Abstract
The authors review the literature concerning all types of synthetics implants used in prolapse repair or the treatment of stress urinary incontinence, and analyze the mechanical properties of and the tolerance to the various products used. Various synthetic implants are also studied, including their advantages and disadvantages, as well as outcome following implantation and tolerance by the host, with respect to the type of product and the type of intervention. A review of current implant products demonstrated that the perfect product does not exist at present. The most promising of theses products for applications in transvaginal surgery to restore pelvic function appears to be the synthetic prostheses made predominantly of polypropylene, which offer mechanical properties of durability and elasticity. Their properties of resistance are undisputed, but it remains to be shown whether they are well tolerated when inserted by the vaginal route. The technical modalities for their use are still under evaluation, which should enable a better identification of the respective indications for these products in prolapse repair and treatment of urinary incontinence by the vaginal route.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
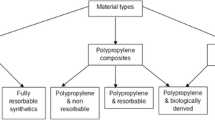
The tissues of patients suffering from disturbances of pelvic function are often structurally altered, particularly with respect to the properties of their collagen [1, 2, 3, 4]. There is therefore a great temptation to use reinforcing materials during surgical treatment of genital prolapse and stress urinary incontinence. Until now, the majority of observations on synthetic prostheses have come from the field of reconstructive surgery of the abdominal wall and the repair of groin hernias [1, 5, 6, 7, 8]. In about the last 20 years, implants have been used in gynecology for transabdominal prolapse repair and in urinary incontinence, in the form of suburethral slings [9, 10, 11, 12]. More recently, the unresolved problem of the treatment of cystocele has led surgeons to try to use these materials by the vaginal route, even though it is reputed to carry a risk of infection [13, 14, 15]. In this review, we assess the different materials and their respective advantages and disadvantages. Many products of biological and synthetic origin have been proposed for this application. We discuss synthetic materials, describing their composition and their mechanical properties when such data were available. We also address the outcome after implantation, dealing with their biomechanical properties as well as how well they were tolerated.
Many techniques has been described using autologous tissues, such as urinary slings made of fascia lata taken from the thigh, or techniques using vaginal tissue for cystocele repair [16, 17, 18, 19]. The latter has esthetic drawbacks and only a limited amount of tissue can be taken. For these reasons and for ease of use, most tissues are of heterologous human origin, such as cadaveric dermis patches or dura mater. We will not discuss dura implants mater further, because although they are well tolerated and their mechanical properties are quite satisfactory, concerns about viral safety now preclude their use, owing to the risk of transmission of Creutzfeld–Jakob disease. As we focus on synthetic protheses nor will we discuss the use of cadaveric dermal allograft, marketed, for example, under the name of Repliform (Microinvasive/Boston Scientific), and also implantable collagens of animal origin such as Pelvicol.
In this first section we will discuss the properties of absorbable synthetic mesh and in the second the non-absorbable prostheses.
Absorbable synthetic prostheses
There is a real temptation to use absorbable prostheses to reinforce surgery for prolapse. These implants cannot undergo secondary rejection and their presence favors postoperative fibroblast activity. Unfortunately, several studies have cast doubts on this enthusiasm [20, 21, 22, 23, 24, 25, 26]. The most commonly used absorbable prostheses are Dexon (polyglycolic acid) and Vicryl (polyglactic acid).
The absorption of absorbable prostheses should be slow. The absorption of Vicryl starts at the beginning of the third week. After 30 days only a few elements remain, with no mechanical value. Absorption of the mesh occurs as a result of the action of macrophages, and it is replaced by healthy scar tissue. The absorption products are recycled into new collagen fibers [20]. Dexon takes 90 days to be absorbed. The scar tissue is not as strong as was the reinforced tissue, and alone is insufficient to provide the strength of the structure. Absorbable prostheses are not threatened by infection, owing to their ephemeral nature. They are not harmful to the viscera. A study by Lamb in 1983 [21] demonstrated that the fibrous reaction was insufficient before the absorption of the implant. Tyrell [22] created and repaired a ventral lesion in rabbits, and secondary hernia was noted in the 40 rabbits treated with absorbable prostheses. Rath [23] confirmed these results using Vicryl implants in rabbits. A further study by Brenner in 1994 [24] also confirmed these findings. However, two randomized trials were recently published in 2001, concerning the use of absorbable prostheses for cystocele repair by the vaginal route. The first was a study published in June 2001 by Sand [25]. This involved 161 randomly selected patients who had undergone transvaginal prolapse repair by colporrhaphy and colpectomy, assessed 1 year postoperatively. One year after the intervention, 43% of the patients without implants had a recurrent cystocele reaching at least halfway to the hymeneal ring, as opposed to 25% when an absorbable prosthesis had been implanted. Eight women with no implant and two with implants had recurrent cystoceles affecting the hymeneal ring. When a subvesical absorbable prosthesis was implanted, the authors noted significantly fewer cystocele recurrences. However, they noted 13 cases of recurrent rectocele, with no difference observed between the two groups. Questions remain about these results, given the subjective, debatable judgment criterion that exists for defining cases of moderate cystocele. The short postoperative follow-up was also a limitation. Finally, the rate of recurrence in both groups was high and ought to raise questions about the use of colporrhaphy without suspension. The second study, by Weber [26], published in December of the same year, involved 109 patients undergoing an anterior colporrhaphy for vaginal prolapse who were randomized into three groups, corresponding to three different surgical techniques. The first group (G1) received the standard technique with simple colporrhaphy. In the second group (G2), a polyglactin mesh was used in conjunction with the standard technique. Finally, an ultralateral anterior colporrhaphy was performed on the third group (G3). The outcome was assessed after about 2 years. The subjective and objective results were good in 30% of the cases in group G1, 42% in G2 and 46% in G3. Statistically there was no significant difference between the three groups and the presence of an implant did not significantly reduce the rate of recurrence. These results highlight, if that were still necessary, the poor results obtained in prolapse repair by simple excision and tightening of the excess vaginal tissue without suspension.
It appears from the literaturethat the implantation of absorbable prostheses for prolapse repair by the vaginal route, based on both animal studies and clinical results, is unfavorable.
Non-absorbable synthetic prostheses
We will quickly retrace the development and history of prosthetic materials, their properties and the experience of their use in gynecologic surgery.
A history of prosthetic materials:
Phels was the first to use metallic silver meshes in 1894. The concept was subsequently developed by a German surgeon, Witzel, in 1900, and exported to the USA from 1903 [5]. This mesh corroded rapidly on contact with tissue fluids [6]. Other metallic meshes have been developed, such as tantalum in 1940 [6] and stainless steel in 1952 [7, 8]. The results appeared encouraging but complications led to the development of new materials.
Non-metallic synthetic meshes have been developed, such as Fortisan cellulose, which was more malleable and economical, and allowed good infiltration by host tissue, but was rapidly shown to be a source of infection and fistulae. Polyvinyl sponge (Ivalon, 1949) is a polymer of polyvinyl alcohol in its formaldehyde form, in which air is blown through a liquid plastic to form a solid with the appearance in cross-section of a slice of bread, but it was poorly tolerated during infection and had a tendency to dissolve and fragment with time.
Developed in 1938 by the firm Dupont de Nemours, nylon became a successful product after the second world war, during which it had been mostly used to make powder bags for the US Navy and parachute cloth. It was first used surgically as Crinoplaque [27], which was woven from a tubular monofilament. Later, interlock knitted nylon was used, resulting in a mesh that does not fray and which can thus be cut with scissors. This nylon product, although better, exhibited progressive alteration in situ and was superseded by other polymers.
Silastic is a polymer comprising a Dacron or nylon mesh sandwiched between two sheets of silicone. It was used predominantly in temporary surgery for congenital defects. In 1964, Gibson [28] reported 50% parietal complications with polytetrafluoroethylene (PTFE, Teflon). Carbon fibers were developed from 1980, but have in fact been little used. A composite made by immersing carbon fibers into a solution of dilute chloroform-treated polyglactic acid allowed better biocompatibility to be attained. Its durability is identical to that of polypropylene.
More recently we find polyester mesh – Dacron. The word Dacron in fact designates a variety of products composed of a saturated polyester, polyethylene terephthalate (PETP) [29]. Dacron appeared in 1956 and is also known as Mersilene (Mersuture) when knitted and Ligatene when woven. During the last 40 years Dacron mesh has been the most popular and most used non-metallic mesh, but currently its use is declining. During the 1970s the use of a silicone–velour prosthesis, the Rhodergon patch [29], rapidly failed because its impermeability rendered it unsuitable for the parietal environment. This product should not be confused with Rhodergon 8000 mesh, which is made of polyester supplemented with a felt, giving it the appearance of an inextensible patchbut which is permeable.
In 1958, Usher [30] introduced Marlex, made by weaving a single monofilament of polypropylene. It was so popular that from 1962, 20% of hernias in the USA were being treated with Marlex mesh. However, it was associated with abdominal sepsis, especially exudative sepsis. Additional complications were exposure of the implant (44%) and digestive fistulae (23%), and these resulted in the material being abandoned. Prolene, an equivalent product made with two filaments, and the multifilament Surgipro, gave good overall results with minimal complications.
Gore-Tex (expanded polytetrafluoroethylene: ePTFE) is a sort of Teflon, transformed by a procedure of expansion (discovered in 1963 in Japan) which renders it microporous and gives it the ability to integrate into the tissue in a way that Teflon does not. Gore-Tex is supposed to be incorporated more rapidly and with minimal inflammatory reactions and few adhesions. It is currently widely used in parietal surgery, notably in surgery of a provisional nature, such as in laparoschisis.
Classification of biomaterials
The prevention of complications requires in-depth knowledge and understanding of the physical properties of the implants, of which porosity and pore size are of supreme importance [31]. The classification system devised by Amid is currently the standard.
-
Type I: Completely macroporous mesh (Atrium, Marlex, Prolene and Trelex). The pore size exceeds 75 μm, the size required for infiltration by macrophages, fibroblasts, blood vessels in angiogenesis and collagen fibers.
-
Type II: Totally microporous mesh (Gore-Tex, surgical membranes). The pore size is smaller than 10 μm in at least one dimension.
-
Type III: Macroporous patch, with multifilaments or a microporous component: PTFE (Teflon), woven Dacron (Mersilene), woven polypropylene (Surgipro), perforated PTFE (Mycro Mesh).
-
Type IV: Biomaterials with submicronic pores (Silastic, Cellgard, dura mater substitute). These materials are often associated with those of type I to prevent adhesion in intraperitoneal implantation.
Implant structures
The principal synthetic implants used at present have the following structures:
-
They are made of polyester, PTFE, polypropylene, polyethylene and nylon.
-
Their mechanical properties depend on the structure of the fabric and the thread.
-
Woven (Fig. 1): plain, twill or satin weave. Their advantages are strength and good memory. Their disadvantages are fraying and poor conformity.
-
Knitted (Fig. 2): warp-knit, interlock and circular-knit. These fabrics are flexible on manipulation, versatile, and have high conformity.
-
The unwoven materials are absorbed well, but have no conformity, are poorly visible, and demand a higher level of treatment.
-
Composite fabrics have two surfaces, one of which prevents adhesion and synergistically enhances the properties of each element, but they are rigid and poorly visible.
-
They can have holes, be kidney-shaped, umbrella-shaped or in the form of a plug.
-
The fiber structure (Fig. 3) can comprise a monofilament or multifilament, can be twisted, coated (by one or two layers), braided and double braided.
Mechanical properties
These properties are directly dependent on the type of thread and the knitting method used in the implant. There are no recommendations concerning the resistance or elasticity of implants used in hernia or prolapse surgery. The information provided by manufacturers is incomplete, so we refer to the results of a study performed in collaboration with the engineering department of the ICAM (Institut Catholique des Arts et Métiers) at Lille, into the mechanical characteristics and ease of use of the main implants marketed for prolapse repair.
The prostheses tested were as follows (Table 1):
-
Biogyn A1: small square mesh, thread twisted in one direction, composed of aligned filaments.
-
Biogyn IT: large rectangular mesh, one thread composed of aligned monofilaments and one twisted warp thread.
-
Biogyn W8: diamond-shaped mesh in an unwoven matrix, created by thermodiffusion of small diamond shapes measuring 10 × 9 tenths of a millimeter.
-
Mersuture: diamond-shaped mesh measuring 23 tenths of a millimeter in length and 11 tenths of a millimeter in width. Triple knot at each intersection.
-
Prolene: interlock knit of a monofilament, with additional links to the stitch plus two links between each knot and a peripheral knot.
The mechanical properties are reported in Table 2. The results are slightly different from those found in the literature, which is explained by the difference in the sizes of the sample of the materials tested and the speed of traction used on the implants (Table 3). Overall, the measurements corresponding to breakage are high, even though the Biogyn W8, Vypro and Mersuture TS are less resistant. Prolene, Biogyn A1 and Biogyn IT are the strongest, so they should be recommended for normal use, although it is also important to take into account their ease of use and implantation, as well as whether they are tolerated by the host. Some implants gave very different values lengthwise and widthwise, as was observed with Vypro, Prolene and Biogyn A1, whether in terms of resistance to breakage or elasticity. However, these properties are clinically unjustifiable, as the resistance for prolapse repair is not always orientated in space in a schematic fashion, particularly in the case of repair by the vaginal route. Some of the results for lengthwise or widthwise stretching prior to breaking are equally surprising for the function for which these products are intended.
Similarly, Brenner [24] reported a maximal vertical resistance of Marlex of 152.7 N and of 245.9 N for Prolene, and a transversal resistance of 90.1 N and 188 N, respectively.
Biological properties
The reaction of the soft tissues to implanted biomaterials is variable. Williams [32] identified four types of response:
-
A minimal response, with a thin layer of fibrosis around the implant.
-
A chemical response, with a severe and chronic inflammatory reaction around the implant.
-
A physical response, with an inflammatory reaction to certain materials and the presence of giant cells.
-
Necrotic tissue: a layer of necrotic debris is produced, resulting from in situ exothermic polymerization.
The first type of response consists essentially of normal scar formation at a wound, in which a thin layer of fibrosis isolates the implant from surrounding tissue. PTFE, polyethylene and silicone patches produce this reaction. PP, PGA, PETP and PTFE have good biocompatibility properties. For example, PTFE has a low critical surface tension, which prevents the attachment and propagation of cell growth, thereby limiting cell penetration into the pores of the knitted structure. Conversely, PETP and PGA, which have numerous ester groups, provoke an acute thrombotic response that encourages fibroblastic cells to attach and proliferate the length of the filamentous surfaces. PP results in a less acute cellular response than PETP and is therefore recommended for reinforcement of the inguinal canal, or for covering sandwiched peritoneum in the repair of incisional hernias. PP mesh is not recommended for integrated implants because of the elevated risk of visceral adhesions in the abdominal cavity.
Kaupp [33] described a histological reaction in four stages:
- Stage 1:
-
In the first week, the symptomatology comprised an intense inflammatory infiltrate around the implant, capillary proliferation, granular tissue and the presence of giant cells containing birefringent material.
- Stage 2:
-
After 2 weeks the granular tissue remained and histiocytes had appeared, with more or fewer giant cells.
- Stage 3:
-
After 4 weeks the acute inflammation had disappeared, capillaries were reduced, and the number of histiocytes and giant cells had increased.
- Stage 4:
-
Some giant cells were present on the external surface of the implant and a dense, fibrous tissue was present.
The reduced inflammatory reaction provoked by the non-absorbable parietal implant was a sign of its being well tolerated by the host, and the intense fibroblastic reaction showed that it was becoming integrated into the surrounding tissue. Under normal conditions the inflammatory reaction, initially an exudate, then cellular, starts on day 3 and the fibroblastic reaction which supersedes it and colonizes the implant begins around day 10 [34]. The relationship between the numbers of inflammatory cells and fibroblastic cells allows a simultaneous evaluation of the mechanical value and the biological tolerance of the implant by the host [35]. A Dacron mesh implant is completely colonized and integrated into the abdominal wall after 4–6 weeks [35]. It is important to note that the critical period for the stability of a parietal implant, just as for the strength of a parietal stitch, is between days 7 and 10. The strength of a prosthesis increases with time: in an animal study it doubled between weeks 3 and 12 for PP or PTFE [36]. The major risk is an early infection. Butha [37] has shown non-infected collections around Dacron velour implants, suggestive of an allergic reaction, but this theory cannot explain why the rejection is not always bilateral. Kaupp [33] claimed that periprosthetic reactions are not due to infection, but showed macroscopic features compatible with an immunological reaction. De Clerk [38] accepted the theory of delayed hypersensitivity and foreign body reaction in the host suggested by Kaupp [33], as he observed an improvement under cyclophosphamide. This immunologic mechanism is difficult to prove, because no test exists and one cannot discriminate histologically between an immunologic reaction and a simple reaction to a foreign body. Studies by Katz [39] have addressed the concept of the hydrophobicity of biomaterials and showed its influence on bacterial adhesion. These properties can also influence the dynamics of absorption and resorption of the organisms on the surface of synthetic materials. Bacterial adhesion is initially a reversible process, and becomes irreversible when the bacteria create an extracellular adherence.
On removal of 18 implants, Klinge [40] noted the presence of 32% inflammatory cells in PP meshes, 12% for those made of ePTFE, 8% for polyester and 7% for reinforced PP. He also noted the presence of macrophages at the interface between the tissue and the PP (45%), polyester (45%), ePTFE (25%) and reinforced PP (22%).
Complications in hernia surgery
Infection
When the size of the pores or gaps in the mesh are less than 10 μm in each of their three dimensions, bacteria, which measure around 1 μm, cannot be eliminated by macrophages and neutrophils because they are too big to enter the pores. Meshes of types II and III are vulnerable to infection because they may harbor bacteria and allow them to proliferate. Type I implants, on the contrary, although they can be a refuge for bacteria, also admit macrophages and especially fibroblasts and angiogenesis, thus preventing infiltration by and the development of germs. Chronic infections occurring with materials of type I are mostly due to the use of multifilament stitches for attaching the mesh (10%–50%). In the case of infection, removal of the implant is not necessary for type I materials, whereas it should be completely removed if using type II and partially removed in the case of type III materials [41, 42].
Exudation
This is caused by an inflammatory reaction of the host to the implant, and the space between the two. The quicker fibrin is fixed to the implant, the quicker the space is filled and the less this phenomenon appears. When the mesh is not in direct contact with subcutaneous fat, but in a retromuscular or subaponeurotic position, this phenomenon is absent.
Intestinal adhesions
These only occur with type I meshes in direct contact with the intestine [43].
Erosions of the hollow viscera and fistulae
This too is a complication of type I materials in contact with organs with or without a serous membrane. This phenomenon is not reduced by using absorbable materials [43].
Retraction
Prosthetic plugs can retract to as much as 75% of their original size. This therefore predisposes to recurrence. Meshes retract during scar formation by about 20%–30% of their surface [44].
The use of meshes in gynecology
The majority of articles refer to the use of meshes in gynecologic surgery over the last 30 years. These implants have been used principally for transabdominal prolapse repair (sacrocolpopexy) and for suburethral slings. Table 4 summarizes the articles with respect to the materials used for these two interventions.
Transabdominal prolapse surgery, notably promontory fixation, has resulted in little or no intolerance. A few cases have been mentioned in the literature [60]. Numerous articles discuss slings inserted by a mixed vaginal and abdominal route, with vaginal and subpubic scarring (Table 4). Very few report on surgery that is exclusively transvaginal. Most frequently they discuss interventions to provide support, as described by Mouchel [56, 57]. In a review of the literature from 1950 to 1996, Iglésia [71] collated 21 retrospective, non-randomized studies using slings and 15 sacrocolpopexies using synthetic material. The slings had been removed in 35% of cases and fistulae were noted in 10%. Promontory fixation resulted in erosions in 9% of cases.
The most frequent symptoms [55] were pain, vaginal discharge, bleeding, induration of the abdominal scar, granuloma of a vaginal scar, abdominal or vaginal fistulae, failure of scar formation and expulsion of the implant.
Many implant rejections occur during the first year, but the period of follow-up is not often long. This may explain the low percentage of rejections reported in certain publications (0%–39.8%; Table 4) following interventions by the vaginal route or both routes.
Norris [59] claims that the smaller the surface of the implant, the fewer intolerance reactions observed. He noticed that the surface area of the synthetic material that he used (10.5 cm2) led to six times less rejection than reported by Bent [61] using patches measuring 60 cm2. This suggests a reaction proportional to the area of contact with the foreign body. Our experience has indicated the same phenomenon [57]. The area of contact between the foreign substance and the exposed tissue is an important determinant of the tissue reaction [72]. One can therefore say that tolerance to the synthetic material is proportional to the exposed surface area and the distance that separates it from the vaginal scar.
TVT (Tension-free Vaginal Tape) should be discussed separately, even though it could be integrated into a sling intervention. The remarkable tolerance of this Prolene strip is confirmed in the literature, with very few rejections reported.
Defects of scar formation are reported in 0.5%–2% of observations [73, 74]. Nilsson [75] describes a case of sepsis of the vaginal wound. Usually this is corrected by debriding the scar, minimal resection and a new suture under antibiotic treatment. Tamussino [76] has described the Austrian registry of 7000 TVT operations and reported no cases of intolerance. This technique is minimally invasive and seems perfectly well tolerated, owing to the small vaginal incision and protection of the strip by plastic-coated sheaths during its insertion.
The problem of transvaginal prolapse repair, notably for cystocele, remains to be discussed. Meshes have been introduced by the abdominal route since the 1970s, but the use of the vaginal route has been much more recent and the the results have only been described during the last decade. Table 5 summarizes the experience of synthetic mesh in prolapse repair, and especially for cystoceles, by the vaginal route. PP is the most frequently used material, and the phenomenon of intolerance is marked by erosions. Delayed scar formation and erosions were present in about 6% of cases (2%–12%). In rare cases, complete removal of the mesh was necessary. Partial resection and local treatment were sufficient and did not compromise the anatomic result.
Conclusion
In the 1950s, Cumberland [27] and Scales [28] developed eight criteria for the ideal prosthesis. The material:
-
Must not be physically modified by tissue fluids;
-
Must be chemically inert;
-
Must not induce an inflammatory reaction or antibodies;
-
Must not be carcinogenic;
-
Must not induce allergy or hypersensitivity;
-
Must be able to resist mechanical stress;
-
Must be able to be manufactured in the required shape;
-
Must be able to be sterilized;
Three criteria should be added:
-
Resistance to infection;
-
Prevention of adhesion at the surface in contact with viscera; and
-
Better in vivo response than autologous tissue.
This review of existing prosthetic products demonstrates that no perfect product currently exists. Two categories of product seem to us to have promising properties with regard to their use in transvaginal surgery for restoring pelvic function. On the one hand are synthetic implants with mechanical properties of strength and elasticity, essentially made of polypropylene. Their strength is unchallenged, but it remains to be established whether they are well tolerated when introduced by the vaginal route. On the other hand are animal collagen implants, which appear to be well tolerated, but these require clinical validation for this indication. The technical modalities for use are still in the process of validation and should allow a better understanding of the respective indications of these products in the correction of prolapse or urinary incontinence by the vaginal route.
Abbreviations
- PP:
-
Polypropylene
- PGA:
-
Polyglycolic acid
- PETP:
-
Polyethylene terephthalate
- PTFE:
-
Polytetrafluoroethylene
- TVT:
-
Tension-free vaginal tape
References
Pans A, Albert A, Lapière CM, Nusgens B (2001). Biochemical study of collagen in adult groin hernias. J Surg Res 95:107–113
Ulmsten U, Ekman G, Giertz G, Malmstrom A (1987) Different biochemical composition of connective tissue in continent and stress incontinent women. Acta Obstet Gynecol Scand 66:455–457
Gilpin SA et al. (1989) The pathogenesis of genitourinary prolapse and stress incontinence of urine. A histological and biochemical study. Br J Obstet Gynaecol 96:15–23
Norton P et al. (1992) Abnormal collagen ratio in women with genitourinary prolapse. Neurourol Urodyn 11: 2–4
Witzel O (1900) Ueber den Verschluss von Bauchwunden und Bruchpforten durch versenkte Silberdrachtnetze. Centralbl Chir Leipz 27:257
Bauer JJ, Salky BA, Gelernt IM (1987) Repair of large abdominal wall defects with expanded polytetrafluoroethylene (PTFE). Ann Surg 206:765–769
Babcock WW (1952) The range of usefulness of commercial stainless steel cloths in general and special forms of surgical practice. Ann West Med Surg 6:15
Goepel R (1928) Der Verschluss von Nabel und Bauchwand hernien unter Verwendung gegliederten Silberdrahtnetze. Münch Med Webnsch 75:127
Morgan JE (1970) A sling operation, using Marlex polypropylene mesh, for treatment of recurrent stress incontinence. Am J Obstet Gynecol 106:369–377
Iosif CS (1993) Abdominal sacral colpopexy with use of synthetic mesh. Acta Obstet Gynecol Scand 72:214–217
Nichols DH (1973) The Mersilene mesh gauze-hammock for severe urinary stress incontinence. Obstet Gynecol 41: 88–93
Stanton SL (1985) Silastic sling for urethral sphincter incompetence in women. Br J Obstet Gynaecol 92:747–750
de Tayrac R, Gervaise A, Fernandez H (2001) Cystocele repair with a fixation-free prosthetic polypropylene mesh. Int Urogynecol J 12 (suppl 3):S92.
Sarsotti C, Lamm M, Testa R (2001) rectocele repair using a prolene mesh in patients with defecatory outlet obstruction. Int Urogynecol J12 (suppl 3):S82
Sarsotti C, Ubertazzi E, Lamm M, Tidone C, Pruneda Paz J, Terta R (2001) The use of heterologous meshes for rectocele repair. Int Urogynecol J12 (suppl 3):S158.
Oliver RF, Grant RA, Kent CM (1972) The fate of cutaneously and subcutaneously implanted trypsin purified dermal collagen in the pig. Br J Exp Pathol 53 :540–549
Chvapil M (1980) Reconstituted collagen. In :Viidick A, Vuust J, eds. Biology of collagen. New York: Academic Press, 1980; 313–323
FitzGerald MP, Mollenhauer J, Brubaker L (2000). The fate of rectus fascia suburethral slings. Am J Obstet Gynecol 183:964–966
Walter AJ, Morse AN, Leslie K, Zobitz M, Hentz JG, Cornella JL (2001) Changes in tensile strength of cadaveric human fascia lata following implantation in a rabbit vagina model. Abstract 43. AUGS Meeting Hilton Head, 18–21 September .
Levasseur JC, Lehn E, Rignier P (1979) Etude expérimentale et utilisation clinique d'un nouveau materiel dans les eviscerations graves post-operatoires. Chirurgie 105 :577–581
Lamb JP, Vitale T, Kamenski DL (1983) Comparative evaluation of synthetic meshes used for abdominal replacement. Surgery 93 :643–648
Tyrell J, Silberman H, Chandrasoma P, Niland H (1989) Absorbable versus permanent mesh in abdominal operations. SGO 168 :227–233
Rath AM, Zhang J, Amouroux J, Chevrel J (1996) Les prothèses pariétales abdominales. Etude biomécanique et histologique. Chirurgie 121:253–265
Brenner J. Mesh materials in hernia repair. In: Schumpelick V, Wantz GE, eds. Inguinal hernia repair. Expert Meeting on Hernia Surgery, St Moritz, 1994. Basel: Karger, 1995;172–179
Sand PK, Koduri S, Lobel RW et al. (2001) Prospective randomized trial of polyglactin 910 mesh to prevent recurrence of cystoceles and rectoceles. Am J Obstet Gynecol 184:1357–1364.
Weber AM, Walters MD, Piedmonte MR, Ballard LA (2001) Anterior colporrhaphy: a randomized trial of three surgical techniques. Am J Obstet Gynecol 185:1299–1306
Acquaviva D.E, Bourret P (1948) Cure des éventrations par plaques de nylon. Press Med 73 :892
Gibson LD, Stafford CE (1964) Synthetic mesh repair of abdominal wall defects. Am Surg 30:481
Meyer Ch, Alexiou D, Calderoli H, Hollender LF (1977) Les matériaux de synthèse dans la cure des grandes éventrations abdominales. Enseignements à propos de 78 observations. Ann Chir 31:221–228
Usher FC, Ochsner J, Tuttle LLD Jr (1958) Use of Marlex mesh in the repair of incisional hernias. Am Surgeon 24:969
Amid PK (1997) Classification of biomaterials and their related complications in abdominal wall hernia surgery. Hernia 1:15–21
Williams DF (1973) The response of the body environment to implants. In: Williams DF, Roaf R, eds. Implants in surgery. Philadelphia: WB Saunders 203–297
Kaupp HA, Matulewicz TJ, Lattimer GL (1979) Graft infection or graft reaction ? Arch Surg 114:1419
Petit J, Stoppa R, Baillet J (1974) Evaluation expérimentale des réactions tissulaires autour des prothèses de la paroi en tulle de Dacron en fonction de la durée d'implantation et du siège en profondeur. J Chir 107:667–672
Adloff M, Arnaud J-P (1976) Etude expérimentale de la résistance et de la tolerance biologique de matériaux prothétiques utilisés dans la réparation des pertes de substance de la paroi abdominale. Chirurgie 102:390–396
Lamb J.P, Vitale T, Kminski DL (1983) Comparative evaluation of synthetic meshes used for abdominal wall replacement. Surgery 93:643–648
Bhuta I, Dorrough R (1981) Noninfectious fluid collection around velour Dacron graft: Possible allergic reaction. South Med J 74:870
De Clerck LS, Houuthooft D, Vermeylen J, De Schepper A, Stevens WJ (1990) Delayed reaction to a Dacron velour bypass graft. J Cardiovasc Surg 31:124–126
Katz S, Izhar M, Mirelman D (1981) Bacterial adherence to vascular prostheses. A determinant of graft infectivity. J Vasc Surg 194:35–41
Klinge U, Klosterhalfen B, Müller M, Schumpelick V (1999) Foreign body reaction to meshes used for the repair of abdominal wall hernias. Eur J Surg 165 :665–673
Capozzi JA, Berkenfield JA, Cheaty JK (1988) Repair of inguinal hernia in the adult with prolene mesh. Surg Gynecol Obstet 167:124–128
Stoppa RE, Rives JL, Warlaumont CR (1984) The use of Dacron in the repair of hernias of the groin. Surg Clin North Am 64:269–285
Soler M, Verhaeghe P, Esssomba A, Sevestre H, Stoppa R (1993) Treatment of post operative incisional hernias by a composite prosthesis. Clinical and experimental study. Ann Chir 47:598–608
Amid PK, Shulman AG, Lichtensten IL (1972). A simple staping technique for the prosthetic repair of massive incisional hernias. In: Arregui ME, Nagan RF (eds) Inguinal hernia advances or controversies? Radcliffe Medical Press, Oxford, pp 511–514
Bryans FE (1979) Marlex gauze hammock sling operation with Cooper's ligament attachment in the management of recurrent urinary stress incontinence. Am J Obstet Gynecol 133:292–294
Morgan JE, Farrow GA, Stewart FE (1985) The Marlex sling operation for the treatment of recurrent stress urinary incontinence. Am J Obstet Gynecol 151:224–226
Drutz HP, Buckspan M, Flax S, Mackie L (1990) Clinical and urodynamic re-evaluation of combined abdovaginal Marlex sling operation for recurrent stress urinary incontinence. Int Urogynecol J 1:70–73
Kersey J (1983) The gauze hammock sling operation in the treatment of stress incontinence. Br J Obstet Gynaecol90:945–949
Iosif CS (1985) Sling operation for urinary incontinence. Acta Obstet Gynecol Scand 64:187–190
Young SB, Rosenblatt PL, Pingeton DM (1995) The Mersilene mesh suburethral sling: a clinical and urodynamic evaluation. Am J Obstet Gynecol 173:1719–1726
Addison WA, Livengood CH, Sutton GP, Parker RT (1985) Abdominal sacral colpopexy with Mersilene mesh in the retroperitoneal position in the management of post hysterectomy vaginal vault prolapse and enterocele. Am J Obstet Gynecol 153: 140–146
Creighton SM, Stanton SL (1991) The surgical management of vaginal vault prolapse. Br J Obstet Gynaecol 98:1150–1154
de Vries MJ, van Dessel TH, Drogendijk AC (1995) Short-term results and long-term patients'appraisal of abdominal colpo-sacropexy for treatment of genital and vaginal vault prolapse. Eur J Obstet Gynecol Reprod Biol 59:35–38
Summit RL, Bent AE, Ostergard DR (1992) Suburethral sling procedure for genuine stress incontinence and low urethral cloture pressure. A continued experience. Int Urogynecol J 3:18–21
Bent AE, Ostergard DR, Zwick-Zaffuto M (1993) Tissue reaction to expanded polytetrafluoroethylene suburethral sling for urinary incontinence: clinical and histologic study. Am J Obstet Gynecol 169:1198–204
Mouchel J (1990) Traitement chirurgical de l'incontinence d'urine à l'effort chez la femme par soutènement sous-urétral à l'aide d'une bandelette de polytétrafluoroéthylène; à propos de 95 observations. Rev Fr Gynecol Obstet 85:399–406
Debodinance P, De Bièvre P, Parmentier D, Dubrulle R, Querleu D. Crepin G (1994) Les 'aléas' de l'utilisation d'une fronde de Gore-Tex dans le traitement de l'incontinence urinaire d'effort. J Gynecol Obstet Biol Reprod 23:665–670
Weinberger MW, Ostergard DR (1995) Long-term clinical and urodynamic evaluation of the polytetrafluoroethylene sling for treatment of genuine stress incontinence. Obstet Gynecol 86:92–96
Norris JP, Breslin DS, Staskin DR (1996) Use of synthetic material in sling surgery: A minimal invasive approach. J Endourol 10:227–230
Snyder TE, Karantz KE (1991) Abdominal retroperitoneal sacral colpopexy for correction of vaginal prolapse. Obstet Gynecol 77:944–949
Van Lindert ACM, Groenendijk AG, Scholten PC (1993) Surgical support and suspension of genital prolapse, including preservation of the uterus, using Gore-Tex soft tissue patch: a preliminary report. Eur J Obstet Gynecol Reprod Biol 50:133–139
Valailas SR, Stanton SL (1994) Sacrocolpopexy: a retrospective study of a clinician's experience. Br J Obstet Gynaecol 101:518–522
Korda A, Peat B, Hunter P (1989) Experience with silastic slings for female urinary incontinence. Aust NZ Obstet Gynaecol 29:150–154
Richardson DA, Bent AE, Ostergard DR, Cannon D (1984) Delayed reaction to the Dacron buttress used in urethropexy. J Reprod Med 3:689–392
Errando C, Batsta JE, Arano P (1996) Polytetrafluoroethylene sling for failure in female stress incontinence surgery. World J Urol 14:S48–S50
Debodinance P, Cosson M, Burlet G (1999) Tolerance of synthetic tissues in touch with vaginal scars: review to the point of 287 cases. Eur J Obstet Gynecol Reprod Biol 87:23–30
Kolmorgen von K, Havenmann O, Siegel W (1980) Duraschingenoperationen und deren Ergebnisse bei der operativen Harninkontinentzbehandlung der Frau. Zbl Gynäkol 102:850–856
Backer KR, Beresford JM, Campbell C (1990) Colposacropexy with Prolene mesh. Surg Gynecol Obstet 171:51–54
Fianu S, Sodeberg G (1983) Absorbable polyglactin mesh for retropubic sling operations in female urinary stress incontinence. Gynecol Obstet Invest 16:45–50
Villet R, Van Den Akker M, Salet-Lizee D, Bastide N (1995) Cure de prolapsus par voie abdominale à l'aide d'un treillis de Vicryl composite. J Gynecol Obstet Biol Reprod 24:717–721
Inglesia CB, Fenner DE, Brubacker L (1997) The use of mesh in gynecologic surgery. Int Urogynecol J 8:105–115
Le Veen HH, Barberio JR (1949) Tissue reaction to plastics used in surgery with special reference to Teflon. Ann Surg 129:74–84
Olsson I, Kroon U (1999) A three-year postoperative evaluation of tension-free vaginal tape. Gynecol Obstet Invest 48:267–269
Meschia M, Pifarotti P, Bernasconi F et al. (2001) Tension-free vaginal tape: analysis of outcomes and complications in 404 stress incontinent women. Int Urogynecol J 12(Suppl 2): S24–S27
Nilsson CG, Kuuva N (2001) The tension-free vaginal tape procedure is successful in the majority of women with indications for surgical treatment of urinary stress incontinence. Br J Obstet Gynaecol 108:414–419
Tamussino K, Hanzal E, Kölle D, Ralph G, Riss P (2001) The Austrian Tension-free Vaginal Tape registry: an update. Int Urogynecol J 12 (Suppl 3):S22
Flood CG, Drutz HP, Waja L (1998) Anterior colporrhaphy reinforced with Marlex mesh for the treatment of cystoceles. Int Urogynecol J 9:200:4
Julian TM (1996) The efficacy of Marlex mesh in the repair of severe recurrent vaginal prolapse of the anterior midvaginal wall. Am J Obstet Gynecol 173:1472–1475
Goh JTW, Dwyer PL (2001) Effectiveness and safety of polypropylene mesh in vaginal prolapse surgery. Int Urogynecol J 12 (Suppl 3):S90
Adile B, Cucinella G, Gugliotta A, Lo Bue S, Grifo S (2001) Tension-free cystocele repair. Two years' follow-up. Int Urogynecol J 12 (Suppl 3):S92
Nicita G (1998) A new operation for genitourinary prolapse. J Urol 160:741–745
Choe Jong M, Ogan K, Battino BS (2000) Antimicrobial mesh versus vaginal wall sling: a comparative outcomes analysis. J Urol 163:1829–1834
Mage Ph (1999) L'interposition d'un treillis synthétique dans la cure par voie vaginale des prolapsus génitaux. J Gynecol Obstet Biol Reprod 28:825–829
Migliari R, Usai E (1999) Treatment results using a mixed fiber mesh in patients with grade IV cystocele. J Urol 161:1255–1258
Author information
Authors and Affiliations
Corresponding author
Additional information
Editorial Comment: This is a timely review of an issue that concerns every reconstructive surgeon. Although it is widely recognized that the ideal reconstructive material does not exist, it is worthwhile to understand the properties, limitations and efficacy evidence for currently available materials
Rights and permissions
About this article
Cite this article
Cosson, M., Debodinance, P., Boukerrou, M. et al. Mechanical properties of synthetic implants used in the repair of prolapse and urinary incontinence in women: which is the ideal material?. Int Urogynecol J 14, 169–178 (2003). https://doi.org/10.1007/s00192-003-1066-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-003-1066-z