Abstract
Summary
This study assesses the costs of non-vertebral osteoporosis-related fractures patients compared with osteoporosis patients without fractures, focusing on the second year following a fracture. Since fracture patients remained more costly in the second year, their economic burden extends beyond the year in which the fracture occurs.
Introduction
The purpose of this study is to examine the comorbidity profile, resource use, and direct costs of patients who incur osteoporosis-related non-vertebral (NV) fractures in the United States during the 2 years following an incident fracture, focusing on the second year following a fracture.
Methods
Osteoporosis patients (ICD-9-CM: 733.0) with a NV fracture (hip, femur, pelvis, lower leg, upper arm, forearm, rib, and multiple sites) were selected from a privately insured health insurance claims database (>8 million lives, ages 18–64, 1999–2006). These NV fracture patients were randomly matched 1:1 on age, gender, employment status, and geographic region to controls with osteoporosis but without a fracture history. Year-by-year and month-by-month rates of comorbidities, resource use, and direct costs were calculated for the matched sample (N = 3,781).
Results
Comorbidity rates and resource use remained significantly higher among NV fracture patients during second year following an NV fracture compared with controls, although absolute rates of comorbidities and service utilization declined. Mean direct excess costs for NV fracture patients fell from $5,267 in the first year to $2,072 in the second year after a fracture, but remained statistically significant (p < 0.01). Patients with fractures of the pelvis, hip, and femur had the highest excess costs in the second year ($5,121, $3,930, and $3,828, respectively). Although hip fractures had highest excess costs over both years, non-vertebral, non-hip fracture patients made up a larger proportion of the sample and were significantly more costly than controls.
Conclusions
Patients with osteoporosis-related NV fractures have substantial excess costs beyond the first year in which the fracture occurs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is the most common bone disease in the United States: approximately 10 million people have been diagnosed, and another 34 million have osteopenia, which puts them at risk for developing the disease [1–3]. The World Health Organization defines osteoporosis as a bone mineral density score that is at least 2.5 standard deviations below the average score for a healthy young adult [4]. Osteoporosis causes bones to become fragile, which often leads to skeletal fractures [3]. In the U.S., more than 1.5 million fractures are attributed to osteoporosis each year [2]. Worldwide, there were an estimated nine million new fractures related to osteoporosis in 2000 [5]. While osteoporosis is commonly thought of as a female disease, 20% of those affected are male, and men over 50 have a 30% estimated lifetime risk of osteoporosis-related fractures [3, 5]. Non-vertebral (NV) fractures comprise 85% of all osteoporosis-related fractures and account for 94% of their total costs [1–4]. In 2005, costs associated with osteoporosis-related fractures in the U.S. were estimated at $19 billion, and they are projected to reach $25.3 billion in 2025 [6]. Most literature on NV fractures focuses on hip fractures, which are the most common type of fracture associated with osteoporosis and are generally understood to be the most expensive as well [1, 4]. Estimates of health care costs per hip fracture patient range from $13,240 to $35,600 annually [7–12]. By comparison, health care cost estimates for patients in the US with non-vertebral, non-hip (NVNH) fractures (e.g., femur, pelvis, forearm) are estimated between $3,000 to $29,600 in the year following a fracture, depending on the site of the fracture [2, 8–14]. In Europe, these NVNH fracture cost estimates range from €565 (approximately $560 in 2006 USD) to €3,651 (approximately $3,650 in 2006 USD) [11].
The literature on health outcomes and costs associated with NV fractures in osteoporosis patients is limited, particularly regarding NVNH fractures. Several studies rely on data collected prior to 2003, and therefore may no longer reflect current medical practice and associated costs. Recently, however, Pike et al. [9] estimated that patients in the U.S. with osteoporosis-related NV fractures have substantial excess costs ($5,961 for ages 18–64, $13,387 for ages 65+) in the year following a fracture over osteoporosis patients with no fractures. Pike et al. also noted that excess costs were significant for patients with NVNH fractures as well as hip fractures and that NVNH fracture patients may actually cost payers more than hip fracture patients in the aggregate.
Few studies have examined the implications of NV fractures beyond the first year. Excess costs may remain substantially higher for a longer duration than 1 year for a variety of reasons, including complications or comorbidities related to the fracture or to subsequent fractures. Studies estimate that more than one quarter of osteoporosis-related fracture patients will suffer from subsequent fractures [15]. This study is an extension of the examination of the 1-year outcomes and costs of NV fracture patients by Pike et al. Here, the authors estimate the rates of comorbidities, resource utilization, and direct costs associated with osteoporosis patients with NV fractures starting 6 months prior to the fracture through the 24 months following a fracture among a privately insured population (ages 18–64) with a focus on examining the changes from the first year to the second year.
Methods
Data
This study uses data from a privately insured administrative claims database covering over eight million privately insured beneficiaries from 1999 through 2006. In addition to monthly enrollment history, the data contain medical and prescription drug claims for all beneficiaries. Medical claims include dates and place of service, provider type and specialty, primary and secondary diagnoses based on the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM), procedures performed based on the American Medical Association’s Current Procedural Terminology and the Healthcare Common Procedure Coding System, and actual dollar amounts paid to providers. Prescription drug claims include National Drug Code (NDC), fill date, days of supply, quantity, strength, and amount paid.
Sample selection
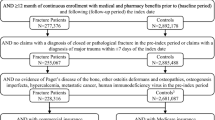
Following the methodology of Pike et al. [9], all patients with an osteoporosis-related NV fracture were identified. Figure 1 illustrates the sample selection process. NV fractures were considered osteoporosis-related if they occurred during the 6 months prior to a patient’s first osteoporosis claim or anytime thereafter. For the purposes of the study, the first such fracture was considered the index fracture. Patients with any NV fracture claim during the six months preceding the index fracture were removed to increase the likelihood that the claim was for an incident fracture rather than for follow-up associated with a previous fracture.
Next, exclusion criteria were applied in an effort to increase the likelihood that the fractures studied were related to osteoporosis. First, any patient with a medical claim with an E-code for severe trauma within 30 days of the index fracture was excluded from the sample, as these fractures may not have been related to osteoporosis [7, 16, 17]. In addition, patients with other conditions found to elevate fracture risk were excluded including those with diagnoses of metastatic cancer, bone cancer, multiple myeloma, and Paget’s disease of bone, those who underwent surgical castration, and those using specific cancer drugs [18–20]. In an effort to further focus specifically on NV fracture patients, those with fractures of the vertebrae, trunk, face, skull, finger, toe, and unspecified sites were also excluded.
The remaining NV fractures patients were then matched one-to-one to osteoporosis controls with no claims for any fracture (NV or otherwise) in their claims history. Patients next were matched to controls one-to-one based on age (±3 years), gender, geographic region, and employment status. Matched controls were assigned the same index date as their NV fracture counterpart, and all fracture patients and controls in the final sample were required to have 12 months of continuous enrollment before their index date and 24 months following (see Pike et al. for further details on the selection criteria).
Analysis
Comorbidities, resource utilization, and direct costs were assessed descriptively over the 24-month period following the index date. Charlson Comorbidity Index (CCI) scores [21, 22] and the prevalence rates of osteoporosis-related and CCI-specific comorbidities were calculated for patients and controls [7]. Medical resource utilization was determined by grouping claims based on place of service (e.g., inpatient, outpatient, emergency department, long-term care) and type of service (e.g., radiology, rehabilitation). The proportion of NV fracture patients and controls that had one or more visits, the mean number of visits per patient, and the mean length of stay for inpatient and long-term care were reported. For prescription drug use, NDCs were used to identify the proportion of patients who were prescribed drugs, with results reported for subcategories of osteoporosis-related (e.g., selective estrogen receptor modulators, bisphosphonates) and fracture-related (e.g., opioids, NSAIDs, prescription-strength acetaminophen) drugs. Direct costs were assessed descriptively over the 24-month study period using actual payments to health care providers from third-party payers. All costs are reported in 2006 dollars (inflated as necessary using the Consumer Price Index for Medical Care). All results are reported year-by-year (i.e., for the first 12 months following the index fracture and then for the subsequent 12 months) and stratified by fracture type: femur, forearm (e.g., hand, radius, ulna, and wrist), hip, lower leg (e.g., ankle, fibula, foot, patella, and tibia), multiple sites, pelvis, ribs, and upper arm (e.g., clavicle, humerus, and scapula).
For purposes of statistical analysis, McNemar tests were used for pair-wise comparisons of proportions (e.g., comorbidity and resource utilization rates), and Wilcoxon Signed-Rank tests were used for pair-wise comparisons of age, CCI, costs, and other counts (e.g., number of visits). P values less than 0.05 were considered statistically significant. All analyses were conducted using SAS 9.2 (SAS Institute, Cary, NC).
Results
Sample characteristics
Table 1 reports the demographic characteristics of the study sample. Fracture patients in the study sample (N = 3,536) were categorized into one of eight groups based on the site of their index fracture. The largest proportion of NV fracture patients (42.1%) fell into the lower leg group. The least common index fracture types were pelvis (1.6%), femur (2.2%), and hip (5.6%). At the time of the index fracture, the mean age of NV fracture patients and matched controls was 56.0 and 56.2 years, respectively, and age was similar across fracture types. The overwhelming majority of fracture patients and controls were female (94.0% in both groups). There was minor variation in the gender distribution of fracture types, with the femur fracture group having a slightly lower proportion of females (88.6%) while the lower leg and forearm groups had a slightly higher proportion of females (95.8% and 95.0%, respectively, no statistical testing was performed).
Comorbidity profile
A smaller proportion of NV fracture patients received a diagnosis for various comorbidities during the second year following the index fracture, but this proportion remained significantly higher than that of controls (see Table 2). The comorbidities for which the largest proportion of patients received a diagnosis during year two remained the same as year one: arthralgia (23.2% vs. 15.4%, p < 0.01), osteoarthritis (15.1% vs. 10.4%, p < 0.01), and malaise/fatigue (13.6% vs. 10.8%, p < 0.01). The overall severity of illness (as measured by the CCI) was significantly greater in year two, although it was slightly lower in absolute terms. In year two, mean CCI score was 0.67 for NV fracture patients compared with 0.48 for controls (p < 0.01). There was variation in year two CCI score by fracture type. The largest differences were for patients with fractures of the femur (1.26 vs. 0.54, p = 0.01), hip (0.97 vs. 0.63, p = 0.01), and ribs (0.81 vs. 0.49, p < 0.01).
Resource use
Health care resource use for NV fracture patients followed a similar pattern during year two: although it was lower in absolute measures, it remained significantly higher in comparison with controls across all categories (see Table 3). The percentage of emergency department visits (29.4% vs. 20.6%, p < 0.01) and hospital inpatient visits (12.8% vs. 8.3%, p < 0.01) remained significantly higher for NV fracture patients during year two, but difference between patients and controls in year two was lower than in year one. Although the average number of outpatient visits per NV fracture patient was lower in year two than in year one (21.6 vs. 15.8), fracture patients still averaged three more outpatient visits than controls in year two (15.8 visits per patient vs. 12.7 visits per control, p < 0.01). Length of stay measures did not exhibit the same degree of change from year one to year two. Among those with at least one hospital inpatient visit, the average length of stay remained constant (7.6 days in year one vs. 7.3 days in year two) and remained significantly higher than the 5.6 days per control in year two. The average length of long-term care days increased from 15.2 days in year one to 17.1 days in year two, but the average excess number of days over controls was 1.4 days lower in year two (17.1 days per patient vs. 7.4 days per control, p < 0.01).
Prescription drug use in year two also stayed significantly higher for NV fracture patients than for controls. A higher percentage of fracture patients filled fracture-related drug prescriptions during year two than controls (54.2% vs. 43.2%, p < 0.01), although the difference between patients and controls was higher in year one (68.0% vs. 44.7%, p < 0.01). Osteoporosis-related drug use was virtually unchanged.
Excess resource use varied widely by fracture type in year two (see Table 4 in Electronic Supplementary Material). Of the NV fracture patients, hip and femur fracture patients had the highest percentage of inpatient hospital stays (23.1% hip patients vs. 8.5% controls, p < 0.01; 20.3% femur patients vs. 6.3% controls, p = 0.01). The percentage of patients visiting the emergency room was highest for patients with fractures of the ribs (37.0% patients vs. 20.2% controls, p < 0.01), hip (36.2% patients vs. 20.6% controls, p < 0.01), and upper arm (34.5% patients vs. 19.9% controls, p < 0.01). Hip fracture patients accounted for more of the long-term care use in the sample as well (hip 2.5% patients vs. 0.5% controls, p = 0.10; NVNH 0.6% patients vs. 0.4% controls, p = 0.21). Lastly, a higher proportion of patients with pelvis, hip, and femur fractures used fracture-related drugs than controls (pelvis 68.4% vs. 42.1%, p = 0.01; hip 59.3% vs. 40.2%, p < 0.01; femur 57.0% vs. 40.5%, p = 0.04).
Direct costs
Compared with controls, direct costs for NV fracture patients were significantly higher in year two, although they were substantially lower in the second year (year one $10,819 vs. $5,552, p < 0.01; year two $7,363 vs. $5,292, p < 0.01). Excess costs were 60.7% lower in the second year ($5,267 vs. $2,072), but remained statistically significant. In total, fracture patients had excess direct costs of $7,339 over the 2-year study period. Excess medical costs dropped from $4,614 in year one ($8,423 vs. $3,810, p < 0.01) to $1,421 in year two ($4,957 vs. $3,536, p < 0.01), while excess prescription drug costs remained constant at $653 in year one ($2,396 vs. $1,743, p < 0.01) and $651 in year two ($2,407 vs. $1,756, p < 0.01).
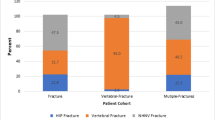
Although there was substantial variation in excess direct costs by fracture type, these differences all remained significantly greater for NV fracture patients than controls in year two (see Fig. 2). In year one, excess costs were largest for patients with hip ($13,334), multiple site ($7,830), and pelvis ($7,083) fractures. In year two, pelvis fracture patients had the greatest excess costs ($5,121) followed by hip ($3,930) and femur ($3,828) fracture patients. Excess costs for femur fracture patients were similar in both years ($4,211 vs. $3,828). Also of note, pelvis fracture patients incurred far greater excess prescription drug costs (31.6% of costs in year one and 50.4% in year two) compared with NV fracture patients as a whole (12.4% in year one and 31.4% in year two).
Figure 3 depicts the excess costs for all NV fracture patients on a month-by-month basis beginning 6 months before the index date and extending through the end of the 2-year study period. Excess costs ranged from $120 to $179 per month before the fracture until the month directly preceding the index fracture, during which costs doubled to $363. NV fracture patients incurred 31.5% of their total 2-year excess costs during the month in which their index fracture occurred. In month two, costs declined substantially and then remained stable for the next several months, ranging from $239 to $373 in month two through month seven. From month eight onward, excess costs continued to remain relatively stable before declining slowly to pre-fracture levels around month 18 following the index fracture. This pattern held for all fracture types.
Discussion
By examining the 2-year patient profile and cost burden of privately insured NV fracture patients in the US, this study offers a novel contribution to the literature and a longer-term perspective on patients with NV fractures. The key finding here is that the burden of NV fracture patients extends beyond the year in which the fracture occurs. On average, NV fracture patients in this study did not return to their pre-fracture cost levels until approximately 18 months following a fracture (as illustrated by Fig. 3) and even then they still had significant excess costs over matched osteoporosis patients with no fracture history. Consequently, studies that focus only on the 1-year costs of patients with NV fractures may miss a substantial portion of their costs and understate their true economic burden. Economic models regarding impacts of new therapies for NV fractures would benefit from considering these results.
The excess resource use burden of NV fracture patients also extends into the second year. Patients with NV fractures had significantly more average hospital inpatient days, long-term care days, and outpatient and emergency room visits. Patients who are hospitalized, in long-term care arrangements, or attend medical appointments related to a fracture will miss work or leisure activities. This suggests that the patient burden resulting from NV fracture also extends into the second year.
While the average cost and utilization trends were decreasing in the second year, it is likely that for some patients, such as those with subsequent fractures, costs and utilization continued to increase. Other studies have shown that an osteoporosis-related fracture is a strong predictor for subsequent fractures [15, 23] and thus, for the patients in this study with subsequent fractures, costs could be significantly higher and continue to increase in the second year. Further research on the prevalence of subsequent fractures and the costs of patients with subsequent fractures would provide useful information regarding the potential benefits of early intervention aimed at preventing first, and therefore subsequent, fractures.
It is also noteworthy that patients with NV fractures incurred increased costs before their index fracture. In the month before a fracture, they averaged approximately the same excess costs as they did from the second month following a fracture and beyond. These prior month excess costs represented a twofold increase from the previous month. Presently, most algorithms that assess the probability of an osteoporosis-related fracture (e.g., the World Health Organization’s FRAX risk assessment tool [24]) typically use demographic characteristics, extended medical history, and other longer-term measures that do not vary from month to month. By better identifying more short-term risk factors, clinicians may be able to intervene more effectively before fractures occur. Further retrospective research should look closely at patients during the months prior to an NV fracture.
These findings add to the limited knowledge base regarding the costs and outcomes associated with NVNH fractures. This study confirms that hip fracture patients have substantial excess costs during the first two years following a fracture, and suggests that patients with fractures of the femur or pelvis have comparable excess costs, which is consistent with the literature pertaining to one year costs [8–13]. Moreover, while patients with fractures of the lower leg, forearm, and other NVNH sites have lower costs on a per person basis, they made up a much larger proportion of this study’s sample. In the aggregate, NVNH patients in this sample cost private payers $15.3 billion in year one and $6.4 billion in year two. Hip fracture patients, by comparison, cost payers $2.7 billion in year one and $0.8 billion in year two. Over the entire 2-year period, NVNH patients represented over six times the total costs to payers as hip fracture patients ($21.7 billion vs. $3.4 billion). To the extent that these sample sizes are representative of the relative prevalence of NVNH and hip fracture patients in privately insured populations, NVNH fracture patients may represent an important and often overlooked fracture subpopulation.
This study has several limitations. First, claims data do not contain clinical detail such as bone mineral density T scores, which could be used to verify whether fractures were osteoporosis-related. This issue is particularly relevant for osteoporosis, which is often under diagnosed [25–27]. As a consequence, an unknown number of patients with osteoporosis-related fractures may have been excluded from this study. This sample is only 6% male, whereas an estimated 20% of osteoporosis patients are male [3], suggesting that men may be under diagnosed in medical claims data. Some evidence suggests that the underdiagnosis of osteoporosis is more likely among patients with multiple comorbid conditions [28, 29], and, to the extent that such patients were disproportionately excluded from this study’s sample, the costs reported here may be understated.
Second, this study focused only on fracture patients with clinically diagnosed osteoporosis in a privately insured U.S. population. The two-year burden of illness for NV fracture patients for other populations and in other regions such as Canada and Europe may differ. For example, given that older patients tend to have longer recovery periods and more complications following a fracture, those in elderly populations (e.g., Medicare) likely exhibit an even greater burden during the second year and beyond. In addition, less is known about the broader population of patients who suffer from NV fractures. As noted earlier, there are an additional 34 million Americans who are at risk for NV fractures due to osteopenia. According to the National Osteoporosis Risk Assessment study, the osteopenic population has a higher incidence of fractures than the osteoporosis population [8]. Research examining patients with osteopenia and other risk factors for fractures may produce a more broadly accurate assessment of the overall cost burden of NV fractures.
Finally, this study focused only on direct healthcare costs and did not include attention to indirect costs such as disability payments and missed days of work, which may also be substantial. In related research, Pike et al. found that patients who had osteoporosis-related fractures were almost three times more likely than osteoporosis patients without fractures to receive disability benefits during the year following their fracture, and had work loss costs that were nearly twice as high ($4,349 vs. $2,393) [9]. Other studies of osteoporosis patients that did not explicitly look at fractures also found substantial indirect costs resulting from work loss and caregiver burdens [30, 31]. These findings suggest that the results in this paper may underestimate the full cost of fractures.
In summary, the economic burden for patients with all types of NV fractures remained significantly higher during the second year following an NV fracture than for controls with osteoporosis and no fracture history. This finding applies to NVNH fracture patients as well as hip fracture patients. This study suggests that although hip fracture patients are more costly per patient, NVNH fracture patients may account for a larger overall cost burden, at least for private payers. NVNH fractures account for 80–90% of all osteoporosis-related fractures globally, so the unmet need in terms of pharmacological treatment to reduce fracture risk is important [32]. More effective treatment to prevent fractures may reduce their associated costs.
References
Boonen S, Singer AJ (2008) Osteoporosis management: impact of fracture type on cost and quality of life in patients at risk for fracture I. Curr Med Res Opin 24(6):1781–1788
Orsini LS, Rousculp MD, Long SR, Wang S (2005) Health care utilization and expenditures in the United States: a study of osteoporosis-related fractures. Osteoporos Int 16(4):359–371
National Osteoporosis Foundation. Osteoporosis Fast Facts. http://www.nof.org/osteoporosis/diseasefacts.htm. Accessed 20 Aug 2009
World Health Organization (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. WHO Technical Report Series, No. 843. Geneva
International Osteoporosis Foundation. Facts and statistics about osteoporosis and its impact. http://www.iofbonehealth.org/facts-and-statistics.html. Accessed 08 Oct 2009
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 22:465–475
Ohlsfeldt RL, Borisov NN, Steer RL (2006) Fragility fracture-related direct medical costs in the first year following a nonvertebral fracture in a managed care setting. Osteoporos Int 17:252–258
Ray NF, Chan JK, Thamer M, Melton LJ 3rd (1997) Medical expenditures for the treatment of osteoporotic fractures in the United States in 1995: report from the National Osteoporosis Foundation. J Bone Miner Res 12(1):24–35
Pike C, Birnbaum H, Schiller M, Sharma H, Burge RT, Edgell ET (2010) Direct and indirect costs of non-vertebral fracture patients with osteoporosis in the U.S. Pharmacoeconomics 28:395–409
Levy P, Levy E, Audran M, Cohen-Solal M, Fardellone P, Le Parc JM (2002) The cost of osteoporosis in men: the French situation. Bone 30(4):631–636
Bouee S, Lafuma A, Fagnani F, Meunier PJ, Reginster JY (2006) Estimation of direct unit costs associated with non-vertebral osteoporotic fractures in five European countries. Rheumatol Int 26(12):1063–1072
Chen Z, Maricic M, Aragaki AK, Mouton C, Arendell L, Lopez AM, Bassford T, Chlebowsk RT (2009) Fracture risk increases after diagnosis of breast or other cancers in postmenopausal women: results from the Women’s Health Initiative. Osteoporos Int 20(4):527–536
Melton LJ, Gabriel SE, Crowson CS, Tosteson AN, Johnell O, Kanis JA (2003) Cost-equivalence of different osteoporotic fractures. Osteoporos Int 14(5):383–388
Melton LJ (2003) Adverse outcomes of osteoporotic fractures in the general population. J Bone Miner Res 18(6):1139–1141
Lindsay R, Burge RT, Strauss M (2005) One year outcomes and costs following a vertebral fracture. Osteoporos Int 16:78–85
Tosteson AN, Gabriel SE, Grove MR, Moncur MM, Kneeland TS, Melton LJ 3rd (2001) Impact of hip and vertebral fractures on quality-adjusted life years. Osteoporos Int 12(12):1042–1049
Owen RA, Melton LJ, Gallagher JC, Riggs BL (1980) The national cost of acute care of hip fractures associated with osteoporosis. Clin Orthop Relat Res 150:172–176
Chen Z, Maricic M, Aragaki AK, Mouton C, Arendell L, Lopez AM, Bassford T, Chlebowski RT (2009) Fracture risk increases after diagnosis of breast or other cancers in postmenopausal women: results from the Women’s Health Initiative. Osteoporos Int 20(4):527–536
Abelson A (2008) A review of Paget’s disease of bone with a focus on the efficacy and safety of zoledronic acid 5 mg. Curr Med Res Opin 24(3):695–705
Blouin S, Libouban H, Moreau MF, Chappard D (2008) Orchidectomy models of osteoporosis. Methods Mol Bio 455:125–134
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis 40(5):373–383
Romano PS, Roos LL, Jollis J (1993) Adapting a clinical comorbidity index for use with ICD-9-CM administrative data. J Clin Epidemiol 46(10):1075–1079
Lyles KW, Schenck AP, Colon-Emeric CS (2008) Hip and other osteoporotic fractures increase the risk of subsequent fractures in nursing home residents. Osteoporos Int 19(8):1225–1233
Kanis JA (2009) FRAX WHO Fracture Risk Assessment Tool. World Health Organization Collaborating Center for Metabolic Bone Diseases, University of Sheffield. http://www.shef.ac.uk/FRAX/. Accessed 10 Sep 2009
Nguyen TV, Center JR, Eisman JA (2004) Osteoporosis: underrated, underdiagnosed and undertreated. Med J Aust 180(5 Suppl):S18–S22
Vestergaard P, Renjnmark L, Mosekilde L (2005) Osteoporosis is markedly underdiagnosed: a nationwide study from Denmark. Osteoporos Int 16(2):134–141
Westesson PL, Lee RK, Ketkar MA, Lin EP (2002) Underdiagnosis and undertreatment of osteoporosis. Lancet 360(9348):1891
Gunter MJ, Beaton SJ, Brenneman SK, Chen YT, Abbott TA 3rd, Gleeson JM (2003) Management of osteoporosis in women aged 50 and older with osteoporosis-related fractures in a managed care population. Dis Manag 6(2):83–91
Sasser AC, Rousculp MD, Birnbaum HG, Oster EF, Lufkin E, Mallet D (2005) Economic burden of osteoporosis, breast cancer, and cardiovascular disease among postmenopausal women in an employed population. Womens Health Issues 15(3):97–108
Kowalski SC, Sjenzfeld VL, Ferraz MB (2004) Resource utilization in postmenopausal osteoporosis without incident fractures. J Rheumatol 31:938–942
Rabenda V, Manette C, Lemmens R, Mariani A-M, Struvay N, Reginster J-Y (2006) The direct and indirect costs of the chronic management of osteoporosis: a prospective follow-up of 3440 active subjects. Osteoporos Int 17:1346–1352
Seeman E (2007) Unmet needs in fracture prevention: new European guidelines for the investigation and registration of therapeutic agents. Osteoporos Int 18(5):569–573
Acknowledgments
We thank Dr Susan Dennett of Eli Lilly and Company for her contributions to the study design. We also thank Dr Anna Gu and Hari Sharma for providing computer programming input on various aspects of the analysis.
Conflict of interest
This research project was funded by Eli Lilly and Company. Drs. Russel Burge and Eric Edgell are employees of Eli Lilly and Company in the Global Health Outcomes department. Eli Lilly and Company markets pharmacological therapies for the prevention and treatment of osteoporosis.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary materials
ESM 1
(PDF 23 kb)
Rights and permissions
About this article
Cite this article
Pike, C., Birnbaum, H.G., Schiller, M. et al. Economic burden of privately insured non-vertebral fracture patients with osteoporosis over a 2-year period in the US. Osteoporos Int 22, 47–56 (2011). https://doi.org/10.1007/s00198-010-1267-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-010-1267-5