Abstract
Whipstitch-post (WSP) tibial fixation is one of the most widely used and clinically successful methods of soft tissue graft fixation for anterior cruciate ligament reconstruction (ACLR). However, some consider the method prone to laxity. We hypothesized that WSP would have low elongation rates after experimental cyclic loading. Eight cadaveric human semitendinosus and gracilis (ST/Gr) tendons had whipstitches woven into their overlapped ends. The grafts were looped around a metal bar, pneumatically clamped, and cyclically loaded. The adjusted mean experimental graft elongation for the WSP was 1.13 mm with a maximum elongation of 1.64 mm and a standard deviation of 0.32. These values are equivalent to the lowest published cyclic loading tibial fixation elongation data. Whipstitch-post tibial ACLR fixation is biomechanically sound with among the lowest rates of elongation after laboratory cyclic loading.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Even in the most experienced hands, normal translational stability (0–2 mm side to side difference) is achieved in only about 70% of anterior cruciate ligament reconstructed patients. It is generally agreed that tibial fixation is the weak link in achieving stability with soft tissue grafts [3]. No consensus exists as to the best tibial fixation technique. The available methods can be divided into three types. The first utilizes direct graft friction fixation within the tibial tunnel with interference screws [16] or interference screw-based systems such as the Intrafix (Mitek, Raynham MA), GTS sleeve [2] (Smith and Nephew, Andover MA), or Centraloc [1] (Arthrotek, Warsaw IN). The second utilizes direct graft friction fixation on the tibial cortex, such as the Washerloc [12] (Arthrotek, Warsaw IN) or staples [27]. The third uses indirect graft fixation with a whipstitch or other interface to anchor the graft to the cortex, such as the whipstitch-post method [20] or Fastlok [7] (Neoligaments, Leeds England).
Some have criticized the whipstitch construct as being of low stiffness and allowing excessive elongation [9]. However, fixation stiffness is only a relevant property until the graft-tunnel interface assumes primary graft attachment site load bearing. This occurs at an estimated 4 weeks for BPTB and 8 weeks for 4HS [15]. At this point, the surgical fixation becomes non-load-bearing and the ACL construct stiffness is the same as the stiffness of the graft.
These three fixation types differ in that friction methods can elongate by slippage between the graft and the interference screw-based friction device or by slippage between the screw and the bone tunnel. WSP, on the other hand, can elongate if the weave tightens within the graft, the knot slips, or if plastic deformation of the sutures occur.
Loosening of friction tibial fixation devices after cyclic loading has been extensively studied experimentally [3, 5, 6, 8, 10, 11, 13, 17–19, 25]. However, whipstitch-post loosening has been little studied. A literature search uncovered only two papers that looked at whipstitch-post fixation [11, 13]. However, both studies provided only a low number of cycles overall, particularly in the range of loads encountered in typical 0 –3 month post-operative activities. This is especially remarkable since WSP was the first widely used soft tissue fixation method [4] and is still one of the most widely used today. It is also quite common for surgeons using friction fixation to back up this fixation with whip-stitch fixation [21]. It is the purpose of this paper to test the hypothesis that loosening of the WSP construct after cyclic loading is minimal and comparable to the lowest loosening values found with other tibial fixation methods.
Methods
Cadaver specimen preparation
Gracilis and semitendinosus tendon grafts were harvested from eight human cadaveric knees (mean age 72 ± 16 years, range 41–90 years) obtained from three different anatomical gift foundations (LifeLegacy Foundation, Phoenix, AZ; ScienceCare Anatomical, Phoenix, AZ; IIAM, Jessup, PA). After harvest, the grafts were wrapped in gauze soaked with normal saline, and frozen to −20°C. Prior to preparation and testing, the tendons were thawed overnight at room temperature. A large, blunt curette was used to remove all extraneous muscle and soft tissue from each tendon. The ST and Gr tendons were overlapped to form eight double thickness tendon grafts. The free ends of each tendon were whipstitched with No. 2 Ultrabraid suture (Smith and Nephew Endoscopy, Andover, MA) using the surgical technique described below and seen in the accompanying video. Normal saline was used to keep the specimens moist during all phases of preparation and testing.
Tensile testing of cadaveric tendons
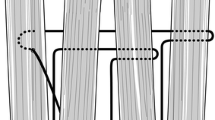
The tendon constructs were tested under cyclic loading conditions in tension on a servohydraulic materials testing system (Model 8521; Instron Corp., Canton, MA). The total test construct length was set at approximately 100 mm. The axilla of the doubled tendons was placed over a metal hook connected to the load cell of the material testing system (Fig. 1). The loose sutures extending from the gracilis and semitendinosus tendons were wrapped around a pneumatic gripping system specifically designed for suture testing. A 50 N preload was then applied.
Infrared reflective 10 mm diameter spherical markers were attached to the graft axilla hook and the suture clamp. In addition, a 10 mm marker was sewn onto the hamstring graft just above the last whipstitch throw using a 0 Ethibond suture and a 6 mm hemi-spherical marker was attached to the four suture legs immediately below the end of the tendons using adhesive tape. A video motion analysis system (SMART; BTS Bioengineering, Padova, Italy) was used to determine the amount of graft-suture slippage by measuring changes in position between the marker on the hamstring graft and the marker on the suture legs before and after cyclic loading. Pre- and post-cyclic marker measurements were recorded with the graft under similar tensile load.
The graft constructs were loaded to 200 N and held for 30 s. The load was then dropped to 145 N and the construct was cycled from 70 to 220 N at a rate of 1 Hz for 1,000 cycles. The construct was then returned to 145 N load. This test protocol was used to simulate the loading protocol used by Coleridge and Amis [3]. The amount of graft-suture slippage was determined by subtracting the distance the suture marker moved due to cyclic loading from the distance the graft marker moved due to cyclic loading. Pre- and post-cyclic marker positions were measured with a 145 N load applied to the graft construct. All measurements were made with a digital micrometer to two decimal places. The accuracy of the digital micrometer is 0.0001 mm.
We assessed the mean error of the video motion analysis system by moving retro-reflective markers to a known distance using a digital micrometer. We displaced two markers by increments of 0.2 mm between the values of 0 and 3 mm in the vertical direction and measured their displacement with the cameras positioned and oriented as they were during the in vitro cyclic load experiments. Measurement error was determined by calculating the absolute values of the difference between known displacement and displacement measured using the video system at each position for the two markers. The mean measurement error of the video motion analysis system was determined to be 0.0207 mm.
Whipstitch surgical technique
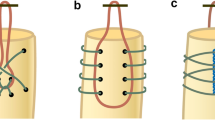
Whipstitches of number 5 braided nonabsorbable suture were used to tubularize the tendons. One whipstitch was put in the common semitendinosus/gracilis insertion. The other whipstitch was put in the overlapped proximal ends of the semitendinosus/gracilis. If a quadruple semitendinosus was used, the two free ends were whipstitched and another whipstitch was put in the axilla of the tendon with a strong tension held on it to equilibrate length. The whipstitches tubularize the tendons. The key technical point is to pull the opposing suture ends with very strong tension periodically to eliminate all slack in the graft. The technique for semitendinosus/gracilis is shown in Figs. 2, 3 and 4 and also in the accompanying real time video. The technique is performed more slowly to allow adequate visualization for the video. Previous studies (C. Prodromos, unpublished data) have shown that a minimum of three passes of suture down and back on the tendon is required to enable the graft tendon interface pullout strength to surpass the rupture strength of the suture.
Results
Cadaveric cyclic loading studies (Table 1)
All grafts successfully underwent the cyclic loading regimen. The mean elongation of the eight grafts after cyclic loading was 1.13 mm. The standard deviation was 0.32 mm. The range was a minimum elongation of 0.66 and a maximum of 1.64 mm.
Discussion
The mean elongation rate of 1.13 mm is among the lowest reported for any soft tissue tibial fixation system [3, 5, 6, 8, 10, 11, 13, 17–19, 25]. These laboratory results thus validate the hypothesis that the whipstitch-post method can produce excellent stability as part of ACL reconstruction.
While excellent results can be achieved with the use of interference type systems [22], we feel that devices that rely on friction are inherently less reliable for smooth compressible soft tissue grafts than they are for the rough surfaced, far less compressible bone plugs found in bone patellar tendon bone (BPTB) grafts. In contrast, whipstitches obtain tight purchase on each graft strand without reliance on friction and also allow individual tensioning. We feel this method is inherently better suited to soft tissue grafts.
To compare these biomechanical results to other methods of tibial fixation, a diligent computerized literature search was performed and data obtained. Table 1 shows the WSP method results in comparison with these other studies. The study by Coleridge and Amis [3] produced the lowest elongation rates for a study with a high number of cyclic load episodes. This study used an identical preload of 50 N and an identical cyclically applied load from 70 to 220 N with an identical rate of 1 Hz also for 1,000 cycles. Thus, while subtle testing methodology differences may exist, the principal testing parameters between the groups are identical such that we believe it is useful to compare results between the studies. The five devices tested in that study (all of which were friction devices) had elongations ranging from 0.69 to 1.3 mm and were statistically identical to each other. The mean WSP elongation of 1.13 from the eight grafts in this study ranked in the middle of those values and was also statistically identical to them (all P values > 0.05) (Table 1). The standard deviation of the WSP was lower than the SDs of all the devices in that study, indicating high consistency. Even more importantly, the maximum elongation for the WSP technique was the lowest of all the devices and the only one under 2 mm. The maximum elongation is even more important than the mean because it is indicative of possibly failed grafts.
Our study produced peak stresses of 220 N and was the first WSP study designed to simulate activities of daily living or light rehab through a high number of moderate strain episodes. Several studies [14, 23] have shown that stresses on the ACL for these activities seldom exceed 220 N. Thus, our results should be directly applicable to the clinical situation. Two other studies have examined WSP fixation but employed very different experimental designs that we feel do not mimic the clinical situation. Magen et al. [13] cycled grafts only 11 times per test. Each test had increasing increments of 50 N tension. Thus, at 250 N, each graft would have seen only 55 cycles, and at 500 N only 110 cycles. Their protocol is thus more a test of load to failure than cyclic loading compared to our study of 1,000 cycles at peak 220 N. The study by Krappinger et al. [11] used formalin-fixed grafts, which introduces a large potential source of error. They had a total of only 200 cycles for each graft. In addition, they used a peak stress of only 75 N, which is significantly less than which is experienced by the ACL in activities of daily living.
A limitation of the study is that the graft constructs were not cycled at higher loads or stressed until breakage. But, except in cases of the severely traumatized knee or the knee undergoing unusually aggressive rehabilitation, higher stress levels are extremely unusual in the clinical situation during the first 2 months postoperatively when the fixation devices are primarily responsible for holding the graft. Therefore, testing with higher forces was considered clinically irrelevant and was not done.
A second limitation of this study is the use of only eight tendon constructs. However, this number is also the same as that used by Coleridge and Amis in their study. A power calculation found that the tests had an 80% power to detect a difference in graft slippage of 1.17 mm (SD = 0.77) with 95% confidence interval. So, it is not likely that these tests missed a clinically significant difference in performance. 1.17 mm is the threshold for clinical significance calculated by Coleridge and Amis.
Another limitation is that an actual cortical screw in bone was not used to anchor the sutures. The high rigidity and strength of fixation of a stainless screw in cortical bone is well established [24] and not in question. Cadaveric bone is known to be softer than that seen in vivo and any results obtained, if we had chosen to use it, would have been suspect. The use of a stainless steel bar more closely approximates the rigidity of human cortical bone than any cadaveric or animal bone model we could have used. Additionally, tying knots around the screw instead of clamping the sutures would have added potential motion. By eliminating the screw and knots, we focused this study on the reliability of the whipstitch weave. However, the elimination of knots did not allow us to measure any slippage that might have occurred through knot loosening.
Number 2 ultrabraid suture was used in this study. The material properties of heavy braided polyester sutures have been characterized [26] and are relatively similar. In the clinical situation, number 2 or number 5 sutures are always used. Any of the available sutures of this size would thus be expected to give similar results although small differences might occur from the reported results if a different suture were used. However, because the second generation sutures such as ultra-braid are stronger than first generation sutures such as Ethibond (Ethicon, Somerville, NJ), we would recommend using a number 5 suture if a first generation suture is used since it would more closely approximate the strength of the second generation number 2 suture used in this study.
It should be noted that the excellent laboratory results of this study mirror the reported clinical results. In a large study of four-strand hamstring ACL reconstruction using exclusively WSP fixation, the mean 1 mm KT-1000 SSD is the lowest reported for a semitendinosus-gracilis study [20]. Also, in a large meta-analysis [21], WSP was associated with high rates of clinical stability. Finally, the 4HS study with the highest arthrometric stability [4] also used exclusively WSP fixation.
Conclusion
Whipstitch-post fixation produced low levels of elongation after cyclic loading comparable to the lowest reported values for tibial fixation methods. This would be expected to be clinically important since tibial fixation is generally felt to be the “weakest link” in the ACL reconstruction “chain”.
References
Bartz RL, Mossoni K, Tyber J et al (2007) A biomechanical comparison of initial fixation strength of 3 different methods of anterior cruciate ligament soft tissue graft tibial fixation: resistance to monotonic and cyclic loading. Am J Sports Med 35:949–954
Brown CH Jr, Darwich N (2007) Intratunnel tibial fixation of soft tissue anterior cruciate ligament grafts: graft sleeve and tapered screw. In: Prodromos CC (ed) The anterior cruciate ligament: reconstruction and basic science. Elsevier, Philadelphia, pp 330–340
Coleridge SD, Amis AA (2004) A comparison of five tibial-fixation systems in hamstring-graft anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 12:391–397
Cooley VJ, Deffner KT, Rosenberg TD (2001) Quadrupled semitendinosus anterior cruciate ligament reconstruction: 5-year results in patients without meniscus loss. Arthroscopy 17:795–800
Ferretti A, Conteduca F, Labianca L et al (2005) Evolgate fixation of doubled flexor graft in anterior cruciate ligament reconstruction: biomechanical evaluation with cyclic loading. Am J Sports Med 33:574–582
Giurea M, Zorilla P, Amis AA et al (1999) Comparative pull-out and cyclic-loading strength tests of anchorage of hamstring tendon grafts in anterior cruciate ligament reconstruction. Am J Sports Med 27:621–625
Gobbi A, Tuy B, Mahajan S et al (2003) Quadrupled bone-semitendinosus anterior cruciate ligament reconstruction: a clinical investigation in a group of athletes. Arthroscopy 19:691–699
Harvey AR, Thomas NP, Amis AA (2003) The effect of screw length and position on fixation of four-stranded hamstring grafts for anterior cruciate ligament reconstruction. Knee 10:97–102
Höher J, Scheffler SU, Withrow JD et al (2000) Mechanical behavior of two hamstring graft constructs for reconstruction of the anterior cruciate ligament. J Orthop Res 18:456–461
Kousa P, Järvinen TL, Vihavainen M et al (2003) The fixation strength of six hamstring tendon graft fixation devices in anterior cruciate ligament reconstruction part ii: tibial site. Am J Sports Med 31:182–188
Krappinger D, Kralinger FS, El Attal R et al (2007) Modified prusik knot versus whistitch technique for soft tissue fixation in anterior cruciate ligament reconstruction: a biomechanical analysis. Knee Surg Sports Traumatol Arthrosc 15:418–423
Liu-Barba D, Howell SM, Hull ML (2007) High-stiffness distal fixation restores anterior laxity and stiffness as well as joint line fixation with an interference screw. Am J Sports Med 35:2073–2082
Magen HE, Howell SM, Hull ML (1999) Structural properties of six tibial fixation methods for anterior cruciate ligament soft tissue grafts. Am J Sports Med 27:35–43
Markolf KL, Gorek JF, Kabo JM et al (1990) Direct measurement of resultant forces in the anterior cruciate ligament. An in vitro study performed with a new experimental technique. J Bone Joint Surg Am 72:557–567
Milano G, Mulas PD, Sanna-Passino E et al (2005) Evaluation of bone plug and soft tissue anterior cruciate ligament graft fixation over time using transverse femoral fixation in a sheep model. Arthroscopy 21:532–539
Namkoong S, Heywood CS, Bravman JT et al (2006) The effect of interference screw diameter on soft tissue graft fixation. Bull Hosp Jt Dis 63:153–155
Nurmi JT, Järvinen TL, Kannus P et al (2002) Compaction versus extraction drilling for fixation of the hamstring tendon graft in anterior cruciate ligament reconstruction. Am J Sports Med 30:167–173
Nurmi JT, Kannus P, Sievänen H et al (2003) Compaction drilling does not increase the initial fixation strength of the hamstring tendon graft in anterior cruciate ligament reconstruction in a cadaver model. Am J Sports Med 31:353–358
Nurmi JT, Sievänen H, Kannus P et al (2004) Porcine tibia is a poor substitute for human cadaver tibia for evaluating interference screw fixation. Am J Sports Med 32:765–771
Prodromos CC, Han YS, Keller BL et al (2005) Stability results of hamstring anterior cruciate ligament reconstruction at 2- to 8-year follow-up. Arthroscopy 21:138–146
Prodromos CC, Joyce BT, Shi K et al (2005) A meta-analysis of stability after anterior cruciate ligament reconstruction as a function of hamstring versus patellar-tendon graft and fixation type. Arthroscopy 21:1202–1208
Scranton PE Jr, Bagenstose JE, Lantz BA et al (2002) Quadruple hamstring anterior cruciate ligament reconstruction: a multicenter study. Arthroscopy 18:715–724
Shelburne KB, Pandy MG (1998) Determinants of cruciate-ligament loading during rehabilitation exercise. Clin Biomech (Bristol, Avon) 13:403–413
To JT, Howell SM, Hull ML (1999) Contributions of femoral fixation methods to the stiffness of anterior cruciate ligament replacements at implantation. Arthroscopy 15:379–387
Weimann A, Rodieck M, Zantop T et al (2005) Primary stability of hamstring graft fixation with biodegradable suspension versus interference screws. Arthroscopy 21:266–274
Wüst DM, Meyer DC, Favre P et al (2006) Mechanical and handling properties of braided polyblend polyethylene sutures in comparison to braided polyester and monofilament polydioxanone sutures. Arthroscopy 22:1146–1153
Yasuda K, Kondo E, Ichiyama H et al (2004) Anatomic reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon grafts. Arthroscopy 20:1015–1025
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material (mpg 91.4 MB)
Rights and permissions
About this article
Cite this article
Prodromos, C.C., Hecker, A., Joyce, B. et al. Elongation of simulated whipstitch post anterior cruciate ligament reconstruction tibial fixation after cyclic loading. Knee Surg Sports Traumatol Arthrosc 17, 914–919 (2009). https://doi.org/10.1007/s00167-009-0761-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-009-0761-9