis (CIA). Synovial expression of cadherin 11 is higher in these mice after IL-17 injection. In vitro stimulation with IL-17 increases cadherin 11 expression of fibroblast-like synoviocytes of mice and RA patients [68]. Thus, induction of cadherin 11 expression is a new mechanism of IL-17–mediated inflammatory bone loss. Stimulation of osteoblasts with IL-17 induces secretion of prostaglandin E2 and prostaglandin E2 and increases osteoclast numbers [69]. Zwerina et al. [70] have demonstrated that IL-17 neutralization reduces local and systemic bone loss in TNF-α–mediated murine arthritis. These mice have enhanced Th2 differentiation, IL-4 and IL-12 expression, and more regulatory T cells, suggesting a central role of IL-17 in TNF-α–mediated arthritis [70].
Recent data suggest a link between IL-17 and chemokines. Mice deficient for the IL-17 receptor subunit IL-17RA have fewer bone erosions in the K/BxN serum transfer mouse arthritis model associated with reduced expression of the chemokines CXCL1, CXCL2, CXCL5, CCL9, CCL7, and CCL20, the cytokines IL-1β, IL-6, and RANKL, and some metalloproteinases. Expression of these factors can be induced by IL-17A in synovial fibroblasts in vitro [71]. Anti-CXCL5 therapy reduces arthritis and bone erosions due to local overexpression of IL-17 leading to decreased joint vascularization [72]. Mice deficient for the chemokine receptor CCR2 develop more severe CIA. This is associated with a higher number of Th17 cells in the draining lymph nodes and higher levels of Th17 cell cytokines in the serum and the joints. Treatment with anti-IL-17 antibody only modestly reduces disease severity, suggesting other factors may also contribute to this severe arthritis in CCR2-deficient mice [73]. IL-25 (IL-17E) is a member of the IL-17 cytokine family. IL-25 is expressed in Th2 cells and mast cells and can induce Th2 cytokines. Kaiwen et al. [74] have shown that IL-25 expression is enhanced in late-stage collagen-induced arthritis while IL-17 expression is increased in the early stage. The authors suggest that IL-25 may inhibit IL-17 expression [74]. Further investigation is needed to clarify the exact role of IL-25 in arthritis.
Other Cytokines and Mediators Linking the Immune System and Bone
One important anti-osteoclastogenic cytokine is IL-4. Previous studies have shown that IL-4 blocks RANKL-induced activation of NF-κB. Yu et al. [75] have recently demonstrated that NF-κB signaling is required for IL-4–induced macrophage fusion to form multinucleated giant cells. IL-4 inhibits the alternative but not the canonical NF-κB pathway [75]. Cheng et al. [76] have shown that IL-4 does not suppress RANKL-dependent NF-κB activation but blocks RANKL-dependent NFATc1 activation dependent on STAT6. Phosphatidylserine-containing liposomes suppress inflammatory bone loss. A recent publication by Ma et al. [77] suggests that this effect is due to increased IL-10 production by macrophages. IFN-γ is considered as an anti-osteoclastogenic cytokine; however, there is also evidence for a pro-osteoclastogenic effect of IFN-γ. Kohara et al. [78] have shown that INF-γ directly inhibits osteoclastogenesis in vitro and after calvarial TNF-α injection in vivo. IFN-γ was added at the same time point as RANKL or TNF-α in these experiments. Ayon Haro et al. [79] investigated osteoclastogenesis in vitro and LPS-induced local bone loss in vivo. In vivo IFN-γ administration together with LPS does not affect osteoclast formation, while IFN-γ injection after LPS injection increases osteoclast formation. In vitro IFN-γ inhibits osteoclastogenesis when added together with M-CSF and RANKL, but IFN-γ accelerates osteoclastogenesis when added together with LPS 48 h after M-CSF and RANKL [79]. Cheng et al. [80] demonstrate that IFN-γ inhibits osteoclastogenesis by suppressing NFATc1 and the activation of NF-κB and JNK pathway. This inhibitory effect is reduced when osteoclast precursors were pre-exposed to RANKL [80]. Further research is needed to clarify the exact role of INF-γ in osteoclastogenesis and inflammatory bone loss.
Recent publications describe new molecular mechanisms of TNF-β and IL-15. TGF-β promotes RANKL-induced osteoclastogenesis through interaction between Smad3 and Traf6. IL-15 regulates osteoclastogenesis via the phospholipase D pathway [81, 82]. IL-32γ promotes osteoclast fusion while IL-27 protects from inflammatory bone loss [83, 84]. Recent data have shown that IL-19, IL-20, IL-21, and IL-22 promote inflammatory bone loss in arthritis [85–90].
Disease activity is reduced in JNK1-deficient mice in a serum transfer model of arthritis. This protective effect is dependent on mast cells. JNK controls mast cell degranulation and FCγR-triggered IL-1β production [91]. Polzer et al. [92] have demonstrated that the proteasome inhibitor bortezomib increases osteoclastogenesis in vitro and in vivo in human TNF transgenic mice. These data may have direct therapeutic impact as proteasome inhibitors are currently available drugs and it is currently unknown whether these drugs induce bone loss. The same group has shown that vitamin D receptor–deficient human TNF transgenic mice have more severe bone erosions. Moreover, vitamin D receptor–deficient monocytes show increased osteoclast differentiation in vitro. Thus, vitamin D receptor may play a critical role in limiting inflammatory bone loss in an arthritis model [93]. MicroRNAs (miRs) are a class of noncoding RNA that regulate gene expression. miRs both positively and negatively regulate inflammatory bone loss. MiR-155–deficient mice are protected from arthritis in animal models [94]. MiR-21 positively regulates osteoclastogenesis by downregulation of expression of programmed cell death protein 4 (PCSP4) leading to increased c-Fos activity. In addition, C-Fos upregulates miR-21, thus showing a positive feedback loop [95]. On the other hand, miR-146a suppressed human osteoclastogenesis in vitro and prevented joint destruction in a murine arthritis model [96].
Conclusions
Tremendous novel insights into the field of inflammatory disease have been made during the last year. In particular, osteocytes have been identified as an important source of RANKL. The protective role of regulatory T cells on inflammatory bone loss has been confirmed. The role of RANKL in the pathogenesis of bone loss during gout has been unraveled. Many new mechanisms have been identified concerning RANKL signaling including epigenetic mechanisms. IL-33 has been established as an important anti-osteoclastogenic cytokine and new data support the role of IL-34 as a pro-osteoclastogenic cytokine. Additional pathways of how TNF-α inhibits osteoblast function have been described. New aspects of IL-6 function and secretion have been demonstrated and new mechanisms supporting the important role of IL-17 as a pro-osteoclastogenic cytokine have been discovered. Among other factors miRs have been shown to regulate inflammatory bone loss. However, numerous questions have not yet been answered and research is needed to further characterize the pathophysiology of inflammatory bone loss. Inhibition of pro-osteoclastogenic cytokines such as TNF-α or IL-6 has already provided potent therapeutic effects in protecting bone in RA patients and new drugs inhibiting intracellular kinases are currently being tested for their anti-inflammatory and bone-protective effects in clinical trials with patients with RA [1]. Increased knowledge of the pathophysiology of inflammatory bone loss may thus help to tailor new therapeutic strategies to protect bone.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Braun T, Zwerina J. Positive regulators of osteoclastogenesis and bone resorption in rheumatoid arthritis. Arthritis Res Ther. 2011;13(4):235.
• Nakashima T, et al. Evidence for osteocyte regulation of bone homeostasis through RANKL expression. Nat Med. 2011;17(10):1231–4. Osteocytes are a major source of RANKL and thus regulate bone homeostasis in vitro and in vivo..
Yeo L, et al. Cytokine mRNA profiling identifies B cells as a major source of RANKL in rheumatoid arthritis. Ann Rheum Dis. 2011;70(11):2022–8.
Ellabban AS, et al. Receptor activator of nuclear factor kappa B ligand serum and synovial fluid level. A comparative study between rheumatoid arthritis and osteoarthritis. Rheumatol Int 2011, Feb 17.
Boumans MJ, et al. Rituximab abrogates joint destruction in rheumatoid arthritis by inhibiting osteoclastogenesis. Ann Rheum Dis. 2012;71(1):108–13.
Mabilleau G, et al. Depth and volume of resorption induced by osteoclasts generated in the presence of RANKL, TNF-alpha/IL-1 or LIGHT. Cytokine. 2012;57(2):294–9.
• Jang E, et al. Deficiency of foxp3 regulatory T cells exacerbates autoimmune arthritis by altering the synovial proportions of CD4 T cells and dendritic cells. Immune Netw. 2011;11(5):299–306. Regulatory T cells protect from inflammatory bone loss in vivo reducing the influx of RANKL-positive cells into synovia..
Claro T, et al. Staphylococcus aureus protein A binds to osteoblasts and triggers signals that weaken bone in osteomyelitis. PLoS One. 2011;6(4):e18748.
• Lee SJ, et al. Bone destruction by receptor activator of nuclear factor kappaB ligand-expressing T cells in chronic gouty arthritis. Arthritis Res Ther. 2011;13(5):R164. This publication shows that RANKL contributes to the pathogenesis of human gouty arthritis..
Choe JY, Lee GH, Kim SK. Radiographic bone damage in chronic gout is negatively associated with the inflammatory cytokines soluble interleukin 6 receptor and osteoprotegerin. J Rheumatol. 2011;38(3):485–91.
Hwang SY, Putney JW. Orai1-mediated calcium entry plays a critical role in osteoclast differentiation and function by regulating activation of the transcription factor NFATc1. FASEB J. 2011.
Noh AL, et al. L-type Ca(2+) channel agonist inhibits RANKL-induced osteoclast formation via NFATc1 down-regulation. Life Sci. 2011;89(5–6):159–64.
Yamaguchi M, Weitzmann MN, Murata T. Exogenous regucalcin stimulates osteoclastogenesis and suppresses osteoblastogenesis through NF-kappaB activation. Mol Cell Biochem. 2012;359(1–2):193–203.
Lee YR, et al. SPA0355, a thiourea analogue, inhibits inflammatory responses and joint destruction in fibroblast-like synoviocytes and mice with collagen-induced arthritis. Br J Pharmacol. 2011;164(2b):794–806.
Soysa NS, et al. Defective nuclear factor-kappaB-inducing kinase in aly/aly mice prevents bone resorption induced by local injection of lipopolysaccharide. J Periodontal Res. 2011;46(2):280–4.
Liu S, et al. The large zinc finger protein ZAS3 is a critical modulator of osteoclastogenesis. PLoS One. 2011;6(3):e17161.
Mabilleau G, Chappard D, Sabokbar A. Role of the A20-TRAF6 axis in lipopolysaccharide-mediated osteoclastogenesis. J Biol Chem. 2011;286(5):3242–9.
Bishop KA, et al. Mouse Rankl expression is regulated in T cells by c-Fos through a cluster of distal regulatory enhancers designated the T cell control region. J Biol Chem. 2011;286(23):20880–91.
Danks L, et al. Elevated cytokine production restores bone resorption by human Btk-deficient osteoclasts. J Bone Miner Res. 2011;26(1):182–92.
Chang BY, et al. The Bruton tyrosine kinase inhibitor PCI-32765 ameliorates autoimmune arthritis by inhibition of multiple effector cells. Arthritis Res Ther. 2011;13(4):R115.
Yoon SH, et al. Adenylate cyclase and calmodulin-dependent kinase have opposite effects on osteoclastogenesis by regulating the PKA-NFATc1 pathway. J Bone Miner Res. 2011;26(6):1217–29.
Bao X, et al. Acid sphingomyelinase regulates osteoclastogenesis by modulating sphingosine kinases downstream of RANKL signaling. Biochem Biophys Res Commun. 2011;405(4):533–7.
He Y, et al. Erk1 positively regulates osteoclast differentiation and bone resorptive activity. PLoS One. 2011;6(9):e24780.
Kukita A, et al. The transcription factor FBI-1/OCZF/LRF is expressed in osteoclasts and regulates RANKL-induced osteoclast formation in vitro and in vivo. Arthritis Rheum. 2011;63(9):2744–54.
Mahoney DJ, et al. TSG-6 inhibits osteoclast activity via an autocrine mechanism and is functionally synergistic with osteoprotegerin. Arthritis Rheum. 2011;63(4):1034–43.
Yasui T, et al. Epigenetic regulation of osteoclast differentiation: possible involvement of Jmjd3 in the histone demethylation of Nfatc1. J Bone Miner Res. 2011;26(11):2665–71.
Cantley MD, et al. Inhibitors of histone deacetylases in class I and class II suppress human osteoclasts in vitro. J Cell Physiol. 2011;226(12):3233–41.
Kim JH, et al. RANKL induces NFATc1 acetylation and stability via histone acetyltransferases during osteoclast differentiation. Biochem J. 2011;436(2):253–62.
Hodge JM, et al. M-CSF potently augments RANKL-induced resorption activation in mature human osteoclasts. PLoS One. 2011;6(6):e21462.
Kimura K, et al. Anti-c-Fms antibody inhibits lipopolysaccharide-induced osteoclastogenesis in vivo. FEMS Immunol Med Microbiol. 2012;64(2):219–27.
Chen Z, et al. The critical role of IL-34 in osteoclastogenesis. PLoS One. 2011;6(4):e18689.
Chemel M, et al. Interleukin 34 expression is associated with synovitis severity in rheumatoid arthritis patients. Ann Rheum Dis. 2012;71(1):150–4.
Lee B, et al. Direct inhibition of human RANK+ osteoclast precursors identifies a homeostatic function of IL-1beta. J Immunol. 2010;185(10):5926–34.
Ignatius A, et al. Complement C3a and C5a modulate osteoclast formation and inflammatory response of osteoblasts in synergism with IL-1beta. J Cell Biochem. 2011;112(9):2594–605.
Lee GT, et al. Bone morphogenetic protein 6-induced interleukin-1beta expression in macrophages requires PU.1/Smad1 interaction. Mol Immunol. 2011;48(12–13):1540–7.
Schulze J, et al. Interleukin-33 is expressed in differentiated osteoblasts and blocks osteoclast formation from bone marrow precursor cells. J Bone Miner Res. 2011;26(4):704–17.
Saleh H, et al. Interleukin-33, a target of parathyroid hormone and oncostatin m, increases osteoblastic matrix mineral deposition and inhibits osteoclast formation in vitro. Endocrinology. 2011;152(5):1911–22.
• Keller J, et al. Transgenic over-expression of interleukin-33 in osteoblasts results in decreased osteoclastogenesis. Biochem Biophys Res Commun. 2012;417(1):217–22. Inhibition of osteoclastogenesis is an important function of IL-33 in vivo in mice..
• Zaiss MM, et al. IL-33 shifts the balance from osteoclast to alternatively activated macrophage differentiation and protects from TNF-alpha-mediated bone loss. J Immunol. 2011;186(11):6097–105. IL-33 reduces TNF-α–mediated inflammatory bone loss and osteoclast number in vivo in mice..
Funakoshi-Tago M, et al. JAK2 is an important signal transducer in IL-33-induced NF-kappaB activation. Cell Signal. 2011;23(2):363–70.
Ali S, et al. The dual function cytokine IL-33 interacts with the transcription factor NF-kappaB to dampen NF-kappaB-stimulated gene transcription. J Immunol. 2011;187(4):1609–16.
Saidi S, et al. IL-33 is expressed in human osteoblasts, but has no direct effect on bone remodeling. Cytokine. 2011;53(3):347–54.
Kageyama Y, et al. Involvement of IL-33 in the pathogenesis of rheumatoid arthritis: the effect of etanercept on the serum levels of IL-33. Mod Rheumatol. 2012;22(1):89–93.
Hong YS, et al. Measurement of interleukin-33 (IL-33) and IL-33 receptors (sST2 and ST2L) in patients with rheumatoid arthritis. J Korean Med Sci. 2011;26(9):1132–9.
Talabot-Ayer D, et al. Distinct serum and synovial fluid interleukin (IL)-33 levels in rheumatoid arthritis, psoriatic arthritis and osteoarthritis. Joint Bone Spine. 2012;79(1):32–7.
Nagano K, et al. The tumor necrosis factor type 2 receptor plays a protective role in tumor necrosis factor-alpha-induced bone resorption lacunae on mouse calvariae. J Bone Miner Metab. 2011;29(6):671–81.
Atanga E, et al. TNFalpha inhibits the development of osteoclasts through osteoblast-derived GM-CSF. Bone. 2011;49(5):1090–100.
Goto H, et al. Primary human bone marrow adipocytes support TNF-alpha-induced osteoclast differentiation and function through RANKL expression. Cytokine. 2011;56(3):662–8.
Yarilina A, et al. TNF activates calcium-nuclear factor of activated T cells (NFAT)c1 signaling pathways in human macrophages. Proc Natl Acad Sci USA. 2011;108(4):1573–8.
Finzel S, et al. Repair of bone erosions in rheumatoid arthritis treated with tumour necrosis factor inhibitors is based on bone apposition at the base of the erosion. Ann Rheum Dis. 2011;70(9):1587–93.
Huang H, et al. Dose-specific effects of tumor necrosis factor alpha on osteogenic differentiation of mesenchymal stem cells. Cell Prolif. 2011;44(5):420–7.
Tsukasaki M, et al. Expression of POEM, a positive regulator of osteoblast differentiation, is suppressed by TNF-alpha. Biochem Biophys Res Commun. 2011;410(4):766–70.
Suzuki M, et al. Intercellular adhesion molecule-1 on synovial cells attenuated interleukin-6-induced inhibition of osteoclastogenesis induced by receptor activator for nuclear factor kappaB ligand. Clin Exp Immunol. 2011;163(1):88–95.
Cheung WY, Simmons CA, You L. Osteocyte apoptosis regulates osteoclast precursor adhesion via osteocytic IL-6 secretion and endothelial ICAM-1 expression. Bone. 2012;50(1):104–10.
Honda K. Interleukin-6 and soluble interleukin-6 receptor suppress osteoclastic differentiation by inducing PGE(2) production in chondrocytes. J Oral Sci. 2011;53(1):87–96.
Terpos E, et al. Early effects of IL-6 receptor inhibition on bone homeostasis: a pilot study in women with rheumatoid arthritis. Clin Exp Rheumatol. 2011;29(6):921–5.
Kanbe K, et al. Osteoprotegerin expression in bone marrow by treatment with tocilizumab in rheumatoid arthritis. Rheumatol Int. 2011;Jul 26.
Natsume H, et al. Wnt3a regulates tumor necrosis factor-alpha-stimulated interleukin-6 release in osteoblasts. Mol Cell Endocrinol. 2011;331(1):66–72.
Kato K, et al. AMP-activated protein kinase regulates PDGF-BB-stimulated interleukin-6 synthesis in osteoblasts: Involvement of mitogen-activated protein kinases. Life Sci. 2012;90(1–2):71–6.
Guo L, et al. Angiotensin II induces interleukin-6 synthesis in osteoblasts through ERK1/2 pathway via AT1 receptor. Arch Oral Biol. 2011;56(3):205–11.
Rego D, et al. IL-6 production is positively regulated by two distinct Src homology domain 2-containing tyrosine phosphatase-1 (SHP-1)-dependent CCAAT/enhancer-binding protein beta and NF-kappaB pathways and an SHP-1-independent NF-kappaB pathway in lipopolysaccharide-stimulated bone marrow-derived macrophages. J Immunol. 2011;186(9):5443–56.
Kamiya S, et al. IL-27 suppresses RANKL expression in CD4+ T cells in part through STAT3. Immunol Lett. 2011;138(1):47–53.
Halvorsen EH, et al. Interleukin-15 induces interleukin-17 production by synovial T cell lines from patients with rheumatoid arthritis. Scand J Immunol. 2011;73(3):243–9.
Hueber AJ, et al. Mast cells express IL-17A in rheumatoid arthritis synovium. J Immunol. 2010;184(7):3336–40.
• Pollinger B, et al. Th17 cells, not IL-17+ gammadelta T cells, drive arthritic bone destruction in mice and humans. J Immunol. 2011;186(4):2602–12. This study shows in vivo that IL-17 produced by Th17 cells promotes inflammatory bone loss while IL-17 secreted by γδ T cells is less important..
Abdollahi-Roodsaz S, et al. Destructive role of myeloid differentiation factor 88 and protective role of TIR-containing adaptor inducing interferon beta in IL-17-dependent arthritis. Arthritis Rheum. 2011, Dec 6.
Oostlander AE, et al. T cell-mediated increased osteoclast formation from peripheral blood as a mechanism for Crohn’s disease-associated bone loss. J Cell Biochem. 2012;113(1):260–8.
Park YE, et al. IL-17 increases cadherin-11 expression in a model of autoimmune experimental arthritis and in rheumatoid arthritis. Immunol Lett. 2011;140(1–2):97–103.
Zhang F, et al. Interleukin-17A induces cathepsin K and MMP-9 expression in osteoclasts via celecoxib-blocked prostaglandin E2 in osteoblasts. Biochimie. 2011;93(2):296–305.
Zwerina K, et al. Anti IL-17A therapy inhibits bone loss in TNF-alpha-mediated murine arthritis by modulation of the T-cell balance. Eur J Immunol. 2012;42(2):413–23.
Sadik CD, et al. IL-17RA signaling amplifies antibody-induced arthritis. PLoS One. 2011;6(10):e26342.
Pickens SR, et al. Anti-CXCL5 therapy ameliorates IL-17-induced arthritis by decreasing joint vascularization. Angiogenesis. 2011;14(4):443–55.
Rampersad RR, et al. Enhanced Th17-cell responses render CCR2-deficient mice more susceptible for autoimmune arthritis. PLoS One. 2011;6(10):e25833.
Kaiwen W, et al. Changes and significance of IL-25 in chicken collagen II-induced experimental arthritis (CIA). Rheumatol Int. 2011;May 29.
Yu M, et al. NF-kappaB signaling participates in both RANKL- and IL-4-induced macrophage fusion: receptor cross-talk leads to alterations in NF-kappaB pathways. J Immunol. 2011;187(4):1797–806.
Cheng J, et al. Interleukin-4 inhibits RANKL-induced NFATc1 expression via STAT6: a novel mechanism mediating its blockade of osteoclastogenesis. J Cell Biochem. 2011;112(11):3385–92.
Ma HM, Wu Z, Nakanishi H. Phosphatidylserine-containing liposomes suppress inflammatory bone loss by ameliorating the cytokine imbalance provoked by infiltrated macrophages. Lab Invest. 2011;91(6):921–31.
Kohara H, et al. IFN-gamma directly inhibits TNF-alpha-induced osteoclastogenesis in vitro and in vivo and induces apoptosis mediated by Fas/Fas ligand interactions. Immunol Lett. 2011;137(1–2):53–61.
Ayon Haro ER, et al. Locally administered interferon-gamma accelerates lipopolysaccharide-induced osteoclastogenesis independent of immunohistological RANKL upregulation. J Periodontal Res. 2011;46(3):361–73.
Cheng J, et al. Molecular mechanisms of the biphasic effects of interferon-gamma on osteoclastogenesis. J Interferon Cytokine Res. 2012;32(1):34–45.
Yasui T, et al. Regulation of RANKL-induced osteoclastogenesis by TGF-beta through molecular interaction between Smad3 and Traf6. J Bone Miner Res. 2011;26(7):1447–56.
Park MK, et al. IL-15 promotes osteoclastogenesis via the PLD pathway in rheumatoid arthritis. Immunol Lett. 2011;139(1–2):42–51.
Kim YG, et al. The influence of interleukin-32gamma on osteoclastogenesis with a focus on fusion-related genes. J Clin Immunol. 2012;32(1):201–6.
Pickens SR, et al. Local expression of interleukin-27 ameliorates collagen-induced arthritis. Arthritis Rheum. 2011;63(8):2289–98.
Hsu YH, Hsieh PP, Chang MS. Interleukin-19 blockade attenuates collagen-induced arthritis in rats. Rheumatology (Oxford). 2012;51(3):434–42.
Hsu YH, Chang MS. Interleukin-20 antibody is a potential therapeutic agent for experimental arthritis. Arthritis Rheum. 2010;62(11):3311–21.
Hsu YH, et al. Anti-IL-20 monoclonal antibody inhibits the differentiation of osteoclasts and protects against osteoporotic bone loss. J Exp Med. 2011;208(9):1849–61.
Kwok SK, et al. Interleukin-21 promotes osteoclastogenesis in rheumatoid arthritis in humans and mice. Arthritis Rheum. 2012;64(3):p740–51.
Marijnissen RJ, et al. Increased expression of interleukin-22 by synovial Th17 cells during late stages of murine experimental arthritis is controlled by interleukin-1 and enhances bone degradation. Arthritis Rheum. 2011;63(10):2939–48.
Kim KW, et al. IL-22 promotes osteoclastogenesis in rheumatoid arthritis through induction of RANKL in human synovial fibroblasts. Arthritis Rheum. 2011;Oct 27.
Guma M, et al. JNK1 controls mast cell degranulation and IL-1{beta} production in inflammatory arthritis. Proc Natl Acad Sci USA. 2010;107(51):22122–7.
Polzer K, et al. Proteasome inhibition aggravates tumor necrosis factor-mediated bone resorption in a mouse model of inflammatory arthritis. Arthritis Rheum. 2011;63(3):670–80.
Zwerina K, et al. Vitamin D receptor regulates TNF-mediated arthritis. Ann Rheum Dis. 2011;70(6):1122–9.
Bluml S, et al. Essential role of microRNA-155 in the pathogenesis of autoimmune arthritis in mice. Arthritis Rheum. 2011;63(5):1281–8.
Sugatani T, Vacher J, Hruska KA. A microRNA expression signature of osteoclastogenesis. Blood. 2011;117(13):3648–57.
Nakasa T, et al. The inhibitory effect of microRNA-146a expression on bone destruction in collagen-induced arthritis. Arthritis Rheum. 2011;63(6):1582–90.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Braun, T., Schett, G. Pathways for Bone Loss in Inflammatory Disease. Curr Osteoporos Rep 10, 101–108 (2012). https://doi.org/10.1007/s11914-012-0104-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-012-0104-5