Abstract
Introduction and hypothesis
Despite minimal fundamental works, there is an increasing use of meshes in urogynecology. The concept is mainly based on experiences with abdominal wall surgery. We aimed to compare the biomechanical properties of vaginal tissue, abdominal aponeurosis, and skin.
Methods
Samples from 11 fresh women cadavers without prolapse were collected. Uniaxial tension tests were performed and stress–strain curves were obtained.
Results
Biomechanical properties of the vagina, aponeurosis, and skin differed significantly. The aponeurosis was much more rigid and less extendible than the vagina and skin. Vaginal tissue was less rigid but more extendible than skin. There was no difference between the vagina and skin at low strains (p = 0.341), but a highly significant difference at large strains (p = 0.005).
Conclusions
Skin and aponeurosis are not suited to predict vaginal tissue biomechanics. We should be cautious when transferring experiences from abdominal wall surgery to vaginal reconstructive surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic organ prolapse (POP) constitutes a major health issue and significantly contributes to a decrease in the quality of life of aging women [1, 2]. There is now strong evidence that abnormalities of the connective tissue composition may contribute to the genesis of POP [3–5]. Such alterations can have a direct impact on the biomechanical properties of pelvic floor supportive tissues, subsequently leading to the development of a clinically relevant POP [6].
In POP surgery, native vaginal tissue is widely used as a corrective support, while its biomechanical properties are unknown. In an attempt to improve outcomes and durability of surgery, and in spite of minimal fundamental work, there is now increasing use of prosthetic materials in the management of POP. However, the mechanical characteristics of these materials have not yet been compared with those of the vagina. To date, the majority of observations on synthetic prostheses have come from the field of abdominal wall surgery and the repair of groin hernias [7, 8], and prostheses currently used in POP surgery are not designed to mirror the biomechanics of “normal vaginal tissue” [9]. A better understanding of vaginal and abdominal wall tissue biomechanics could enhance the development of “more functional” prostheses designed for use in vaginal prolapse surgery in the future. If vaginal and abdominal wall tisssues were comparable from a biomechanical point of view, it would be tempting to speculate on a simple skin test in order to predict vaginal tissue properties. Moreover, the investigation of vaginal tissue biomechanics can provide new insights into the pathophysiology of POP. However, to date, there is a paucity of data on these issues.
Therefore, we aimed to test if tissues from the abdominal wall can be studied to extrapolate the biomechanics of vaginal tissue. To reach this goal, we characterized and compared the biomechanical properties of tissues derived from the vagina, the abdominal aponeurosis, and skin of 11 fresh women cadavers without POP.
Materials and methods
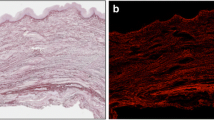
Recently, we were able to establish and validate a new experimental protocol for the biomechanical characterization of vaginal tissue [10]. Tissues were obtained from 11 fresh women cadavers without a clinically relevant POP, which was excluded by gynecological examination and using a Pozzi clamp to pull the cervix. The cadavers were not formolized but frozen for conservation and unfrozen just before the dissection. Each patient consented prior to death to have their cadaver used for medical purposes according to the legislation in force. The institutional review board approved the experimental protocol. Vaginal specimens were collected from the anterior and posterior vaginal wall by the vaginal route. A midline incision was performed in the longitudinal axis of the vaginal wall. The bladder or rectum was reflected off the vaginal wall before the full-thickness vaginal tissue was excised. Tissue measuring at least 3 × 1 cm was excised in the longitudinal axis of the vagina with the initial midline incision as the medial border. Abdominal skin was obtained after excision of a rectangularly shaped tissue matrix from the lower part of the abdomen at the level of the halfline distance between the pubic symphysis and the umbilicus. The skin was excised in longitudinal direction and was carefully separated from any surrounding fatty tissue. Subsequently, tissue of at least 5 × 3 cm from the subjacent aponeurosis was excised in a longitudinal direction starting from a midline incision. All samples were orientated and marked before being frozen in 0.9% salt solution at −18°C. The excised tissues were used to carry out uniaxial tension tests to the point of rupture as previously described [10]. Importantly, all parameters that could alter tissue behavior during the test (e.g., conditioning of tissue before test, conditions of tension test such as temperature, rate of deformation, hydrometry) have been exhaustively studied before [10]. Briefly, the tissue samples were unfrozen 9 h before the tests. In order to obtain an area of uniform stress in the center of the test samples during the tension test, standardized 25 × 4-mm test samples were excised from the tissues using a punch (Fig. 1a). The thickness of each sample was measured with palmer to further determine the nominal stress (F/S 0, where F is the load and S 0 is the size of the initial cross section). The thickness varied between 1 and 2 mm depending on the tissue, while the controlled width was equal to 4 mm, as determined by the punch. Each sample was clamped in a tightening grip and strained at a constant strain rate (2 × 10−2 s−1) at ambient temperature (20°C) within 24 h after unfreezing. The distance between the tightened grips was 15 mm, and 5 mm of tissue was clamped on each end. The grips fixture has been designed in a way that prevents tissue slippage during the test (Fig. 1b) [10]. Samples were directly loaded, without preloading phase. The presented results are taking into account the complete response from zero force up to rupture. The rupture tests were performed using a conventional tension machine (Instron 4302™). Each test was repeated for each tissue on different samples from the same cadaver, at least twice (range, 2–5). A low capacity load cell (1 kN) was used to measure the nominal stress (force per unit of surface) during the test, knowing the forces and the initial cross section of the samples. The load cell sensitivity was 0.01 N (0.001 class) and is in agreement with the quantity measured. Strains (l − l 0 / l 0 where l is the length and l 0 the initial length) were measured with a contactless video extensometer. Subsequently, the stress–strain curves were obtained and analyzed to characterize the biomechanical behavior of the considered tissues. The mechanical response of the specimens before rupture was then studied. The fact of studying nonlinear elasticity required at least the application of two parameters: C0 and C1. The stress–strain curves allowed calculation of these values which are identified on the complete mechanical response, thanks to a least-squared roots method (Mooney–Rivlin model) [11–13]. C0 characterizes the stress–strain curve at its beginning phase (i.e., low strains, under 5%), whereas C1 characterizes the form of the asymptote towards the end of the stress–strain curve (i.e., large strains).
For statistical analysis, the SPSS version 16.0 (SPSS Inc., Chicago, IL, USA) was used. Homogeneity between the 11 cadavers with respect to their biomechanical properties (i.e., C0 and C1 values obtained for vaginal tissue, skin, and aponeurosis, respectively) was analyzed using nonparametric Kruskal–Wallis tests. Mann–Whitney U test was performed to reveal potential differences in biomechanical properties among the different tissues investigated (i.e., vagina, abdominal skin, aponeurosis). p values of <0.05 were considered to be statistically significant.
Results
Tissue samples from the vagina, the abdominal skin, and the aponeuroris were collected from 11 fresh women cadavers without a clinically relevant POP. The mean age was 78.5 (range, 61–87) years. The 11 cadavers were homogenous regarding their biomechanical properties (all p > 0.05).
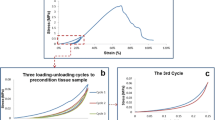
We were able to demonstrate a nonlinear relationship between stress and strain and a hyperelastic behavior (i.e., with large deformation) of the tissues examined (Fig. 2). The tensile strength of the investigated tissues was 0.58 ± 0.07, 0.25 ± 0.04, and 1.25 ± 0.25 MPa for vagina, skin, and aponeurosis, respectively.
Of note, in all 11 cases, mean C0 and C1 values characterizing the biomechanical behavior of the aponeurosis before rupture were remarkably higher than those calculated for the vagina, and the same was true when comparing aponeurosis and skin in 9 out of 11 cases, both for C0 and C1. As expected, the statistical analysis confirmed that these differences were significant (all p < 0.001) (Table 1). In line with these findings, the rupture tests on aponeurosis revealed significantly lower values for the ultimate strain compared to tissue samples derived from the vagina and skin, respectively (all p < 0.01) (Table 1). Thus, the aponeurosis was much more rigid and less extendible than skin regarding low and also large strain levels.
When comparing vaginal tissue and skin, there was no difference with regard to C0 [i.e., low strain levels (p = 0.341)], but a highly significant difference with regard to C1 [i.e., large strain levels (p = 0.005)] (Table 1). The rupture tests revealed a significantly higher ultimate strain for vaginal tissue compared to skin (17% vs. 12%, p < 0.001). Concluding, vaginal tissue was less rigid and significantly more extendible than skin at the level of large strains.
Discussion
In the present study, we were able to demonstrate that the biomechanical properties of vaginal tissue, abdominal aponeurosis, and skin differed significantly. Although at first glance this result might not be surprising, our primary rationale for investigating these tissues was to test if the abdominal wall can be studied to extrapolate the biomechanics of vaginal tissue. This was not the case. The aponeurosis was much more rigid and less extendible compared to skin and vaginal tissue. This was true for low as well as for large strain levels.
We were also able to reveal a significant difference between abdominal skin and vaginal tissue on C1 level. Such large deformations can occur in physiological situations (e.g., delivery or intercourse) or during pathological conditions (e.g., POP). Therefore, the abdominal skin, although easily accessible, does not appear to represent a suitable tool to extrapolate the biomechanical properties of the vagina. In line with this, we found a significantly higher ultimate strain at rupture for vaginal tissue compared to skin. Thus, the vagina was less rigid and significantly more elastic than abdominal skin at large strain levels. However, we were not able to detect a significant difference between skin and vagina on C0 level with our sample size. Despite this, and especially from a mechanical perspective, it is evident that both stress–strain curves are in fact not truly congruent, especially for low strains (Fig. 2). Our study could also be underpowered to detect such a difference on C0 level, and therefore, we might have succumbed a type II error. However, this does not change substantially our conclusion, because even if skin is considered to be up to 5% of strain equivalent to vaginal tissue, the skin parameters would also have to satisfy vaginal behavior in all strains available (i.e., on C1 level, too), and this was virtually not the case.
To date, there are no valid estimations of the strain levels occurring in POP. Parente et al. investigated the effects that the passage of a fetal head can induce on the muscles of the pelvic floor, from a mechanical point of view [14]. The authors were able to show that the maximum deformation obtained was 0.66 for a vertical displacement of the fetal head of approximately 60 mm. However, the biomechanical characteristics in physiological conditions such as intercourse or delivery might be quite different from those in pathological situations like POP. Abdominal skin and aponeurosis taken together cannot be used to extrapolate the biomechanical properties of the vaginal tissue. Therefore, we have to study the biomechanics of the vagina itself. If a noninvasive test is considered in the future, it would be reasonable to develop it for the use in the vaginal cavity, rather than on skin.
Moreover, it becomes clear that a simple transfer of knowledge from the abdominal wall to vaginal reconstructive surgery seems to be inappropriate. In this paradigm, the knowledge of biomechanical properties of normal vaginal tissue may enhance the development of more suitable and “functional” synthetic prostheses designed for use in vaginal reconstructive surgery. Increasing evidence suggests that the concept of the stress transmission at the tissue–implant interface is of outstanding importance [15]. It is characterized by the biomechanical properties of the implant and native surrounding tissue, respectively. A mismatch between both could lead to a disturbed transmission of loads at this interface and thus influence the likelihood of complications, such as erosions or poor clinical results.
We could also demonstrate a nonlinear relationship between stress and strain and a hyperelastic behavior (i.e., with large deformation) of the tissues examined, which was in accordance with our previous data [13]. Interestingly, this kind of nonlinearity has also been observed in experimental results of polypropylene meshes [16]. In this paradigm, we believe that the appropriate mesh is not necessarily the strongest, but one which most closely resembles native human tissue. This has also been supported by the observations of other studies [16–18].
To date, there has been a paucity of literature related to the biomechanical studies of the human vagina [19–23]. Goh revealed age-related changes in full-thickness anterior vaginal wall tissue strips derived from POP surgery [21]. Unfortunately, we cannot comment on age-related effects due to our small sample size and the quite homogenous cohort of cadavers well advanced in years. Lei et al. investigated vaginal tissue derived from surgeries and revealed comparable data to ours with regard to the tensile strength and maximum elongation [23]. On the contrary, the tensile strength of skin for an average adult has typical values in the range of 2.5–16 MPa. It varies among others with site (e.g. sternum, 20 MPa; thigh, 1–5 MPa), main fiber orientation, and age [24]. These values are higher than those found in our study using cadaveric tissue. This applies also for the ultimate strain at rupture, which can reach more than 40% [24]. It is not possible to conclude if these differences are due to age-related changes, the fact of studying cadaveric tissue, or both. However, the comparison with other studies is hampered by the very different methodologies applied to investigate biomechanical properties.
Although the 11 cadavers examined in this study were biomechanically comparable, we could observe a great variability in the C0 and C1 values with a wide interindividual dispersion between minimum and maximum values. We believe that such variations are obviously induced by the physiological differences among women, and therefore, the “unique prosthesis” is propably rather a myth [25]. Also, some of the surgical failures could be attributed to such interindividual differences in tissue biomechanical properties (i.e., tissues of “poor quality”). Cosson et al. pointed to this phenomenon when studying the resistance of vaginal tissue on presurgical samples [26]. However, given our relatively low number of cases, we were not able to account for such interindividual differences by creating different patient groups and establishing a clinically meaningful “mean behavior”.
In addition to a relatively small study group, other potential limitations of this study are that the mechanical properties of the investigated specimen may not be representative of those in the entire structure. Furthermore, we cannot exclude some variability due to minimal variations at the biopsy site. We did not study the certainly much more complex interactions between vaginal tissue, ligaments, fasciae, and muscles. We investigated cadaveric tissue of a population well advanced in years, and post-mortem changes as well as the potential effect of freezing for conservation on the biomechanical properties must be taken into account. Finally, we had no information about the use of hormone replacement therapy. The size of the error introduced by these limitations is unknown. However, these limitations do emphasize the need for in vivo measurement systems.
Our findings clearly demonstrate that vaginal tissue, abdominal skin, and aponeurosis do not exhibit similar biomechanical behavior. Therefore, caution should be exercised when transferring the knowledge derived from abdominal hernial repair to vaginal reconstructive surgery. In the future, further insights into the biomechanical properties of the normal human vagina are warranted, which may lead to the production of more “physiological” and thus functional prosthetics.
References
Luber KM, Boero S, Choe JY (2001) The demographics of pelvic floor disorders: current observations and future projections. Am J Obstet Gynecol 184:1496–1503
Barber MD, Kuchibhatla MN, Pieper CF, Bump RC (2001) Psychometric evaluation of 2 comprehensive condition-specific quality of life instruments for women with pelvic floor disorders. Am J Obstet Gynecol 185:1388–1395
Gabriel B, Denschlag D, Göbel H, Fittkow C, Werner M, Gitsch G et al (2005) Uterosacral ligament in postmenopausal women with or without pelvic organ prolapse. Int Urogynecol J 16:475–479
Gabriel B, Watermann D, Hancke K, Gitsch G, Werner M, Tempfer C et al (2006) Increased expression of matrix metalloproteinase 2 in uterosacral ligaments is associated with pelvicorgan prolapse. Int Urogynecol J 17:478–482
Kerkhof MH, Hendriks L, Brölmann HAM (2009) Changes in connective tissue in patients with pelvic organ prolapse—a review of the current literature. Int Urogynecol J 20:461–474
Alperin M, Debes K, Abramowitch S, Meyn L, Moalli PA (2008) LOXL1 deficiency negatively impacts the biomechanical properties of the mouse vagina and supportive tissues. Int Urogynecol J 19:977–986
Bauer JJ, Salky BA, Gelernt IM (1987) Repair of large abdominal wall defects with expanded polytetrafluoroethylene (PFTE). Ann Surg 206:765–769
Pans A, Albert A, Lapière CM, Nusgens B (2001) Biochemical study of collagen in adult groin hernias. J Surg Res 95:107–113
Afonso JS, Jorge RM, Martins PS, Soldi MD, Alves OL, Patricio B et al (2009) Structural and thermal properties of polypropylene mesh used in treatment of stress urinary incontinence. Acta Bioeng Biomech 11:27–33
Rubod C, Boukerrou M, Brieu M, Dubois P, Cosson M (2007) Biomechanical properties of vaginal tissue. Part 1: new experimental protocol. J Urol 178:320–325
Mooney M (1947) A theory of large elastic deformation. J Appl Phys 1940(11):582–592
Rivlin RS (1948) Large elastic deformations of isotropic materials. I. Fundamental concepts. II. Some uniqueness theorems for pure homogenous deformations. Philos Trans R Soc Lond Ser A: Math Phys Sci A240:459–490
Rubod C, Boukerrou M, Brieu M, Clay J-C, Dubois P, Cosson M (2008) Biomechanical properties of vaginal tissue: preliminary results. Int Urogynecol J 19:811–816
Parente MP, Jorge RM, Mascarenhas T, Fernandes AA, Martins JA (2008) Deformation of the pelvic floor muscles during a vaginal delivery. Int Urogynecol J 19:65–71
Dietz HP, Vancaillie P, Svehla M, Walsch W, Steensma AB, Vancaillie TG (2003) Mechanical properties of urogynecologic implant materials. Int Urogynecol J 14:239–243
Afonso JS, Martins PALS, Girao MJBC, Natal Jorge RM, Ferreira AJM, Mascarenhas T et al (2008) Mechanical properties of polypropylene mesh used in pelvic floor repair. Int Urogynecol J 19:375–380
Neumeyer J, Abdul-Wahab W, Beer M, Speethman J, Groneberg D, Große-Siestrup C (2007) Laboratory testing of suburethral mesh slings: a comparison of their static and dynamic properties. Int Urogynecol J 18(Suppl 1):S111
Krause H, Bennet M, Forwood M, Goh J (2008) Biomechanical properties of raw meshes used in pelvic floor reconstruction. Int Urogynecol J 19:1677–1681
Cosson M, Lambaudi E, Boukerrou M, Lobry P, Crépin G, Ego A (2004) A biomechanical study of the strength of vaginal tissues. Results on 16 post-menopausal patients presenting with genital prolapse. Eur J Obstet Gynecol Reprod Biol 112:201–205
Ettema GJ, Goh JT, Forwood MR (1998) A new method to measure elastic properties of plastic–viscoelastic connective tissue. Med Eng Phys 20:308–314
Goh JT (2002) Biomechanical properties of prolapsed vaginal tissue in pre- and postmenopausal women. Int Urogynecol J 13:76–79
Martins P, Pena E, Calvo B, Doblare M, Mascarenhas T, Jorge RN et al (2010) Prediction of nonlinear elastic behaviour of vaginal tissue: experimental results and model formulation. Comput Methods Biomech Biomed Eng. doi:10.1080/10255840903208197
Lei L, Song Y, RiQi C (2007) Biomechanical properties of prolapsed vaginal tissue in pre- and postmenopausal women. Int Urogynecol J 18:603–607
Haut RC (2002) Biomechanics of soft tissue. In: Nahum AM, Melvin JW (eds) Accidental injury. Biomechanics and prevention. Springer, New York, pp 236–238
Cosson M, Debodonance P, Boukerrou M, Chauvet MP, Lobry P, Crépin G et al (2003) Mechanical properties of synthetic implants used in the repair of prolapse and urinary incontinence in women: which is the ideal material? Int Urogynecol J 14:169–178
Cosson M, Boukerrou M, Lambaudie E, Lobry P, Crépin G, Ego A (2003) Biomécanique de la réparation et résistance des tissus biologiques dans les cures de prolapsus: pourquoi utiliser des prothèses? J Gynécol Obstét Biol Reprod 32:329–337
Acknowledgments
BG was awarded an International Fellowship grant by the International Urogynecological Association (IUGA) in 2009, which partly funded this research project, and received also a grant for basic research from the Ministry of Health of the Czech Republic (No. 9299-3/2007). BG thanks Klaus Gabriel for the support with general mechanics understanding. The authors announce an unconditioned financial support of basic research by ETHICON Women’s Health & Urology.
Conflicts of interest
MC is a consultant of ETHICON Women’s Health & Urology.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Gabriel, B., Rubod, C., Brieu, M. et al. Vagina, abdominal skin, and aponeurosis: do they have similar biomechanical properties?. Int Urogynecol J 22, 23–27 (2011). https://doi.org/10.1007/s00192-010-1237-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-010-1237-7