Abstract
Purpose
The anterolateral ligament, a structure that has been known for 130 years, has again attracted the attention both of orthopaedic doctors and anatomists. Since its initial description until now, this structure has had different names. Whether labelled as the mid-third lateral capsular ligament, the anterior oblique band of the fibular collateral ligament or the anterolateral ligament of the knee, this structure has been responsible for the so-called Segond avulsion fractures. The aim of this study was to determine the precise position and layer of the lateral knee compartment within which the anterolateral ligament is located, as well as its type.
Methods
In this study, the anatomical dissection of the lateral segment of 14 cadaveric knees (six male, eight female; seven right, seven left; average age of subjects: 78 years) was performed. The dissection was carried out in keeping with Seebacher, layer by layer.
Results
The anterolateral ligament was identified in seven out of 14 cadaveric knee joints (50 %). The length of the ligament was 41 ± 3 mm, while the width was 4 ± 1 mm and the thickness 1 mm (in the middle section). In 14 % of the cases, the anterior oblique band was identified as a part of the FCL. In all of the knee joints, a part of the fibres of the ITT with the same insertions and direction as the ALL was found, located, however, at a much more superficial level than the ALL.
Conclusion
Analysis of the current scientific literature related to the anterolateral ligament and layer-by-layer dissection of the lateral region of 14 cadaveric knees has led to the conclusion that the anterolateral ligament is a thickening of the knee joint capsule located in the third layer of the lateral region of the knee (according to Seebacher) which is not always clearly morphologically differentiated from the remainder of the joint capsule. The anterolateral ligament is unequivocally a part of the joint capsule, which is why any damage to it should be treated in the same way as any other damage to the joint capsule.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As of late, the anterolateral ligament of the knee joint has become an issue of interest. This structure was not ascribed much importance by previous generations of orthopaedic surgeons and anatomists, as far as its role in the mechanics of the knee joint is concerned. It is not even listed in the Terminologia anatomica as a separate structure [10]. In 1879, the French surgeon Segond [9] described the avulsion fractures of the lateral tibial condyle which he attributed to the thin but firm bundle of ligamentous fibres connecting the lateral femoral condyle to the anterior segment of the lateral tibial condyle. At forced internal rotation, of the knee joint, this bundle would often become detached from its distal insertion carrying with it a part of the anterior aspect of the lateral tibial condyle.
Just like many other areas of research, the lateral region of the knee also carries several controversial issues and points of dispute. The first issue is related to the classification by Seebacher [8]. All authors agree that there are three deep layers in this region. However, some authors [5] divide the first layer into the superficial part (oblique fibres of iliotibial tract ending on the patella) and profound part (lateral patellofemoral ligament, the transverse retinaculum and the patellotibial band). These two layers are joined posteriorly by the iliotibial tract (ITT) and are followed by the second layer (the fibular collateral ligament, patellofemoral ligament, fabellofibular ligament and arcuate ligament) and the third layer containing the joint capsule. Other authors [1, 7] have interpreted the classification by Seebacher in the following way: the first layer is composed only of the oblique ITT fibres, while the second layer consists of the lateral patellofemoral ligament, the transverse retinaculum and the patellotibial band. Finally, the third layer consists of a superficial and a deep part. The superficial part contains the fibular collateral ligament (FCL), patellofemoral ligament (PFL), fabellofibular ligament (FFL) and the arcuate ligament (AL), and the deep part contains the joint capsule.
By dissection of the soft tissue of the lateral region of 41 knees, Claes et al. [3] reached the third layer and within it described a fibre bundle originating from the lateral femoral condyle, somewhat in front of the FCL insertion, descending to the front and inwards with its insertion being 6 mm under the surface of the joint, on the tibia, midway between the Gerdy tubercle and the head of the fibula. Also, the authors state that the proximal segment of this ligament is sometimes connected to the proximal segment of the FCL. The average length of the ligament at full extension of the lower leg was 38.5 mm, and the thickness, at the level of the joint fissure, was 6.7 × 1.3 mm. The existence of the ligament was determined in 40 out of 41 knees [3]. The authors provided a detailed anatomical characterization of the anterolateral ligament, but it remained unclear to which layer this ligament belongs to as well as if there are others structures with the same orientation and point of insertion but in different layers.
In this paper, it is hypothesized that there are several structures in different layers of anterolateral knee compartment that can support the function of anterolateral ligament.
Materials and methods
During December 2013, at the Institute of Anatomy, School of Medicine, University of Belgrade, precise dissection of the lateral segment of 14 formalin-fixed cadaveric knees (six male, eight female; seven right, seven left; average age 78 years) was performed. After the removal of the skin and subcutaneous fatty tissue, the lateral region of the knee was precisely dissected, from the patella, in front, to the posterior cruciate ligament, in the back, and from the proximal insertion of the short biceps head to the neck of the fibula, distally. The superficial layer of the oblique ITT fibres was removed from the tibial insertion, together with the ITT and its distal insertion, and folded forwards over the patella. The ITT was left to hang by the intermuscular septum and on the fibres ending on the lateral condyle of the femur. Next, the elements of the following layer (patellofemoral ligament, the transverse retinaculum and the patellotibial band) were detached from their posterior insertions (the lateral epicondyle of the femur, the iliotibial tract and the tibia, respectively) and folded forwards, over the previous layer.
In all the dissected knees, directly behind the second layer (lateral patellofemoral ligament, the transverse retinaculum and the patellotibial band), a thin, translucent and broad fibrous band was found, which connected the lateral epicondyle of the femur and the point located midway between the Gerdy tubercle and the head of the fibula, and whose fibres were a continuation of the ITT (Fig. 1). Also, these fibres, in addition to the insertion on the posterior part of the Gerdy tubercle, continued into the fascia cruris.
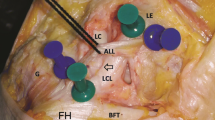
Lateral region of the right knee. The pink markers show the direction and position of the FCL. The green markers show the direction and position of the deep fibres of the ITT which connect the lateral epicondyle (LE) of the femur and the anterior part of the lateral condyle of the tibia located between the Gerdy tubercle (Ge) and the fibular head (FH). P patella, Bi–m. biceps femoris
After cutting through this structure transversely, the second and third deep layers were accessed, where, in addition to the FCL, the knee joint capsule is located. Between the FCL and the patellar ligament, the capsule is not homogenous, neither in thickness nor in the orientation of the fibres. In its anterior part, closer to the patellar ligament, the joint capsule is thin and the fibres are oriented vertically or from the top downwards and outwards. In its posterior part, closer to the FCL, the capsule is thicker and the fibres of the joint capsule are oriented vertically or from the top downwards and inwards. Immediately in front of the FCL and behind this thickening, the joint capsule is exceptionally thin and represents the part of the capsule where, just like on the FCL, the lateral meniscus does not have its insertion. At the same time, the thickened part of the capsule is the first part where the lateral meniscus is attached after the popliteal hiatus.
Results
In all the dissected knees, directly behind the second layer (lateral patellofemoral ligament, the transverse retinaculum and the patellotibial band), a thin, translucent and broad fibrous band was found (length 49 ± 4 mm, width 11 ± 2 mm, thickness <1 mm).
In the third layer of the lateral segment of the knee, in front of the fibular collateral ligament, the knee capsule was thickened. This thickened part has shown a different morphology in 14 investigated knees. In two right male knees (14 %), the proximal end of this ligament had a joint initial part with the FCL, 18 mm in length, upon which it separated arching to the front ending midway between the Gerdy tubercle and the head of the fibula. The free part of this ligament was 25 ± 4 mm long, 3.5 ± 1 mm wide and 2 mm thick. The angle that the free part of this ligament formed with the FCL was 27° ± 5° (Fig. 2).
In three right male knees, two left male knees and two right female knees a clearly defined thickening of the joint capsule was found with the fibres running from the lateral condyle of the femur, somewhat in front of the FCL insertion to the lateral tibial condyle where they were attached midway between the Gerdy tubercle and the head of the fibula (Fig. 3). The length of the ligament in this case was 41 ± 3 mm, while the width was 4 ± 1 mm and the thickness 1 mm (in its middle section). This structure was identified as anterolateral ligament (ALL).
The remaining seven knees (one left male knee, four left and two right female knees) did not show a clearly defined ALL. In the part where in the previously described knees a clearly detectible thickening of the capsule had been identified, the remaining seven knees displayed a mild thickening which was possible to differentiate from the FCL but not from the anterior, thin segment of the joint capsule (Fig. 4).
Second and third layer of the lateral region of the left knee. The entire joint capsule located between the lateral condyles of the femur and the tibia and in front of the FCL is approximately of the same thickness. In front of the FCL a bundle of meniscotibial (MT) fibres connecting the lateral meniscus and the tibia is visible. Ge the Gerdy tubercle, ITT iliotibial tract, LC-T lateral tibial condyle, LC-F lateral femoral condyle, LE lateral epicondyle, FH fibular head
Discussion
The most important result of this study is that anterolateral ligament, clearly defined bundle of fibrous tissue of articular capsule of lateral compartment of knee joint, is present in approximately 50 % of investigated cases. The functional importance of this structure, which is around 1 mm thick and approximately 4 mm wide, is rather small. Also, the study proves that the parts of iliotibial tract (in all cases) or fibular collateral ligament (in some cases) may have the same direction and attachment with the anterolateral ligament, but they are positioned more superficially. They do not represent the part of articular capsule and cannot be morphologically equal to ALL; however, together with the ALL, they make up the morphological structure of the anterolateral compartment of the knee, which has a significant role in the stabilization of the knee joint.
Furthermore, the implementation of a new transversal lamination of the lateral region of the knee which would consist of four layers, and would prevent any further differences in the interpretation of the number of sublayers in the first or third layer, is proposed in this study. The first layer would consist of oblique part consisting of fibres stemming from the ITT and ending on the patella. The second layer would contain horizontal fibres that make up the lateral patellofemoral ligament, transverse retinaculum and the patellotibial band and the authors of this study feel that the bundle of vertical fibres located behind the transversal layer should be added to the second layer (the transversal layer of the patellar retinaculum). These fibres are a continuation of the iliotibial tract and the intermuscular septum which are attached on the lateral epicondyle of the femur and then on the anterior part of the lateral tibial condyle, in the middle, between the Gerdy tubercle and articular surface for fibular head. Similar data were given by Vieira et al. [11]. The authors of this paper propose that the anterior oblique band (AOB), which shares its origin and its initial part with the FCL, should be categorized under the third layer together with the FCL, PFL, FFL and the AL (second layer according to Gray). The authors of this paper also add that this ligament is not a permanent structure and that it exists in around 14 % of the cases. The fourth layer would consist of articular capsule with anterolateral ligament, which is at the same time its integral part.
Vieira et al. [11] in the study of ten cadaveric knees described precisely the distal part, of ITT, as well as attachments of its parts. Their deepest part of ITT, capsular-osseous layer, which starts at lateral epicondyle of femur and has insertion lateral to the Gerdy tubercle equals to the data in the present study related to ITT.
The anterolateral ligament of the knee (ALL) is a capsular ligament which is presumed by the authors of the present study to be visible depending on the strain that the knee joint is put under. As the fibrous joint capsule is not a continuous layer of connective tissue, depending on the different directions of force impact on the knee joint, the knee capsule reacts by thickening certain bundles. The authors of the present study presume that the joint capsule of the knees which had been put under greater strain (male type body constitution, dominant extremity) had developed thicker fibre bundles in places of greater force impact, with one of these results being the thickening of the fibre bundle of the joint capsule extending from the lateral epicondyle of the femur to the middle between the Gerdy tubercle and articular surface for fibular head. Knees that had not been exposed to a greater force impact did not have the need to strengthen the aforementioned part, which is why the joint capsule from the FCL to the LP is characterized by a continuous decrease in thickness from the back towards the front with no clear border differentiating the ALL from the rest of the capsule.
The question arises as to whether ALL should be differentiated from the structure of the joint capsule or not. The fact that this ligament is clearly distinguishable in some knees without any additional interventions (lower leg traction, etc.) speaks in favour of this differentiation. However, the very site of insertion of this ligament, which is in no way different from the insertion of the rest of the joint capsule, the existence of the synovia on the internal side of the ALL as well as the fact that it cannot be clearly distinguished on some knees, speaks against it.
It must be noted that the results of the present study partially differ from the results of other authors [3, 12]. These authors describe a much greater incidence of ALL. The authors of the present study would like to emphasize that this research was methodologically based on a clearly differentiated bundle which could be defined as the ALL. Vincent et al. [12] stated that ALL of cadaveric knees was 34 mm long, 8 mm wide and 2–3 mm tick. The methodology applied by these authors reflects how difficult it is to distinguish the ALL from the surrounding joint capsule. Namely, they removed the extensor apparatus of the knee, the cruciate ligaments, the medial collateral ligament and the ITT and then placed the Hohmann Retractor between the femur and the tibia tightening the lateral joint capsule until the anterolateral ligament became clearly visible as a thickening in the lateral capsule. During this procedure, they accessed the ligament from the internal aspect which was covered by the synovia. Also, the same authors identified the ALL in all of 30 consecutive knees during preparation for total knee arthroplasty [12]. Considering that the cadaveric knees of the cited study are older than the cadaveric knees in the present study (85 vs. 78 years) and that 80 % are female (in the present study, there are 57 % female), it can be concluded that the ALL length is approximately equal (34 vs. 41 mm). The authors of the present study assume that a greater width of the ALL in the cited study was the result of Hohmann Retractor use, which isolated tightened higher number of bundles of anterolateral part of articular capsule. Greater thickness of ALL of cited study can be the result of AOB of FCL existence (which is not noted in the study), as well as ITT bundles, attached to tibia, in the middle between the Gerdy tubercle and fibular head (authors mentioned that ITT bundles, attached to fibular head in the Gerdy tubercle, were removed).
Claes et al. [3] also published the dimensions of ALL ligament, which were somewhat greater than in the present study, although cadaveric knees originated from the same population that was equal to the research material belonging to the present study. Namely, the length is the same in both studies, but the width of ligament of cited study is about 70 % greater, whereas the thickness is about 30 % greater. The authors of the present study feel that the reasons for the difference in dimensions are twofold. The first reason is the method of preparation fixation (in the present study formalin-fixed specimens were used). On the other hand, it can be stipulated that the presence of AOB of FCL and ITT bundles also impacted an increase in width and thickness of ALL of cited study.
The anterior oblique band (AOB), as a part of the FCL with its insertion on the superior portion of the tibia, has been described by Irvine et al. [6]. In their prospective study in 1985, they had 9 cases of “Segond” avulsion fractures occurring during semiflexion in the knee joint with internal or external rotation. In order to determine which ligament is key to avulsion fractures, these authors dissected seven cadaveric knees and concluded that avulsion region corresponded to tibial attachment of the (AOB) of FCL. As opposed to Segond [9] who stressed that these avulsion fractures were accompanied by damage to the synovia or other ligaments, Irvine et al. [6] emphasized that these fractures were mostly isolated. In parallel to above-mentioned study, Goldman et al. [4] followed clinical and radiographical findings of Segond avulsion fractures and their relation to soft tissue injuries. Having reviewed medical documentation for the period of 9 years, they concluded that all of the patients in their study (9/9) had a combined ACL rupture with Segond avulsion fractures. They attribute this to the mid-third (from the front towards the back) of the lateral capsular ligament situated in the third layer. The question remains whether the ruptures are isolated phenomena or related to the ACL rupture. Both authors (Irvine and Goldman) were probably right since they described two different ligaments.
Some authors [2, 11] noted that ITT participated in ALL structure with the bundles which stretched from lateral femoral epicondyle up to anterolateral part of lateral tibial condyle. The band of ITT fibres, located somewhat more superficially, whose direction is similar, only is at a more superficial level than the FCL and has a proximal insertion behind and not in front of the FCL, was also separated.
Figure 1 published in the paper by Claes [3] shows, in detail, the structure that the authors described as the ALL. However, the picture shows that this structure is located more superficially than the FCL (the joint capsule, whose part the ALL is, lies deeper) and also that the proximal insertion of this structure is behind the FCL (the ALL has a proximal insertion directly in front of the FCL). The authors of the present study presume that the structure in this figure defined as the ALL is, in fact, a band of vertical fibres of the ITT.
If one were to eliminate the ITT fibres as well the AOB of the FCL, which is variable and can be considered to be a part of the FCL, future studies should outline the criteria under which the thickening of the joint capsule directly in front of and deeper than the FCL can be considered to be a ligament and not merely a thickening of the joint capsule, thereby removing personal subjectivity in the estimation of the width of the ALL, which, in front continues onto the joint capsule without any marked border (Fig. 4).
If the practical implications of identifying and describing this ligament are taken into consideration, the authors of the present study feel that most of the facts are already known. The reparation of the lesions of soft tissue structures of the lateral region of the knee, amongst other things, entails suturing the joint capsule both behind and in front of the FCL. Therefore, whether identified as an individual ligament or as a part of the joint capsule, the ALL will be repaired. Finally, the question arises as to the necessity of isolated reconstruction of a capsular ligament 4 × 1 mm thick. The authors of the present study presume that isolated reparation of this bundle with the aid of a different autograft would be one more of many tenodese operations with the aim to reduce anterolateral rotatory instability.
Conclusion
The anterolateral ligament is a capsular bundle of ligamentous fibres situated in the fourth layer of the lateral soft tissue of the knee which connects the lateral epicondyle of the femur and the anterior part of the lateral condyle of the tibia, directly underneath the joint cartilage. Posteriorly, the ALL is clearly differentiated from the FCL, while in the front, it continues onto the joint capsule, very often without a clear border between these two structures. Due to the attachment and direction, AOB of FCL and capsular-osseous layer of ITT can functionally be equated to ALL. Morphologically, they represent parts that do not belong to articular capsule like ALL, but to fibular collateral ligament, that is iliotibial tract.
References
Campbell WC (2008) Knee injuries. In: Canale ST, Beaty JH (eds) Campbell’s operative orthopaedics, 11 edn, Chap 43. Mosby Elsevier, Philadelphia
Campos JC, Chung CB, Lektrakul N, Pedowitz R, Trudell D, Yu J, Resnick D (2001) Pathogenesis of the Segound fracture: anatomic and MR imaging evidence of an iliotibial tract or anterior oblique band avulsion. Radiology 219:381–386
Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J (2013) Anatomy of the anterolateral ligament of the knee. J Anat 223:321–328
Goldman AB, Pavlov H, Rubenstein D (1988) The Segound fracture of the proximal tibia: a small avulsion that reflects major ligamentous damage. Am J Roentgenol 151:1163–1167
Gray H (2005) Pelvic girdle and lower limb. In: Standring S (ed) Gray’s anatomy, 39 edn. Elsevier, Churchill, Livingstone, London
Irvine GB, Dias JJ, Finlay DB (1987) Segound fractures of the lateral tibial condyle: brief report. J Bone Joint Surg (Br) 69:613–614
Lešić A, Ukropina D, Mariani PP (1997) Lezije i lečenje ligamenata kolena. Beograd: CIBIF, Medicinski fakultet Univerziteta u Beogradu (Serbian)
Seebacher JR, Inglis AE, Marchall JL, Warren JF (1982) The structure of the posterolateral aspect of the knee. J Bone Joint Surg Am 64:536–541
Segond P (1879) Recherches cliniques et expérimentales sur les e´panchements sanguins du genou par entorse. Progrés Med 7:297–341
Terminologia anatomica, international anatomical terminology (1998) Sederative committee on anatomical terminology (SCAT). Thieme Stuttgart, New York
Vieira EL, Vieira EA, da Silva RT, Berlfein PA, Abdalla RJ, Cohen M (2007) An anatomic study of the iliotibial tract. Arthroscopy 23:269–274
Vincent JP, Magnussen RA, Gezmez F, Uguen A, Jacobi M, Weppe F, Al-Saati MF, Lustig S, Demey G, Servien E, Neyet P (2012) The anterolateral ligament of the human knee: an anatomic and histologic study. Knee Surg Sports Traumatol Arthrosc 20:147–152
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stijak, L., Bumbaširević, M., Radonjić, V. et al. Anatomic description of the anterolateral ligament of the knee. Knee Surg Sports Traumatol Arthrosc 24, 2083–2088 (2016). https://doi.org/10.1007/s00167-014-3422-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3422-6