Abstract
Aim: To compare the number of patients diagnosed with osteoporosis and osteoporotic fractures in Denmark, with the number of subjects expected to have osteoporosis. Subjects and methods: From the National Hospital Discharge Register, records for all patients diagnosed with osteoporosis and/or with osteoporotic fractures between 1995 and 1999 were retrieved. Based on normal Danish values for BMD, the expected number of subjects aged 50 years or more with osteoporosis according to the WHO definition was calculated. Results: The estimated prevalence of osteoporosis was 40.8% of women aged ≥50 years and 17.7% among men. The expected annual incidence was 58,658/million inhabitants in women ≥50 years of age and 23,648/million in men ≥50 years. However, the observed incidence was only 4,823 and 862/million per year, respectively (8.2% and 3.6% of the expected). In 1999, a total of 34,691 hip, spine, and forearm fractures were reported in subjects ≥50 years, and of these, 18,566 were potentially attributable to osteoporosis (14,240 fractures in women and 4,326 in men equaling 14,976 and 5,297/million per year). Only 0.3% of men ≥50 years were receiving a bisphosphonate, while 2.2% of women received a bisphosphonate or raloxifene. Among women ≥50 years, 27.7% received hormone replacement therapy. Conclusions: Osteoporotic fractures of the hip, spine, and forearm are rather frequent in Denmark, but the diagnosis of osteoporosis is rarely used. It seems that osteoporosis is markedly underdiagnosed and undertreated in Denmark as probably also elsewhere. This may have significant implications for the prevention of osteoporotic fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporotic fractures are frequent in many countries, and a significant increase in incidence has been seen [1]. Osteoporosis thus presents a major health problem [2]. Osteoporosis may be diagnosed as low bone mineral density (BMD, g/cm2) measured by dual-energy X-ray absorptiometry (DXA or osteodensitometry). A working group associated with the WHO have suggested that in females a T-score measured by osteodensitometry of more than 2.5 standard deviations below the mean of normal young adult females should be diagnostic for osteoporosis [3]. Although the definition of a T-score diagnostic for osteoporosis in males poses more difficulties, a T-score <–2.5 may also be applied [4]. The diagnosis thus does not require previous or actual low-energy fractures. The diagnosis based on osteodensitometry makes it possible to identify individuals with an increased fracture risk and thereby to prevent fractures from occurring through life style changes and pharmaceutical therapy [5]. However, although this possibility has been present for 2 decades, it still seems that osteoporosis may be underdiagnosed.
If the distribution of BMD in normal subjects is known in a population, it is possible to calculate the number of men and women aged ≥50 years with a T-score <–2.5; i.e., the number who per definition have osteoporosis. This number may then be compared with the number of subjects actually diagnosed with osteoporosis.
A large proportion of fractures of the hip (80–95%) [6], forearm (70–84%) [7], and spine (82–89%) [7] in subjects aged 50 years or more are thought to be attributable to osteoporosis. These fractures may thus be used as proxy variables for the occurrence of osteoporosis in a population in the absence of densitometric data.
The aims of this study were (1) to assess the expected prevalence (proportion) of subjects with osteoporosis in Denmark judged from the normal age- and sex-stratified values for BMD, (2) to establish the actual number of subjects diagnosed with osteoporosis, and (3) to report the number of subjects with osteoporotic fractures (hip, spine, and forearm) as well as the number of subjects receiving antiresorptive therapy, and examine to what extent this number was in the range expected from the number of subjects expected to have osteoporosis.
Subjects and methods
Denmark offers good possibilities for studies of the occurrence of osteoporosis due to the extensive nature of registers covering contacts with the health sector [8]. Furthermore, the population is relatively homogeneous, and studies on the BMD of normal subjects are available [9]. In the actual study, additional data were included (see below).
The National Hospital Discharge Register [10] covers all contacts (on an inpatient or outpatient basis) to hospitals from 1995 and onwards. The register was founded in 1977, but outpatient records were first completely incorporated from 1995. The register has nationwide coverage of public hospitals with an almost 100% completeness of recordings and a high precision of diagnoses [10] especially of fracture diagnoses [11]. The National Health Service is financed via taxes and is free of charge to the inhabitants. We used this register to track the number of subjects diagnosed with osteoporosis and the number sustaining fractures.
Records for all subjects having a diagnosis of osteoporosis (ICD10: M80, osteoporosis with a pathological fracture; M81, osteoporosis without a pathological fracture; M82, osteoporosis following diseases—see “Appendix” for details) between 1995 and 1999 were retrieved. Also, records for all subjects with fractures of the hip (S720, S721), forearm (S520–S529), or spine: S120–S129, S220–S221, S320–S328) between 1995 and 1999 were retrieved. By doing this, subjects with a diagnosis of osteoporosis were identified irrespective of presence or not of an osteoporotic fracture (hip, spine, or forearm). Furthermore, subjects with typical osteoporotic fractures (hip, spine, or forearm) were also identified irrespective of whether or not they had received a diagnosis of osteoporosis (i.e., based on densitometry). By including fracture cases (hip, spine, forearm) it was possible to identify subjects who—in combination with the age criterion—have a high likelihood of osteoporosis. Since Danish orthopedic surgeons most often only diagnose the fracture and not the underlying disease (osteoporosis), misclassification is avoided. The Danish population totaled 5,313,568 in 1999 [12].
The age-specific incidence of fractures of the hip, spine, and forearm, and osteoporosis was calculated as cumulated incidence proportions based on the numbers from the register and the number of subjects in each age stratum using the national census from the National Bureau of Statistics (Danmarks Statistik). The incidence was calculated for first-time fractures—i.e., second fractures and second admissions were excluded. We had access to data from the period 1977–1999, and the data presented span the period 1995–1999. Upon admission for a new (incident) fracture, codes for the trauma that led to the fracture are entered, while the register separates readmissions for the same fracture, e.g., for removal of osteosynthesis material and complications. It is thus possible to extract the number of first-time admissions for any given fracture, and from information on the individual, it is possible to exclude subjects admitted, e.g., twice with incident forearm fractures. We compared our fracture data with those from Sweden [13] (a neighboring Scandinavian country) and the United States [14]. In the Swedish data [13], second fractures were excluded the same way as in our data. In the US data [14], second fractures were apparently not excluded. However, since fracture incidence is low, this only represents a minor source of error.
The original WHO technical report on osteoporosis stated that in women, osteoporosis was present if a measurement of BMD at any skeletal site gave a T-score below −2.5 [3]. This T-score <−2.5 criterion has also been adopted in men, although problems exist making the cut point in men uncertain [4]. More recent guidelines from the IOF and NOF have put emphasis on hip BMD measurements [15] based on data from the NHANES III study [16]. Data from the NHANES III study have demonstrated hip BMD variations with different ethnic origin [16]. Danes have a somewhat different ethnic background from white Americans in the same way as white and Hispanic Americans differ in ethnic background.
Calculations on the number of subjects with a T-score <−2.5 were performed using both the NHANES III data and a normal range for the Danish population.
The normal range for Danish citizens in the hip and spine was based on the normal data from T.J. Kelly [17] supplied by Hologic. These data for the normal range were tested against hip and spine BMD based on a database of 11,359 Danish subjects (1,426 men and 9,933 women) who had been screened on a Hologic 2000 DXA machine from 1990 to 2000 in order to recruit participants for different clinical studies. The deviations between these 11,359 Danish subjects and the data by T.J. Kelly [17] were minute in the hip, and a little larger in the spine (within ±0.3 SD) showing that the data gathered by T.J. Kelly were [17] indeed representative as Danish reference values. The change in BMD with age was based on the T.J. Kelly data [17], as the deviations between these data and the 11,359 Danish subjects were small. Based on the knowledge about the BMD change with age, it was possible to calculate the proportion of subjects in each age that would have a T-score <−2.5, as the BMD distribution was approximately Gaussian in each age strata. From the proportion in each age strata with a T-score <−2.5 and knowledge about the distribution of subjects in each age stratum from the census, it was possible to calculate the number of subjects with a T-score <−2.5.
The T-score in the spine was based on the mean values for a 30-year-old subject. In the hip, the NHANES values were based on the age group of 20–29 years, and the T.J. Kelly data [17] on the mean values of a 30-year-old subject. The mean (SD) femoral neck BMD in 20–29-year-old female Caucasians in the NHANES III sample is 0.858 (0.12) and 0.886 (0.10) for 30-year-old women in the T.J. Kelly data [17] that is equivalent to normal Danish subjects as confirmed by the cross-reference with the 11,359 subjects mentioned above.
National guidelines on reimbursement of antiosteoporotic drugs state that the diagnosis of osteoporosis should be based on a T-score <−2.5 in either the hip or spine [18]. Thus in Denmark a diagnosis of osteoporosis may be based on BMD data from the hip, spine, or both. To address this, we calculated the likelihood of having a T-score <−2.5 in the hip, spine, or both. Due to the correlation between BMD of the hip and spine, there is considerable overlap but not total overlap between BMD values. The overlap was assessed using the database of 11,359 subjects. Data for a T-score below −2.5 in the hip, spine, or both has been presented separately.
From the data described above it was possible to calculate the expected prevalence (PP) of subjects with osteoporosis (a T-score <−2.5). However, from the available registers, only the incidence rate of newly diagnosed osteoporosis could be retrieved. It is, however, possible to estimate the incidence of osteoporosis from the prevalence if the mean disease duration (D) is known [19]. If osteoporosis is assumed to be irreversible (at least in the untreated state), the disease duration must be the time interval from the age of diagnosis of osteoporosis until death of the individual. This disease duration is thus the mean life expectancy minus the mean age at diagnosis of osteoporosis. The life expectancy was adjusted to match the increased death risk in subjects with osteoporosis. From these two sources (disease duration, D, in years, and estimated prevalence, PP, derived from the calculations of osteoporosis prevalence above), the incidence rate (IR) of newly diagnosed osteoporosis can be estimated from the formula: IR=(PP/(1−PP))/D [19]. This expected incidence rate was then compared with the number of patients actually receiving a diagnosis of osteoporosis and the number of subjects with fractures attributable to osteoporosis.
The number of subjects actually receiving antiosteoporotic treatment (raloxifene, hormonal replacement therapy, and bisphosphonates, but not calcium and vitamin D) was retrieved from the Danish Medicines Agency (http://www.laegemiddelstyrelsen.dk/index_en.htm). As these drugs are reimbursed by the authorities, an almost 100% coverage of subjects treated for osteoporosis with these drugs is ensured. Calcium and vitamin D are not reimbursed, so their use cannot be assessed from the register.
Results
Table 1 shows the prevalence proportion of subjects aged ≥50 years with osteoporosis (BMD T-score <−2,5) in either the femoral neck or the spine. The prevalence increased steadily with age in both men and women. The estimated prevalence of osteoporosis was 40.8% of women aged ≥50 years and 17.7% among men based on a T-score <−2.5 in either the hip, spine, or both. The proportion with osteoporosis in the femoral neck based on the NHANES III database was smaller than that based on the reference range from the Danish citizens.
The hip was the main contributor to a T-score <−2.5 in the population, but the spine also contributed, especially in women, and to some degree in men aged less than 85 years.
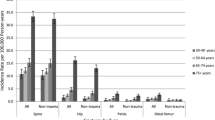
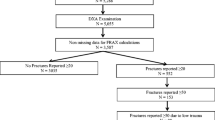
The mean age at diagnosis of osteoporosis was 73 years in women and 70 years in men, and the expected disease duration (D) was 11 years in women and 9 years in men (equaling the expected remaining lifetime). This yielded an expected annual incidence rate for 1999 in subjects aged ≥50 years of 58,658/million inhabitants (55,775 subjects) in women and 23,684/million in men (19,341 subjects, combined 42,499/million per year or 75,116 subjects). According to the National Hospital Discharge Register, only 5,929 subjects received the diagnosis of osteoporosis in 1999. Among these, 5,290 were 50 years or older, yielding an observed incidence of 4,823 in women and 862/million per year in men, respectively (8.2% and 3.6% of the expected). Table 2 shows the age- and gender-specific incidence rates for the diagnosis of osteoporosis (M80–M82) between 1995 and 1999, according to the National Hospital Discharge Register. Figures 1, 2, 3, and 4 show the annual incidence of all fracture types and of fractures in the hip, forearm, and spine.
Incidence rate (cumulated incidence proportion) for hip fractures between 1995 and 1999 in Denmark. In 1999, a total of 11,151 subjects sustained a hip fracture. Shown for comparison are fracture rates from the United States (modified from Melton et al. [14]) and Sweden (modified from Kanis et al. [13]). Note the difference on the abscissa
Incidence of distal forearm fractures (cumulated incidence proportion) between 1995 and 1999 in Denmark. In 1999, a total of 19,947 subjects sustained a distal forearm fracture. Shown for comparison are fracture rates from the United States (modified from Melton et al. [14]) and Sweden (modified from Kanis et al. [13]). Note the difference on the abscissa
Incidence rate (cumulated incidence proportion) of vertebral fractures in Denmark between 1995 and 1999. In 1999, a total of 3,593 subjects sustained a vertebral fracture. Shown for comparison are fracture rates from the United States (modified from Melton et al. [14]) and Sweden (modified from Kanis et al. [13]). Note the difference on the abscissa
In 1999, a total of 34,691 hip, spine, and forearm fractures were reported in subjects ≥50 years, and of these 18,566 (9,686 hip, 6,857 distal forearm, and 2,023 spine fractures) were potentially attributable to osteoporosis (14,240 fractures in women and 4,326 in men equaling 14,976 and 5,297/million per year).
Hip fractures first started to emerge after the age of 50, earlier in women than men (Fig. 2), while distal forearm fractures had the same bimodal course as for all fracture types (Fig. 3). Spine fractures were rare before the age of 50 (Fig. 4) resulting in a bimodal course for all fracture types combined (Fig. 1) with a peak in young individuals around puberty and a steady increase with age after age 50 years in women and 80 years in men.
The incidence rates for hip and forearm fracture were similar in Denmark and Sweden, and a little higher for the hip and somewhat higher in older women for the forearm fractures compared with the US data (Figs. 2 and 3).
Osteoporosis treatment
In 1999, at total of 21,027 women (2.2% of women ≥50 years) were reimbursed for a prescription for raloxifene and/or a bisphosphonate, and a total of 2,776 men (0.3% of men ≥50 years) were reimbursed for a prescription for a bisphosphonate. In addition, a total of 263,711 women (27.7% of women ≥50 years) used postmenopausal hormone replacement therapy.
Among those aged ≥50 years with any fracture, 4.6% of men and 27.7% of women had used any antiresorptive drug (bisphosphonate, SERM, or HRT). Among the women, HRT was used by 16.4%, bisphosphonates by 12.8%, and SERM by 1.1%. Among those aged ≥50 years with a hip fracture, 2.7% of the men and 9.4% of the women had used a bisphosphonate. Among the women, 9.0% had used HRT and 0.5% had used SERM. In patients with Colles fractures the corresponding numbers were 1.3% of men and 6.1% of women for bisphosphonates. Among women, 13.8% had used HRT, while 0.6% had used a SERM. Among spine fracture cases, 6.9% of men and 21.0% of women had used a bisphosphonate, while 14.3% of the women had used HRT and 1.4% had used a SERM.
Discussion
In this nationwide epidemiological study, we have demonstrated that osteoporosis is significantly underdiagnosed in Denmark.
The retrieved sum of registered fractures potentially attributable to osteoporosis was high (approximately 18,000 per year) but most likely underreported. Some of the osteoporosis codes covered fractures (M81), thus the actual number of osteoporotic fractures may be even higher. Other fracture sites (e.g., the proximal humerus and the pelvis [20]), which may contribute to osteoporotic fractures, were not included in the present study. Furthermore, only a smaller proportion of all spine fractures are symptomatic [21], and some patients with back pain may not be referred for hospital care or X-rays of the spine [9]. The number of osteoporotic fractures in the spine may thus be higher than estimated from the registers in this study. In this paper, figures for spine fractures cover symptomatic cases. However, the percentage of spine fractures that are symptomatic may vary. In the FIT study of women aged 51–81 years, only around a third of all vertebral fractures were symptomatic [21], while only around 10% of vertebral fractures in women aged 45–58 years were symptomatic in a Danish trial [9]. In Sweden, 42% of vertebral fractures in men and 22% in women come to clinical attention [22]. The presence of pain in patients with vertebral fractures may also be related to the fracture type [23]. These differences in vertebral fractures that come to clinical attention are a further source of uncertainty in evaluating the incidence of spine fractures. The number of vertebral fractures coming to clinical attention thus seems to be lower in Denmark than in Sweden. Based on figures from Sweden [13], a total of 8,068 vertebral fractures should have been expected, in contrast to the 2,309 observed fractures among men and women aged ≥50 years in 1999—i.e., considerably fewer.
It may be that some of these fractures are potentially preventable, if an earlier diagnosis of osteoporosis was made based on DXA and preventive measures initiated before fractures occurred.
However, the incidence rates for hip and forearm fracture were similar in Denmark and Sweden [13], and a little higher for the hip and somewhat higher in older women for the forearm fractures compared with the US data [14] (Figs. 2 and 3). Our data and the Swedish data were sampled excluding second fractures, while this was not the case with the US data, but despite this, the rates in the US data were smaller. However, as fracture risk is low, second fractures only add marginally to the overall fracture incidence.
The Hospital Discharge Register does not capture diagnoses made by general practitioners and practicing specialists in endocrinology, rheumatology, etc., along with patients being enrolled in clinical trials and not managed in the public health system. The incidence rate for osteoporosis at 5,000 subjects per year in 1999 may thus be severely underestimated. However, despite this, the fraction of subjects receiving antiosteoporotic drugs is very limited even in high-risk groups [24, 25], supporting the conclusion that there is not only a significant underdiagnosing, but also a significant undertreatment. The weakness in these registers is that use of calcium and vitamin D are not covered, as these drugs are not reimbursed. Furthermore, estrogen-containing preparations may be used mainly for treatment of menopausal symptoms and only to a degree to prevent osteoporosis [26]. The reason fewer fracture patients had used HRT than in the general population was that the fracture cases were older than the general population, and older women were less likely to use HRT than younger women.
The study also demonstrates differences in the proportion being diagnosed as having osteoporosis if different normal data for BMD (the NHANES III or the country-specific normal datal) are used. Danish citizens have higher BMD values than non-Hispanic white Americans, and thus fewer will receive a diagnosis of osteoporosis if the NHANES III reference values are used. Despite their BMD being higher, the fracture rates were much higher in Denmark than in America [14] (e.g., around 3.5% per year for hip fractures vs around 2% per year in 80-year-old women). If US BMD values were applied, few patients would be offered preventive measures against osteoporosis.
In our study, prevalence data for T-scores <−2.5 are presented for both the hip and spine. The NOF guidelines [15] emphasize using the hip site for diagnosis of osteoporosis. By using the combined sites of the hip and spine, more subjects would be diagnosed with osteoporosis than by just using the hip site. However, even though this may have been the case in the actual study as the diagnosis of osteoporosis in Denmark may be based on either the hip or the spine, the number actually diagnosed with osteoporosis was still much lower than anticipated and would have been even lower if only the hip site had been used.
The incidence of fractures is also high compared with other European countries [27]. However, the bimodal fracture pattern for the forearms was close to that observed in other studies [28, 29]. The incidence of hip fractures was within the range seen in other Scandinavian countries [2, 30]. The reasons for the high fracture rates are only partly understood, but may be related to (1) low vitamin D levels due to low exposure to sunlight in northern Europe [31], and (2) a high smoking frequency [32] and perhaps also underdiagnosis and undertreatment as stated. The change in fracture risk is the same with 1 SD decrease in BMD in Denmark [9] as in other countries [33], so differences in bone quality cannot explain the difference in fracture risk between Danish and US citizens.
The reason the spine only contributed a little to the total prevalence of a T-score <−2.5 in older men was a high concordance between the hip and spine site, whereas the concordance was lower in women and younger men.
The definition of osteoporosis based on BMD is at present uncertain in men, and revised data may be necessary to determine the prevalence of osteoporosis in men. In our study, we have used the same cut point (T-score <−2.5 ) as in women, but a different cut point may perhaps be necessary in men [4]. From these data, the prevalence of osteoporosis was lower in men than in women, and the number of osteoporotic fractures of the hip, spine, and forearm was also lower in men than in women. The incidence of osteoporotic fractures of the hip, spine, and forearm started to increase later in men than in women at all sites.
Men have a shorter life expectancy than women, and this was reflected in the observation that the disease duration was shorter (9 years) in men than in women (11 years). However, despite the appearance of osteoporotic fractures at a later age in men than in women, osteoporosis was diagnosed at an earlier age in men. This may reflect that the cutoff values for the diagnosis of osteoporosis in men should be at a different level from −2.5; however, it may also reflect that in men secondary osteoporosis is more frequent than in women [34]. The causes of secondary osteoporosis (hypogonadism, hyperthyroidism, inflammatory bowel disorders, etc.) all present at a younger age than age-related osteoporosis, and this may also contribute to the younger age at diagnosis in men.
In conclusion, osteoporotic fractures of the hip, spine, and forearm are rather frequent in Denmark, but the diagnosis of osteoporosis is rarely used. It seems that osteoporosis is markedly underdiagnosed and undertreated in Denmark, as it probably also is elsewhere. This may have significant implications for the prevention of osteoporotic fractures.
References
Kannus P, Niemi S, Parkkari J et al (1999) Hip fractures in Finland between 1970 and 1997 and predictions for the future [see comments]. Lancet 353:802–805
Kannus P, Parkkari J, Sievanen H et al (1996) Epidemiology of hip fractures. Bone 18:57S–63S
Alexeeva L, Burkhardt P, Christiansen C et al (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: report of a WHO Study Group, 1st edn. WHO Technical Report Series, No. 843. World Health Organization, Geneva
Faulkner KG, Orwoll E (2002) Implications in the use of T-scores for the diagnosis of osteoporosis in men. J Clin Densitom 5:87–93
Vestergaard P, Rejnmark L, Mosekilde L (2001) Hip fracture prevention: cost-effective strategies. Pharmacoeconomics 19:449–468
Ray NF, Chan JK, Thamer M, Melton LJ (1997) Medical expenditures for the treatment of osteoporotic fractures in the United States in 1995: report from the National Osteoporosis Foundation. J Bone Miner Res 12:24–35
Phillips S, Fox N, Jacobs J, Wright WE (1988) The direct medical costs of osteoporosis for American women aged 45 and older, 1986. Bone 9:271–279
Frank L (2000) Epidemiology: when an entire country is a cohort. Science 287:2398–2399
Mosekilde L, Beck-Nielsen H, Sørensen OH et al (2000) Hormonal replacement therapy reduces forearm fracture incidence in recent postmenopausal women—results of the Danish Osteoporosis Prevention Study. Maturitas 36:181–193
Andersen TF, Madsen M, Jørgensen J, Mellemkjaer L, Olsen JH (1999) The Danish National Hospital Register. Dan Med Bull 46:263–268
Vestergaard P, Mosekilde L (2002) Fracture risk in patients with celiac disease, Crohn’s disease, and ulcerative colitis: a nation-wide follow-up study in 16,416 patients in Denmark. Am J Epidemiol 156:1–10
Anonymous (1999) Statistical yearbook 1999, 1st edn. Danish Bureau of Statistics, Copenhagen
Kanis JA, Johnell O, Oden A et al (2000) Long-term risk of osteoporotic fracture in Malmo. Osteoporos Int 11:669–674
Melton LJ III, Crowson CS, O’Fallon WM (1999) Fracture incidence in Olmsted County, Minnesota: comparison of urban with rural rates and changes in urban rates over time. Osteoporos Int 9:29–37
Dawson-Hughes B, Gold DT, Rodbard HW, Bonner FJ JR, Khosla S, Swift S (2003) Physician’s guide to prevention and treatment of osteoporosis, 2nd edn. National Osteoporosis Foundation, Washington DC
Looker AC, Wahner HW, Dunn WL et al (1999) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8:468–489
Kelly TJ (1990) Bone mineral density reference database for American men and women. J Bone Miner Res 5[Suppl 2]:S249
Anonymous (2000) [Changes in the criteria for reimbursement of bisphosphonates or raloxifen for preventing osteoporosis] (in Danish). Ugeskr Laeger 162:6512
Rothman KJ (2002) Epidemiology: an introduction, 1st edn. Oxford University Press, Oxford
Melton LJ III (1995) Epidemiology of fractures. In: Riggs BL, Melton LJ III (eds) Osteoporosis: etiology, diagnosis, and management, 2nd edn. Lippincott-Raven, Philadelphia, pp 225–247
Black DM, Cummings SR, Kerpf DB et al (1996) Randomised trial of the effect of alendronate on risk of fracture in women with existing vertebral fractures. Lancet 348:1535–1541
Kanis JA, Johnell O, Oden A et al (2004) The risk and burden of vertebral fractures in Sweden. Osteoporos Int 15:20–26
Ismail AA, Cooper C, Felsenberg D et al (1999) Number and type of vertebral deformities: epidemiological characteristics and relation to back pain and height loss. European Vertebral Osteoporosis Study Group. Osteoporos Int 9:206–213
Christensen PM, Kristensen IS, Brøsen K, Brixen K, Abrahamsen B, Andersen M (1999) The use of prednisolone and concurrent pharmacological prophylaxis against osteoporosis: a population based study using a drug prescription database. J Bone Miner Res 14[Suppl 1]:S524 (Abstract)
Olesen C, Sørensen HT, Steffensen FH, Nielsen GL, Olsen J (1996) Danish data confirm low prevalence of HRT among women prescribed oral corticosteroids. BMJ 313:344–346
Køster A (1990) Hormone replacement therapy: use patterns in 51-year-old Danish Women. Maturitas 12:345–356
Felsenberg D, Silman AJ, Lunt M et al (2002) Incidence of vertebral fracture in europe: results from the European Prospective Osteoporosis Study (EPOS). J Bone Miner Res 17:716–724
Falch JA (1983) Epidemiology of fractures of the distal forearm in Oslo, Norway. Acta Orthop Scand 54:291–295
Kramhøft M, Bødtker S (1988) Epidemiology of distal forearm fractures in Danish children. Acta Orthop Scand 59:557–559
Bacon WE, Maggi S, Looker A et al (1996) International comparison of hip fracture rates in 1988–89. Osteoporos Int 6:69–75
Brot C, Vestergaard P, Kolthoff N, Gram J, Sørensen OH (2001) Vitamin D status and its adequacy in healthy Danish perimenopausal women: relationships to dietary intake, sun exposure and serum parathyroid hormone. Br J Nutrition 86[Suppl 1]:97–103
Vestergaard P, Mosekilde L (2003) Fracture risk associated with smoking: a meta-analysis. J Intern Med 254:572–583
Marshall D, Johnell O, Wedel H (1996) Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 312:1254–1259
Stein E, Shane E (2003) Secondary osteoporosis. Endocrinol Metab Clin North Am 32:115–134
Author information
Authors and Affiliations
Corresponding author
Appendix: ICD10 codes for osteoporosis
Appendix: ICD10 codes for osteoporosis
- M80.:
-
Osteoporosis with a pathological fracture
- M80.0.:
-
Postmenopausal osteoporosis with a pathological fracture
- M80.1.:
-
Osteoporosis after oophorectomy presenting with a pathological fracture
- M80.2.:
-
Disuse osteoporosis with a pathological fracture
- M80.3.:
-
Osteoporosis linked to malabsorption after surgery on the stomach or intestine presenting with a pathological fracture
- M80.4.:
-
Drug-induced osteoporosis (e.g., glucocorticoid-induced osteoporosis—an ATC code is mandatory) presenting with a pathological fracture
- M80.5.:
-
Idiopathic osteoporosis with a pathological fracture
- M80.8.:
-
Other forms of osteoporosis with a pathological fracture
- M80.9.:
-
Nonspecified osteoporosis with a pathological fracture
- M81.:
-
Osteoporosis without a pathological fracture
- M81.0.:
-
Postmenopausal osteoporosis
- M81.1.:
-
Osteoporosis after oophorectomy
- M81.2.:
-
Disuse osteoporosis
- M81.3.:
-
Osteoporosis linked to malabsorption after surgery on the stomach or intestine
- M81.4.:
-
Drug-induced osteoporosis (e.g., glucocorticoid induced osteoporosis—an ATC code is mandatory)
- M81.5.:
-
Idiopathic osteoporosis
- M81.6.:
-
Localized osteoporosis
- M81.8.:
-
Other forms of osteoporosis
- M81.9.:
-
Nonspecified osteoporosis
- M82.:
-
Osteoporosis following other classified diseases
- M82.0.:
-
Osteoporosis following multiple myeloma
- M82.1.:
-
Osteoporosis following endocrine disorders (e.g., hyperthyroidism)
- M82.8.:
-
Osteoporosis in other classified diseases
Rights and permissions
About this article
Cite this article
Vestergaard, P., Rejnmark, L. & Mosekilde, L. Osteoporosis is markedly underdiagnosed: a nationwide study from Denmark. Osteoporos Int 16, 134–141 (2005). https://doi.org/10.1007/s00198-004-1680-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-004-1680-8