Abstract
Objective
To determine the factors associated with adherence and persistence to bisphosphonate therapy in osteoporosis.
Design
Cross-sectional survey.
Setting
National survey in the UK.
Participants
Participants were recruited through the National Osteoporosis Society and advertisements in the press and on the radio and included 533 women over age 50 with osteoporosis who were currently taking or had taken bisphosphonate therapy within the previous 12 months.
Main outcome measures
Self-reported factors influencing adherence and persistence to bisphosphonate therapy in osteoporosis: fracture history, pain, practical difficulties taking medication (frequency of dosing, dealing with comedications, impact on daily routine), perceptions of therapy, and concerns about bisphosphonate therapy.
Results
Adherence to bisphosphonate therapy was 48% and was associated with previous fracture [odds ratio (OR) 1.62, 95% confidence interval (CI) 1.14–3.02], concerns about medication (OR 1.49, 95% CI 1.01–2.20), and less dissatisfaction with medication (OR 0.65, 95% CI 0.44–0.97). Nonpersistence was associated with dissatisfaction with medication (hazard ratio (HR) 1.83, 95% CI 1.38–2.43), side effects (HR 3.69, 95% CI 2.74–4.97), and concerns about bisphosphonate therapy (HR 2.21, 95% CI 1.48–3.30). For both daily (HR 1.53, 95% CI 1.1–2.33) and weekly bisphosphonates (HR 1.90, 95% CI 1.17–3.07), practical difficulties taking bisphosphonate medication—in particular, too frequent dosing—were associated with nonpersistence.
Conclusions
Self-reported nonadherence to daily and weekly bisphosphonates is independent of the decision to stop taking treatment (nonpersistence). Nonpersistence is associated with side effects and other factors that could be modified in clinical practice through education, information, and concordant partnerships.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bisphosphonates are the main treatment for preventing fractures in osteoporosis, but nonadherence to treatment is common and similar to that in other therapy areas. Nonadherence reduces the effectiveness of treatment and exposes patients to an increased risk of fracture [1] with consequently increased rates of hospitalisation and use of healthcare services, or to multiple changes in therapy because of lack of effectiveness.
Studies in osteoporosis have identified that some patients stop taking bisphosphonates because of side effects [2], because the instructions for taking bisphosphonate medication are too restrictive or difficult to follow, and because osteoporosis is largely asymptomatic; therefore, it is difficult to link treatment to an experience of efficacy [3]. There is some evidence that simplifying the therapeutic dosing regimen may increase adherence to bisphosphonates. Weekly bisphosphonate dosing regimens are preferred to daily regimens [4] and do increase adherence, but adherence is still suboptimal.
What are the possible explanations for this nonadherence? Individual studies in other therapy areas suggest that complex and personal characteristics might have a role. These include the specific beliefs that patients have about their condition and treatment [5], their knowledge and understanding of treatment [6], their expectations of treatment [7], their use of parallel systems of healthcare, and their interpretation of the treatment risks [7]. Few of these characteristics have been evaluated in relation to adherence to bisphosphonate therapy, but they are likely to be relevant. For example, evaluation of treatment risks is influenced by the principle of discounting; risks are more likely to be taken if they correspond to immediate symptomatic benefit than if they prevent some future adverse event such as an osteoporotic fracture.
We aimed to examine all of these factors in relation to medication-taking behaviour in osteoporosis in order to identify those factors associated with adherence and persistence to bisphosphonate therapy and to calculate the risk of nonadherence and nonpersistence for these factors.
Methods
We undertook a telephone interview survey of women with osteoporosis in the United Kingdom. The survey collected retrospective data relating to patients’ decisions to take bisphosphonate medication other than as prescribed (nonadherence) and to stop taking bisphosphonate medication altogether (nonpersistence).
Participants
We recruited women with osteoporosis through advertisements placed with the National Osteoporosis Society and other patient groups, in community magazines with a predominantly middle-aged and older readership, and on radio stations designed to appeal to a middle-aged and older population. Eligible participants were women older than 50 years with a diagnosis of osteoporosis who were currently taking or had taken bisphosphonates within the previous 12 months. Participants were told that the study's purpose was to gain information on their experience of osteoporosis and osteoporosis treatment.
Data collection
The telephone interview was based on three validated questionnaires: PHIT, a modified European Vertebral Osteoporosis Study (EVOS) study questionnaire, and a patient preference rating scale.
PHIT is a validated questionnaire designed to capture patients’ experience of medication [8]. It assesses the impact of the condition on the patient; the patient’s experience of medication, including how he or she takes the medication and any difficulties experienced in taking it; and the patient’s expectations and beliefs about treatment. It also collects information about side effects that patients attribute to their medication.
The modified EVOS questionnaire [9] captures detailed information on risk factors for osteoporosis and was used to gather detailed data on fracture history.
The patient preference rating scale is designed to obtain relative valuations for a health state (osteoporosis) and four different treatment scenarios relating to bisphosphonates (daily, weekly, monthly, monthly with a support programme) on a 0–100 rating scale where 0 is the least desirable and 100 the most desirable. This questionnaire quantifies the satisfaction/dissatisfaction with the current treatment and the relative preference for alternative bisphosphonate therapy. It was used to identify whether dissatisfaction with therapy was associated with nonadherence and nonpersistence.
Definitions of adherence and persistence
We defined adherence as taking bisphosphonate medication as prescribed and nonadherence as taking a dose different from that prescribed (taking more, taking less, or missing doses). For the purposes of this analysis, we considered the medication-taking behaviour for current bisphosphonate users and for lapsed users independent of whether they had stopped medication. Medication-taking behaviour was ascertained by asking subjects a series of questions phrased in different ways during the course of the interview. These questions yielded information about the number of tablets taken within the last month, the ways in which tablets were taken (timing, frequency, special instructions), whether doses were forgotten or not taken, and whether the doses taken were more or less than prescribed. When there were any discrepancies in the responses to questions addressing the same aspect of adherence behaviour, the actual number of doses reported as having been taken was assumed to be the most accurate information.
We defined persistence as the duration of bisphosphonate therapy before ceasing therapy, irrespective of adherence. Persistence was established by asking subjects about all current medication. Those not currently taking a bisphosphonate were asked about the decision to stop therapy, how long ago they had completely stopped bisphosphonate therapy, and how long they had been on therapy. Only subjects who had stopped taking bisphosphonate therapy within the last 12 months were eligible for the study.
Statistical analysis
We used logistic regression analysis to identify factors influencing adherence to bisphosphonates and to calculate the corresponding probability of adherence. We used Cox proportional hazards models to identify factors influencing the duration of therapy before it was stopped (persistence) and to calculate the probability of nonpersistence.
We performed univariate analyses with all variables, examining their relationship to two dependent variables: adherence and persistence. Depending on the data being examined, we used the chi-square test, Student’s t-test, and the Mann–Whitney U-test in the univariate analyses. We generated Kaplan–Meier curves for persistence data. In the multivariate logistic regression, we calculated odds ratios for the risk of nonadherence to bisphosphonate therapy for all of the factors significant in the univariate analyses, controlling for the effects of age and duration of osteoporosis. We added variables by backward likelihood ratio, retaining only variables with p≤0.1 in the model. If variables were highly correlated, we retained the one leading to the best improvement of the model. In the Cox proportional hazards models we calculated hazard ratios for the risk of being nonpersistent to therapy.
We used SPSS version 13.0 to analyse all data.
Results
Between May and July 2005 we recruited and interviewed 533 eligible women. Of these, 334 were currently taking bisphosphonate therapy, and 199 had stopped taking bisphosphonate therapy within the previous 12 months.
The mean age of the sample participants was 70.7 years (SD 8.3, minimum-maximum 51–90). Most (67%, n=533) had been diagnosed with osteoporosis 5 or more years previously (median duration of osteoporosis 78.0 months, range 48–120, minimum-maximum 0.46–384). Forty-two percent (n=533) had sustained an osteoporotic fracture. Forty-five percent (n=533) experienced pain they attributed to their osteoporosis constantly or every day.
Fifty-two percent of women had been diagnosed by their general practitioner and 45% by a hospital specialist. Most women were currently taking (81%, n=334) or had recently taken (53%, n=199) a weekly bisphosphonate.
Some women had mistaken fears of bisphosphonate treatment: 32% (n=533) believed that if they took their bisphosphonate medication regularly, it would be less effective; 40% (n=533) were worried about becoming dependent on bisphosphonates; and 58% were afraid that any side effects from bisphosphonate medication would be worse than symptoms from their osteoporosis. Women had conservative expectations of the efficacy of bisphosphonate therapy: 14% expected that treatment would restore their bones to “normal,” and 44% expected that therapy would prevent future fractures. Women who had sustained a previous osteoporotic fracture were more pessimistic in their expectations than those who had not (chi square 12.13, p=0.02): 49% of them felt that bisphosphonate therapy was unlikely to prevent future fractures.
Adherence to bisphosphonate therapy
Nonadherence to bisphosphonate therapy was 52% (n=533) and was independent of persistence (chi square 1.65, p=0.20). Fifty-four percent (n=334) of women currently taking bisphosphonates and 49% (n=199) of women who had stopped taking bisphosphonates (nonpersisters) were nonadherent. Nonadherence ranged from occasionally forgetting to take doses (20%, n=533), occasionally making an active decision to not take a dose (13%, n=533), occasionally making an active decision to take more than the prescribed dose (2%, n=533), and regularly deciding not to take medication (26%, n=533). Nonadherence was similar for daily (51%) and weekly (53%) bisphosphonates overall and across all the subcategories of nonadherence.
In the univariate analysis (Table 1), adherence was associated with previous osteoporotic fracture, longer duration of osteoporosis, and dissatisfaction with bisphosphonate therapy. Concerns about bisphosphonate medication such as fears of addiction or dependence, concern about taking medication over a long period of time, and a perception that side effects could be worse than the symptoms or outcome of osteoporosis were also associated with adherence, but this reached only borderline statistical significance (p=0.055). In the multivariate logistic regression, controlling for the effects of age, duration of osteoporosis, duration of therapy, and the type of bisphosphonate taken, adherence was significantly associated with previous fracture, less dissatisfaction with bisphosphonate therapy, and concerns about bisphosphonate medication (Table 2).
Persistence on bisphosphonate therapy
Factors associated with persistence were different from those associated with adherence. In the univariate analyses, persistence was associated with weekly rather than daily bisphosphonates, a shorter duration of disease, and frequent pain (Table 3). Nonpersistence was associated with side effects (an event defined by the subject as a side effect and attributed by the subject to the bisphosphonate therapy), practical difficulties in taking bisphosphonate medication (too frequent dosing, having to take too many tablets, difficulty fitting it into a daily routine, difficulty following the special instructions for taking bisphosphonates), dissatisfaction with bisphosphonate therapy, and concerns about bisphosphonate medication (Table 3).
In the multivariate Cox proportional hazards model, controlling for age, duration of disease, and side effects, nonpersistence was significantly associated with concerns about medication and dissatisfaction with bisphosphonate therapy (Table 4). Dissatisfaction with bisphosphonate therapy and practical difficulties taking medication affected patients on daily and those on weekly bisphosphonates. Women taking daily bisphosphonates who had experienced practical difficulties taking their medication were 1.53 times more likely to have stopped taking their medication than those who had not had difficulties (HR 1.53, 95% CI 1.10–2.33). For women taking weekly bisphosphonates, the specific difficulty most associated with nonpersistence was frequency of dosing. Patients taking weekly bisphosphonates who felt that taking medication once a week was too frequent were 1.90 times more likely to have stopped taking their medication than those who did not find once-weekly medication too frequent (HR 1.90, 96% CI 1.17–3.07).
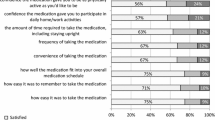
Dissatisfaction with therapy
A small number of patients (9%, n=533), rated all treatment scenarios lower (worse) than untreated osteoporosis. These patients were more likely to be nonadherent to treatment or to have stopped taking their bisphosphonate. Twenty-six percent of patients (n=533) rated their current or most recent treatment lower than untreated osteoporosis. This dissatisfaction with treatment was associated with nonadherence (chi square 3.91, p=0.05) and nonpersistence (chi square 42.88, p<0.0001). The main reasons for dissatisfaction with treatment were experience of side effects (47% of dissatisfied patients, n=141, chi square 4.10, p=0.043) and practical difficulties taking the medication, including too frequent dosing, having to take too many tablets, difficulty fitting it into a daily routine, and difficulty following the special instructions for taking bisphosphonates (52%, n=141, chi square 7.85, p=0.005).
Discussion
Around half of the women in this study who were taking daily or weekly bisphosphonates were not taking their medication as prescribed. No clear factor influencing nonadherence was identified, but patients who had sustained a previous osteoporotic fracture were more likely to adhere to treatment. Although the most frequently reported reason for stopping bisphosphonate therapy was side effects, other factors were also associated with nonpersistence. Dissatisfaction with bisphosphonate therapy (primarily related to practical difficulties taking bisphosphonate medication, particularly the perception that dosing was too frequent) increased the risk of nonpersistence, as did concerns about the possibility of becoming addicted to bisphosphonates and about taking medication over a long period of time.
Strengths and weaknesses of the study
This study collected detailed information about medication-taking behaviour and the reasons behind that behaviour direct from a community-based sample of patients across England, Wales, and Scotland. Although the sample was predominantly recruited via a patient organisation, several different methods of recruitment were additionally used (press and radio advertisements) to minimise the bias of using a well-motivated, well-informed patient population. Nevertheless, because recruitment relied on subjects volunteering themselves, it is possible that the participants were more motivated in relation to their bisphosphonate medication. This could potentially result in overestimates of adherence and persistence.
The study was cross-sectional and observational and can identify associations between factors influencing adherence and persistence but cannot determine causality. The data collected were largely retrospective, which introduces the possibility of bias due to recall or rationalisation of patient experiences. For example, patients who stopped therapy may feel a need to justify this behaviour in terms of the experience of side effects or practical difficulties taking medication, such as too frequent dosing and the need to follow special instructions. Alternatively, anxious patients may report retrospective nonadherence more frequently than it occurred. These factors need further examination in prospective studies.
Definitions of adherence in this study were broad because it was thought important to capture the spectrum of medication-taking behaviour that varies from occasional nonadherence, to consistent reductions or increases in dose, to stopping medication completely (nonpersistence). Different factors may determine different levels of nonadherence, but being able to accurately differentiate between different levels and motivators for adherence is difficult in any situation. The use of retrospective and self-reported data on adherence potentially introduces bias as discussed above, but even in prospective studies, obtaining accurate, meaningful data about medication-taking behaviour is difficult. For example, counting tablets gives no information about the motivation behind missed doses—whether they were forgotten or the result of a deliberate decision. This may explain why this study did not identify any factor clearly associated with nonadherence. It is easier to accurately classify patients as those who are still taking medication (whatever the degree of adherence) and those who had completely stopped taking medication. This study found factors associated with nonpersistence, many of which could be addressed in patient education and information. Any intervention aimed at addressing these would likely benefit patients at all levels of adherence.
The measures of adherence and persistence are self-reported and may therefore be overestimates; however, there are few alternatives, particularly in a community-based study, and no measures can guarantee complete accuracy. Medication possession ratio, for example, still provides no information about how, when, and if patients take their medication, simply that they picked up their prescriptions from the pharmacy. Studies have shown that self-reports of nonadherence are accurate but that reports of adherence are often overestimated [10]. However, inaccuracies in reported adherence can be minimised by using independent researchers to interview patients and by asking simple, direct questions [11].
This study was undertaken in the UK, where issues of treatment cost to individual patients are less relevant than in other settings. For this reason, information on cost was not collected in this study, but it is possible that in settings where the cost of medication and the availability and coverage of insurance are real issues for patients, these factors may be associated with patients’ decisions about whether and how to take medication.
Comparison with the literature
Self-reported adherence to bisphosphonate therapy is generally considered to be higher than other measures of adherence and has been reported to be 90% [12]. Self-reported adherence in this study was much lower, even amongst a population of well-motivated and informed patients who were members of a patient organisation. This may be related to the study design. Other studies of adherence are generally clinical trials with follow-up in which adherence and self-reported adherence would be expected to be higher. Adherence data based on prescription information have suggested that adherence to bisphosphonate therapy is much lower in clinical practice [13].
Previous studies of adherence to bisphosphonate therapy have identified associations between adherence and knowledge of osteoporosis [7], satisfaction with medication [7], and beliefs about the safety and necessity of treatment [14]. We demonstrated an association between adherence and satisfaction—patients dissatisfied with their medication were more likely to be nonadherent. We also found that patients who were concerned about bisphosphonate medication were 50% more likely to adhere to medication than those with no concerns. This seems counterintuitive but may reflect a specific type of patient who is anxious about medication but also anxious enough about his or her condition to adhere to treatment despite concerns about it.
Most of the literature on adherence and persistence with bisphosphonate therapy has focussed on the impact of dosing frequency. The introduction of formulations that can be taken at weekly rather than daily intervals has made this an important clinical question. The overwhelming evidence from crossover trials [15, 16], prospective observational studies [6], and interrogation of prescription claims data [17, 18] is that adherence and persistence are higher with weekly than with daily bisphosphonates. We found that persistence was higher in women taking weekly compared with daily bisphosphonates. We also found that a perception that dosing was too frequent was significantly associated with nonpersistence for patients taking weekly bisphosphonates. These patients were almost twice as likely to have stopped taking their bisphosphonate as women who did not perceive weekly dosing to be too frequent.
Clinical implications
Improving adherence and persistence with bisphosphonate medication is an important clinical goal because of the potential link between adherence and outcome. We have identified factors associated with nonpersistence with bisphosphonate therapy that could be modified in clinical practice. Patients’ concerns about becoming addicted to bisphosphonates or about having to take them over long periods of time could be addressed in patient literature, in medical consultations, and in community pharmacies when patients collect their prescriptions. Pharmacists could also address the problem of managing bisphosphonates alongside comedication by providing individual treatment plans documenting how and when to take each medication on a daily or weekly basis. Although the special requirements for taking bisphosphonates (timing of the dose, fasting, and so on) cannot be modified, frequency of dosing could be addressed by offering patients the choice of how often they would prefer to take their medication. This choice will increase with the introduction of bisphosphonates that can be taken monthly rather than daily or weekly.
Conclusions
Patients’ decisions to stop taking bisphosphonate medication are based on more than simply the experience of side effects. Concerns about medication, dissatisfaction with treatment, and practical difficulties taking the medication, including too frequent dosing and management of comedications, are associated with nonpersistence in taking daily and weekly bisphosphonates. Addressing these issues in clinical practice may improve adherence and persistence and result in better disease outcomes for patients.
References
Caro JJ, Ishak KJ, Huybrechts KF, Raggio G, Naujoks C (2004) The impact of compliance with osteoporosis therapy on fracture rates in actual practice. Osteoporosis Int 15:1003–1008
Tosteson AN, Grove MR, Hammond CS et al (2003) Early discontinuation of treatment for osteoporosis. Am J Med 115:209–216
Miller NH (1997) Compliance with treatment regimens in chronic asymptomatic diseases. Am J Med 102:43–49
Simon JA, Lewiecki EM, Smith ME et al (2002) Patient preference for once-weekly aledronate 70 mg versus once daily aledronate 10 mg: a multicenter, randomised, open label, cross-over study. Clin Ther 24:1871–1886
Donovan JL, Blake DR (1992) Patient noncompliance: deviance or reasoned decision-making? Soc Sci Med 34:507–513
Donovan JL, Blake DR, Fleming WG (1989) The patient is not a blank sheet: lay beliefs and their relevance to patient education. Br J Rheumatol 28:58–61
Horne R (1999) Patients’ beliefs about treatment: the hidden determinant of treatment outcome? J Psychosom Res 47:491–495
Carr AJ, Hughes RA, Vincent K, Carr M, Thwaites C (2004) The impact and implications of new treatments in arthritis: validation of a questionnaire to measure the ‘real life’ effectiveness of medication. Rheumatology 43(suppl):ii83
O’Neill TW, Cooper C, Cannata JB, Diaz Lopez, Hoszowski K et al (1994) Reproducibility of a questionnaire on risk factors for osteoporosis in a multicentre prevalence survey: The European Vertebral Osteoporosis Study. Int J Epidemiology 23(3):559–565
Fletcher RH (1989) Patient compliance with therapeutic advice: a modern view. The Mount Sinai Journal of Medicine 56:453–458
Kaplan RM, Simon HJ (1990) Compliance in medical care: reconsideration of self-predictions. Annals of Behavioural Medicine 12:66–71
Turbí C, Herrero-Beaumont G, Acebes JC, Torrijos A, Graña J, Miguélez R, Sacristán JA, Marín F (2004) Compliance and satisfaction with raloxifene versus alendronate for the treatment of postmenopausal osteoporosis in clinical practice: an open-label, prospective, nonrandomized, observational study. Clin Ther 26:245–256
Cramer J, Amonkar M, Hebborn A, Suppapanya N (2004) Does dosing regimen impact persistence with bisphosphonate therapy among postmenopausal osteoporotic women? J Bone Miner Res 19(Suppl 1):S448 (Abstract M434)
Unson CG, Siccion E, Gaztambide J, Gaztambide S, Mahoney Trella P, Prestwood K (2003) Nonadherence and osteoporosis treatment preferences of older women: a qualitative study. J Women’s Health 12:1037–1045
Kendler D, Kung AWC, El-Hajj Fuleihan G, González JGG, Gaines KA, Verbruggen N, Melton ME (2004) Patients with osteoporosis prefer once weekly to once daily dosing with alendronate. Maturitas 48; 243–251
Simon JA, Lewiecki EM, Smith ME, Petruschke RA, Wang L, Palmisano JJ (2002) Patient preference for once-weekly alendronate 70 mg versus once-daily alendronate 10 mg: a multicenter, randomized, open-label, crossover study. Clin Ther 24:1871–1886
Boccuzzi SJ, Folz SH, Omar MA, Kahler KH (2005) Assessment of adherence and persistence with daily and weekly dosing regimens of oral bisphosphonates. Osteoporosis Int 16(Suppl 4):S35–S36 (Abstract P7.10)
Ettinger MP, Gallagher R, Amonkar M, Smith JC, MacCosbe PE (2004) Medication persistence is improved with less frequent dosing of bisphosphonates, but remains inadequate. Arthritis Rheum 15(Suppl.):S513 (Abstract 1325)
Funding
This study was funded by Roche Products and GlaxoSmithKline. The funders had no role in the day-to-day running of the study, the data analysis or interpretation, the drafting of the paper, or the decision to publish. The study was run by an independent clinical research company, Clinimatrix, in association with C.C. and P.W.T. Data were collected and analysed by Clinimatrix and reviewed and interpreted by C.C. and P.W.T. The authors were responsible for determining the content of the paper, writing the paper, and deciding when and where to publish. The funders had no role in these processes.
Declaration of competing interests
P.T. and C.C. have received consulting fees from Roche Products, Merck Sharp & Dohme, and Procter & Gamble, all manufacturers of competing bisphosphonates. A.C. has shares in Clinimatrix, the independent clinical research company that obtained funding for this study from Roche Products and GlaxoSmithKline.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carr, A.J., Thompson, P.W. & Cooper, C. Factors associated with adherence and persistence to bisphosphonate therapy in osteoporosis: a cross-sectional survey. Osteoporos Int 17, 1638–1644 (2006). https://doi.org/10.1007/s00198-006-0166-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-006-0166-2