Abstract
Purpose
Restoration of posterior tibial translation (PTT) after reconstruction of the posterior cruciate ligament (PCL) is deemed necessary to restore physiological knee kinematics. However, current surgical techniques have failed to show a complete reduction of posterior laxity. It was hypothesized that early postoperative PTT increases over time.
Methods
The study comprised of 46 patients (10 female, 36 male; 30 ± 9 years), who underwent PCL reconstruction in a single-surgeon series. Patients were evaluated by bilateral stress radiographs in a prospective manner preoperatively; at 3, 6, 12 and 24 months; and at a final follow-up (FFU) of at least 5 years. Covariants included age, gender, BMI, tibial slope (TS) and the number of operated ligaments. Two blinded observers reviewed all radiographs, evaluating the TS and the posterior tibial translation.
Results
All patients were evaluated at a mean final follow-up of 102 (range 65–187) months. Mean side-to-side difference of the PTT significantly improved from preoperative to 3-month postoperative values (10.9 ± 3.1 vs. 3.6 ± 3.8 mm; P < 0.0001). The PTT increased to 4.6 ± 3.7 mm at 6 months, to 4.8 ± 3.3 mm at 12 months, to 4.8 ± 3.2 mm at 24 months, to 5.4 ± 3.4 mm at FFU. Consequently, there was a significant increase of PTT between 3-month and final follow-up (3.6 ± 3.8 vs. 5.4 ± 3.4 mm; P = 0.02). Flattening of the TS resulted in a significantly higher PTT compared to subjects with a high TS at 24 months and FFU. There was no significant influence by BMI, age, gender and the number of operated ligaments.
Conclusions
Early results after PCL reconstruction seem promising as posterior tibial translation is significantly improved. However, there is a significant increase in PTT from early postoperative values to the final follow-up of at least 5 years. This is particularly notable in patients with flattening of the TS. As a consequence, surgeons and patients need to be aware that initial posterior stability should not be equated with the final outcome.
Level of evidence
Cohort study, Level III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The functional importance of the posterior cruciate ligament (PCL) has been widely acknowledged. After injury, reconstruction of the PCL is deemed necessary to enable physiological joint biomechanics [3, 12, 22, 35].
Surgical techniques for PCL reconstruction continue to evolve and to improve clinical results. Even though early results appear to be satisfactory, outcome parameters in the long term remain contentious and seem to deteriorate [2, 24, 33, 34, 42]. This mismatch is illustrated by a discord between biomechanical studies, which indicate that current surgical techniques can restore native knee kinematics close to the physiological state [15, 30] and clinical studies, which reveal a remaining residual laxity of 4–6 mm over time [8, 19, 21, 37].
Several covariants for recurring instability are discussed controversially, including patient gender, age, or body weight; improper graft placement, strength, size, or tensioning; or reinjury [4, 19, 20]. Just recently Gwinner et al. reported that the degree of tibial slope (TS) also influences posterior laxity after PCL reconstruction [13]. To the best of our knowledge, no study exists evaluating the time-dependent behavior of knee stability after PCL reconstruction. However, this might help to avoid overly optimistic expectations and might help to identify patients at risk of recurrent instability.
Consequently, the aim of the current study is to evaluate posterior laxity after PCL reconstruction over time by repeated stress radiographs. It was hypothesized that the posterior tibial translation (PTT) significantly increases from initial postoperative values to final follow-up. Additionally, it was sought to elucidate whether gender, age, body weight, the number of operated ligaments, or the TS influence the change in PTT over time.
Materials and methods
All PCL surgeries were performed by the senior author (A.W.). Inclusion criteria comprised of patients with at least grade II laxity (≥ 6 mm) according to Harner and Höher [14] as assessed by the posterior drawer test and posterior stress radiographs (GA II stress device; Telos, Weiterstadt, Germany). Only patients with a primary reconstruction of the PCL using autologous hamstring tendon grafts were included. The cohort was evaluated in a prospective manner, and analysis of the data was performed retrospectively. Patients received stress radiographs preoperatively; at 3, 6, 12 and 24 months; and at the final follow-up. Anthropometric and demographic measures including age (years), gender and BMI (kg/m2) were documented. Additionally, the number of operated ligaments (i.e., isolated PCL reconstruction; combined PCL and posterolateral corner reconstruction; or combined ACL, PCL and posterolateral corner reconstruction) of each patient was recorded. Patients needed to have a minimum of four out of the six radiographs; including the preoperative radiograph, one within the first 6 months postoperatively and the final follow-up radiograph. The minimum follow-up was 5 years.
Patients with bilateral injuries, combined lower extremity fractures or prior surgery to the uninvolved knee were excluded. Furthermore, we excluded patients whose radiographs did not include a true lateral view of the tibia as determined by proper superimposition of the femoral condyles. Patients with poor-quality or non-digital radiographs were excluded to improve interrater comparability and to decrease the number of confounding variables.
Surgical technique
All PCL reconstructions were performed by a single surgeon. The patient was placed in supine position under general anesthesia and preoperative intravenous antibiotics were administered.
Ipsilateral, autologous, five-folded semitendinosus and gracilis tendons were used as the PCL graft. In cases of combined reconstruction of the posterolateral corner or the anterior cruciate ligament, contralateral hamstring grafts were used.
Remnants of the PCL were retained whenever possible. Femoral tunnel creation for the single-bundle PCL reconstruction was performed through a low-anterolateral portal using a dedicated femoral drill guide (Karl Storz GmbH, Tuttlingen, Germany) centered at the anterolateral bundle of the PCL.
Tibial tunnel creation was done with direct arthroscopic visualization using an additional posteromedial portal and standardized drill guides. Femoral and tibial fixation was performed in a hybrid manner using biodegradable interference screws and the EndoPearl device (Linvatec Corp., Largo, USA) on the femoral site and additional sutures tight over a bony bridge on the tibial site.
Rehabilitation
Postoperative care consisted of immobilization of the knee in full extension in a dedicated splint (PTS; posterior tibial support; Medi, Bayreuth, Germany) for 6 weeks. Partial weightbearing and gradual passive mobilization in a prone position was performed during this period. After 6 weeks, full weightbearing was established and the PTS splint was changed into a functional PCL brace.
Radiological assessment
Posterior stress radiographs of both knees were used for radiographic assessment. Two observers (C.G. and I.S.) evaluated the TS and the posterior tibial translation using a PACS workstation (Centricity RIS-I 4.2 Plus, GE Healthcare, Milwaukee, WI, USA). Both parameters were measured in a blinded manner. The mean values for the TS and the posterior tibial translation were calculated.
Posterior laxity was evaluated by conventional stress radiographs at 90° of flexion using a stress device (GA II stress device; Telos, Weiterstadt, Germany) with a posteriorly directed force of 150 N at the level of the tibial tuberosity. Perpendicular to the joint line, the midpoints between the most posterior contours of the medial and lateral femoral condyles and tibial plateaus were established [18, 32]. The distance between these two points of the injured side was compared to the distance of the uninjured contralateral knee, henceforth referred to as the posterior tibial translation (PTT).
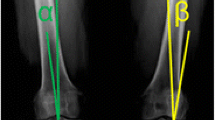
The TS is defined as the angle between the posterior inclination of the tibial plateau and a line perpendicular to the diaphyseal shaft axis. The diaphyseal shaft axis was determined according to Dejour and Bonnin [7] using two midpoints between the anterior and posterior tibial cortex; one at 5 cm below the tibial tuberosity and the other one 15 cm below the tibial joint line. Although the best available radiographs were chosen, not all included enough tibial shaft to determine the width of the shaft at a distance of 15 cm distal to the joint line. In these instances, the most distal width was measured based on the aforementioned conditions (Fig. 1).
Measurement of the PTT (a). The PTT (asterisk) is defined as the distance between the mean posterior contours of the femoral condyles and the tibial plateau; measurement of the TS (b). The TS (asterisk) is defined as the tangent line to the medial tibial plateau and a line perpendicular to the longitudinal tibial axis
The ethics committee of Charité-Universitaetsmedizin Berlin approved the current study (EA1/003/16), and all patients gave informed consent.
Statistical analysis
Statistical analysis was performed using Prism Version 6 (GraphPad Software Inc., San Diego, CA). Continuous data are expressed as mean ± SD and or median (interquartile range) according to their distribution. D’Agostino and Person omnibus normality tests were used to test Gaussian distribution. The comparison of parametric data was performed with a t test and non-parametric data was tested by a Mann–Whitney test. The intraclass correlation coefficient (ICC) was used to evaluate interrater reliability. Notably, values of 0.5 through 0.6 are regarded as moderate agreement whereas 0.7 through 0.8 indicate a strong agreement. P < 0.05 was considered statistically significant. Additionally, Bland Altman plots were used to visualize uncertainty between both reviewers for measurement of the TS and the PTT (final follow-up).
Results
A total of 46 patients met our inclusion criteria and were enrolled in this study. Seven patients (15%) received an isolated PCL reconstruction, 26 patients (57%) a combined PCL and posterolateral corner reconstruction and 13 patients (28%) a reconstruction of both the anterior and posterior cruciate ligament as well as of the posterolateral corner. All patients were evaluated at a mean final follow-up of 102 (range 65–187) months.
Intraclass correlation coefficient between the observers was 0.82 for the TS and 0.84 for the PTT, indicating a high interrater agreement. The corresponding Bland Altman plots are shown in Fig. 2.
Mean side-to-side difference of the PTT significantly improved from preoperative to the 3 months postoperative values (10.9 ± 3.1 vs. 3.6 ± 3.8 mm; P < 0.0001). The PTT increased to 4.6 ± 3.7 mm at 6 months, 4.8 ± 3.3 mm at 12 months, to 4.8 ± 3.2 mm at 24 months and 5.4 ± 3.4 mm at the final follow-up. Consequently, there was a significant difference in the PTT between the 3-month and the final follow-up values (3.6 ± 3.8 vs. 5.4 ± 3.4 mm; P = 0.02; Fig. 3).
Taking only the injured side into account, the absolute PTT significantly improved from 13.1 ± 3.1 mm preoperatively to 6.1 ± 3.6 mm 3 month postoperatively (P = 0.0001). The absolute PTT increased to 7.0 ± 3.5 mm at 6 months, to 7.2 ± 3.0 mm at 12 months, to 7.3 ± 3.1 mm at 24 months and to 8.1 ± 3.2 mm at the FFU. Likewise, there is a significant difference between the PTT at 3 months and at FFU (6.1 ± 3.6 vs. 8.1 ± 3.2 mm; P = 0.01).
Analysis of the tibial slope
The mean TS was 8.3° (± 3.6°; range 1–14°) for the operated and 7.9° (± 3.4°; range 2–15°) for the contralateral knee. A threshold was drawn at 9°, to establish two equal cohorts of 23 patients each (group A = 5.1 ± 2°; range 1–8° and group B = 11.4 ± 1.6°; range 9–14°). There were no significant differences between group A and B at preoperative, 3, 6 or 12 month values. Patients in Group A had a significantly higher PTT compared to Group B both at the 24-month (6.6 ± 3.4 vs. 3.8 ± 2.6 mm; P = 0.0033) and final follow-up (7.2 ± 3.4 vs. 3.7 ± 2.5 mm; P = 0.0002) values (Fig. 4).
Anthropometric analysis
The mean age of the patients was 30 ± 8.9 years (range 18–47). A threshold at 30 years was created to establish two equal cohorts of 32 patients each (Group C 22.3 ± 3.8 years; range 18–30 years and Group D 38 ± 4 years; range 31–47 years). There were no statistically significant differences of the TS or of the PTT at any time between both groups.
Likewise, the TS and PTT in female (n = 10) versus male (n = 36) patients was compared. There were no significant differences regarding the TS between female and male patients (7.8 ± 3.5° vs. 8.4 ± 3.7°; n.s.). Additionally, there were no significant differences of the PTT between both female and male patients at any time.
Subgrouping according to the number of operated ligaments was performed: isolated PCL reconstruction (Group E; N = 7); reconstruction of the PCL and the posterolateral corner (Group F; N = 26); and reconstruction of the ACL, PCL and posterolateral corner (Group G; N = 13). There were no significant differences in the TS and the PTT between the subgroups (Fig. 5).
Average BMI was 26.9 ± 4.2 kg/m2 (range 22–36) preoperatively and 28.5 ± 4.8 kg/m2 (range 21–41) at time of final follow-up (n.s.). There was no significant correlation between patients’ BMI and posterior knee laxity at any time.
Discussion
The most important finding of the present study was, that initial posterior laxity degrades over time after PCL reconstruction. Specifically, posterior tibial translation significantly increases from early postoperative values to the final follow-up. This is particularly notable in patients with flattening of the TS. Thus, the tested hypothesis was confirmed by the results of the current study. Other covariants did not have a significant influence in the present data. Consequently, this might help to adjust overly optimistic patients’ and surgeons’ expectations, as results seem to deteriorate over time and initial postoperative results cannot be equated with the final outcome.
Despite recent advancement in PCL surgery, a considerable number of patients fail to recover from their injuries and clinical results remain less predictable than those after ACL reconstruction. Reproducible results are dependent on a number of different variables, including choice of graft tissue, graft position, tensioning and postoperative rehabilitation. Small alterations in any of these parameters may result in an early or late construct elongation. Early construct elongation occurs on the basis of graft slippage or graft elongation [31, 38]. The latter can be attributed to the inherent viscoelastic and viscoplastic properties of soft-tissue grafts and their fixations. Numerous studies have indicated that this usually occurs within the first hours after surgery [1, 5, 28]. Inferior graft anchorage within the bone–screw interface or loosening of the tibial fixation devices have been studied extensively in ACL surgery [10, 16, 29, 39, 40]. Contrary to its anterior counterpart, there is a paucity regarding loss of fixation after PCL reconstruction. Nevertheless, early construct elongation is predominantly relevant until the graft–tunnel interface incorporates into a primary graft attachment. This usually occurs up to an estimate of 4 weeks for bone–tendon–bone and 8 weeks for hamstring tendons [25]. Thus, the current study could not elucidate any of these early covariants, as the first postoperative evaluation of posterior stability was performed at a 3-month follow-up.
Late causes for residual construct elongation can be summarized to increased in situ forces of the reconstructed ligament [6, 11, 17]. This may be particularly relevant in patients with a flattening of the TS, as these patients had a significantly higher PTT at 24 months and final follow-up compared to patients with a high TS. Even though the influence of the underlying geometry of the operated knee on clinical outcome has long been underestimated, flattening of the TS has been shown to be associated with a significantly higher residual posterior tibial translation as well as a decreased reduction of posterior tibial translation after PCL reconstruction [13]. As an implication of this, isolated soft-tissue procedures may only incompletely address posterior knee instability in this subset of patients. Thus, a preoperative determination of the TS should be a mandatory part of the surgical planning.
The results of this study further account for the mismatch in the current literature between the promising short- and worsened long-term results after PCL reconstruction in regard to the restoration of posterior laxity [23, 27, 36]. Notably, the change in posterior tibial translation in the present study coincides with the changes in patients’ activity, which scrutinizes current rehabilitation algorithms. Fanelli advocated that a slow and deliberate rehabilitation following PCL reconstruction is mandatory to a successful clinical outcome [9]. Mook et al. validated this caution in a recent biomechanical analysis and concluded that rehabilitation protocols should avoid implementation of early full weightbearing, as this resulted in acquired graft laxity [26]. Because of this premise, most clinical studies—including the present study—have implemented a rather conservative rehabilitation protocol, but results still deteriorate in the long term [21, 34]. Consequently, development of an optimal postoperative algorithm still merits further investigation, in particular for patients with a flattening of the TS.
There are a few limitations to the study, which should be noted. Since clinical endpoints have not been accounted for in the current study, the clinical applicability in regard to patient-reported outcomes or resumption of sporting activities may be limited. However, posterior stress radiographs have been acknowledged to provide a highly accurate, objective quantification of posterior laxity, which is crucial to delineate potential risk factors in the setting of multiple endpoints over time.
Furthermore, there was a relatively wide range of concomitant injuries within our patient cohort. However, no significant difference could be established in regard to the number of operated ligaments at any follow-up. Additionally, in an effort to reduce variability we set stringent inclusion criteria in this single-surgeon series and used a standardized surgical and rehabilitation protocol.
Another drawback of the current study is the measurement of the TS on a standard radiograph, thus potentially ignoring a possible asymmetry between the medial and lateral TS [41]. Nevertheless, there was a high interrater reliability for both the TS as well as the posterior tibial translation in the current study and a previous investigation [13].
Conclusion
Early radiographic results after reconstruction of the posterior cruciate ligament seem promising as posterior tibial translation is significantly decreased. However, there is a significant increase of posterior tibial translation from early postoperative values to the final follow-up of at least 5 years. Thus initial results after PCL reconstruction should not be equated with the final outcome, particularly in patients with flattening of the TS.
References
Arnold MP, Lie DT, Verdonschot N, de Graaf R, Amis AA, van Kampen A (2005) The remains of anterior cruciate ligament graft tension after cyclic knee motion. Am J Sports Med 33:536–542
Barrett GR, Savoie FH (1991) Operative management of acute PCL injuries with associated pathology: long-term results. Orthopedics 14:687–692
Boynton MD, Tietjens BR (1996) Long-term followup of the untreated isolated posterior cruciate ligament-deficient knee. Am J Sports Med 24:306–310
Campbell RB, Torrie A, Hecker A, Sekiya JK (2007) Comparison of tibial graft fixation between simulated arthroscopic and open inlay techniques for posterior cruciate ligament reconstruction. Am J Sports Med 35:1731–1738
Ciccone WJ, Bratton DR, Weinstein DM, Elias JJ (2006) Viscoelasticity and temperature variations decrease tension and stiffness of hamstring tendon grafts following anterior cruciate ligament reconstruction. J Bone Jt Surg Am 88:1071–1078
Corsetti JR, Jackson DW (1996) Failure of anterior cruciate ligament reconstruction: the biologic basis. Clin Orthop Relat Res 325:42–49
Dejour H, Bonnin M (1994) Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Jt Surg Br 76:745–749
Fanelli GC, Edson CJ (2004) Combined posterior cruciate ligament-posterolateral reconstructions with Achilles tendon allograft and biceps femoris tendon tenodesis: 2- to 10-year follow-up. Arthroscopy 20:339–345
Fanelli GC (2008) Posterior cruciate ligament rehabilitation: how slow should we go? Arthroscopy 24:234–235
Ferretti A, Conteduca F, Labianca L, Monaco E, De Carli A (2005) Evolgate fixation of doubled flexor graft in anterior cruciate ligament reconstruction biomechanical evaluation with cyclic loading. Am J Sports Med 33:574–582
Getelman MH, Friedman MJ (1999) Revision anterior cruciate ligament reconstruction surgery. J Am Acad Orthop Surg 7:189–198
Gill TJ, DeFrate LE, Wang C, Carey CT, Zayontz S, Zarins B, Li G (2004) The effect of posterior cruciate ligament reconstruction on patellofemoral contact pressures in the knee joint under simulated muscle loads. Am J Sports Med 32:109–115
Gwinner C, Weiler A, Roider M, Schaefer FM, Jung TM (2017) Tibial slope strongly influences knee stability after posterior cruciate ligament reconstruction. Am J Sports Med 45:355–361
Harner CD, Höher J (1998) Evaluation and treatment of posterior cruciate ligament injuries. Am J Sports Med 26:471–482
Harner CD, Janaushek MA, Kanamori A, Yagi M, Vogrin RM, Woo SL (2000) Biomechanical analysis of a double-bundle posterior cruciate ligament reconstruction. Am J Sports Med 28:144–151
Harvey AR, Thomas NP, Amis AA (2003) The effect of screw length and position on fixation of four-stranded hamstring grafts for anterior cruciate ligament reconstruction. Knee 10:97–102
Jackson DW, Grood ES, Cohn BT, Arnoczky SP, Simon TM, Cummings JF (1991) The effects of in situ freezing on the anterior cruciate ligament. An experimental study in goats. J Bone Jt Surg Am 73:201–213
Jacobsen K (1976) Stress radiographical measurement of the anteroposterior, medial and lateral stability of the knee joint. Acta Orthop Scand 47:335–344
Kim YM, Lee CA, Matava MJ (2011) Clinical results of arthroscopic single-bundle transtibial posterior cruciate ligament reconstruction: a systematic review. Am J Sports Med 39:425–434
Lin YC, Chen SK, Liu TH, Cheng YM, Chou PP (2013) Arthroscopic transtibial single-bundle posterior cruciate ligament reconstruction using patellar tendon graft compared with hamstring tendon graft. Arch Orthop Trauma Surg 133:523–530
Lipscomb AB, Anderson AF, Norwig ED, Hovis WD, Brown DL (1993) Isolated posterior cruciate ligament reconstruction Long-term results. Am J Sports Med 21:490–496
Logan M, Williams A, Lavelle J, Gedroyc W, Freeman M (2004) The effect of posterior cruciate ligament deficiency on knee kinematics. Am J Sports Med 32:1915–1922
MacGillivray JD, Stein BE, Park M, Allen AA, Wickiewicz TL, Warren RF (2006) Comparison of tibial inlay versus transtibial techniques for isolated posterior cruciate ligament reconstruction: minimum 2-year follow-up. Arthroscopy 22:320–328
Matava MJ, Ellis E, Gruber B (2009) Surgical treatment of posterior cruciate ligament tears: an evolving technique. J Am Acad Orthop Surg 17:435–446
Milano G, Mulas PD, Sanna-Passino E, Careddu GM, Ziranu F, Fabbriciani C (2005) Evaluation of bone plug and soft tissue anterior cruciate ligament graft fixation over time using transverse femoral fixation in a sheep model. Arthroscopy 21:532–539
Mook WR, Civitarese D, Turnbull TL, Kennedy NI, O’Brien L, Schoeberl JB, LaPrade RF (2016) Double-bundle posterior cruciate ligament reconstruction: a biomechanical analysis of simulated early motion and partial and full weightbearing on common reconstruction grafts. Knee Surg Sports Traumatol Arthrosc 8:2536–2544
Petrigliano FA, Suero EM, Voos JE, Pearle AD, Allen AA (2012) The effect of proximal tibial slope on dynamic stability testing of the posterior cruciate ligament- and posterolateral corner-deficient knee. Am J Sports Med 40:1322–1328
Pilia M, Murray M, Guda T, Heckman M, Appleford M (2015) Pretensioning of soft tissue grafts in anterior cruciate ligament reconstruction. Orthopedics 38:e582–e587
Prodromos CC, Hecker A, Joyce B, Finkle S, Shi K (2009) Elongation of simulated whipstitch post anterior cruciate ligament reconstruction tibial fixation after cyclic loading. Knee Surg Sports Traumatol Arthrosc 17:914–919
Race A, Amis AA (1998) PCL reconstruction. In vitro biomechanical comparison of ‘isometric’ versus single and double-bundled ‘anatomic’ grafts. J Bone Jt Surg Br 80:173–179
Scheffler SU, Südkamp NP, Göckenjan A, Hoffmann RF, Weiler A (2002) Biomechanical comparison of hamstring and patellar tendon graft anterior cruciate ligament reconstruction techniques: the impact of fixation level and fixation method under cyclic loading. Arthroscopy 18:304–315
Schulz MS, Steenlage ES, Russe K, Strobel MJ (2007) Distribution of posterior tibial displacement in knees with posterior cruciate ligament tears. J Bone Jt Surg Am 89:332–338
Sekiya JK, West RV, Ong BC, Irrgang JJ, Fu FH, Harner CD (2005) Clinical outcomes after isolated arthroscopic single-bundle posterior cruciate ligament reconstruction. Arthroscopy 21:1042–1050
Song EK, Park HW, Ahn YS, Seon JK (2014) Transtibial versus tibial inlay techniques for posterior cruciate ligament reconstruction: long-term follow-up study. Am J Sports Med 42:2964–2971
Strobel MJ, Weiler A, Schulz MS, Russe K, Eichhorn HJ (2003) Arthroscopic evaluation of articular cartilage lesions in posterior-cruciate-ligament-deficient knees. Arthroscopy 19:262–268
Wajsfisz A, Christel P, Djian P (2010) Does combined posterior cruciate ligament and posterolateral corner reconstruction for chronic posterior and posterolateral instability restore normal knee function? Orthop Traumatol Surg Res 96:394–399
Wang CJ, Chen HS, Huang TW (2003) Outcome of arthroscopic single bundle reconstruction for complete posterior cruciate ligament tear. Injury 34:747–751
Weiler A, Richter M, Schmidmaier G, Kandziora F, Südkamp NP (2001) The EndoPearl device increases fixation strength and eliminates construct slippage of hamstring tendon grafts with interference screw fixation. Arthroscopy 17:353–359
Weiler A, Peine R, Pashmineh-Azar A, Abel C, Südkamp NP, Hoffmann RF (2002) Tendon healing in a bone tunnel. Part I: Biomechanical results after biodegradable interference fit fixation in a model of anterior cruciate ligament reconstruction in sheep. Arthroscopy 18:113–123
Weiler A, Hoffmann RF, Bail HJ, Rehm O, Südkamp NP (2002) Tendon healing in a bone tunnel. Part II: Histologic analysis after biodegradable interference fit fixation in a model of anterior cruciate ligament reconstruction in sheep. Arthroscopy 18:124–135
Weinberg DS, Williamson DF, Gebhart JJ, Knapik DM, Voos JE (2016) Differences in medial and lateral posterior tibial slope an osteological review of 1090 tibiae comparing age, sex, and race. Am J Sports Med 1:106–113
Yang JH, Yoon JR, Jeong HI, Hwang DH, Woo SJ, Kwon JH, Nha KW (2012) Second-look arthroscopic assessment of arthroscopic single-bundle posterior cruciate ligament reconstruction: comparison of mixed graft versus achilles tendon allograft. Am J Sports Med 40:2052–2060
Acknowledgements
We would like to show our gratitude to Kevin C. Wang (Northwestern University Feinberg School of Medicine Chicago, IL, USA) for his constructive criticism and for his correction of the manuscript, which led to a significant improvement of the study.
Funding
All authors declare that they have not received any funding or research Grants in the course of study, research or assembly of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors have seen and approved submission of the manuscript, and have taken due care to ensure the integrity of the work. CG: Data collection, Writing and editing the manuscript. TMJ: Data analysis, Revising the manuscript. IS: Data collection, Writing the manuscript. AW: Co-ordinated the study, Data collection, Writing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest in the authorship and publication of this contribution. More specifically, none of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. None of the authors, or their institution(s), had any financial relationship, with any entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. In addition, all authors declare that they have had no other relationships, or have been engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work.
Ethical approval
The ethics committee of Charité-Universitaetsmedizin Berlin approved the current study (EA1/003/16).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Gwinner, C., Jung, T.M., Schatka, I. et al. Posterior laxity increases over time after PCL reconstruction. Knee Surg Sports Traumatol Arthrosc 27, 389–396 (2019). https://doi.org/10.1007/s00167-018-5035-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5035-y