Abstract
Purpose
Functional outcomes after knee arthroplasty (TKA) remain poor. The ability to restore the soft tissue envelope intraoperatively may improve such outcomes. The aim of this study was to extend the scope of computer navigation as a tool to quantifying the envelope of laxity during subjective stress testing preoperatively and to quantify the effects of knee replacement and how it changes as a result of ligamentous failure.
Methods
Loaded cadaveric legs were mounted on a purpose-built rig. Envelope of laxity was measured in 3 degrees of freedom using computer navigation. Knees were subjectively stressed in varus/valgus, internal/external rotation and anterior draw. This was performed preoperatively, during TKA and after sequential sectioning of ligaments. Real-time data were recorded at 0°, 30°, 60° and 90° of flexion. Mixed effect modelling was used to quantify the effects of intervention on degree of laxity.
Results
In all cases, there was an increase in laxity with increasing flexion or ligament sectioning. Operator and movement cycle had no effect. Insertion of a TKA showed increased stability within the joint, especially in internal/external rotation and anterior drawer. Once the PCL and popliteus were cut, the implant only maintained some rotatory stability; thereafter, the soft tissue envelope failed.
Conclusions
This work has shown a novel way by which computer navigation can be used to analyse soft tissue behaviour during TKA beyond the coronal plane and throughout range of motion. Despite subjective stress testing, our results show reproducible patterns of soft tissue behaviour—in particular a wide range of mid-flexion excursion. It also quantifies the limits within which a cruciate-retaining TKR can maintain knee stability. This functionality may guide the surgeon in identifying and/or preventing soft tissue imbalances intra-operatively, improving functional results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The long-term results of total knee arthroplasty (TKA) with revision as an endpoint are consistently reported at greater than 90 % out to 10 years [8] Revision is a crude endpoint and does not reflect the consistent finding of poor functional outcome in a significant percentage of this cohort [28]. Indeed, several studies report dissatisfaction rates following TKA approaching 20 % [1, 12, 33, 34]. Whilst poor outcomes may be multifactorial [24, 33, 36], surgeon-controlled factors are consistently improving with modern instrumentation, navigation tools and prosthetic design [15, 26, 32]. Knee replacement, however, remains largely a soft tissue operation. Stability of the knee joint is often performed by manual stressing after trial component insertion preoperatively. This in itself has its own limitations but may influence further ligament resection, bony cuts, implant position, polyethylene thickness or level of implant constraint [6, 19, 22]. Intuitively, the ability to restore the patient’s soft tissue envelope to lie within a normal non-arthritic range of laxity should lead to optimal function [30].
At its simplest level, soft tissue balancing is based upon traditional methods of gap balancing which are performed at 0° and 90° knee flexion [25]. Whether one chooses measured resection, gap equalisation, spacer blocks or tensioning devices [8, 20, 36], final assessment of knee laxity is usually decided after insertion of the trial components and manual stressing of the knee through a range of flexion. The concept of restoring the ‘Envelope of Laxity’ (EoL) mandates a balanced knee through a continuous arc of functional movement [3, 5, 25]. Whilst some work has attempted to quantify this behaviour [9, 16, 25], our aim was to extend the scope of this technology in order to quantify the ‘normal’ physiological soft tissue envelope in 3 degrees of freedom. Also, we aimed to identify to what extent TKA restores this soft tissue envelope and how well navigation can detect abnormal laxity.
Cadaveric work was performed, as a preclinical study using mixed effect modelling to account for uncontrolled variations.
Materials and methods
Eight radiologically normal fresh-frozen lower limbs (4 right, 4 left) including 20 cm of femur and whole lower legs were obtained from a tissue bank following ethical approval. The area over the knee joint was untouched. At the proximal femur, the flexor and extensor muscle groups were indentified. The quadriceps were divided into three components:
-
1.
rectus femoris (RF) + vastus intermedius (VI),
-
2.
vastus lateralis longus (VLL) + vastus lateralis obliquus (VLO)
-
3.
vastus medialis longus (VML) + vastus medialis obliquus (VMO).
The hamstring muscles were split into two groups:
-
1.
Semimembranosus + semitendinosus
-
2.
Biceps femoris (short and long head).
Cloth strips were looped over and sutured to the muscle bellies of each group and then attached to a loading cable. This allowed distribution of load across the muscle bellies and prevented tearing. Finally, a 12-mm-diameter stainless steel intramedullary rod was cemented into the femur using polymethylmethacrylate (PMMA) [13].
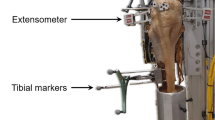
Experiment set-up
The knee specimen was mounted by securing the intramedullary rod onto a clamp on the custom-made rig. A muscle alignment system was used consisting of polished nylon pulleys along a stainless steel bar that could be adjusted, allowing each muscle group to be loaded in its physiological direction relative to the femoral axis [11, 18]. A load of 100N was applied to the quadriceps, and a further 100N is used to co-contract the hamstring muscle groups using hanging weights on the cable/pulley system. Hamstring co-contraction was used to reduce excessive anterior translation and tibial internal rotation from quadriceps loading alone as well as restore some inherent stability of the knee joint [2, 20, 21] (Fig. 1).
An 8-mm threaded rod 30 cm long was passed through the tibia from medial to lateral, 25 cm below the joint line. This allowed application of internal/external rotation torque to the tibia. Similarly, a hook was secured to the anterior tibia 8 cm below the level of the joint line. This allowed consistency of the position where the anterior drawer force was applied [33].
Optical trackers were screwed into the fixed femur and the mobile tibia and motion tracked using computer navigation (Stryker eNdtrac ASM Knee Navigation System, Michigan USA) to an accuracy of ±0.5 mm, ±0.5° [10]. Each knee was then taken through 20 flexion/extension cycles to reduce the effect of hysteresis and minimise the effects of sequential manipulation [29]. In biomechanical terms, laxity has been defined as a measure of joint movement within the constraints of ligaments, capsule and cartilage [7] when an external force is applied to the joint. The EoL was therefore quantified by measuring the path of the tibia in relation to the femur when the operating surgeon (senior author) performed varus/valgus moment, internal/external rotation torque and anterior drawer force to what he felt as a subjective endpoint. This was done at 0°, 30°, 60° and 90° of knee flexion. The EoLs were measured in (1) the native knee, (2) after arthrotomy, (3) after insertion of a standard posterior cruciate ligament retaining (CR) knee replacement (Stryker Scorpio NRG, Michigan USA) and (4) finally after sequential sectioning of key ligaments (Fig. 2).
Data capture
Raw data from an optical tracking navigation system (Stryker eNdtrac ASM Knee Navigation System, Michigan USA) were stored digitally and then plotted as individual (x , y, z) coordinates showing maximal displacements of the tibia in relation to the femur for each condition as the operating surgeon performed varus/valgus, internal/external rotation and anterior draw stress to a subjective endpoints. An example of the movement ‘clusters’ recorded is shown in Fig. 3. The range of the trajectories and sequence number for each manipulation at each angle of flexion were extracted for subsequent analysis. Displacements were then recorded with varus/valgus, internal/external rotation measured in degrees (°) and anterior translation measured in millimetres (mm).
Data representation
Data are presented as mean and standard error [95 % confidence interval (CI)] for all knee specimens (n = 8). They are represented as a magnitude of change in the excursion of the tibia in relation to the femur for each ‘intervention’ at 0, 30, 60 and 90° knee flexion—in relation to the native knee
a = maximum tibial excursion (either in degrees or millimetres), int = intervention, nat = native, x = angle of knee flexion.
Statistical analysis
To quantify the impact of knee flexion, surgical intervention and TKA in a simulated per-operative environment, variation in knee movement due to fixed effects, unmeasured and repeated measures on each knee had to be included. The fixed effects were range of knee flexion, implantation of TKA, arthrotomy and ligament resection. Unmeasured variations were size, age and gender of knee specimen, repeated manipulation/handling of the knee and operating surgeon. Repeated measured variations account for the effect of hysteresis during live data acquisition. A mixed effect modelling approach allowed fixed effects to be investigated whilst quantifying the amount of variation due to these unmeasured variables (given as a percentage) [27]. Models were assessed on the basis of the Wald test for individual fixed effects (mean divided by standard error) and the relative contribution of unmeasured random effects to the remaining unexplained variation. All analysis was undertaken using the R statistical software package (R Foundation for Statistical Computing, Vienna, Austria).
Results
Varus/valgus laxity (Fig. 4)
Varus–valgus laxity increased significantly (p < 0.05) with knee flexion, from 5° in extension to 15° at 90° flexion. Knee arthrotomy did not affect this significantly.
ACL resection increased overall laxity by less than 1°. The maximal effect occurred in extension, where the laxity increased by 38 % (27–48 %)—mean (95 % CI)—compared to that of the native knee.
On insertion of a TKA, varus–valgus laxity returned to a level not significantly different to that of the native knee.
Transection of the PCL, popliteus and MCL post-implantation of TKA increased overall varus–valgus laxity by 1°, 2° and 6°, respectively (all p < 0.05). Their maximal effect was noted at 60° and 90° of knee flexion. At these points, laxity increased by 28 and 55 %, respectively, for PCL; 36 and 78 %, respectively, for popliteus, and 136 and 195 % for MCL, respectively.
Internal–external rotation laxity (Fig. 5)
In the native knee, rotatory laxity was 22° whilst extended, and increased with knee flexion from 0° to 90° by 13° ± 0° (p < 0.05). Knee arthrotomy had no significant effect on rotatory laxity. ACL resection increased overall laxity by 2° ± 0° (p < 0.05). Insertion of a TKA reduced rotatory laxity to 2° ± 0° less than in the native knee (p < 0.05). With the implant in situ, resection of the PCL had no significant effect on rotatory laxity. However, with subsequent resection of popliteus and then MCL, the rotatory laxity of the knee increased significantly by 3° and 11° ± 0°, respectively (both p < 0.05), in comparison with the native knee.
The increase in laxity following popliteus resection was most significant at 60° −13 % (7–18 %) and 90° knee flexion −26 % (18–35 %).
Resection of the MCL produced a significant increase in rotatory laxity in all angles of knee flexion.
Anterior drawer laxity (Fig. 6)
Anterior–posterior (AP) drawer increased with knee flexion, by 7 ± 0 mm from 0° to 90° (p < 0.05). Knee arthrotomy increased AP laxity by 1 ± 0 mm (p < 0.05). ACL deficiency increased AP laxity by 2 ± 0 mm (p < 0.05). Implantation of a TKR returned AP knee laxity back to that of the native knee. Resection of the PCL, popliteus and MCL increased AP laxity by 1, 1 and 2 mm, respectively (all p < 0.05).
The increase in laxity following ligamentous resection was most marked at 30° knee flexion for arthrotomy: 29 % (20–38 %), ACL resection 85 % (79–91 %) and MCL resection 50 %, (43–57 %).
PCL resection caused a maximal increase in laxity at 60° knee flexion: 48 % (33–63 %).
Mixed effect model
Forty-eight per cent of the observed variation was attributable to knee specimen alone in Varus/Valgus manipulation, 49 % during internal/external rotation and 39 % attributable to the knee in anterior drawer manipulation. There was no significant effect of surgeon or manipulation cycle number on observed movement when included as random effects in the model, indicating that the operator did not affect the laxity of the joint during manipulation.
Discussion
The most important finding of the present study was that a model could be developed that objectively quantified the physiological soft tissue envelope of the intra-operative knee. It also identified to what extent TKA restored this soft tissue envelope and how soft tissue deficiency expanded it. This study has extended the ability of computer navigation to assess the soft tissue envelope by coupling it with a statistical analysis method which will be used to build a database describing variability across the population. Thus, in the future, navigation could be used as a technique that will allow detection of abnormal laxity to guide the surgeon and facilitate decision-making with respect to soft tissue balancing, implant choice or level of constraint. By aiming to restore more physiological laxity patterns, functional outcome may improve.
This paper has used an optical navigation system to quantify the laxity behaviour of the normal knee, and then a novel implementation of the mixed effect analysis method to demonstrate the effects of implantation of TKA and various levels of soft tissue damage to simulate an abnormal laxity envelope. The key findings were that: in all cases, there was an increase in laxity with increasing angle of knee flexion or ligament sectioning. Knee replacement did not restore laxity to its native state; once the posterior cruciate ligament and popliteus were sectioned, the CR implant could only maintain normal laxity in internal/external rotation and further ligament sectioning resulted in failure of the implant to maintain the soft tissue envelope; operator and movement cycle had no significant effect upon maximal laxity in any plane for a given state. Analogous to some previous work, it was also found that the largest observed discrepancy in laxity was from mid-to-deep flexion [4, 9, 25], although other studies found the largest discrepancy arose from loss of the anterior cruciate ligament near knee extension [4, 31].
Previous studies have tried to objectively quantify soft tissue behaviour after TKA in vivo and in vitro. This may either be by analysing principal retinacular [13] or collateral structures [14], using soft tissue tensioning devices [17, 24], or, as in this study, using computer navigation to collect real-time kinematic data [4, 9, 25, 31].
D’Lima et al. [9] investigated how effective standard soft tissue balancing techniques were in equalising the mediolateral distribution of forces across the knee during intraoperative passive knee flexion. Although the investigators achieved balanced flexion and extension gaps, pressure readings showed substantial pressure discrepancies across mid-flexion angles between 0° and 90°. They also acknowledged the need to look beyond coronal plane stability stating that ideal soft tissue balance in other planes was not yet known.
Bull et al. [4] and Stoddard et al. [31] performed very similar studies to the present work, using preloaded cadaveric specimens, but with known loads across the knee joint to reduce unmeasured variations. Despite the use of subjective endpoints in the present study, and a mixed effect model, the key findings were similar. TKA did not restore normal laxity. The implant reduced varus/valgus and rotatory laxity to within normal limits. Anterior translation did increase with knee flexion. The present results showed larger magnitudes of laxity during internal/external rotation and varus/valgus stress, but a smaller anterior drawer. This may be due to differing muscle loading strategies, greater forces imparted by the operating surgeon and that the present study simply measured anterior translation, not anteroposterior translation.
Norris et al. [25] developed the concept of envelope of laxity (EoL) by obtaining real-time laxity curves during varus/valgus stress on 20 consecutive osteoarthritic patients undergoing TKR using the same implant and navigation system. They recorded on average an increase in laxity of 4° at 30°–60° flexion in their cohort. TKA reduced this by 2°. The present study showed a consistent increase in varus/valgus laxity with increased knee flexion 5° in extension and 15° at 90° knee flexion. The cadaveric specimens were disease free and may account for the larger excursion; however, after TKA, coronal plane excursion was not reduced by as much as 2°. This may reflect the inherent stiffness in degenerate soft tissues when bony defects have been resurfaced [35, 37].
This work has added to the previous studies in three principal areas.
Firstly, a physiologically normal laxity envelope was quantified to act as a datum by which all other parameters could be compared. Secondly, the knees were examined in 3 planes of motion—anterior drawer, internal/external rotation and varus/valgus using subjective, surgeon-controlled endpoints. This has allowed a more global assessment of the soft tissue envelope in a manner familiar to clinicians. Finally, comparable results have been obtained through mixed effect modelling. This method allowed for separation of fixed effects that are expected to operate over all knees from those that arise from unmeasurable or uncontrolled effects, such as inter-knee variation, surgeon manipulation and repeated measurements [4]. Mixed effect modelling, by assuming a normal distribution permits reliable predictive quantification of how much inter-knee behavioural variation will occur for a standard surgical procedure. The reliability of this model improves as the data set is expanded and validates future in vivo work where we plan to obtain intraoperative laxity envelopes for a wider population.
There are a number of limitations with this work. The use of normal cadaveric specimens may not represent the pathological tissues in osteoarthritic knees. However, it is important to first understand and quantify the behaviour of the normal knee. Only then, can one properly assess the ability of an implant to restore normal kinematic behaviour, as well as the effects of soft tissue release. Laxity behaviour beyond 90° of knee flexion was not examined because of the design constraints of the rig and the inability of the motion tracker to see the tibial markers beyond 100° knee flexion. Muscle loading, though physiological in direction, was not representative of true muscle loads in vivo and this may affect soft tissue characteristics. However, the loads were sufficient to compress all of the articulations, stabilising the joint. Ligament sectioning was always done in the specified sequence. A random pattern of ligament releases would have been more powerful, but that would have required many more knees.
Finally, the statistical analysis is one not conventionally used for cadaveric studies. This novel approach acknowledges the likelihood of unmeasured variables and its proportionately large effect with small sample size. However, the goal is to expand this study to a larger population with in vivo analysis where unmeasured variations will remain but as sample size increases the proportionate effect of unmeasured variables and random effects decreases.
As the data set expands, the intraoperative laxity patterns of a wider population will be defined. It is hoped that this increased knowledge will facilitate the development of surgical algorithms. Such algorithms will act as decision-making tools to help guide future generations of surgeons either in arthroplasty training or during minimally invasive surgery where soft tissue balancing can be more challenging [23].
Conclusions
This study has used computer navigation to accurately quantify soft tissue laxity throughout range of motion. The novel use of a mixed effect model has shown an increase in laxity with knee flexion, and sequential ligament release. TKA did not restore the envelope of laxity to that of the native knee. The most significant changes were noted from mid-to-deep flexion. These changes were independent of operating surgeon.
References
Agletti P, Buzzi R, Gauderizi A (1998) Patellofemoral functional results and complications with posterior stabilised total knee prosthesis. J Arthroplasty 3:17–25
Andrews JG (1987) The functional roles of the hamstrings and quadriceps during cycling: Lombard’s paradox revisited. J Biomech 20:565–575
Blankevoort L, Huiskes R, De Lange A (1998) The envelope of passive knee joint motion. J Biomech 21:705–720
Bull AMJ, Kessler O, Alam M, Amis AA (2008) Changes in knee kinematics reflect the articular geometry after arthroplasty. Clin Orthop Relat Res 466:2491–2499
Bull AM, Amis AA (1998) Knee joint motion: description and measurement. Proc Inst Mech Eng 212H:357–372
Bottros J, Gad B, Krebs V, Barsoum W (2006) Gap balancing in total knee arthroplasty. J Arthroplasty 21(Supp 1):11–15
Cross M (1996) Clinical terminology for describing knee instability. Sports Med Arthrosc Rev 4:313–318
Dennis DA, Komistek RD, Kim RH, Sharma A (2010) Gap balancing versus measured resection technique for total knee arthroplasty. Clin Orthop Relat Res 468:102–107
D’lima DD, Patil S, Steklov N, Colwell CW (2007) Dynamic intraoperative ligament balancing for total knee arthroplasty. Clin Orthop Relat Res 463:208–212
Elfring R, de la Fuente M, Radermacher K (2010) Assessment of optical localizer accuracy for computer aided surgery systems. Comput Aided Surg 15:1–12
Farahmand F, Senavongse W, Amis AA (1998) Quantitative study of the quadriceps muscles and trochlear groove geometry related to instability of the patellofemoral joint. J Orthop Res 16:136–143
Fu Y, Wang M, Lui Y, Fu Q (2012) Alignment outcomes in navigated total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 20:1075–1082
Ghosh KM, Merican AM, Iranpour F, Deehan DJ, Amis AA (2009) Length change patterns in the extensor retinaculum and the effects of total knee replacement. J Orthop Res 27:865–870
Ghosh KM, Merican AM, Iranpour F, Deehan DJ, Amis AA (2012) Length change patterns of the collateral ligaments after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20:1349–1356
Hetalmish BM, Khan MM, Simunovic N, Al-Harbi HH, Bhandari M, Zalzal PK (2012) Meta-analysis of navigation versus conventional total knee arthroplasty. J Arthroplasty 27:1177–1182
Kamat YD, Aurakzai KM, Adhikari AR (2012) Computer navigation of soft tissue in total knee replacement J Knee Surg 30. doi:10.1055/s-0032-1322600
Kwak DS, Kong CG, Han SH, Kim DH, In Y (2012) Development of a pneumatic tensioning device for gap measurement during total knee arthroplasty. Clin Orthop Surg 4:188–192
Kwak SD, Ahmad CS, Gardner TR (2000) Hamstrings and iliotibial band forces affect knee kinematics and contact pattern. J Orthop Res 18:101–108
Lanting BA, Snider MG, Chess DG (2012) Effect of polyethylene component thickness on range of motion and stability in primary total knee arthroplasty. Orthopedics 35:170–174
Li G, Rudy TW, Sakane M, Kanamori A, Ma CB, Woo SL (1999) The importance of quadriceps and hamstring muscle loading on knee kinematics and in-situ forces in the ACL. J Biomech 32:395–400
Lombard WP, Abbott FM (1907) The mechanical effects produced by the contraction of individual muscles of the thigh of the frog. Am J Physiol 20:1–60
Lotke PA, Ecker ML (1977) Influence of positioning of the prosthesis in total knee replacement. J Bone Joint Surg Am 59:77–79
Matsumoto T, Muratsu H, Kubo S, Mizuno K, Kinoshita K, Ishida K, Matsushita T, Sasaki K, Tei K, Takayama K, Sasaki H, Oka S, Kurosaka M, Kuroda R (2011) Soft tissue balance measurement in minimal incision surgery compared to conventional total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19:880–886
Matsumoto T, Muratsu H, Kubo S, Matsushita T, Kurosaka M, Kuroda R (2011) Soft tissue tension in cruciate-retaining and posterior-stabilized total knee arthroplasty. J Arthroplasty 26:788–795
Norris M, Gill K, Karadaglis D, Chauhan S (2009) The envelope of laxity and balancing of total knee replacement using navigation. J Bone Joint Surg Br 91B:426
Pang HN, Yeo SJ, Chong HC, Chin PL, Ong J, Lo NN (2011) Computer-assisted gap balancing technique improves outcome in total knee arthroplasty, compared with conventional measured resection technique. Knee Surg Sports Traumatol Arthrosc 19:1496–1503
Pinheiro JC, Bates DM (2000) Mixed-effects models in S and S-PLUS. Springer Verlag, New York
Price AJ, Longino D, Rees J, Rout R, Pandit H, Javaid K, Arden N, Cooper C, Carr AJ, Dodd CA, Murray DW, Beard DJ (2010) Are pain and function better measures of outcome than revision rates after TKR in the younger patient? Knee 17:196–199
Schatzmann L, Brunner P, Staubli HU (1998) Effect of cyclic preconditioning on the tensile properties of human quadriceps tendons and patellar ligaments. Knee Surg Sports Traumatol Asthrosc 6:56–61
Scott CE, Howie CR, Macdonald D, Biant LC (2010) Predicting dissatisfaction following total knee replacement: a prospective study of 1,217 patients. J Bone Joint Surg Br 92:1253–1258
Stoddard JE, Deehan DJ, Bull AMJ, McCaskie AW, Amis AA (2013) The kinematics and stability of single-radius versus multi-radius femoral components related to mid-range instability after TKA. J Orthop Res 31:53–58
Song EK, Park SJ, Yoon TR, Park KS, Seo HY, Seon JK (2012) Hi-flexion and gender-specific designs fail to provide significant increases in range of motion during cruciate-retaining total knee arthroplasty. J Arthroplasty 27:1081–1084
The national joint registry 8th annual report. Sept 2011, pp 95
Van Damme G, Defoort K, Ducoulombier Y, Van Glabbeek F, Bellemans J, Victor J (2005) What should the surgeon aim for when performing computer assisted total knee arthroplasty? J Bone Joint Surg Am 87:52–58
Wada M, Imura S, Baba H, Shimida S (1996) Knee laxity in patients with osteoarthritis and rheumatoid arthritis. Br J Rheumatol 35:560–563
Winemaker MJ (2002) Perfect balance in total knee arthroplasty: the elusive compromise. J Arthroplasty 17:2–10
Zalzal P, Papini M, Petruccelli D, de Beer J, Winemaker MJ (2004) An in vivo biomechanical analysis of the soft tissue envelope of osteoarthritic knees. J Arthroplasty 19:217–223
Acknowledgments
This project was supported and undertaken at the Newcastle Surgical Training Centre (Freeman Hospital, Newcastle Upon Tyne, UK). The authors declare no financial arrangements with the fund holding company.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ghosh, K.M., Blain, A.P., Longstaff, L. et al. Can we define envelope of laxity during navigated knee arthroplasty?. Knee Surg Sports Traumatol Arthrosc 22, 1736–1743 (2014). https://doi.org/10.1007/s00167-013-2574-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-013-2574-0