Abstract
Purpose
To evaluate the results of combined anterior cruciate ligament (ACL) and anterolateral ligament (ALL) reconstruction in patients with chronic ACL injury. It was hypothesized that patients who underwent combined ACL and ALL reconstruction would exhibit less residual laxity and better clinical outcomes.
Methods
Two groups of patients were evaluated and compared retrospectively. Both groups consisted only of patients with chronic (more than 12 months) ACL injuries. Patients in group 1 underwent anatomical intra-articular reconstruction of the ACL and patients in group 2 underwent anatomic intra-articular ACL reconstruction combined with ALL reconstruction. The presence of associated meniscal injury, the subjective International Knee Documentation Committee (IKDC) and Lysholm functional outcome scores in the postoperative period, KT-1000 evaluation, the presence of residual pivot shift and graft rupture rate were evaluated.
Results
One hundred and one patients who underwent reconstruction of chronic ACL injuries were evaluated. The median follow-up was 26 (24–29) months for group 1 and 25 (24–28) months for group 2. There were no significant differences between groups regarding gender, age, duration of injury until reconstruction, follow-up time or presence of associated meniscal injuries in the preoperative period. Regarding functional outcome scores, patients in group 2 presented better results on both the IKDC (p = 0.0013) and the Lysholm (p < 0.0001) evaluations. In addition, patients in group 2 had better KT-1000 evaluation (p = 0.048) and a lower pivot shift rate at physical examination, presenting only 9.1% positivity versus 35.3% in the isolated ACL reconstruction (p = 0.011). Regarding re-ruptures, group 1 presented 5 (7.3%) cases, and group 2 presented no cases.
Conclusion
The combined ACL and ALL reconstruction in patients with chronic ACL injury is an effective and safety solution and leads to good functional outcomes with no increase in complication rate. The clinical relevance of this finding is the possibility to indicate this type of procedure when patients present with more than 12 months after injury for surgery.
Level of evidence
Level III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Although several studies about this subject were recently published, there is still some controversy regarding the anterolateral ligament (ALL). While the tibial insertion has been described consistently between the fibular head and Gerdy’s tubercle, the femoral insertion is still a topic of some debate, although more recent studies are describing it posterior and proximal to the lateral epicondyle. Furthermore, some authors are referring to the ALL as an extra-capsular structure, whereas others are referring to it as a structure in layer 3 according to Seebacher et al. [5, 12, 14, 15, 18, 34, 36, 38, 41]. Despite some controversy as well, biomechanical studies have shown that when there is a combined lesion of the anterior cruciate ligament (ACL) and the anterolateral structures, the ACL reconstruction alone does not restore normal knee biomechanics [1, 10, 23].
Following anatomical and biomechanical studies of the ALL, some research groups developed surgical techniques and started series of reconstructions of this structure combined with reconstruction of the ACL to obtain improvements in the clinical outcomes of treatment of anterior and anterolateral rotational instability of the knee [11, 21, 40]. To date, despite controversies in biomechanical studies, in vivo results have had a tendency to favor this type of combined ACL and ALL reconstruction [21, 39, 46]. One series of combined ACL and ALL reconstructions in a high-risk population found a lower graft rupture rate than the isolated ACL reconstructions that used a bone-patellar tendon-bone graft or a quadrupled hamstring tendon graft. Another randomized study showed an improvement in knee laxity measured using a KT-1000 arthrometer in patients with combined ACL and ALL reconstruction versus patients with isolated ACL reconstructions, although the other measured parameters were not significantly different [21, 39]. Rezende et al. [35] in a recent metanalysis showed that combined intra- and extra-articular ACL reconstruction provided marginally improved knee stability and comparable failure rates, but no difference in patient-reported functional outcomes scores when compared to isolated intra-articular reconstruction.
Despite the lack of evidence regarding indications for lateral extra-articular procedures, authors suggest to perform such a procedure in patients with high-demand sports activities associated with frequent rotational movements of the knee, young patients, high-grade ligamentous laxity, revision surgeries or cases of chronic ACL injury [9, 11, 21, 30, 31, 38,39,40, 44]. Subjects with chronic ACL deficiency have been shown to have a higher anterolateral laxity [30]. Nevertheless, in the existing ALL reconstruction studies, only a few patients with chronic ACL injuries were included, which makes it difficult to extrapolate the results found for this specific population [21, 39].
Thus, the aim of the present study is to evaluate the results of combined ACL and ALL reconstruction in patients with chronic ACL injury. The primary outcome will be residual laxity and functional scales will be used as secondary outcomes. It is clinically relevant, as no study has showed safety and potential efficacy of the ALL reconstruction in this specific population. It was hypothesized that patients who underwent combined ACL and ALL reconstruction would exhibit less residual laxity and better clinical outcomes. Clinical studies about ALL reconstruction are needed, as there is paucity of literature regarding its possible benefits, especially regarding this specific chronic ACL population, which was not studied in detail before.
Materials and methods
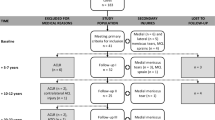
Between 2014 and 2015 patients with chronic ACL tears underwent combined ACL and ALL reconstruction. This group consisted only of patients with more than 12 months of injury, confirmed by clinical and imaging examinations and without associated peripheral ligament injuries apart from the anterolateral corner. Patients who required procedures for axis correction, treatment of chondral injuries, meniscal repair or larger meniscectomies with resection of more than 50% of the meniscus width were excluded from this analysis (Fig. 1). This group was compared to a control group with the same inclusion and exclusion criteria submitted to an isolated ACL reconstruction between January 2011 and June 2012 and evaluated in July 2014 (same follow-up period). The difference between enrollment period was due to the fact that combined ALL and ACL reconstruction as a routine procedure in chronic ACL cases was only started in our hospital since 2014.
The patients in group 1 (control) underwent anatomical intra-articular reconstruction of the ACL with a quadruple-hamstring tendon graft (double gracilis and double semitendinosus). Patients in group 2 (combined ACL and ALL reconstruction) underwent anatomic ACL reconstruction similar to those in group 1, with quadruple grafts (triple semitendinosus and simple gracilis). The difference between the groups, besides the ACL graft assembly, was that in the patients of group 2, the remaining gracilis was used for reconstruction of the ALL [15] (Fig. 2).
Clinical image of a left knee undergoing combined reconstruction of the anterior cruciate ligament (ACL) and anterolateral ligament (ALL). The remaining portion of the gracilis tendon that will be used for ALL reconstruction emerges from outside-in through the femoral tunnel of the ACL reconstruction
ALL reconstruction was performed with a surgical access to the lateral knee. After separation of the ITB, two 5 mm metal anchors were inserted with use of radioscopy, one at the posterior aspect, the lateral epicondyle and the other one between Gerdy’s tubercle and the fibular head, around 10 mm below the joint line [13]. The remaining gracilis from the ACL femoral tunnel was initially fixed to the femoral anchor and posteriorly to the tibial anchor, located between the Gerdy tubercle and the fibular head, approximately 7 mm distal from the articular cartilage of the lateral tibial plateau. The fixation of the graft in the tibia occurred close to full extension and neutral rotation (Fig. 3).
Clinical image of the anterolateral ligament (ALL) reconstruction of one right knee. An anchor is initially inserted into the anatomic site of the tibia, and the length of the gracilis graft of the ALL is checked (a). Next, the graft passes under the iliotibial band (ITB) and is fixed to the tibial anchor (b, c). After fixation, the ITB is sutured (d)
The rehabilitation protocol of the two groups was performed in the same way, no changes in any exercise or progression parameter was carried out due to the extra-articular reconstruction. No immobilization in the postoperative period was used, range of motion and quadriceps activation exercises from the first postoperative day and gait training with load progression as tolerated by the patient was stimulated.
In addition to the demographic data for similarity comparisons between the groups, the following were also assessed: the presence of associated meniscal injury, the intra-articular ACL graft diameter, the International Knee Documentation Committee (IKDC) and Lysholm functional outcome scores, KT-1000 arthrometer, the presence of residual pivot shift [25] and graft rupture rate.
The rupture rate was based on clinical instability and radiological criteria showing a new discontinuity of the graft. The pivot shift test is part of the regular follow-up protocol and was assessed by two examiners with experience in physical examination who were not involved in the surgical procedure. The most experienced examiner served as the primary examiner, and the second examiner was used to the correlation tests. The same examiners were used for clinical assessment in both patient groups.
IRB approval for this study was obtained at University of São Paulo (number 2.472.968) and informed consent was obtained.
Statistical analysis
Statistical analysis was performed using the Pearson’s Chi-Square test for categorical variables and t test or Wilcoxon rank-sum test for continuous variables. The inter-rater agreement for pivot shift test by the two examiners was performed using the kappa test. Statistical significance was considered when the p value was less than 0.05. All normally distributed continuous variables are reported as mean ± standard deviation and not normally distributed variables as median (interquartile range). No sample size calculation was performed before conducting the study, as all patients who met the inclusion criteria were included in this study. A post hoc power calculation revealed a power of 84% for analysis regarding residual pivot shift, 89% regarding subjective IKDC score and 97% regarding Lysholm score at least 2 years postoperative.
Results
One hundred and one patients who underwent reconstruction of chronic ACL injuries were evaluated according to the established criteria. Group 1 (control) consisted of 68 patients, and group 2 (combined ACL and ALL reconstruction) consisted of 33. There were no statistically significant differences between the groups with respect to baseline data and demographics (Table 1). Intra-articular graft diameter did not present any difference between groups as well.
At final follow-up, patients in group 2 presented better pivot shift (p = 0.011) and better results on both the IKDC (p = 0.0013) and the Lysholm (p < 0.0001) evaluations, indicating a better postoperative functional outcome in patients with combined ACL and ALL reconstruction. Other comparative data is shown in Table 2. The inter-examiner assessment of the physical examination specific for the pivot shift test by the kappa test was 0.716, which was considered substantial agreement.
Regarding the complications found, one patient in group 1 presented a hypertrophic scar on the thigh in the topography of the access to create the outside-in femoral tunnel, and one patient had a pretibial cyst in the ACL tunnel. One patient in group 2 presented femoral anchor loosening with irritation of the lateral soft parts of the knee that needed to be removed. None of the surgical cases in these series evolved with infection, and there were no cases of significant range of motion loss in any of the groups evaluated. In both groups, a significant number of patients presented temporary pain on the lateral side of the thigh due to incision and opening of the ITB, with complete resolution approximately 2–3 months after surgery and without causing problems for rehabilitation.
Discussion
The main finding of this study is that patients with chronic ACL injury who underwent combined intra- and extra-articular reconstruction showed better pivot shift and improvements in the functional outcome scores when compared to those submitted to isolated intra-articular reconstruction. In this way, they may benefit from this type of reconstruction.
Chronic ACL injuries present a difference in relation to the acute injuries, because they show a higher anterolateral laxity [28]. This instability is due to an anterior asymmetrical translation of the lateral tibial plateau [24, 28]. When there is injury or insufficiency of anterolateral structures, either by acute injury that does not heal properly or by the loosening resulting from an untreated ACL injury, isolated ACL reconstruction does not reestablish normal knee kinematics; thus, something more is required to treat these patients [23]. Ferretti et al. [7], in a series of 60 patients with acute ACL injury where the anterolateral structures were explored, found 90% of injuries associated with these structures. The healing potential of ALL is yet unknown, but given the percentage of residual pivot shift in the most diverse techniques used for ACL reconstruction, a portion of these anterolateral injuries likely do not heal adequately without surgery [2, 3, 8, 9, 20, 27, 31, 35, 39, 40, 44].
Studies with magnetic resonance imaging (MRI) showed that in series in which chronic ACL injuries are considered, the rates of ALL abnormalities found are greater than the cases of acute injuries, which may be explained by the greater demand of anterolateral structures in this population [4, 16, 17, 45]. MRI value in the assessment of anterolateral structures in chronic ACL injuries is still limited, because the healing potential and the cicatricial aspect of this structure are not known. In these situations, although MRI may serve as a guide, the final indication of combined reconstruction should be based on physical examination findings and physical activity characteristics of each patient.
The residual pivot shift findings in this study are consistent with findings in part of literature and favor the reconstruction of ALL in combination with ACL [20, 21, 39, 44]. Even though Jarvela et al. [26] showed almost all patients in their series with negative pivot shift with 10 years follow-up, Hussein et al. [20], in a study comparing the residual pivot shift rates after ACL reconstruction with isometric single-bundle, anatomic single-bundle and double-bundle, found rates of 58.3, 33.4 and 6.9%, respectively. The rate of 35.3% found in this study is similar to that found by those authors in a similar population of isolated intra-articular anatomical reconstruction. Finally, Sonnery-Cottet et al. [40], in the first described series of patients submitted to anatomic reconstruction of the ALL, and Ibrahim et al. [21], in a more recent series, presented residual pivot shifts of 8.4 and 9.4%, respectively, numbers close to this study for the same type of reconstruction. These similarities are important to validate the accuracy of this test, which is not always easy to perform with a non-anesthetized patient, even with adequate correlations between the examiners [29, 32].
In relation to the functional outcomes scales, this study shows different results from those reported in the literature by several authors [9, 19, 21, 35, 39]. As previously mentioned, all of these studies present variable populations with regard to the duration of injury. Thus, by isolating a more homogeneous sample of chronic injuries, such as in this study, the extra-articular reconstruction seems to also carry a subjective benefit, besides the objective improvement by the pivot shift test and the KT-1000 test. Zhang et al. [46] presented functional results of patients operated upon an average of 1.3 years after ACL injury. These authors also found a difference in functional outcomes scores at 6 and 12 months postoperatively, similar to the results found in this study.
In absolute numbers, the observed graft rupture rate was lower in group 2. Due to the low number of events, this result had no statistical significance. Sonnery-Cottet et al. [39], in a cohort of 502 patients, concluded that combined ACL and ALL reconstruction had 2.5-fold lower odds of failure than reconstruction of the patellar tendon and 3.1-fold lower odds than with hamstrings tendons. Trojani et al. [43] showed that adding the extra-articular reconstruction decreases the failure rate by more than 50%. Considering that, according to Inderhaug et al., the extra-articular reconstruction restores normal knee biomechanics in combined injuries of the ACL and the anterolateral structures, and, according to Engbretsen et al., decreases the forces in the ACL graft by approximately 43%, these results seem consistent [6, 23]. In the near future, increased follow-up time and larger sample size may lead to more accurate data on the rate of graft failure.
In this series, even with one more incision in the lateral region of the knee, the complication rate was very low, with only minor events, except for the cases of graft rupture, what proves the safety of this associated procedure. Extra-articular reconstruction did not cause any cases of loss of range of motion. The most significant complication was the release of an anchor that needed to be removed, without major consequences for the patient. In a recent series, Thaunat et al. [42]. showed that the rate of re-operations in the combined ACL and ALL reconstruction procedure was very low and was not different in relation to the isolated ACL reconstructions.
Even though this study showed possible benefits of extra-articular reconstruction in a clinical scenario of chronic ACL lesions, study performed by Noyes et al. [33] found no benefit of an ALL reconstruction. Furthermore, Schon et al. [37] found overconstraint of tibial rotation with this kind of reconstruction. Inderhaug et al. [22] also found increased contact pressure in the lateral compartment depending on the surgical technique used and the angle of the extra-articular graft fixation.
This study has limitations. The retrospective design, comparing patients treated on different time periods could be a source of bias due to differences of care, and the groups were neither randomized or matched, which could be a source of selection bias. Nevertheless, the groups were similar in regard to all recorded characteristics, all surgeries were performed in the same hospital by the same surgeons. The option of a historical control was due to the change in standard care in the hospital where this study was performed, as after 2013, combined extra-articular reconstruction was adopted for chronic ACL injuries. This study allowed empirical evaluation of this change of conduct, as there are no prior series demonstrating results on combined reconstructions in chronic injuries. In light of the current results, a randomized controlled trial is warranted to confirm these results, and this observational study will be useful in motivating, justifying and planning future trials.
The groups had considerably different sizes in this study, although similar proportions of chronic ACL tears included in this research in relation to total ACL surgeries were maintained, as all patients who met the inclusion and exclusion criteria were selected. There was a remarkably higher proportion of males in both groups, and this reflects the prevalence of ACL injuries in the studied population. Because of the small number of women in the study, there is a possibility that these results cannot be extrapolated for female patients, and future studies should address this topic.
Another limitation is the quantification of the pivot shift test performed manually and without anesthesia. It is known that the test is more accurate when performed with a completely relaxed patient, but this relaxation is not always possible in daily clinical practice. Because the correlation of the test was substantial between the examiners and similar to several studies in the literature, this design does not invalidate or interfere with the results obtained.
The main strength and clinical relevance of this study is the fact that it is the first series on combined ACL and ALL reconstruction on chronic ACL injuries, whereas previous studies had a small number of chronic lesions. The inclusion of the historical control group from before the introduction of extra-articular reconstruction, in the same setting and by the same surgeons, provide an adequate comparison for the technique outcomes. Sample size was adequate according to our estimation and to provide statistical significance to most of the observed differences. Furthermore, clinical studies regarding ALL reconstruction in combination to ACL reconstruction are important to show safety and efficacy of this kind of procedure compared to current literature regarding isolated ACL procedures.
Conclusion
The combined ACL and ALL reconstruction in patients with chronic ACL injury is an effective and safety solution and leads to good functional outcomes with no increase in complication rate.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- ALL:
-
Anterolateral ligament
- IKDC:
-
International Knee Documentation Committee
- ITB:
-
Iliotibial band
- MRI:
-
Magnetic resonance imaging
References
Amis AA (2017) Anterolateral knee biomechanics. Knee Surg Sports Traumatol Arthrosc 25:1015–1023
Ayeni OR, Chahal M, Tran MN, Sprague S (2012) Pivot shift as an outcome measure for ACL reconstruction: A systematic review. Knee Surg Sports Traumatol Arthrosc 20:767–777
Chambat P, Guier C, Sonnery-Cottet B, Fayard JM, Thaunat M (2013) The evolution of ACL reconstruction over the last 50 years. Int Orthop 37:181–186
Claes S, Bartholomeeusen S, Bellemans J (2014) High prevalence of anterolateral ligament abnormalities in magnetic resonance images of anterior cruciate ligament-injured knees. Acta Orthop Belg 80:45–49
Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J (2013) Anatomy of the anterolateral ligament of the knee. J Anat 223:321–328
Engebretsen L, Lew WD, Lewis JL, Hunter RE (1990) The effect of an iliotibial tenodesis on intraarticular graft forces and knee joint motion. Am J Sports Med 18:169–176
Ferretti A, Monaco E, Fabbri M, Maestri B, De Carli A (2017) Prevalence and classification of injuries of anterolateral complex in acute anterior cruciate ligament tears. Arthroscopy 33:147–154
Ferretti A, Monaco E, Labianca L, De Carli A, Conteduca F (2008) Double bundle or single bundle plus extra-articular tenodesis in ACL reconstruction? A CAOS study. Knee Surg Sports Traumatol Arthrosc 16:98
Ferretti A, Monaco E, Ponzo A et al (2016) Combined intra-articular and extra-articular reconstruction in anterior cruciate ligament-deficient knee: 25 years later. Arthroscopy 32:2039–2047
Guenther D, Irarrázaval S, Bell KM, Rahnemai-Azar AA, Fu FH, Debski RE, Musahl V (2017) The role of extra-articular tenodesis in combined ACL and anterolateral capsular injury. J Bone Jt Surg Am 99(19):1654–1660
Helito CP, Bonadio MB, Gobbi RG et al (2015) Combined intra- and extra-articular reconstruction of the anterior cruciate ligament: the reconstruction of the knee anterolateral ligament. Arthrosc Tech 4:e239–e244
Helito CP, Demange MK, Bonadio MB et al (2013) Anatomy and histology of the knee anterolateral ligament. Orthop J Sports Med 1:2325967113513546
Helito CP, Demange MK, Bonadio MB et al (2014) Radiographic landmarks for locating the femoral origin and tibial insertion of the knee anterolateral ligament. Am J Sports Med 42:2356–2362
Helito CP, do Amaral C Jr, Nakamichi YD et al (2016) Why do authors differ with regard to the femoral and meniscal anatomic parameters of the knee anterolateral ligament? Dissection by layers and a description of its superficial and deep layers. Orthop J Sports Med 4:2325967116675604
Helito CP, do Prado Torres JA, Bonadio MB et al (2017) Anterolateral ligament of the fetal knee. Am J Sports Med 45:91–96
Helito CP, Helito PV, Costa HP, Demange MK, Bordalo-Rodrigues M (2017) Assessment of the anterolateral ligament of the knee by magnetic resonance imaging in acute injuries of the anterior cruciate ligament. Arthroscopy 33:140–146
Helito CP, Helito PV, Leao RV, Demange MK, Bordalo-Rodrigues M (2017) Anterolateral ligament abnormalities are associated with peripheral ligament and osseous injuries in acute ruptures of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 25:1140–1148
Herbst E, Albers M, Burnham JM, Shaikh HS, Naendrup JH, FU FH, Musahl V (2017) The anterolateral complex of the knee: a pictorial essay. Knee Surg Sports Traumatol Arthrosc 25:1009–1014
Hewison CE, Tran MN, Kaniki N, Remtulla A, Bryant D, Getgood AM (2015) Lateral extra-articular tenodesis reduces rotational laxity when combined with anterior cruciate ligament reconstruction: a systematic review of the literature. Arthroscopy 31:2022–2034
Hussein M, van Eck CF, Cretnik A, Dinevski D, Fu FH (2012) Prospective randomized clinical evaluation of conventional single-bundle, anatomic single-bundle, and anatomic double-bundle anterior cruciate ligament reconstruction: 281 cases with 3- to 5-year follow-up. Am J Sports Med 40:512–520
Ibrahim SA, Shohdy EM, Marwan Y et al (2017) Anatomic reconstruction of the anterior cruciate ligament of the knee with or without reconstruction of the anterolateral ligament. Am J Sports Med 45:1558–1566
Inderhaug E, Stephen JM, Williams A, Amis AA (2017) Anterolateral tenodesis or anterolateral ligament complex reconstruction: effect of flexion angle at graft fixation when combined with ACL reconstruction. Am J Sports Med 45:3089–3097
Inderhaug E, Stephen JM, Williams A, Amis AA (2017) Biomechanical comparison of anterolateral procedures combined with anterior cruciate ligament reconstruction. Am J Sports Med 45:347–354
Isberg J, Faxen E, Laxdal G, Eriksson BI, Karrholm J, Karlsson J (2011) Will early reconstruction prevent abnormal kinematics after ACL injury? Two-year follow-up using dynamic radiostereometry in 14 patients operated with hamstring autografts. Knee Surg Sports Traumatol Arthrosc 19:1634–1642
Jakob RP, Staubli HU, Deland JT (1987) Grading the pivot shift. Objective tests with implications for treatment. J Bone Jt Surg Br 69:294–299
Järvelä S, Kiekara T, Suomalainen P, Järvelä T (2017) Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective randomized study with 10-year results. Am J Sports Med 45:2578–2585
Liu A, Sun M, Ma C et al (2017) Clinical outcomes of transtibial versus anteromedial drilling techniques to prepare the femoral tunnel during anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 25:2751–2759
Logan M, Dunstan E, Robinson J, Williams A, Gedroyc W, Freeman M (2004) Tibiofemoral kinematics of the anterior cruciate ligament (ACL)-deficient weightbearing, living knee employing vertical access open “interventional” multiple resonance imaging. Am J Sports Med 32:720–726
Lopomo N, Signorelli C, Rahnemai-Azar AA et al (2017) Analysis of the influence of anaesthesia on the clinical and quantitative assessment of the pivot shift: a multicenter international study. Knee Surg Sports Traumatol Arthrosc 25:3004–3011
Magnussen RA, Reinke EK, Huston LJ, Group M, Hewett TE, Spindler KP (2016) Factors associated with high-grade lachman, pivot shift, and anterior drawer at the time of anterior cruciate ligament reconstruction. Arthroscopy 32:1080–1085
Marcacci M, Zaffagnini S, Giordano G, Iacono F, Presti ML (2009) Anterior cruciate ligament reconstruction associated with extra-articular tenodesis: A prospective clinical and radiographic evaluation with 10- to 13-year follow-up. Am J Sports Med 37:707–714
Nakamura K, Koga H, Sekiya I et al (2017) Evaluation of pivot shift phenomenon while awake and under anaesthesia by different manoeuvres using triaxial accelerometer. Knee Surg Sports Traumatol Arthrosc 225:2377–2383
Noyes FR, Huser LE, Jurgensmeier D, Walsh J, Levy MS (2017) Is an anterolateral ligament reconstruction required in ACL-reconstructed knees with associated injury to the anterolateral structures? Am J Sports Med 45:1018–1027
Pomajzl R, Maerz T, Shams C, Guettler J, Bicos J (2015) A review of the anterolateral ligament of the knee: current knowledge regarding its incidence, anatomy, biomechanics, and surgical dissection. Arthroscopy 31:583–591
Rezende FC, de Moraes VY, Martimbianco AL, Luzo MV, da Silveira Franciozi CE, Belloti JC (2015) Does combined Intra- and extraarticular ACL reconstruction improve function and stability? A meta-analysis. Clin Orthop Relat Res 473:2609–2618
Seebacher JR, Inglis AE, Marshall JL, Warren RF (1982) The strucuture of the posterolateral aspect of the knee. J Bone Jt Surg Am 64:536–541
Schon JM, Moatshe G, Brady AW, Serra Cruz R, Chahla J, Dornan GJ, Turnbull TL, Engebretsen L, LaPrade RF (2016) Anatomic anterolateral ligament reconstruction of the knee leads to overconstraint at any fixation angle. Am J Sports Med 44:2546–2556
Sonnery-Cottet B, Daggett M, Fayard JM et al (2017) Anterolateral ligament expert group consensus paper on the management of internal rotation and instability of the anterior cruciate ligament-deficient knee. J Orthop Traumatol 18:91–106
Sonnery-Cottet B, Saithna A, Cavalier M et al (2017) Anterolateral ligament reconstruction is associated with significantly reduced ACL graft rupture rates at a minimum follow-up of 2 years. Am J Sports Med 45:1547–1557
Sonnery-Cottet B, Thaunat M, Freychet B, Pupim BH, Murphy CG, Claes S (2015) Outcome of a combined anterior cruciate ligament and anterolateral ligament reconstruction technique with a minimum 2-year follow-up. Am J Sports Med 43:1598–1605
Stijak L, Bumbasirevic M, Radonijc V, Kadija M, Puskas L, Milovanovic D, Filipovic B (2016) Anatomic description of the anterolateral of the knee. Knee Surg Sports Traumatol Arthrosc 24:2083–2088
Thaunat M, Clowez G, Saithna A, Cavalier M, Choudja E, Vieira TD, Fayard JM, Sonnery-Cottet B (2017) Reoperation rates after combined anterior cruciate ligament and anterolateral ligament reconstruction: a series of 548 patients from the SANTI Study Group with a minimum follow-up of 2 years. Am J Sports Med 45:2569–2577
Trojani C, Beaufils P, Burdin G et al (2012) Revision ACL reconstruction: Influence of a lateral tenodesis. Knee Surg Sports Traumatol Arthrosc 20:1565–1570
Vadala AP, Iorio R, De Carli A et al (2013) An extra-articular procedure improves the clinical outcome in anterior cruciate ligament reconstruction with hamstrings in female athletes. Int Orthop 37:187–192
Van Dyck P, Clockaerts S, Vanhoenacker FM et al (2016) Anterolateral ligament abnormalities in patients with acute anterior cruciate ligament rupture are associated with lateral meniscal and osseous injuries. Eur Radiol 26:3383–3391
Zhang H, Qiu M, Zhou A, Zhang J, Jiang D (2016) Anatomic anterolateral ligament reconstruction improves postoperative clinical outcomes combined with anatomic anterior cruciate ligament reconstruction. J Sports Sci Med 15:688–696
Funding
No funding was obtained.
Author information
Authors and Affiliations
Contributions
CPH—designed the study, analyzed the data and wrote the manuscript. DBC—designed the study, analyzed the data and wrote the manuscript. MFS—analyzed the data and wrote the manuscript. PNG—analyzed the data and wrote the manuscript. MBB—analyzed the data and wrote the manuscript. JRP—supervision of the study. GLC—manuscript review, and supervised the study. MKD—analyzed the data, and supervised the study.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest in relation to this study.
Ethical approval
Ethical approval was obtained at University of São Paulo (number 2.472.968).
Informed consent
Informed consent was obtained from all individual participants included.
Rights and permissions
About this article
Cite this article
Helito, C.P., Camargo, D.B., Sobrado, M.F. et al. Combined reconstruction of the anterolateral ligament in chronic ACL injuries leads to better clinical outcomes than isolated ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 26, 3652–3659 (2018). https://doi.org/10.1007/s00167-018-4934-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-4934-2