Abstract
Purpose
The purpose of this study was to compare the outcomes of arthroscopic transtibial single-bundle posterior cruciate ligament reconstruction using autologous patellar tendon and hamstring tendon grafts.
Methods
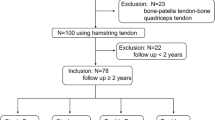
From 1998 to 2007, 59 patients with symptomatic isolated posterior cruciate ligament injury were included in this retrospective study. Twenty-five knees were reconstructed using bone-patellar tendon-bone graft, and 34 knees were reconstructed using hamstring graft. In both groups, surgical techniques were similar, except material of fixation screws. Patients were evaluated pre-operatively and post-operatively at the latest follow-up with several parameters, including symptoms, physical examination, outcome satisfaction, functional scores, radiography and complications.
Results
Average follow-up period was 51.6 months in patellar tendon group and 51.1 months in hamstring tendon group. Significantly more kneeling pain (32 vs. 3 %), squatting pain (24 vs. 3 %), anterior knee pain (36 vs. 3 %), posterior drawer laxity and osteoarthritic change were shown in patellar tendon group than in hamstring tendon group post-operatively. No significant differences were found in other parameters between both groups.
Conclusions
Several shortcomings, including anterior knee pain, squatting pain, kneeling pain and osteoarthritic change, have to be concerned when using patellar tendon autograft. In conclusion, hamstring tendon autograft may be a better choice for transtibial tunnel PCL reconstruction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Posterior cruciate ligament (PCL) injuries constitute about 1 to 44 % of all acute ligamentous knee injuries [26, 28]. Treatment of PCL injury is still controversial [11, 22]. Some studies have shown that conservative treatment can achieve good results [4, 16, 29, 31], whereas other studies have demonstrated that surgical reconstruction leads to good functional outcomes [6, 13, 15, 17, 27, 34, 35]. Many reconstruction methods have been described in the literature [6, 12, 13, 15, 17, 27, 34, 35]. There are some controversies, such as single or double bundles [13, 15, 34, 35], transtibial or tibial inlay technique [6, 15, 17, 27]. One of the interesting issues is graft selection. Both autograft and allograft can be chosen. Patellar tendon and hamstring tendon grafts are frequently used. In the literature, the maximum strength of hamstring tendon graft is not less than patellar tendon graft [12]. However, there are some concerns with the use of patellar tendon graft, including anterior knee pain, tenderness over the bony defects and problems with kneeling. Furthermore, there are risks of patellar fracture and weakening of the extensor mechanism, which acts as a synergist to the PCL [12]. Reviewing the literature, there has been no study focusing on comparison of using patellar tendon and hamstring tendon grafts in single-bundle PCL reconstruction with arthroscopic transtibial technique. The purpose of this study was to compare the outcomes of arthroscopic transtibial single-bundle PCL reconstruction using autologous patellar tendon and hamstring tendon grafts. The hypothesis of this study is that more anterior knee pain and kneeling pain appear with the use of autologous patellar tendon graft.
Materials and methods
From 1998 to 2007, 59 patients with isolated PCL injury were included in this retrospective study. This study had been approved by the ethical committees related to the institution in which this study was performed. Patients with combination of meniscal, chondral or other ligamentous injury were excluded according to physical examination, magnetic resonance imaging (MRI) and diagnostic arthroscopy. Inclusion criteria were (1) persistent symptoms, such as pain and giving way that bothered the patients and (2) persistent posterior laxity greater than or equal to grade two, which were not improved by conservative treatment (medication and physical therapy) for more than 6 months. Twenty-five knees were reconstructed using bone-patellar tendon-bone (PT) graft from 1998 to 2002, and 34 knees were reconstructed using hamstring (HT) graft from 2002 to 2007. All surgeries were carried out by same surgeon. All grafts were autologous harvested from ipsilateral knee. In both groups, surgical techniques were similar, except material of fixation screws. All patients underwent same rehabilitation protocol after surgery.
Surgical techniques
The patient was positioned in supine on the operation table. Under general anesthesia, physical examination of the injured knee was performed comparing with the noninjured knee. A tourniquet was applied on the surgical leg, which was then prepared and draped sterilely. A diagnostic arthroscopic examination was conducted through the anterolateral and anteromedial portals to identify PCL injury and to exclude any meniscal or chondral lesions.
Grafts were harvested and prepared before tunnel creation. Outside-in method was used for both tibial and femoral tunnels creation. A posteromedial portal and a posterolateral portal were created first. Then, a posterior trans-septal portal was established for assistance of tibial tunnel preparation [2]. The posterior trans-septal portal provided an excellent visualization of the PCL tibial attachment. Thus, the remnant of the original PCL was easily preserved to be healed with the graft as an integrated structure. After posterior capsule elevation, the tibial drill guide was introduced through the anteromedial portal to guide the creation of tibia tunnel. The entry point of tibial guide pin was on the anteromedial aspect of proximal tibia about 1–2 cm distal to tibial tubercle. In PT group, a skin incision about 1 cm was made to expose the entry point. In HT group, the entry point was almost exposed in the graft-harvesting wound. The exit point of tibial guide pin was about 13–14 mm distal to the medial plateau surface and inferolateral to the anatomic PCL tibial insertion site visualized in the posteromedial portal. After placing tibial guide pin appropriately, the tibial tunnel was created using a sized cannulated reamer.
The femoral drill guide was inserted through the anteromedial portal to guide the creation of femoral tunnel. The entry point of femoral guide pin was on the femoral medial epicondyle, which was approached via anteromedial aspect of the distal femur. The exit point of femoral guide pin was on the center of the footprint of PCL anterolateral bundle visualized in the anterolateral portal. When knee flexed in 90°, it is usually about 6–8 mm posterior to the margin of joint cartilage and in the direction of 1 o’clock for right knee and 11 o’clock for left knee. The femoral tunnel was then created with a sized cannulated reamer.
A self-made loop was passed from the tibial tunnel through the knee joint to the femoral tunnel. The traction sutures of the grafts were attached to the loop, and the grafts were then pulled into position. The graft in femoral tunnel was fixed first with an interference screw, which was of the same size as the tunnel diameter. Then, the graft was tensioned in 70° of knee flexion followed by an anterior drawer force applied on the proximal tibia. Under tension, the graft in tibial tunnel was fixed with an interference screw with the same diameter of the tunnel. Metal interference screws (Arthrex, Naples, Florida) were used in PT group (Fig. 1), while bio-absorbable interference screws (Linvatec, Largo, Florida) were used in HT group (Fig. 2). The fixation in each tunnel was further secured by a post-screw with a washer.
After PCL reconstruction, the graft was visualized with arthroscopy, and knee stability was tested again. The knee was then immobilized in a long leg splint with a posterior tibia support to prevent posterior sagging post-operatively.
The day after operation, a knee brace, instead of long leg splint, was used and locked in full extension for 3 weeks. During the first 3 weeks crutches were used with non-weight bearing, and isometric muscle strengthening exercises were performed. In 4–6th week, partial weight bearing was allowed with the knee in full extension; the knee brace was unlocked three times daily for progressive passive range of motion. Active range of motion was allowed after 6 weeks from surgery. Full range of motion was expected in 3 months after surgery. After 2nd month, crutches were discontinued, and strengthening and range of motion exercises were performed progressively. Once the patient achieved 120° of knee flexion, close chain exercises were instituted. Open chain exercises were instructed after 3 months from surgery. Deep squatting was prohibited for 6 months after the surgery. Jogging and light sports were allowed after 6 months, whereas return to heavy labor or sports were allowed after 6–9 months after surgery.
Patients were evaluated pre-operatively (pre-op) and post-operatively (post-op) at the latest follow-up with several parameters, including symptoms, physical examination, outcome satisfaction, functional scores, radiography and complications. Symptoms were composed of pain, kneeling pain, squatting pain, anterior knee pain, instability, swelling and weakness. Pain was measured using visual analogue scale (VAS), while the others were graded as yes or no. Physical examination consisted of posterior drawer test, range of motion (ROM), thigh girth difference and KT1000 (MEDmetric, San Diego, California) side-to-side difference (using quadriceps neutral angle). Posterior drawer test was graded as grade 0 (no laxity), grade 1 (laxity < 5 mm), grade 2 (laxity: 5 ~ 10 mm) and grade 3 (laxity > 10 mm) compared with another knee. Outcome satisfaction included patient’s and surgeon’s satisfaction, which were graded as poor, fair, good and excellent. Lysholm scores and international knee documentation committee (IKDC) were used as functional scores. Osteoarthritis (OA) was evaluated in radiography. OA was graded using Ahlbäck classification [1]. Stage I was defined as at most a slight reduction of the cartilage height. Stage II was defined as obliteration of the joint space. Stage III was defined as bone loss of ≦7 mm measured along the medial or lateral margins of the joint from a line perpendicular to the axis of the tibia and tangential to the unaffected articular surface. Stage IV was defined as bone loss >7 mm measured along the medial or lateral margins of the joint from a line perpendicular to the axis of the tibia and tangential to the unaffected articular surface. Stage V was defined as bone loss >7 mm with subluxation, defined as lateral displacement of the tibia by at least 10 mm in relation to the femur. All evaluations except outcome satisfaction were performed by same author other than the surgeon. Surgeon’s satisfaction was completed by the surgeon. The pre-op and post-op results of both groups were analyzed statistically using Student t test, Mann–Whitney U test and chi square test for continuous, ordinal and nominal data, respectively. Significance levels were set at 0.05.
Results
Demographic data are shown in Table 1. Average age was 26.8 years in PT group and 26.2 years in HT group. In PT group, 68 % were males and 32 % were females. In HT group, 79 % were males and 21 % were females. Injury mechanism included traffic (85 %) and sports injury (15 %). Average length of time prior to surgery was 9.2 months in PT group and 9.1 months in HT group. Average follow-up period was 51.6 months in PT group and 51.1 months in HT group. No differences were found between both groups statistically.
Pre-op and Post-op results of symptoms are presented in Table 2. There were no significant differences between both groups pre-operatively. Post-operatively, significantly more kneeling pain (32 vs. 3 %), squatting pain (24 vs. 3 %) and anterior knee pain (36 vs. 3 %) were shown in PT group than in HT group (P = 0.002, P = 0.013 and P = 0.001, respectively). No significant differences were found in pain (VAS), swelling and weakness between both groups. There was no symptom of instability post-operatively.
Pre-op and Post-op results of physical examination are presented in Table 3. There were no significant differences between both groups pre-operatively. Post-operatively, posterior drawer test showed significant difference between both groups (P = 0.011). Sixteen percent of knees in PT group and 47 % of knees in HT group had no posterior laxity, whereas 68 % of knees in PT group and 47 % of knees in HT group presented grade 1 laxity. There were only 16 % of knees in PT group and 6 % of knees in HT group having grade 2 laxity. No grade 3 laxity was found in both groups. No significant differences were found in ROM, thigh girth difference and KT1000 side-to-side difference between both groups.
Patient’s and surgeon’s satisfaction were similar in both groups post-operatively, as shown in Table 4. Eighty-eight percent of patients in PT group and 97 % of patients in HT group were satisfied with good or excellent results.
Pre-op and Post-op results of functional scores are presented in Table 4. There were no significant differences between both groups pre-operatively. Post-operatively, average Lysholm scores were 91.9 in PT group and 93.1 in HT group, which showed no significant difference. Results of IKDC grading were also not significantly different between both groups.
Pre-op and Post-op results of radiographic OA change are presented in Table 4. There were no significant differences between both groups pre-operatively. Post-operatively, 64 % of knees in PT group and 38 % of knees in HT group were found with OA change (stage I, II and III), which was significantly different (P = 0.033).
No infection, thromboembolism, nerve injury, vascular injury, fracture or ligamentous injury was found in both groups post-operatively.
Discussion
Both PT and HT groups in our study achieved good results in clinical outcome, such as outcome satisfaction and functional scores. However, there are still some concerns which are discussed below.
In the literature, there has been no study comparing the outcomes of isolated PCL reconstruction between using patellar tendon and hamstring tendon autografts with same surgical technique (arthroscopic transtibial tunnel) and anatomy (single bundle). Only few studies have focused on comparison of the outcome between using patellar tendon and hamstring tendon autografts in PCL reconstruction with different surgical techniques and anatomy. Seon et al. [27] compared the clinical results of PCL reconstruction using hamstring autograft with transtibial tunnel technique and patellar tendon autograft with tibial inlay technique. They demonstrated that no significant differences were found between both groups which produced relatively good clinical results. Houe et al. [13] described the results of PCL reconstruction using either a patella bone-tendon-bone single-bundle autograft or hamstring double-bundle autografts. They concluded that both techniques could improve patients’ activity level and relieve symptoms, but no differences in outcome between both techniques were noted. However, in these studies, surgical techniques or anatomy were different between patellar tendon and hamstring tendon group. The outcomes might be influenced by different grafts, different surgical techniques, different reconstructed anatomy or all. It was difficult to find out how each parameter affected the outcomes, because there were so many independent variables. In our study, biases were reduced by same surgical technique and same reconstructed anatomy; thus the effect of graft choice in PCL reconstruction could be ascertained clearly.
Significantly more post-op kneeling pain, squatting pain and anterior knee pain in PT group were found in our study. Seon et al. [27] reported one of 21 cases (4.8 %) using hamstring autograft with transtibial tunnel technique and four of 22 cases (18.2 %) using patellar tendon autograft with tibial inlay technique had anterior knee pain. Houe et al. [13] described that two patients had squatting pain, but they did not mention what grafts were used for these patients. Contrary to few studies comparing the outcomes of PCL reconstruction using patellar tendon and hamstring tendon autografts, many studies have compared the same issue in anterior cruciate ligament (ACL) reconstruction [7, 8, 23]. More anterior knee pain, squatting pain and kneeling pain were shown with use of patellar tendon graft in some of these ACL studies [7, 23]. These are compatible with the results in our study. In general, anterior knee pain, squatting pain and kneeling pain are thought as harvest site morbidities [5, 21]. However, there are some different opinions. Shelton et al. [30] found that anterior knee pain was equally common after ACL reconstruction using bone-patellar tendon-bone autograft and allograft. In other words, anterior knee pain probably did not result from harvest site morbidity. The reasons for anterior knee pain may be quadriceps weakness, loss of motion and inadequate rehabilitation [9, 25].
In both groups of our study, post-operative stability seemed consistent with several PCL studies [6, 15, 27]. Most of knees under posterior drawer test and KT1000 arthrometer examination post-operatively represented less than grade 2 and smaller than 5 mm laxity, respectively. While no significant difference was found in KT1000 arthrometer examinations between both groups, there were significantly more knees with posterior laxity in PT group than in HT group when doing posterior drawer test. The statistical differences were the proportions of laxity of each grade. Most post-operative posterior laxity in PT group belonged to grade 1 (68 %), while in HT group, proportions of grade 0 and grade 1 were equal (47 %). Although no significant difference was found in KT1000 arthrometer examinations between both groups; there was a trend similar to the outcome of posterior drawer test when the measured results of KT1000 were transformed from continuous variables to ordinal variables (grading). In PT group, most post-operative side-to-side difference (60 %) belonged to 3 ∼ 5 mm, while in HT group, most post-operative side-to-side difference (56 %) belonged to 1 ∼ 3 mm. Hence, the inference was that PT group might have increased post-operative posterior laxity comparing with HT group. Quadriceps strength may be a possible affecting factor. Li et al. [19] demonstrated that increasing in quadriceps loading on tibia would decrease posterior tibial translation, whereas increasing in hamstring loading on tibia would increase posterior tibial translation. In PT group, probable quadriceps weakness with normal hamstring loading may increase posterior tibial translation. Despite quadriceps strength, hamstring strength may also influence the stability. In HT group, probable hamstring weakness with normal quadriceps loading may decrease posterior tibial translation. Besides, graft fixation methods may have an effect on the stability. In both femoral and tibial tunnels, stiffness of hamstring graft fixed with bioabsorbable screw is greater than stiffness of bone-patellar tendon-bone graft fixed with metal screw [12]. This means that more forces are needed to deform the graft in HT group. More studies in the future with more evidences will be needed to stand for these.
Osteoarthritic change, which may affect prognosis, is an important and most concerning issue in PCL injury [14]. Under arthroscopy, Strobel et al. [31] reported that 57.3 % of patients with isolated PCL injuries had articular cartilage lesions. The rate of articular degeneration may also increase with time from injury [4, 29]. Degenerative changes of PCL injured knees have been reported in several studies [16, 32, 34]. Wang et al. [33] noted that rate of OA change is proportional to severity of posterior laxity, even after PCL reconstruction. Jari et al. and Besier et al. [3, 14] pointed out that increased contact pressure in knee could be one of the mechanisms resulting in degeneration. Some studies indicated that more laxity led to more contact pressure, therefore, contributing to more knee OA [10, 18, 20, 24]. In this study, the incidence of OA changes showed significant differences between both groups post-operatively. This could imply a trend of more degeneration using patellar tendon grafts for PCL reconstruction. However, the relationship between the choice of graft and the incidence of OA remained to be seen through a long-term follow-up.
There are several strengths in this study, including same surgeon, same surgical technique, same reconstructed anatomy and variation of only graft choice and graft fixation. The limitations of this study include intermediate-term, small study population size and retrospective study. A prospective, randomized controlled study with a larger population sample, for long-term results, will be conducted in the future.
Conclusions
For symptomatic patients with isolated PCL injuries, reconstruction with both patellar tendon and hamstring tendon autografts can yield good functional outcomes. Nonetheless, several shortcomings, including anterior knee pain, squatting pain, kneeling pain and OA change, have to be concerned when using patellar tendon graft. In conclusion, hamstring tendon autograft may be a better choice for transtibial tunnel PCL reconstruction.
References
Ahlbäck S (1968) Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh) 277:7–72
Ahn JH, Ha CW (2000) Posterior trans-septal portal for arthroscopic surgery of the knee joint. Arthroscopy 16:774–779
Besier TF, Gold GE, Beaupré GS et al (2005) A modeling framework to estimate patellofemoral joint cartilage stress in vivo. Med Sci Sports Med 37:1924–1930
Boynton MD, Tietjens BR (1996) Long-term followup of the untreated isolated posterior cruciate ligament-deficient knee. Am J Sports Med 24:306–310
Cole DW, Ginn TA, Chen GJ et al (2005) Cost comparison of anterior cruciate ligament reconstruction: autograft versus allograft. Arthroscopy 21:786–790
Cooper DE, Stewart D (2004) Posterior cruciate ligament reconstruction using single-bundle patella tendon graft with tibial inlay fixation: 2- to 10- year follow-up. Am J Sports Med 32:346–360
Corry IS, Webb JM, Clingeleffer AJ et al (1999) Arthroscopic reconstruction of the anterior cruciate ligament: a comparison of patellar tendon autograft and four-strand hamstring tendon autograft. Am J Sports Med 27:444–454
Freedman KB, D’Amato MJ, Nedeff DD et al (2003) Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med 31:2–11
Fu F, Christel P, Miller MD et al (2009) Graft selection for anterior cruciate ligament reconstruction. Instr Course Lect 58:337–354
Gill TJ, DeFrate LE, Wang C et al (2004) The effect of posterior cruciate ligament reconstruction on patellofemoral contact pressures in the knee joint under simulated muscle loads. Am J Sports Med 32:109–115
Grassmayr MJ, Parker DA, Coolican MRJ et al (2008) Posterior cruciate ligament deficiency: biomechanical and biological consequences and the outcomes of conservative treatment. A systematic review. J Sci Med Sport 11:433–443
Höher J, Scheffler S, Weiler A (2003) Graft choice and graft fixation in PCL reconstruction. Knee Surg Sports Traumatol Arthrosc 11:297–306
Houe T, Jørgensen U (2004) Arthroscopic posterior cruciate ligament reconstruction: one- vs. two-tunnel technique. Scand J Med Sci Sports 14:107–111
Jari S, Shelbourne KD (2001) Natural history and nonoperative treatment of posterior cruciate ligament injuries. Oper Tech Sports Med 9:53–59
Jung YB, Tae SK, Jung HJ et al (2004) Replacement of the torn posterior cruciate ligament with a mid-third patellar tendon graft with use of a modified tibial inlay method. J Bone Joint Surg Am 86-A:1878–1883
Keller PM, Shelbourne KD, McCarroll JR et al (1993) Nonoperatively treated isolated posterior cruciate ligament injuries. Am J Sports Med 21:132–136
Kim SJ, Kim SH, Kim SG et al (2009) Comparison of the clinical results of three posterior cruciate ligament reconstruction techniques. J Bone Joint Surg Am 91:2543–2549
Li G, DeFrate LE, Zayontz S et al (2004) The effect of tibiofemoral joint kinematics on patellofemoral contact pressures under simulated muscle loads. J Orthop Res 22:801–806
Li G, Most E, DeFrate LE et al (2004) Effect of the posterior cruciate ligament on posterior stability of the knee in high flexion. J Biomech 37:779–783
MacDonald P, Miniaci A, Fowler P et al (1996) A biomechanical analysis of joint contact forces in the posterior cruciate deficient knee. Knee Surg Sports Traumatol Arthrosc 3:252–255
Miller SL, Gladstone JN (2002) Graft selection in anterior cruciate ligament reconstruction. Orthop Clin North Am 33:675–683
Peccin MS, Almeida GJ, Amaro J et al. (2005) Interventions for treating posterior cruciate ligament injuries of the knee in adults. Cochrane Database Syst Rev 18(2):CD002939
Pinczewski LA, Lyman J, Salmon LJ et al (2007) A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med 35:564–574
Ramaniraka NA, Terrier A, Theumann N et al (2005) Effects of the posterior cruciate ligament reconstruction on the biomechanics of the knee joint: a finite element analysis. Clin Biomech (Bristol, Avon) 20:434–442
Sachs RA, Daniel DM, Stone ML et al (1989) Patellofemoral problems after anterior cruciate ligament reconstruction. Am J Sports Med 17:760–765
Schulz MS, Russe K, Weiler A et al (2003) Epidemiology of posterior cruciate ligament injuries. Arch Orthop Trauma Surg 123:186–191
Seon JK, Song EK (2006) Reconstruction of isolated posterior cruciate ligament injuries: a clinical comparison of the transtibial and tibial inlay techniques. Arthroscopy 22:27–32
Shelbourne KD, Davis TJ, Patel DV (1999) The natural history of acute, isolated, nonoperatively treated posterior cruciate ligament injuries. A prospective study. Am J Sports Med 27:276–283
Shelbourne KD, Gray T (2002) Natural history of acute posterior cruciate ligament tears. J Knee Surg 15:103–107
Shelton WR, Papendick L, Dukes AD (1997) Autograft versus allograft anterior cruciate ligament reconstruction. Arthroscopy 13:446–449
Strobel MJ, Weiler A, Schulz MS et al (2003) Arthroscopic evaluation of articular cartilage lesions in posterior-cruciateligament- deficient knees. Arthroscopy 19:262–268
Torg JS, Barton TM, Pavlov H et al (1989) Natural history of posterior cruciate ligament-deficient knee. Clin Orthop 246:208–216
Wang CJ, Chen HS, Huang TW et al (2002) Outcome of surgical reconstruction for posterior cruciate and posterolateral instabilities of the knee. Injury 33:815–821
Wang CJ, Weng LH, Hsu CC et al (2004) Arthroscopic single- versus double-bundle posterior cruciate ligament reconstructions using hamstring autograft. Injury 35:1293–1299
Yoon KH, Bae DK, Song SJ et al (2005) Arthroscopic double-bundle augmentation of posterior cruciate ligament using split Achilles allograft. Arthroscopy 21:1436–1442
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, YC., Chen, SK., Liu, TH. et al. Arthroscopic transtibial single-bundle posterior cruciate ligament reconstruction using patellar tendon graft compared with hamstring tendon graft. Arch Orthop Trauma Surg 133, 523–530 (2013). https://doi.org/10.1007/s00402-013-1679-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-013-1679-8