Abstract
Summary
Osteoporosis treatments reduce the risk of fractures. The objective of this study was to investigate adherence to treatment of osteoporosis and its association to fractures in Sweden. Adherence to treatment of osteoporosis in Sweden is poor, and time on treatment was found to be significantly associated with fracture incidence.
Introduction
The objective of this study was to estimate persistence and compliance to treatment of primary osteoporosis in Sweden. A second aim was to investigate the determinants of non-persistence and the association between adherence and fracture incidence.
Methods
Patients were identified through filled prescriptions for alendronate, risedronate, strontium ranelate, and raloxifene between 2005 and 2009 from the Swedish Prescribed Drug Register. Persistence was investigated using survival analysis. Medication possession ratio (MPR) was used to measure compliance in persistent patients. The outcome measure in the analysis of adherence and fracture incidence was hospitalized osteoporotic fractures.
Results
The final cohort consisted of 56,586 treatment-naïve patients (mean age 71, 86% women). A total of 51%, 35%, 25%, and 14% were still on treatment (switching allowed) after 1, 2, 3, and 4 years, respectively. Average MPR in persistent patients was 94.2% (CI95 94.2–94.3%). Compared with <1 month of therapy, treatment for 1 month to 1 year, 1 to 2 years, and 2 to 3 years was associated with a lower 3-year fracture incidence (HR 0.86, p = 0.091; HR 0.67, p < 0.001; and HR 0.59, p < 0.001, respectively). No significant relationship was identified between MPR and fracture risk.
Conclusions
Persistence to treatment of osteoporosis in Sweden is poor and approximately 50% of all treatment-naïve patients discontinue therapy within 1 year. Average refill compliance, estimated only while the patients were persistent, was found to be close to perfect. A strong association was identified between treatment persistence and fracture incidence, which calls for action to improve the current situation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a chronic progressive disease characterized by porous and weak skeletal bone. It is a major public health problem, affecting hundreds of millions of people worldwide [1], predominantly postmenopausal women [2]. During the past two decades, several medications have been made available for the treatment and prevention of osteoporosis. The primary aim of pharmaceutical therapy is to reduce the risk of osteoporotic fractures. However, patients need to take the medication for the intended duration (persistence) and according to treatment instructions (compliance) in order to receive the desired clinical benefit. Several studies have shown that persistence and compliance to treatment of osteoporosis is poor, resulting in suboptimal real-world treatment effectiveness. It has been estimated that between 18% and 78% of all patients persist with therapy for 1 year [3, 4]. However, there are significant methodological differences between previous studies and the results are therefore not necessarily comparable. Moreover, disease patterns and treatment practices differ between countries and regions and previous findings may consequently only be valid for the population and setting studied. It is therefore necessary to obtain country-specific estimates. To date, persistence and compliance to treatment of osteoporosis in Sweden is unknown.
The determinants of low persistence and compliance to treatment are not very well understood. Research suggests that several factors are important, including dosing requirements and frequency, adverse events, the patient–physician relationship, and patient inability to detect improvements in an asymptomatic disease [5–10].
The main objective of the present study was to estimate persistence and compliance to treatment of primary osteoporosis in Sweden. A second study aim was to investigate the determinants of non-persistence as well as the association between persistence and fracture incidence and compliance and fracture incidence, respectively.
Methods
Data sources and patient selection
The study was based on an open historical cohort extracted from the Swedish Prescribed Drug Register. The register contains all filled prescriptions dispensed by “Apoteket AB”, the (at the time of study) sole provider of prescription drugs outside the hospital setting to the Swedish population (9,345,135 individuals [11]). Patients aged 50 or older were identified through records of filled prescriptions for one or several osteoporosis drugs (alendronate, risedronate, strontium ranelate, and raloxifene) between June 1, 2005 and December 31, 2009. A separate persistence analysis was performed on patients filling prescriptions for parathyroid hormone (PTH) during the same study period. Zoledronate and etidronate were not represented in the study since the former medication received reimbursement recently (and therefore had an unsatisfactory follow-up) and because etidronate is prescribed sparingly in combination with calcium. Treatment with hormone replacement therapy is no longer recommended in Sweden for fracture prevention except under special circumstances [12] and was consequently not included in the study. Patients with records of filled prescriptions for any osteoporosis treatment 5 months prior to the start of their treatment in this study were excluded. The length of the mandatory drug-free period was chosen to comprise a standard 3-month prescription and the base case grace period (described later) and was not extended due to data limitations. Included patients are henceforth referred to as “treatment-naïve.” Patients filling prescriptions that would last more than 112 days with standard osteoporosis treatment, indicating secondary caused osteoporosis, were also removed from the cohort. The Swedish Prescribed Drug Register was linked to the National Patient Register to extract patient level inpatient care fracture and comorbidity data 5 years prior to the index prescription. Patients with neoplasms (malignant, in situ, uncertain) or secondary osteoporosis, identified with ICD-10 codes (C.x, D00.x-D09.x, D35.1-D35.2, D37-D48, E03.9, E05.x, E21.0, E23.0-E24.0, E24.2-E24.4, E24.8-E24.9, E27.1, E72.1, E83.1, F50.0, G40.x, G81.9, K72.x, K90.x, M05.x-M06.x, M80.1, M80.3-M80.5, M81.1, M81.3-M81.5, M82.x-M83.x, M86.x-M90.x, N17.x-N19.x, Q79.6, Q82.2, Q96, and Q98.0-Q98.4), were excluded. Patients exposed to high levels of oral glucocorticoid drugs (defined as more than 2 g of accumulated glucocorticoid medication 12 months prior to index prescription [13]) were also removed from the cohort. Dates of deaths were collected from the Causes of Death Register. Patient identifiers were encrypted, and an ethical approval was granted by the Regional Ethical Review Board in Stockholm.
The quality and accuracy of the Swedish national registers are high. On average, 98.6% of all inclusions in National Patient Register are entered correctly and the frequency of missing values is very low. Missing values in the Causes of Death Register is less than 0.5%, and the loss of patient information in the Swedish Prescribed Drug Register is at maximum 0.6% [14]. In the present study, patients with missing values and/or ambiguous coding were excluded.
The primary outcome measure in the analysis of adherence and fracture incidence was hospitalized osteoporotic fractures. Patient level fracture data was extracted from the National Patient Register. The study included fractures to the neck (S12.x), rib, sternum, and thoracic spine (S22.x), lumbar spine and pelvis (S32.x), shoulder and upper arm (S42.x), forearm (S52.x), femur (including hip) (S72.x), lower leg (including ankle) (S82.x), as well as unspecified osteoporotic fractures (M80.0, M80.2, and M80.8-M80.9). Information regarding the causes of the fractures (determined by the physician) was available, but the coverage was incomplete, and all fractures were therefore included in the main analysis. Fractures caused by low energy trauma, defined as fall from the same level, were explored in sensitivity analysis.
Terminology
Several different definitions and categorizations of medication adherence, persistence, and compliance have been suggested in the literature [15]. The following definitions were used in this study:
Adherence
In this study, adherence was used as a general term encompassing both persistence and compliance.
Persistence
In a medical context, persistence may be defined as the accumulation of time from treatment initiation to discontinuation of therapy (i.e., time on treatment). In this study, the term was operationalized as the number of days on treatment.
Compliance
Medication compliance refers to the extent the patient acts in accordance with the prescribed treatment regimen. Ideally, the term should include aspects such as if the drug was taken correctly (e.g., after fasting overnight), at the correct time of day, whether larger doses were taken to compensate for forgotten doses, et cetera. Due to the nature of historical data, the only part of compliance that may be measured in retrospective studies is unplanned drug holidays (i.e., when the patient does not have medication available). In the present study, compliance was quantified as medication possession ratio (MPR) and measured only during the period of time patients were on treatment.
Measuring persistence and compliance
Medication persistence was operationalized as number of days on treatment and measured from index prescription until the end of the duration of the last prescription. Patients were allowed to have gaps between filled prescriptions, but were defined non-persistent if they had a gap exceeding 8 weeks (the “grace period”). Grace periods of 4 and 12 weeks were explored in sensitivity analysis. Hospitalizations during the observation period were taken into account by adding the time at the hospital as an extra prescription. The analysis took into account that some patients returned their medication to the pharmacy. The Swedish pharmacy system allows patients to refill prescriptions when two thirds of the previous refill has been consumed (e.g., after 2 months of a 3-month prescription) and diligent patients may thus accumulate large amounts of pills. Patients were therefore permitted to accumulate medication from overlapping prescriptions and use it to cover future gaps between filled prescriptions. However, patients not refilling within the grace period after consuming any accumulated medication were not allowed to consume their accumulated medication at all and were instead deemed non-persistent after depleting their last filled prescription. Consequently, the decision rule permitted patients to consume their accumulated medication as long as they afterwards filled a new prescription within the grace period.
Treatment switching was defined as initiation of therapy with another of the included osteoporosis medications within the grace period. To avoid underestimating true persistence, switching between the included medications was allowed when establishing persistence status for all treatments combined. Switchers were excluded when persistence was estimated for the individual treatment types.
Medication compliance was quantified using MPR, defined as the number of days of medication available to the patient, divided by the number of days on treatment. MPR was estimated only while the patient was persistent. For example, a patient who persisted with therapy for 365 days but only filled prescriptions with medication covering 325 days would have had an estimated MPR of (325/365) × 100 ≈ 89%.
Statistical analysis
Persistence estimates were derived using non-parametric survival analysis. Kaplan–Meier survival functions were estimated with treatment termination as failure event. Patients were right censored for death and the data limit of the Swedish Prescribed Drug Register (December 31, 2009). The determinants of non-persistence were investigated with a parametric multivariate proportional hazards model and estimated on the same set of survival data used in the analysis of persistence.
The relationship between persistence and fracture incidence was estimated with a parametric multivariate proportional hazards model with hospitalized osteoporotic fracture as failure event (multiple fractures allowed). The incidence of fractures was measured from treatment initiation until register limit (December 31, 2008) or death, irrespective of persistence status. Persistence was included as categories of time on treatment (<1 month, 1 month to 1 year, 1 to 2 years, and 2 to 3 years). The relationship between compliance and fracture incidence was investigated in a similar approach, quantifying compliance as per-patient mean MPR and measuring the incidence of fractures during time on treatment.
The parametric models were specified to include age, sex, urban/rural living, weekly/daily dosing regimen, prevalent hospitalized fracture, individual comorbidities (as defined by Charlson et al. [16]), institutionalized living (“ApoDos”), low-level exposure to glucocorticoid medication (defined as less than or equal to 2 g of accumulated glucocorticoid medication 12 months prior to index prescription), and filled prescription for gastroprotective agent (proton pump inhibitor, H2-receptor antagonist, sucralfate, and/or alginic acid) during the first 6 months of osteoporosis treatment, to control for confounding effects (Table 1). The variable “ApoDos” indicates that the patient received predispensed medication in a special living accommodation and was used as a proxy for being institutionalized. Model distribution (Weibull) and covariate selection for the parametric multivariate proportional hazards models were chosen by minimizing the Akaike information criterion and maximizing the log-likelihood, two metrics commonly used to discriminate between models. The proportional hazards assumption [17] was investigated using graphical inspections and by exploring if the included covariates significantly varied with time. The assumption was satisfied for all covariates. The statistical analyses were executed in Stata 11, StataCorp, Collage Station, TX.
Results
Study population
The final cohort consisted of a total of N = 56,586 subjects (Fig. 1), contributing a total of 61,322 person years of observation time. Table 1 contains summary of baseline characteristics for the included patients. Approximately 86% of the cohort was women, and 95% of all patients were on a weekly dosing regimen. Less than 3% of all included patients switched between the included medications while on treatment. The maximum follow-up (days on treatment) was 1,491 days (December 1, 2005 through December 31, 2009). Furthermore, the final cohort filled a total of 406,949 prescriptions between December 1, 2005 and December 31, 2009. Out of all prescription records, 84% were for alendronate, 14% risedronate, 0.66% for strontium ranelate, and 1.62% for raloxifene.
A total of 399 treatment-naïve patients with primary osteoporosis initiated therapy with PTH during the study period. Out of those, 257 individuals (mean age 69 years, 98% women) did not fill prescriptions for any other osteoporosis medication.
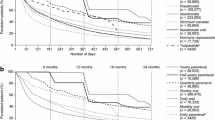
Statistical analysis of persistence
The estimated Kaplan–Meier life table is presented in Table 2, including significantly different estimates for women and men (log-rank test, p < 0.001). A large proportion (23%) of the total cohort terminated treatment immediately after the duration of the index prescription. Median time on treatment, defined as the earliest time at which half of the study participants had discontinued treatment, was 378 days. The parametric hazards model employed to investigate the determinants of non-persistence predicted a mean time on treatment of 711 days (controlling for variables listed in Table 1). Of the oral treatments, patients taking bisphosphonates had the highest persistence rates, followed by raloxifene and strontium ranelate (Fig. 2). The persistent proportion after 1 year of treatment was estimated at 51.7% (CI95 51.2–52.2%), 50.6% (CI95 49.5–51.8%), 42.4% (CI95 38.7–46.0%), and 18.4% (CI95 15.5–21.6%) for alendronate, risedronate, raloxifene, and strontium ranelate, respectively. The proportion persisting with PTH, the only injectable treatment in the study, for 1 year was 70.3% (CI95 64.0–75.8%). Persistence with PTH decreased markedly after approximately 18 months of therapy, in line with Swedish treatment guidelines which recommend that consecutive treatment with PTH should not exceed 18 months [12].
Sensitivity analysis of the grace period was performed by allowing gaps without medication between filled prescriptions of 4 and 12 weeks, respectively. Persistence rates were found to be fairly insensitive to the length of the grace period, as the estimated proportion on treatment never deviated more than 7 percentage units from the base case scenario (8-week grace period) for any treatment at any time point.
Statistical analysis of compliance
Compliance was quantified as MPR and measured while the patients were on treatment. Mean MPR was estimated at 94.2% (CI95 94.2–94.3%). Approximately 38% of the cohort had a MPR of 100% (i.e., no gaps between prescriptions) and approximately 95% had a MPR greater than 80%. Varying the grace period from 8 weeks to 4 and 12 weeks, respectively, had a trivial impact on the estimated mean MPR, only causing variation of less than 2 percentage units.
Statistical analysis of the determinants of non-persistence
A multivariate Weibull model was estimated to identity variables that were significantly associated with non-persistence. The covariates that were under consideration are presented in Table 1. The final estimated model is presented in Table 3. The model could on average predict 15.6% (p < 0.001) of the observed treatment duration for the included subjects. Individuals who received a weekly dosing regimen were estimated to have better persistence compared with those given daily dosing. Switching, being institutionalized, being female, and starting treatment with a prevalent fracture were also found to be significantly associated with a lower probability of terminating treatment. Moreover, individuals living in an urban region, as well as patients who filled at least one prescription for a gastroprotective agent during the first 6 months of osteoporosis treatment, were less likely to persist with therapy. Patients with any prevalent comorbidity or history of low-level glucocorticoid exposure were also found to have an increased risk of terminating treatment. A crude analysis of persistence with weekly and daily dosing regimens was performed for patients prescribed alendronate and risedronate (Fig. 3; log-rank test, p < 0.001).
Statistical analysis of adherence and fracture incidence
Two multivariate Weibull models were constructed to investigate the association between persistence and fracture incidence and compliance and fracture incidence, respectively. In total, 2,980 fractures were identified and approximately 2% of all patients sustained more than one fracture. Persistence (days on treatment) was found to be significantly inversely associated with 3-year incidence of hospitalized fractures (p < 0.001). Figure 4 presents estimated HRs for four treatment durations (<1 month as reference): 1 month to 1 year (HR 0.86, CI95 0.72–1.02), 1 to 2 years (HR 0.67, CI95 0.56–0.82), and 2 to 3 years (HR 0.59, CI95 0.48–0.72).
Relative risk of fracture for different treatment durations. Note: Robust estimates were obtained using the Huber–White estimator of variance. The HRs were estimated with a multivariate Weibull hazards model allowing for multiple fractures. The black bars represent bootstrapped 95% CI and should be interpreted in relation to the reference treatment length (<1 month). The overall trend was tested separately employing days on treatment (i.e., persistence) as a continuous covariate (p < 0.001). The following covariates were included in the estimated model: sex, age, urban region, ApoDos (institutionalized patient), weekly regimen, switcher, prior fracture (neck, rib, sternum, and thoracic spine; lumbar spine and pelvis; shoulder and upper arm; forearm; femur (including hip); lower leg (including ankle), unspecified fracture), prevalent comorbidities (myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic pulmonary disease, rheumatologic disease, peptic ulcer disease, mild liver disease, diabetes without chronic complication, diabetes with chronic complication, hemiplegia or paraplegia, renal disease, moderate or severe liver disease, HIV/AIDS), low-level exposure to glucocorticoid medication, and filled prescription for gastroprotective agent during the first 6 months of osteoporosis treatment
In addition, increased fracture rates were found in patients who were of old age (per year; HR 1.05, CI95 1.04–1.05), living in an urban region (HR 1.13, CI95 1.03–1.25), switched treatment (HR 1.42, CI95 1.12–1.76), and were institutionalized (HR 2.54, CI95 2.23–2.88). Being female, dosing regimen, and starting treatment with a gastroprotective agent did not have any significant impact on the estimated hazard ratios. Individuals with a history of low-level glucocorticoid exposure had, on average, a 17% lower fracture risk (HR 0.83, CI95 0.72–0.95). Prevalent hospitalized fracture was, on average, associated with an increased 3-year fracture incidence (HR 1.93, CI95 1.73–2.14). Including only fractures with defined low energy coding (51% of all fractures) yielded similar hazard ratios and model fit characteristics as the main analysis. No statistically robust relationship was identified between compliance (measured as MPR) and fracture risk.
Discussion
Treatment adherence
Persistence to treatment of osteoporosis has been shown to be poor in many countries and the median treatment duration rarely exceeds 1 year [3, 4]. Treatment persistence in Sweden appears to be in line with these findings. The reasons for the low persistence rates cannot be elicited from the present study, but deserves further investigation. Differentiated persistence estimates by the included medications in the main analysis revealed that patients on oral bisphosphonates were least likely to discontinue treatment, followed by raloxifene. Persistence with strontium ranelate was markedly lower, with approximately 18% remaining on treatment after 1 year. Although introduced on the Swedish market in September 2004, not a single patient included in this study persisted with strontium ranelate for the entire observation period. The reasons for this are unclear but physicians’ and patients’ concerns with adverse events and dosing convenience may be possible explanations. Due to limited patient follow-up, it was not possible to explore if patients who discontinued therapy restarted treatment at a later point in time (>6 months or even years later). This is likely to occur to some extent and should be the focus of future research.
Persistence with PTH was noticeably better compared with the other treatments. PTH is different from the other included therapies as it is only recommended for patients with a T-score below −3.0 SD and two or more vertebral fractures. In addition, PTH is only prescribed by specialists, who can be expected to have more experience and knowledge regarding pharmaceutical fracture prevention compared with the general health care practitioner, and may therefore be more inclined to ensure that these relatively fragile patients adhere to therapy. As expected, discontinuation rates for PTH increased rapidly in relation to the 1.5-year mark, since the treatment in Sweden only is reimbursed for durations up to that time point. Accordingly, our results suggest that prescribers adhere to current prescription guidelines for treatment with PTH.
Compliance while on treatment was found to be very high; average MPR was estimated at 94%, noticeably higher than findings by other researchers [3]. A possible reason for this result, in addition to actual differences in medication possession and structural characteristics of the Swedish health care system, is methodological differences in the calculation of MPR. In the present study, MPR was only measured while the patient was still on treatment, while other studies, for example Siris et al. [18] and Cramer et al. [19], measured MPR during a fixed time frame. The estimates are therefore not necessarily comparable. It should be noted that when a fixed time frame is used, the estimated MPR is directly related to the chosen length of the frame, and the measure is therefore a combination of both persistence and compliance. A fixed frame may also result in problems concerning the interpretation of the association between MPR and outcome variables, e.g., fracture incidence, since taking every other dose for 2 years will not necessarily have the same impact on fracture risk as taking every dose for 1 year and then stopping treatment. We therefore recommend that MPR is measured in a way that distinguishes compliance from persistence, which is desirable if the results are to be used in either decision making or decision analytic modeling.
Neither the estimates of persistence or compliance were sensitive to the length of the grace period. These results, together with the estimated high mean MPR, indicate that patients in Sweden generally had few and short gaps between filled prescriptions and therefore discontinued treatment in relation to their last filled prescription (and not because they had a break in treatment exceeding the grace period).
The investigation of the determinants of non-persistence showed that institutionalized patients had a significantly lower risk of terminating treatment compared with non-institutionalized subjects. This may be explained by the fact that individuals receiving care in an institutionalized setting are monitored and therefore receive assistance to persist with therapy. Women were found to be significantly more persistent to treatment (compared with men), as well as patients with a prevalent fracture. The latter finding may be explained by stronger support and encouragement from prescribers to continue with therapy after a fracture event (because of the increased fracture risk). Also, the patient may be more aware of the consequences of the disease if it were to be left untreated. In agreement with previous research, weekly dosing regimens were found to be related to better persistence compared with daily dosing [20, 21]. Furthermore, patients who switch therapy while on treatment were found to have higher persistence rates, which also have been shown in previous studies [22]. As expected, switchers had lower persistence if only the index medication was taken into account, but higher when all consecutive medications were included. Lastly, subjects with any prevalent comorbidity were found to have lower persistence. This may be explained by the fact that patients with many concomitant diseases receive several treatments and therefore may find it more problematic to persist with their osteoporosis treatment since the medication is not essential to survival and the disease is asymptomatic. It should be noted, however, that the model was only able to predict approximately 16% of the observed treatment durations and the estimated hazard ratios discussed above should consequently be interpreted with some caution.
Treatment adherence and fracture incidence
The estimated relative risk of 3-year fracture incidence was significantly associated with treatment persistence within that time frame. The estimated hazard ratios relate the total treatment exposure to fracture incidence over 3 years and should thus not be interpreted as a change in risk reduction over time. On the contrary, the linear decrease of our estimated hazard ratios over time indicate that risk reductions are similar over time and that real-world effectiveness in persistent patients is in line with estimates of trial-based efficacy [23–25].
Patients with records of filled prescriptions for high doses of glucocorticoids (more than 2 g during the last 12 months) are more likely to have concomitant diseases and high fracture risk [26] and were, together with other well-known secondary causes of osteoporosis, excluded from our sample. However, patients with low-level exposure to glucocorticoids 1 year prior to index prescription were included and were found to have a lower fracture risk compared with non-users. This may seem counterintuitive given that use of glucocorticoids has been shown to dose-dependently increase fracture risk [26]. A possible reason for the lower estimated fracture risk is that glucocorticoid users receiving bisphosphonates may have a higher bone mineral density (BMD)and therefore lower fracture risk compared with the typical osteoporotic patient, since use of glucocorticoids is an independent factor for initiation of antifracture treatment [13].
No statistically robust relationship was found between compliance, measured as MPR while the patients were on treatment, and the incidence of fractures. Approximately 96% of patients had an MPR >80%, which is a commonly cited threshold for sufficient compliance [18, 27], and it was therefore difficult to draw any conclusions whether or not treatment gaps in persistent patients were associated with fracture risk.
Limitations
Adherence is problematic to measure in prospective studies because patients are likely to change their behavior when observed. Retrospective register studies, on the other hand, utilize historical prescription data and are therefore not troubled by bias caused by the study’s impact on patient behavior. They are also less labor intensive and expensive compared with prospective investigations. The retrospective approach has for these reasons been commonly employed in studies of prescription patterns. However, a limitation with retrospective studies lies in the fact that data may not be available on all variables of interest to the researcher. Due to such data limitations, it was not possible to control for bone mineral density, socioeconomic variables, lifestyle factors, or a general “healthy adherer effect” in the present analyses. Non-adherent patients have been reported to have more comorbidities, be more frail, and have higher health care expenditures [27–29] and confounding may consequently explain some part of the estimated association between adherence and fracture incidence. We attempted to alleviate this problem by controlling for all available and relevant variables, including comorbidities, prior fractures, living location, use of glucocorticoids, and institutionalization.
A second limitation of the present study is that only hospitalized fractures were included in the analyses. The association between adherence and fracture incidence should therefore be interpreted with some caution. Furthermore, the National Patient Register contains information regarding the cause of the fracture (low/high energy trauma), but the coverage is not complete (35% missing or unspecified fracture causes). All fractures were therefore taken into account in the analyses, which may have overestimated the incidence of hospitalized osteoporotic fractures. However, our estimated hazard ratios for persistence and fracture incidence indicate that treatment had similar effect on low energy fractures, which to some extent justifies including all fractures in the statistical models.
The present study of persistence and compliance was based on a cohort of patients who were supposed to be treatment-naïve. A washout period of 5 months was used to capture individuals who had not previously been treated with any osteoporosis medication, and it was not extended due to data limitations. The purpose was to avoid including patients who previously had terminated treatment, i.e., to measure persistence and fracture incidence in an already non-persistent population. Medication persistence in a non-treatment-naïve population could be different, for example because fracture risk would possibly be affected by the residual effect (offset) from past treatments [30]. However, it may be the case that the 5-month mandatory drug-free period was insufficient and that a proportion of the included subjects already had been on treatment previously. The implication of this potential bias is not clear.
Policy aspects
Osteoporosis is a chronic disease requiring long-term therapy. It is therefore important that osteoporotic patients adhere to therapy. However, the optimal duration of treatment of osteoporosis remains to be defined [30, 31]. Although it has been shown that the effects of continuous treatment with alendronate sustain over a 10-year period [32], there are concerns that long-term suppression of bone remodeling may eventually lead to reduced bone strength [31, 33, 34]. In Sweden, the recommended duration of treatment of osteoporosis is 3 to 5 years [12].
This study has shown that persistence to treatment of primary osteoporosis in Sweden is poor, not in line with treatment guidelines, and should be recognized as a serious problem in the medical management of osteoporotic patients. Previous clinical and health economic research on treatment of osteoporosis has to a large extent been concerned with relative fracture risk reductions estimated in randomized controlled trials. However, medication adherence has been shown to be an equally important aspect of successful pharmacotherapy [35]. Drugs only work if patients take them, and poor adherence to treatment of osteoporosis will consequently result in that the public health objectives of fracture reduction are not met.
Moreover, patients who terminate therapy prematurely will have a higher fracture risk compared with patients who remain on therapy for the entire treatment duration. A higher fracture risk results in a higher incidence of fractures, reduced quality of life and increased mortality for the patient, and larger health care costs for the society. Thus, poor adherence is associated with a burden, both for the individual patient and from a societal perspective. Additional research is needed to assess the societal burden of unsatisfactory treatment adherence, how the problem should be addressed, and whether it would be cost-effective.
Conclusion
Persistence to treatment of osteoporosis in Sweden is poor and approximately 50% of all treatment-naïve patients discontinue therapy within 1 year. Average refill compliance, estimated only while the patients were persistent, was found to be close to perfect. A strong association was identified between treatment persistence and fracture incidence, which calls for action to improve the current situation.
References
Reginster JY, Burlet N (2006) Osteoporosis: a still increasing prevalence. Bone 38:S4–S9
EFFO, NOF (1997) Who are candidates for prevention and treatment for osteoporosis. Osteoporos Int 7:1–6
Kothawala P, Badamgarav E, Ryu S, Miller RM, Halbert RJ (2007) Systematic review and meta-analysis of real-world adherence to drug therapy for osteoporosis. Mayo Clin Proc 82:1493–1501
Cramer JA, Gold DT, Silverman SL, Lewiecki EM (2007) A systematic review of persistence and compliance with bisphosphonates for osteoporosis. Osteoporos Int 18:1023–1031
Tosteson AN, Grove MR, Hammond CS, Moncur MM, Ray GT, Hebert GM, Pressman AR, Ettinger B (2003) Early discontinuation of treatment for osteoporosis. Am J Med 115:209–216
Lamberg L (2000) Patient-physician relationship critical even during brief “medication checks”. Jama 284:29–31
Eraker SA, Kirscht JP, Becker MH (1984) Understanding and improving patient compliance. Ann Intern Med 100:258–268
Cramer JA (1995) Relationship between medication compliance and medical outcomes. Am J Health-Syst Pharm 52:S27–S29
Claxton AJ, Cramer J, Pierce C (2001) A systematic review of the associations between dose regimens and medication compliance. Clin Ther 23:1296–1310
Carr AJ, Thompson PW, Cooper C (2006) Factors associated with adherence and persistence to bisphosphonate therapy in osteoporosis: a cross-sectional survey. Osteoporos Int 17:1638–1644
SCB, Statistics Sweden. Available from: http://www.scb.se
The Swedish Medical Products Agency (2007) Behandling av osteoporos. Information från Läkemedelsverket 18:19–38
Ettinger B, Chidambaran P, Pressman A (2001) Prevalence and determinants of osteoporosis drug prescription among patients with high exposure to glucocorticoid drugs. Am J Manag Care 7:597–605
The National Board of Health and Welfare. Available from: http://www.socialstyrelsen.se
Cramer JA, Roy A, Burrell A, Fairchild CJ, Fuldeore MJ, Ollendorf DA, Wong PK (2008) Medication compliance and persistence: terminology and definitions. Value Health 11:44–47
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA (2005) Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 43:1130–1139
Hosmer D, Lemeshow S (1999) Applied survival analysis: regression modeling of time to event data. Wiley, New York, p 386
Siris ES, Harris ST, Rosen CJ, Barr CE, Arvesen JN, Abbott TA, Silverman S (2006) Adherence to bisphosphonate therapy and fracture rates in osteoporotic women: relationship to vertebral and nonvertebral fractures from 2 US claims databases. Mayo Clin Proc 81:1013–1022
Cramer JA, Amonkar MM, Hebborn A, Altman R (2005) Compliance and persistence with bisphosphonate dosing regimens among women with postmenopausal osteoporosis. Curr Med Res Opin 21:1453–1460
Brankin E, Walker M, Lynch N, Aspray T, Lis Y, Cowell W (2006) The impact of dosing frequency on compliance and persistence with bisphosphonates among postmenopausal women in the UK: evidence from three databases. Curr Med Res Opin 22:1249–1256
Cramer JA, Lynch NO, Gaudin AF, Walker M, Cowell W (2006) The effect of dosing frequency on compliance and persistence with bisphosphonate therapy in postmenopausal women: a comparison of studies in the United States, the United Kingdom, and France. Clin Ther 28:1686–1694
Ideguchi H, Ohno S, Takase K, Ueda A, Ishigatsubo Y (2008) Outcomes after switching from one bisphosphonate to another in 146 patients at a single university hospital. Osteoporos Int 19:1777–1783
Black DM, Thompson DE, Bauer DC, Ensrud K, Musliner T, Hochberg MC, Nevitt MC, Suryawanshi S, Cummings SR (2000) Fracture risk reduction with alendronate in women with osteoporosis: the fracture intervention trial. FIT Research Group. J Clin Endocrinol Metab 85:4118–4124
Cummings SR, Black DM, Thompson DE, Applegate WB, Barrett-Connor E, Musliner TA, Palermo L, Prineas R, Rubin SM, Scott JC, Vogt T, Wallace R, Yates AJ, LaCroix AZ (1998) Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from the Fracture Intervention Trial. Jama 280:2077–2082
Reginster J, Minne HW, Sorensen OH, Hooper M, Roux C, Brandi ML, Lund B, Ethgen D, Pack S, Roumagnac I, Eastell R (2000) Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Vertebral Efficacy with Risedronate Therapy (VERT) Study Group. Osteoporos Int 11:83–91
van Staa TP, Leufkens HG, Abenhaim L, Zhang B, Cooper C (2000) Oral corticosteroids and fracture risk: relationship to daily and cumulative doses. Rheumatology (Oxford) 39:1383–1389
Huybrechts KF, Ishak KJ, Caro JJ (2006) Assessment of compliance with osteoporosis treatment and its consequences in a managed care population. Bone 38:922–928
Caro JJ, Ishak KJ, Huybrechts KF, Raggio G, Naujoks C (2004) The impact of compliance with osteoporosis therapy on fracture rates in actual practice. Osteoporos Int 15:1003–1008
McCloskey E, de Takats D, Orgee J (2005) Characteristics associated with non-persistence during daily therapy. Experience from the placebo wing of a community based clinical trial. J Bone Miner Res 20(suppl 1):S282
Black DM, Schwartz AV, Ensrud KE, Cauley JA, Levis S, Quandt SA, Satterfield S, Wallace RB, Bauer DC, Palermo L, Wehren LE, Lombardi A, Santora AC, Cummings SR (2006) Effects of continuing or stopping alendronate after 5 years of treatment: the fracture intervention trial long-term extension (FLEX): a randomized trial. Jama 296:2927–2938
Strewler GJ (2004) Decimal point–osteoporosis therapy at the 10-year mark. N Engl J Med 350:1172–1174
Bone HG, Hosking D, Devogelaer JP, Tucci JR, Emkey RD, Tonino RP, Rodriguez-Portales JA, Downs RW, Gupta J, Santora AC, Liberman UA (2004) Ten years’ experience with alendronate for osteoporosis in postmenopausal women. N Engl J Med 350:1189–1199
Iizuka T, Matsukawa M (2008) Potential excessive suppression of bone turnover with long-term oral bisphosphonate therapy in postmenopausal osteoporotic patients. Climacteric 11:287–295
Odvina CV, Zerwekh JE, Rao DS, Maalouf N, Gottschalk FA, Pak CY (2005) Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab 90:1294–1301
De Geest S, Sabate E (2003) Adherence to long-term therapies: evidence for action. Eur J Cardiovasc Nurs 2:323
Conflicts of interest
This study was sponsored by Amgen. EL, OS, and FB have previously received funding from several pharmaceutical companies involved in marketing products for treatment of osteoporosis. SR is an employee of Amgen (Europe) GmbH, Zug, Switzerland.
Author information
Authors and Affiliations
Corresponding author
Additional information
Erik Landfeldt and Oskar Ström made equal contributions to this work.
Rights and permissions
About this article
Cite this article
Landfeldt, E., Ström, O., Robbins, S. et al. Adherence to treatment of primary osteoporosis and its association to fractures—the Swedish Adherence Register Analysis (SARA). Osteoporos Int 23, 433–443 (2012). https://doi.org/10.1007/s00198-011-1549-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-011-1549-6