Abstract
Summary
The influence of various stroke impairments on bone health is poorly understood. This study showed that muscle function and small artery compliance were more strongly associated with the bone strength index at the tibial diaphyseal and epiphyseal regions, respectively. These impairments should be targeted in promoting bone health post-stroke.
Introduction
This study examined the bone structural properties of the tibial distal epiphysis and diaphysis after chronic stroke and identified the clinical correlates of the bone strength index measured at these sites.
Methods
The tibial distal epiphysis (4 % site) and diaphysis (66 % site) were scanned on both sides in 66 chronic stroke patients and 23 control participants using peripheral quantitative computed tomography. Dynamic knee muscle strength, balance function, spasticity, arterial compliance, and endurance were also measured in the stroke group.
Results
At the 4 % site, multivariate analysis showed a significant side × group interaction effect (Wilk’s lambda = 3.977, p < 0.001), with significant side-to-side differences in total volumetric bone mineral density (vBMD), trabecular vBMD, and bone strength index in the stroke group, but not in the control group. A significant side × group interaction was also found at the 66 % site (Wilk’s lambda = 4.464, p < 0.001), with significant side-to-side differences in cortical vBMD, cortical area, cortical thickness, and bone strength index in the stroke group only. Balance and endurance were independently associated with bone strength index at both tibial sites in the paretic leg (p < 0.05) after adjusting for relevant factors in multivariate regression analysis. Small artery compliance and muscle strength were significantly associated with the bone strength index at the 4 % site and 66 % site, respectively.
Conclusions
The influence of various stroke impairments on bone was region-specific. While muscle function was more strongly associated with the bone strength index in the diaphyseal region, the effect of vascular health was more apparent in the tibial epiphysis in the paretic leg.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stroke is one of the most prevalent disabling conditions worldwide [1]. Fragility fractures are a common complication in stroke patients [2]. Approximately 4–6 % of stroke patients will sustain a fracture within 2 years after the onset of stroke, and the proportion will increase to about 11 % by 10 years post-stroke [2, 3]. Indeed, the risk of fractures after hospitalization for stroke can be more than seven times the rate of fracture in the general population [4]. The most common site where most post-stroke fractures occur is the hip region [2, 4]. The exaggerated fracture rate in this patient population can be partially attributable to accelerated bone loss following a stroke [5].
Earlier studies have used dual-energy X-ray absorptiometry to investigate the changes in hip bone mineral density post-stroke and found that the paretic side sustained a more severe loss than the non-paretic side [6]. More recent research, however, has used peripheral quantitative computed tomography (pQCT) to study the distal tibia as a surrogate [7–11], because the tibia in theory should be subject to similar loading patterns as the femur [7]. Studying the distal tibia/ankle remains clinically relevant, for several reasons. First, fractures in the distal tibia are not uncommon in people after stroke. In a cohort of 2,696 stroke patients, Dennis et al. [2] showed that out of 13 skeletal sites, the distal tibia/ankle region is the fourth most common site where fractures occur, accounting for 6.8 % of all fractures, only behind the hip (29.5 %), wrist (23.8 %), and ribs (8.0 %). Another study by Ramnemark et al. [12] found an even higher incidence of ankle fractures, accounting for 9 % of all fractures after stroke. Second, although the relationship between hip fracture risk and tibial bone strength index among stroke patients is uncertain, good correlations have been identified between hip bone mineral density derived from DXA and bone strength index of the tibia generated by pQCT in both the paretic and non-paretic legs (r = 0.6–0.8) [13]. Using pQCT to study tibial bone sites would also allow us to gain insight into how stroke influences bone geometry, which is also an important determinant of bone strength [14].
Previous pQCT studies have consistently found that tibial bone strength index in the paretic leg is substantially lower than that in the non-paretic leg, regardless of the measurement site [7–11]. Researchers have also endeavored to identify the clinical correlates of bone status in stroke patients. Identifying the modifiable stroke impairments that may have important effects on the integrity of bone tissue is essential for guiding the design of effective strategies that promote bone health in these patients. Only two pQCT studies have examined the clinical correlates of bone strength index measured at lower extremity long bone sites in individuals with stroke [7, 8]. At the tibial diaphysis, muscle mass and peak oxygen consumption rate (a measure of cardiorespiratory fitness) were identified as the major determinants of bone strength index in a sample of 55 patients with chronic stroke [7]. These same factors, in addition to mobility and spasticity, were shown to be associated with the compressive bone strength index measured at the distal tibia epiphysis in a cohort of 45 chronic stroke survivors [8] However, other important factors may have been overlooked in these studies. In particular, vascular health, which has been shown to be intimately associated with bone health in other populations, was not specifically evaluated [15–17]. It is also possible that the effects of stroke impairments on the same bone may be region-specific (e.g., epiphysis vs. diaphysis). For example, muscle strength may be more strongly associated with integrity of bone tissue at the diaphysis due to its proximity to insertions of major muscle groups. On the other hand, vascular health may be a more important factor in influencing bone health at the epiphyseal site, which is highly vascularized. To facilitate a more meaningful comparison of the relative effects of various stroke impairments on bone status at different sites, it is important that measurements of different bone sites are taken from the same sample of stroke patients, yet none of the previous pQCT studies has made such a comparison.
The current study was undertaken to address these knowledge gaps. To further strengthen the study design, a group of healthy control participants was included. The objectives of this pQCT study were to examine the bone status at the distal epiphysis and diaphysis of the tibia in patients with stroke and to identify the clinical factors associated with the bone strength index measured at these sites. It was hypothesized that the bone strength index on the affected side would be significantly lower on the unaffected side in both measurement sites of the tibia and that muscle function would be more strongly associated with bone strength index at the diaphyseal site, whereas the influence of vascular health would be more predominant at the epiphyseal site.
Methods
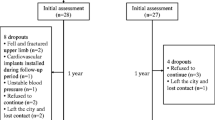
Participants
Individuals with stroke were recruited on a volunteer basis from community-based self-help groups for stroke patients (i.e., convenience sampling). All individuals were screened by the research personnel through a telephone interview. The inclusion criteria were a diagnosis of hemispheric stroke resulting in hemiparesis (Chedoke McMaster Stroke Assessment lower extremity composite motor impairment score <14) [18], at least 1-year post-stroke, adult aged ≥18, able to understand simple verbal commands, and medically stable. The exclusion criteria were recurrent stroke, other neurological disorders, serious musculoskeletal conditions (e.g., amputations), metal implants in a lower limb, recent fracture of a lower limb, taking medication for the treatment of osteoporosis before or after stroke (e.g., bisphosphonates), and other serious illnesses that prevented the individual from participating in the study (e.g., neoplasms). Control participants were recruited on a volunteer basis from the community. The eligibility criteria were the same as for the stroke group, except that these individuals did not have a history of stroke.
Ethical approval was obtained from the Human Research Ethics Review Committee of the University. The details of the study were explained to the participants before informed written consent was obtained. All of the experimental procedures were conducted in accordance with the Helsinki Declaration for human experiments.
Measurements
Demographics
Relevant demographic information (e.g., medications, stroke history) was collected through face-to-face interviews and a hospital discharge summary provided by the participants. The Physical Activity Scale for the Elderly (PASE) questionnaire [19], which has been used in previous research in stroke [20], was administered by the researcher to assess the participants’ physical activity levels. The Abbreviated Mental Test [21] and Chedoke McMaster Stroke Assessment [18] were administered to the stroke group to assess cognition and motor impairment, respectively.
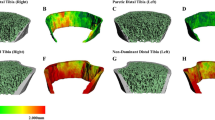
Bone imaging
Each participant in the stroke group and control group underwent scanning of the tibia on each side using pQCT (XCT 3000, Stratec Medizintechnik GmbH; Pforzheim, Germany). The anatomical reference line was positioned at the cortical end plate of the distal medial edge of the tibia. Scans (2.3 mm in thickness; scan speed at 25 mm/s, voxel size of 500 μm) were acquired at two different sites of the tibia: the tibial epiphysis (at 4 % of the total bone length proximal to the anatomical reference line, primarily a trabecular bone site) and the tibial diaphysis (at 66 % of the total bone length proximal to the reference line, mainly a cortical bone site).
The images of the 4 % site were analyzed using CALCB Contour Mode 2 and Peel Mode 2, with a density threshold of 169/400 mg/cm3. The variables of interest were total volumetric bone mineral density (vBMD), trabecular vBMD, total area, and compressive bone strength index (cBSI). The cBSI was calculated using the formula total vBMD2 × total area [22]. The cBSI has been validated in a human cadaver study and is considered to be a reasonable estimate of bone strength against compressive loads at the distal end of long bones, where axial compression is more predominant [22]. The precision of the pQCT scanner was evaluated by measuring 30 healthy participants twice, with repositioning after the first scan. The coefficients of variation of the above outcomes were 0.79, 0.47, 1.41, and 0.97 %, respectively.
Cortical bone analysis at the 66 % site was performed using CORTBD (Mode 1), with a threshold of 710 mg/cm3. The total area, cortical bone area, cortical bone mineral content (BMC), cortical vBMD, cortical thickness, marrow cavity area, and polar stress–strain index (p-SSI) were measured. The marrow cavity area was generated by subtracting the cortical area from the total area. The p-SSI, a validated bone strength index indicative of the torsional rigidity, is a more appropriate bone strength estimate at this site compared with cBSI, as torsional/bending forces are more predominant in the diaphyseal region [22, 23]. The coefficients of variation for the aforementioned variables were 1.70, 1.44, 0.47, 1.44, 1.05, 2.53, and 1.73 % respectively.
Knee muscle strength
The concentric and eccentric knee extensor work (in Joules or J) on both sides was measured using an isokinetic dynamometer (NUMAC® NORMTM Testing & Rehabilitation System, Computer Sports Medicine, Inc, Stoughton, MA, USA). Each participant sat upright with the trunk and thigh of the tested leg stabilized by straps and was then instructed to perform each type of knee muscle contraction with maximal effort at a constant angular speed of 60°/s, through a range of motion between 10° and 70° knee flexion. The sequence of concentric/eccentric/paretic leg/non-paretic leg testing was randomized to avoid an order effect. Three trials were recorded for each test condition, and the data were averaged to obtain the mean concentric and eccentric work (J) of each leg using customized software. Previous work has shown that these measurements have good test–retest reliability (intra-class correlation coefficient (ICC) 3,1 = 0.73–88) [24].
Balance function
The 14-item Mini-Balance Evaluation Systems Test (Mini-BESTest) was used to evaluate balance performance [25]. Each item was rated on an ordinal scale from 0 to 2, yielding a maximal score of 28, with higher scores indicating better balance ability. The Mini-BESTest has excellent intra-rater (ICC3,1 = 0.97) and inter-rater reliability (ICC2,1 = 0.96) when administered to people with stroke [25].
Spasticity
The Modified Ashworth Scale (MAS) was used to evaluate spasticity at the ankle joint on the paretic side. The ankle joint was moved into flexion and extension alternately by the researcher while the participant was in a supine position, and the amount of resistance to passive movement was noted. A higher MAS score (range = 0–4) is indicative of more severe spasticity [26]. The reliability of the MAS has been established for use with stroke patients (Kendall’s tau correlation = 0.847) [26].
Arterial compliance
Arterial compliance was evaluated using pulse wave contour analysis (HDI/PulseWave CR-2000 Research CardioVascular Profiling System; HDI Hypertension Diagnostics Inc., Eagan, MN, USA) [27]. Participants were placed in a supine position and asked to relax. A blood pressure cuff was applied to the left upper arm. With the right forearm in a supinated position, a piezoelectric-based acoustical sensor was applied over the radial artery in proximity to the radius styloid process. The sensor was adjusted so that the highest relative signal strength was acquired. A rigid plastic wrist stabilizer was then placed on the right wrist region to minimize the movement of the radial artery during measurement. Blood pressure was assessed using a linear dynamic deflation method. When the waveform was stable, the radial arterial blood pressure waveform data were obtained over a 30-s period and used for subsequent analysis [28]. Two trials were performed and the data were averaged. A 1-min rest period was given between measurements. The large artery elasticity index (C 1) and small artery elasticity index (C 2) were used as outcome measures. The C 1 index is an indicator of the compliance of the aorta and large arteries. Increased stiffness of the walls of these large arteries has been demonstrated in atherosclerotic disease [29]. The C 2 index represents the compliance of small arteries and arterioles, which has been associated with flow-mediated vasodilation [30] and risk of cardiovascular events [31]. The test–retest reliability of the system has been found to be excellent (ICC3,2 > 0.90) [9].
Endurance
The Six-Minute Walk Test (6MWT) was administered to assess endurance [32]. Participants were asked to walk along a 15-m corridor and cover as much distance as possible in 6 min. For those who were not ambulatory, the distance was recorded as zero. The 6MWT has excellent reliability (ICC = 0.97–0.99) in stroke patients [32].
Statistical analyses
The sample size calculation was performed using GPower 3.1 (Heinrich Heine Universitat Dusseldorf, Germany) and Statistic Calculator 3.0 (http://www.danielsoper.com/statcalc3/default.aspx) software programs, based on an alpha of 0.05 and power of 0.80. A previous study found a significant side-to-side difference in cortical BMC in the tibial diaphysis among people with chronic stroke, yielding a large effect size of 0.86 [7]. Assuming the same effect size, the estimated sample size required to detect significant between-group differences in side-to-side comparisons of pQCT parameters was estimated as 46 participants (23 people with stroke, 23 controls).
The main objective of this study was to examine the associations between bone strength and various stroke impairments. Research has shown certain stroke impairments (e.g., muscle weakness, cardiorespiratory fitness, and mobility) to be significantly associated with the compressive bone strength index (cBSI) or polar stress–strain index (p-SSI) of the hemiparetic tibia, yielding medium to large effect sizes (f = 0.2–1.1) [7, 8]. The addition of five stroke impairment variables to the regression model, over and above age, sex, post-stroke duration, and physical activity level, meant that a minimum sample size of 61 stroke patients was required for a hierarchical multiple regression analysis, assuming a medium to large effect size of f = 0.25.
Statistical analyses were performed using IBM SPSS software 20.0 (IBM, Armonk, NY, USA). The demographic characteristics of the stroke and control groups were compared using independent t tests (for continuous data), Mann–Whitney U tests (for ordinal data), and chi-squared tests (for nominal data). To compare the bone properties, multivariate analysis of variance (ANOVA) with a mixed design (within-participant factor: side; between-participant factor: group) incorporating all pQCT outcomes of interest was used to determine whether there was a significant side × group interaction. If a significant result was found for a particular outcome, post hoc paired t tests were performed to compare the two sides in the stroke group and control group separately. Next, the Pearson product–moment correlation coefficient (r) or Spearman’s rho, depending on the level of data, was used to determine the bivariate correlation between the stroke impairment variables (muscle strength, balance function, spasticity, arterial compliance, and endurance) and cBSI and p-SSI. Those variables that demonstrated a significant association with cBSI or p-SSI in the bivariate correlation analysis were then entered as independent variables in subsequent multiple regression analyses while accounting for the effects of age, sex, post-stroke duration, and physical activity level. To avoid possible multicollinearity, bivariate correlations among the independent variables were assessed. If there was a strong correlation (r > 0.5), the two independent variables were not entered into the same regression model [33]. The level of significance was set at 0.05; it was adjusted to 0.01 for the post hoc t tests and bivariate correlation analyses to avoid the probability of making type I errors being inflated due to multiple comparisons.
Results
Characteristics of participants
Sixty-six individuals with stroke and 23 control participants were enrolled in the study (Table 1). The mean Chedoke McMaster Stroke Assessment lower limb motor score was 7.6 out of 14, indicating moderate motor impairment. Forty-six individuals in the stroke group (69.6 %) required a mobility aid for locomotion. The stroke group had significantly lower physical activity levels and was taking a greater number of medications than the controls (p < 0.001).
The stroke-related impairments are displayed in Table 2. The concentric and eccentric knee extension strength on the paretic side was significantly lower than on the non-paretic side (p < 0.001) by 45.3 and 24.4 %, respectively (p < 0.001). The mean Mini-BESTest score was 19.3, indicating moderate impairment in balance function. Spasticity was rated as mild to moderate. While the majority of participants demonstrated normal C 1 values, C 2 was below the normal range in 55 participants (83 %). The mean 6MWT distance was also well below the median distance of 576 m for men (median age = 59.5, n = 117) and 494 m for women (median age = 62.0, n = 113) previously reported by Enright and Sherrill [34].
Tibial distal epiphysis
For the 4 % site, multivariate analysis revealed a significant side × group interaction (Wilk’s lambda = 3.977, p = 0.005). The total area was the only variable that did not show a significant side × group interaction in the univariate analysis. Post hoc analysis further showed that the total vBMD, trabecular vBMD, and cBSI values on the paretic side were significantly lower than their counterparts on the non-paretic side in the stroke group, whereas there were no significant side-to-side differences in these variables among the controls (Table 3). These trends were consistent in both the men and women (not shown).
The results of the bivariate correlation analysis are shown in Table 4. The cBSI on both sides was significantly associated with Mini-BESTest, C 2, and 6MWT scores (p < 0.001). As the Mini-BESTest and 6MWT were highly correlated (r = 0.745, p < 0.001), they were entered in separate regression models to predict cBSI to avoid multicollinearity. After accounting for age, sex, physical activity, and post-stroke duration, C 2 (p = 0.025) and Mini-BESTest (p = 0.007) remained independently associated with the cBSI on the paretic side, accounting for 5.9 and 7.4 % of the variance, respectively (Table 5, model 1). In the second regression model (model 2), the 6MWT was used as a predictor variable instead. After adjusting for the relevant factors, the association between the 6MWT and the cBSI remained significant and explained 8.7 % of the variance. On the non-paretic side, both the Mini-BESTest (model 3) and the 6MWT (model 4) were significantly associated with the cBSI, explaining 5.7 and 6.2 % of the variance, respectively. The relationship between C 2 and the cBSI in the non-paretic leg did not quite reach statistical significance (p = 0.057) (model 3).
Tibial diaphysis
For the 66 % site, multivariate ANOVA revealed a significant side × group interaction (Wilk’s lambda = 4.464, p = 0.001). All of the variables showed a significant side × group interaction except total area (p = 0.964) and marrow cavity area (p = 0.054) in the univariate analysis (Table 3). Post hoc analysis revealed that the cortical BMC, cortical vBMD, cortical bone area, cortical thickness, and p-SSI on the paretic side had significantly lower values (p < 0.01) than on the non-paretic side, whereas none of the pQCT variables showed significant side-to-side differences in the controls. Similar findings were obtained for both sexes (not shown).
The variables that were significantly associated with the p-SSI in the bivariate analysis (Table 4) were used for the subsequent regression analyses. After adjusting for relevant factors, eccentric leg muscle strength (Table 6, models 1 and 2), the Mini-BESTest (model 1), and the 6MWT (model 2) remained independently associated with the p-SSI on the hemiparetic side, explaining 3.1, 4.1, and 4.3 % of the variance, respectively. Separate regression models were used on the non-paretic side, as concentric and eccentric knee extension strength was strongly correlated (r = 0.781, p = 0.001). Eccentric (Table 6, model 3) and concentric knee extension strength (model 4) was found to be independently associated with the p-SSI on the non-paretic side, explaining 3.4 and 6.2 % of the variance, respectively. There were no concerns with multicollinearity in the regression models, as indicated by the low variance inflation factor (VIF) values (1.0–1.5) (Tables 5 and 6).
Discussion
The most interesting finding of this study was that muscle function was more strongly associated with bone strength index in the diaphyseal region, whereas the effect of vascular health was more apparent in the epiphyseal site of the tibia in the paretic leg.
Compromised bone strength index on the paretic side
Our findings confirmed the detrimental effect of stroke on the integrity of bone tissue. At the 4 % site, the lower cBSI on the paretic side was attributable to the lower vBMD, but not total area, which demonstrated no significant side-to-side difference (Table 3). This finding is consistent with a previous study involving a Canadian sample of chronic stroke survivors [8]. The results suggest that the paretic side may have sustained bone decorticalization, loss of trabecular elements, disruption of trabecular microstructure, or thinning of trabeculae [35], although the resolution of our pQCT scanner was not high enough to identify which of these mechanisms were operating.
The lower p-SSI on the paretic side at the 66 % site can be explained by both the compromised vBMD and bone geometry. Although the total area showed no side-to-side difference, the marrow cavity area was significantly larger on the paretic side, indicating the possibility of endosteal resorption after stroke (Table 3). Interestingly, a previous study reported a significantly smaller total area measured at the tibial diaphysis on the paretic side in female stroke survivors only, suggesting periosteal resorption [7]. There are several possible explanations for the discrepancy in the results. First, the studies used different measurement sites: We used the 66 % site whereas their study used the 30 % site. Second, although a direct comparison cannot be made due to the use of different outcome measurements, the women in our stroke group tended to have more severe motor impairments. For example, the proportion of walking aid users was higher in our study (70 %) than in theirs (31 %). Nevertheless, a prospective study is required to determine the actual geometric changes after stroke and whether the changes differ with sex.
Clinical correlates of bone strength index
While muscle strength, cardiorespiratory fitness, and mobility have been implicated as clinical correlates of bone strength measured at the tibial distal epiphysis [8] and diaphysis [7], this study is the first to show that the same stroke impairments have differential effects on the integrity of bone tissue at different sites of the tibia.
First, vascular health, as indicated by C 2, was independently associated with the bone strength index on the hemiparetic side at the 4 % site, but not at the 66 % site. A decline in C 2 represents an alteration in endothelial function in very small arteries and arterioles, which is an important indicator of progressive structural changes in vasculature. The 4 % site consists of mainly trabecular bone, which is more vascular and metabolically active than cortical bone, which is predominant at the 66 % site [36]. Changes in blood flow and endothelial function may thus have more effect on bone at the 4 % site. The finding that cardiovascular health may have a greater effect on trabecular than cortical bone sites has also been reported in two previous studies [7, 8]. Peak VO2 (an indicator of cardiorespiratory fitness) accounted for 10.8 % of the variance in the cBSI at the 4 % site in one study [8], whereas it contributed to only 5.8 % of the variance in the p-SSI at the 30 % site in another study [7]. A direct comparison with our study cannot be made due to the different outcome measures used. Unlike the pulse wave contour analysis used in our study, peak VO2 does not provide specific information on the integrity of the vascular system. In addition, we measured both skeletal sites in the same sample, enabling us to make a more meaningful comparison of the effect of stroke impairments on different bone sites. The pathophysiological mechanisms underlying the link between vascular function and bone metabolism are not entirely clear and will require further study, although oxidized lipids, homocysteine, and cytokines have been implicated [15, 36, 37]. We also found that vascular health had less influence on the 4 % site on the non-paretic side. It is possible that the presence of other stroke impairments on the paretic side (e.g., muscle weakness and reduced mechanical loading) may have made the bone tissue more sensitive to alterations in vascular health.
It is interesting that C 2, but not C 1, was significantly associated with the cBSI on the hemiparetic side. While both indices have been shown to be independently associated with subclinical coronary atherosclerosis [38], C 1 indicates the integrity of the large arteries, and its decline is indicative of more advanced vascular disease. In our sample, however, only a few individuals had C 1 values below the norm, which may partially explain the stronger relationship between the cBSI and C 2 compared to C 1. Nevertheless, the significant relationship between small artery compliance and bone strength index of the tibial distal epiphysis found in this study indicated that the detrimental effect on bone strength was apparent before the vascular disease progressed to an advanced stage.
In contrast, muscle strength was independently associated with the bone strength index at the 66 % site on both sides, but not the 4 % site. The strong association with muscle strength was not surprising, as the 66 % site is subjected to strong bending and torsional forces generated by muscle contractions. Indeed, this skeletal site is where the muscle belly is the largest [39], so the muscle–bone relationship should be more apparent. In contrast, the distal end of the tibia does not have major muscle attachments and is primarily subjected to compressive loads, which may account for the weaker relationship between bone strength and muscle strength. Such differential effects of muscle function on bone tissue at different skeletal sites were implicated in the two aforementioned stroke studies. Leg lean mass accounted for 12.1 % of the variance in the p-SSI at the 30 % site in one study [7] but explained only 8.2 % of the variance in the cBSI at the 4 % site in another [8]. While leg lean mass is related to muscle strength, the ability to voluntarily generate muscle force post-stroke is also dependent on other factors such as the strength of the central drive, the integrity of the descending motor pathways, the recruitment and synchronization of motor units, and biochemical changes in muscles. Direct measurement of muscle force would be a better indicator of muscle function. Using a single sample of stroke patients, this study has shown for the first time that muscle strength is more strongly associated with the integrity of bone tissue at the tibial diaphysis compared with the epiphysis.
It is surprising that eccentric, but not concentric, muscle strength was associated with the p-SSI on the paretic side. However, four of the participants in the stroke group, who had very different p-SSI values (range = 950.7–3,588.5 mm3), recorded zero concentric knee extension work, as they were unable to perform the contraction through the set knee range at the required speed (60°/s). In contrast, only one stroke patient recorded zero eccentric knee extension work. Additionally, the data for the eccentric work were more heterogeneous than those for the concentric data. Other than those who attained zero muscle strength values, the range of eccentric strength values varied from 18.0 to 128.7 J, compared with 5.7–75.9 J for concentric strength. It is well known that homogeneity of data contributes to lower correlations [40].
Balance function and endurance were independently associated with the bone strength index at both measurement sites on the paretic side. Maintaining body balance requires not only the ability to assume a symmetrical posture, but also the ability to efficiently shift the body weight from one leg to another in different functional activities such as reaching, transferring, and walking. Stroke patients often favor the non-paretic side and have poorer weight-bearing ability on the paretic side [41]. The reduced loading on the paretic limb, which is associated with poor balance function [41], may adversely affect bone quality at both the tibial epiphysis and diaphysis.
Another related factor is walking endurance. The distance achieved in the 6MWT has been significantly correlated with cardiovascular fitness in ambulatory people with chronic stroke [42]. This is consistent with previous findings that peak VO2 was independently associated with bone strength indices at both the epiphyseal and diaphyseal sites of the tibia [7, 8]. However, the ability to achieve a long 6MWT distance is also dependent on balance [42], which may explain the high correlation between the Mini-BESTest and the 6MWT found in this study. Those with poor 6MWT distances also have limited ambulatory activity [43]. The combination of reduced repetitive loading due to low ambulatory activity and impaired weight-bearing ability on the paretic side may account for the lower tibial bone strength index. The effect of balance function and endurance on the p-SSI on the non-paretic side was less remarkable, probably because the influence of muscle strength was more predominant on this side. In a study involving 23 people with stroke, Talla et al. [10] also showed that the muscle–bone relationship was stronger in the non-paretic than the paretic limbs. The mechanism underlying this phenomenon is unknown.
Clinical and research implications
This study identified several clinical correlates of post-stroke bone health that are highly modifiable. Specifically, vascular health was independently associated with bone strength index measured at the tibial distal epiphysis on the paretic side. Increasing research has focused on the link between cardiovascular health and bone health [15–17]. Our finding here may help open the field for research and potential clinical applications in cardiovascular function and bone health among individuals with stroke. For example, is there any potential of common therapeutic interventions [15]? Do pharmacological treatments used to improve vascular health have any impact on the integrity of bone tissue in stroke patients? Further research is needed in this important area.
Another clinical implication pertains to the potential use of non-invasive interventions such as exercise training to improve bone strength through modifying vascular health. To date, the effects of exercise training on arterial compliance in people with stroke are uncertain. Recent research has also shown impaired arterial compliance in other patient groups with limited physical activity, such as people after spinal cord injury [44]. In addition, it was also found that leg cycle ergometry with functional electrical stimulation was effective in improving small artery compliance among these patients [45]. It would be interesting to determine whether exercise training could improve small artery compliance and bone health post-stroke.
Apart from vascular health, we have also identified other clinical correlates of bone strength index. Muscle strength was independently associated with bone strength index at the tibial diaphysis, while balance and endurance were significant determinants of bone strength index at both the tibial diaphysis and distal epiphysis. Therefore, the physical exercise program should be multidimensional and address these different stroke impairments through a combination of resistance exercise, aerobic exercise, and balance training. A previous randomized controlled study provided preliminary evidence that circuit-based exercise training which incorporated muscle strengthening, balance, and aerobic activities may be beneficial for improving trabecular BMC at the 4 % site and cortical thickness at the 50 % site of the tibia in the paretic leg [20]. Further study is required to test the efficacy of different exercise intervention protocols on bone quality. As the relationship between bone strength index and stroke impairments seems to be region-specific, it would be interesting to determine whether different types of exercise (e.g., cardiovascular exercise versus muscle strength training) have differential effects on bone outcomes at different skeletal sites.
Limitations
This study was cross-sectional and could not provide information on the actual changes in bone outcomes over time. Although significant associations between the bone strength indices and certain stroke impairment variables were found, cause and effect could not be established. Our various regression models only explained 43.2–60.6 % of the variance in bone strength indices, indicating that some potentially important factors were not captured (e.g., nutrition). Future studies should use a larger sample size and examine the relationship between these factors and bone health in chronic stroke survivors.
Conclusion
In summary, the effects of various stroke impairments on bone tissue differed depending on the tibial sites measured. While the effects of vascular health were more apparent in the distal epiphysis of the tibia on the paretic side, muscle strength had more effect on the diaphyseal site.
References
Feigin VL, Lawes CM, Bennett DA et al (2009) Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol 8:355–369
Dennis MS, Lo KM, McDowall M, West T (2002) Fractures after stroke: frequency, types, and associations. Stroke 33:728–734
Whitson HE, Pieper CF, Sanders L, Horner RD, Duncan PW, Lyles KW (2006) Adding injury to insult: fracture risk after stroke in veterans. J Am Geriatr Soc 54:1082–1088
Kanis J, Oden A, Johnell O (2001) Acute and long-term increase in fracture risk after hospitalization for stroke. Stroke 32:702–706
Poole KES, Reeve J, Warburton EA (2002) Falls, fractures, and osteoporosis after stroke: time to think about protection? Stroke 33:1432–1436
Beaupre GS, Lew HL (2006) Bone-density changes after stroke. Am J Phys Med Rehabil 85:464–472
Pang MY, Ashe MC, Eng JJ (2008) Tibial bone geometry in chronic stroke patients: influence of sex, cardiovascular health, and muscle mass. J Bone Miner Res 23:1023–1030
Pang MYC, Ashe MC, Eng JJ (2010) Compromised bone strength index in the hemiparetic distal tibia epiphysis among chronic stroke patients: the association with cardiovascular function, muscle atrophy, mobility, and spasticity. Osteoporos Int 21:997–1007
Pang MYC, Cheng AQ, Warburton DE, Jones AYM (2012) Relative impact of neuromuscular and cardiovascular factors on bone strength index of the hemiparetic distal radius epiphysis among individuals with chronic stroke. Osteoporos Int 23:2369–2379
Talla R, Galea M, Lythgo N et al (2011) Contralateral comparison of bone geometry, BMD and muscle function in the lower leg and forearm after stroke. J Musculoskelet Neuronal Interact 11:306–313
MacIntyre NJ, Rombough R, Brouwer B (2010) Relationships between calf muscle density and muscle strength, mobility and bone status in the stroke survivors with subacute and chronic lower limb hemiparesis. J Musculoskelet Neuronal Interact 10:249–255
Ramnemark A, Nyberg L, Borssen B, Olsson T, Gustafson Y (1998) Fractures after stroke. Osteoporos Int 8:92–95
Lam FMH, Pang MYC (2013) The relationship between tibial bone parameters measured by quantitative computed tomography and hip bone density measured by dual-energy x-ray absorptiometry in chronic stroke patients. Hong Kong Physiother J 31:55. doi:10.1016/j.hkpj.2013.01.039
Augat P, Reeb H, Claes L (1996) Prediction of fracture load at different skeletal sites by geometric properties of the cortical shell. J Bone Miner Res 11:1356–1363
Farhat GN, Cauley JA, Matthews KA et al (2006) Volumetric BMD and vascular calcification in middle-aged women: the Study of Women’s Health Across the Nation. J Bone Miner Res 21:1839–1846
Naves M, Rodríguez-García M, Díaz-López JB et al (2008) Progression of vascular calcifications is associated with greater bone loss and increased bone fractures. Osteoporos Int 19:1161–1166
Collins TC, Ewing SK, Diem SJ et al (2009) Peripheral arterial disease is associated with higher rates of hip bone loss and increased fracture risk in older men. Circulation 119:2305–2312
Gowland C, Stratford P, Ward M et al (1993) Measuring physical impairment and disability with the Chedoke-McMaster Stroke Assessment. Stroke 24:58–63
Washburn RA, Zhu W, McAuley E et al (2002) The physical activity scale for individuals with physical disabilities: development and evaluation. Arch Phys Med Rehabil 83:193–200
Pang MYC, Ashe MC, Eng JJ et al (2006) A 19-week exercise program for people with chronic stroke enhances bone geometry at the tibia: a peripheral quantitative computed tomography study. Osteoporos Int 17:1615–1625
Chu L, Pei C, Ho M, Chan P (1995) Validation of the Abbreviated Mental Test (Hong Kong version) in the elderly medical patient. Hong Kong Med J 1:207–211
Kontulainen SA, Johnston JD, Liu D et al (2008) Strength indices from pQCT imaging predict up to 85 % of variance in bone failure properties at tibial epiphysis and diaphysis. J Musculoskelet Neuronal Interact 8:401–409
Lochmüller E-M, Lill CA, Kuhn V et al (2002) Radius bone strength in bending, compression, and falling and its correlation with clinical densitometry at multiple sites. J Bone Miner Res 17:1629–1638
Pang MYC, Lau RWK, Yip SP (2013) The effects of whole-body vibration therapy on bone turnover, muscle strength, motor function, and spasticity in chronic stroke: a randomized controlled trial. Eur J Phys Rehabil Med 49:439–450
Tsang CSL, Liao L-R, Chung RCK, Pang MYC (2013) Psychometric properties of the Mini-Balance Evaluation Systems Test (Mini-BESTest) in community-dwelling individuals with chronic stroke. Phys Ther 93:1102–1115
Bohannon RW, Smith MB (1987) Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther 67:206–207
Zimlichman R, Shargorodsky M, Boaz M et al (2005) Determination of arterial compliance using blood pressure waveform analysis with the CR-2000 system: reliability, repeatability, and establishment of normal values for healthy European population–the seven European sites study (SESS). Am J Hypertens 18:65–71
Hypertension Diagnostics Inc HDI (2005) HDI/PulseWaveTM CR-2000 Research Cardio Vascular Profiling System manual. USA HDI Hypertens. Diagnostics Inc., Eagan
Duprez DA, De Buyzere MML, De Bruyne L et al (2001) Small and large artery elasticity indices in peripheral arterial occlusive disease (PAOD). Vasc Med 6:211–214
Wilson AM, O’Neal D, Nelson CL et al (2004) Comparison of arterial assessments in low and high vascular disease risk groups. Am J Hypertens 17:285–291
Grey E, Bratteli C, Glasser SP et al (2003) Reduced small artery but not large artery elasticity is an independent risk marker for cardiovascular events. Am J Hypertens 16:265–269
Flansbjer U-B, Holmbäck AM, Downham D et al (2005) Reliability of gait performance tests in men and women with hemiparesis after stroke. J Rehabil Med 37:75–82
George D, Mallery P (2008) SPSS for windows step by step: a simple guide and reference. 15.0 update. Allyn and Bacon, Boston
Enright PL, Sherrill DL (1998) Reference equations for the six-minute walk in healthy adults. Am J Respir Crit Care Med 158:1384–1387
Riggs BL, Melton Iii LJ, Robb RA et al (2004) Population-based study of age and sex differences in bone volumetric density, size, geometry, and structure at different skeletal sites. J Bone Miner Res 19:1945–1954
Whitney C, Warburton DER, Frohlich J et al (2004) Are cardiovascular disease and osteoporosis directly linked? Sports Med 34:779–807
Parhami F, Morrow AD, Balucan J et al (1997) Lipid oxidation products have opposite effects on calcifying vascular cell and bone cell differentiation. A possible explanation for the paradox of arterial calcification in osteoporotic patients. Arterioscler Thromb Vasc Biol 17:680–687
Panaich SS, Zalawadiya SK, Veeranna V, Afonso L (2012) Association between arterial elasticity indices and coronary artery calcium in a healthy multi-ethnic cohort. Cardiology 123:24–30
Rittweger J, Beller G, Ehrig J et al (2000) Bone-muscle strength indices for the human lower leg. Bone 27:319–326
Glass GV, Hopkins KD (1996) Statistical methods in education and psychology, 3rd edn. Allyn & Bacon, Needham Heights
Kamphuis JF, De Kam D, Geurts ACH, Weerdesteyn V (2013) Is weight-bearing asymmetry associated with postural instability after stroke? A systematic review. Stroke Res Treat. doi:10.1155/2013/692137
Pang MYC, Eng JJ, Dawson AS (2005) Relationship between ambulatory capacity and cardiorespiratory fitness in chronic stroke: influence of stroke-specific impairments. Chest 127:495–501
Michael KM, Allen JK, MacKo RF (2005) Reduced ambulatory activity after stroke: the role of balance, gait, and cardiovascular fitness. Arch Phys Med Rehabil 86:1552–1556
Phillips AA, Cote AT, Bredin SS, Krassioukov AV, Warburton D (2012) Aortic stiffness increased in spinal cord injury when matched for physical activity. Med Sci Sports Exerc 44:2065–2070
Zbogar D, Eng JJ, Krassioukov AV, Scott JM, Esch BT, Warburton DE (2008) The effects of functional electrical stimulation leg cycle ergometry training on arterial compliance in individuals with spinal cord injury. Spinal Cord 46:722–726
Acknowledgments
This study was supported substantially by the Research Grants Council (General Research Fund no. 526708).
Conflicts of interest
Marco Y. C. Pang and Feigo Z. H. Yang declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, F.Z.H., Pang, M.Y.C. Influence of chronic stroke impairments on bone strength index of the tibial distal epiphysis and diaphysis. Osteoporos Int 26, 469–480 (2015). https://doi.org/10.1007/s00198-014-2864-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-014-2864-5