Abstract
Purpose
The aims of this article were to report the objective results of revision ACL reconstruction and to assess the influence of an associated lateral extra-articular tenodesis on knee stability and IKDC score.
Methods
This study focused on revision ACL reconstruction and was conducted over a 10-year period, from 1994 to 2003 with ten French orthopedic centers participating. The minimum follow-up required was 2 years. To be included, patients had to be evaluated at follow-up with the objective International Knee Documenting Committee (IKDC) scoring system. In 2006, 163 patients met the inclusion criteria.
Results
The objective IKDC knee score improved significantly after revision ACL reconstruction, with 72% IKDC A + B (26% A). When a lateral tenodesis was performed, 80% had a negative pivot shift, versus 63% without (P = 0.03), but there was no significant difference in the IKDC score.
Conclusion
This study shows a significant improvement in the IKDC score after revision ACL reconstruction. The association of a lateral extra-articular tenodesis with the intra-articular graft increases knee stability after revision ACL reconstruction; however, this additional procedure does not significantly alter the IKDC score at follow-up.
Level of evidence
Retrospective case series, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Due to failure of primary ACL reconstruction, some patients need revision surgery. Authors have reported their experience in revision ACL reconstruction using bone-patellar tendon-bone (BTB) autograft [6, 9, 22, 28, 34, 41], allografts [14], and different graft types [5, 18, 31]. There are concerns regarding the objective results of revision ACL reconstruction, generally considered as inferior to those of primary reconstruction [1, 5, 6, 10–15, 17, 18, 20–22, 26–28, 30–34, 37–39, 41], and regarding knee stability after revision. Few studies [3, 8, 9, 13, 25, 31, 40, 43] advocate the use of a lateral extra-articular tenodesis associated with the intra-articular graft in these revisions. Furthermore, while Ferretti et al. [13] reported 90% of patients IKDC A + B with a 10% failure rate by using hamstrings graft and lateral extra-articular tenodesis, Salmon et al. [32] reported 50% of patients IKDC A + B with the same failure rate by using isolated hamstrings graft. However, no study as yet compared the two following groups: isolated revision ACL reconstruction versus revision ACL reconstruction associated with a lateral tenodesis.
Therefore, on the basis of a multicenter retrospective series of revision ACL reconstruction conducted by the French Arthroscopic Society [7], this study was designed to assess the objective IKDC results of revision ACL reconstruction in a large cohort of patients and the influence of an associated lateral extra-articular tenodesis with the intra-articular graft on knee stability and IKDC score. The hypothesis was that the association of a lateral extra-articular tenodesis with the intra-articular graft used for revision ACL reconstruction increases knee stability.
Materials and methods
Patients included in this retrospective multicenter study were operated over a ten-year period, between 1994 and 2003 with ten French orthopedic centers participating. Inclusion criteria were failure of a primary autogenous anterior cruciate ligament reconstruction, an intact posterior cruciate ligament, an uninjured contralateral knee, and revision ACL reconstruction performed with an autogenous ipsilateral or contralateral graft. ACL reconstruction is commonly considered a failure for one of the two following reasons: loss of knee motion due to the development of progressive arthrofibrosis or loss of stability secondary to recurrent pathological laxity [36]. In this study, only the primary ACL reconstruction that led to the recurrence of knee instability and to revision ACL reconstruction was considered a failure. Injuries to the collateral ligaments, medial and lateral, and failure of synthetic grafts were excluded to render the patient group as homogenous as possible. The minimum follow-up required was 2 years. To be included in the study, patients had to be evaluated with the objective International Knee Documenting Committee (IKDC) scoring system [19]. The objective IKDC form includes ligament, mobility, and radiographic assessment. Ligament stability was measured by the Lachman [35] and pivot shift [16] tests graded as recommended by the IKDC form. Instrumented knee testing was performed with the KT-1000 arthrometer using the manual maximum test and/or with the TELOS using 250 Newtons of anterior drawing. Mobility was assessed comparatively and was graded as recommended by the IKDC form. According to the IKDC, radiologic evaluation of the knees included bilateral full-extension AP and lateral mono weight-bearing views, comparative 30° flexion AP, and skyline views. Data for each patient were collected in a database edited on File Maker Pro 6. Data were collected on both the primary and the revision ACL reconstruction, the postoperative rehabilitation, the complications and reoperations, the objective IKDC score before and after the revision ACL reconstruction, and the radiological status before and after the revision surgery.
At a minimum of 2-year follow-up, 189 patients were available for the study. There were 127 men and 123 right knees. The median age at the time of primary ACL reconstruction was 22.7 years (13–57), the interval between primary and revision surgery was 5 years (5 months to 15 years), and the median age at revision was 27.6 (14–63). The median follow-up was 44 months (24–120). The primary ACL reconstruction was a BTB graft in 72% (136 patients), a semitendinosus and gracilis (ST/G) in 25% (47 patients), and a quadriceps tendon graft (QTG) in 3% (n = 6) of the patients. A lateral tenodesis was associated with the intra-articular graft in 14% (26 patients), a concomitant medial meniscectomy in 25% (64 patients), and a lateral meniscectomy in 8% (22 patients). To render the group of patients as uniform as possible, the 26 patients for whom a lateral tenodesis was performed during the primary ACL reconstruction were excluded from statistical analysis, leaving 163 patients in the study.
Statistical analysis
After inclusion and complete review of the data, datafiles were centralized for correction and statistical analysis. In a univariate analysis, the statistical tests used were the chi-square test and the Student’s t test, when required (Symantec Inc.). The level of significance was set at P < 0.05.
Results
The revision ACL reconstruction graft was a BTB in 50% (n = 83), a ST/G in 40% (n = 64), and a QTG in 10% of the patients (n = 16). A medial and a lateral meniscectomy was performed in 40 and 10% of the patients, respectively (n = 65 and 16). An associated lateral tenodesis was performed in 51% of the patients (n = 84), according to the surgeon’s preference, on a routine basis. After revision, the complication and reoperation rates were, respectively, 8% and 12%. Primary BTB (117 patients) was revised by a BTB, ipsilateral, or contralateral in 45% (52 patients), by an ipsilateral ST/G in 45% (53 patients), and by a QTG in 10% (12 patients). Primary ST/G (43 patients) was revised by an ipsilateral BTB in 67% (28 patients), a contralateral ST/G in 24% (11 patients), and a QTG in 9% (4 patients). Primary QTG (3 patients) was revised by a BTB. The contralateral nonoperated knee was harvested in 25% of the patients (40 out of 163).
Failure was defined as a grade 2 or 3 pivot shift test and a KT-1000 test showing a difference >5 mm, in accordance with the literature [28, 33]. With these criteria, the failure rate was 11% (18 patients). Eight of the failures were BTB grafts, 8 were ST/G, and 2 were QTG. In 12 cases of failure, the revision was performed with an isolated ACL graft versus 6 failures when a lateral extra-articular tenodesis was added. These results lead to a 15% failure rate for revision with isolated ACL reconstruction (12/79) versus 7% for revision with ACL reconstruction associated with lateral extra-articular tenodesis (6/84). However, this difference is not significant (P = n.s.). Of these failures, 3 patients had a second revision, and the other 15 did not consider further surgery.
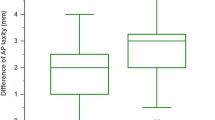
Objective results before and after revision ACL reconstruction show no significant improvement in the mobility and no decrease in the radiological status (Table 1). Improvement was due to the anterior tibial translation: After revision, laxity decreased significantly (Table 1) with the KT 1000 from 7.1 mm (mm) to 2.5 mm (89 patients) and with the TELOS from 9.5 mm to 4.9 mm (74 patients). At 44-month follow-up, 25% of the patients were IKDC C, and 3% D.
Three different grafts (BTB, ST/G, and QTG) were used for revision. Whatever the graft, there was no difference in the objective IKDC score (Table 2). The different graft harvesting strategies are summarized in Table 3: In the case of primary BTB, an ipsilateral or contralateral BTB or an ipsilateral ST/G was performed, whereas in the case of primary ST/G, the surgeons used an ipsilateral BTB or a contralateral ST/G. We found no difference whichever strategy was used.
Table 4 demonstrates that a lateral tenodesis associated with the intra-articular graft for revision ACL reconstruction increased knee stability significantly with a 80% negative pivot shift versus 63% without tenodesis. Secondly, the data illustrate that this additional procedure does not influence the IKDC score at follow-up.
Discussion
The main finding of this study is that the association of a lateral tenodesis with the intra-articular graft, initially described by Lemaire [23] and then by Mac Intosh and Darby [24] and recently revisited by Colombet [8, 9], increases the knee stability after revision ACL reconstruction. However, this extra-articular graft does not improve the global IKDC score and is therefore questionable, as proven by two recent retrospective studies on revision ACL reconstruction: While Ferretti et al. report the systematic association of a lateral tenodesis with ST/G graft on 30 patients [13], Salmon et al. report on 50 patients operated with an isolated ST/G graft [32] with the same failure rate. The present study demonstrates for the first time that the residual rate of positive pivot shift is significantly lower if a lateral tenodesis is associated with the intra-articular graft. This “belt and suspenders” procedure, that is, lateral extra-articular tenodesis associated with an intra-articular ACL autograft, is not commonly used nowadays but is advocated by short- and long-term studies for ACL reconstruction to control both anterior laxity and rotational instability [3, 29]. The use of navigation in a recent study demonstrated that this additional procedure improves internal tibial rotation control [9]. In the present study, the lateral extra-articular tenodesis is of significant influence as patients with this additional procedure have a tendency to a lower failure rate and a significantly higher percentage of negative pivot shift. Furthermore, this extra-articular procedure does not increase long-term osteoarthritis [25].
Secondly, this study shows that the objective results of revision ACL reconstruction in a large number of patients are acceptable, with a 72% rate of IKDC A + B and a 11% failure rate. This study presents the objective results of a mid-term follow-up retrospective series of 163 patients. To our knowledge, this is the largest series published in the medical literature on this topic, as the MARS cohort [4, 42] is a descriptive epidemiologic prospective study. Objective assessment was performed in the study with the IKDC scoring system. Evaluations show a significant improvement after revision. However, although the rate of IKDC A + B is 72%, we report 26% of patients IKDC A, solely which can be considered as normal knees. These results are consistent with those reported by Salmon et al. [32], Rollier et al. [31], and Denti et al. [11] but do not compare favorably with those reported by Ferretti et al. [13]. Previous studies reported a global IKDC A + B rate between 12 and 83% [14, 15, 17, 22, 27, 30, 41]. Considering the same criteria for failure previously used in the literature, the 11% failure rate reported in this study is consistent with that reported recently by Ferretti et al. [13], Salmon et al. [32], Denti et al. [11], and Muneta et al. [26]. These results challenge the generally accepted belief that the failure rate of revision ACL reconstruction is two to three times that of primary ACL reconstruction [2]. Furthermore, the failure rate is higher in the group of patients revised with an isolated ACL graft, which leads to consider that the association of a lateral extra-articular tenodesis with the intra-articular graft may decrease the failure rate of revision ACL reconstruction.
Thirdly, this study shows that BTB and ST/G are valuable grafts for revision ACL reconstruction and that the graft used for revision surgery may be harvested from the same source for BTB as for primary surgery or that surgeons can switch to the non-harvested graft. This is in accordance with the results recently published in two studies that recommend that when available, hamstring tendon autografts should be considered for revision ACL reconstruction [13, 32]. Nonetheless, patellar tendon yields comparable results and is also validated by previous studies [10, 22, 41]. Therefore, one logical strategy could be to use ipsilateral BTB for revision of previous ST/G and ipsilateral ST/G for revision of previous BTB: The surgical knowledge of these two grafts may be necessary for the knee surgeon to solve revision ACL reconstruction problems. However, in this study, this “switched graft strategy” is not superior to the use of a contralateral BTB for revision of a previous BTB or to using a contralateral ST/G for revision of a previous ST/G.
Finally, this study has some limitations. First, it is a retrospective study, but no prospective or randomized study has yet been published on revision ACL reconstruction. Secondly, the follow-up is short. Thirdly, the use of a lateral extra-articular tenodesis depended on the surgeon’s decision. Fourth, an objective way of measuring the rotational stability is missing, only the pivot shift test gives the information on rotation, and finally, three different grafts are used for revision. Despite this lack of evidence, these results should be considered as those of other retrospective studies because of the large patient population, the inclusion criteria, and the methods of analysis.
The clinical relevance of this study is that the association of a lateral extra-articular tenodesis with the intra-articular graft increases knee stability after revision ACL reconstruction.
Conclusion
This study shows a significant improvement after revision ACL reconstruction, with good IKDC score and acceptable failure rate. Association of a lateral extra-articular tenodesis with the intra-articular graft decreases the failure rate and increases knee stability but not IKDC score at follow-up.
References
Bach B (2003) Revision anterior cruciate ligament surgery. Arthroscopy 19:14–29
Bach B (2005) Revision ACL issues [editorial comment]. Sports Med Arthrosc Rev 13:1
Bignozzi S, Zaffagnini S, Lopomo N, Martelli S, Iacono F, Marcacci M (2009) Does a lateral plasty control coupled translation during antero-postérior stress in single-bundle ACL reconstruction? Knee Surg Sports Traumatol Arthrosc 17:65–70
Borchers JR, Kaeding CC, Pedroza AD, Huston LJ, Spindler KP, Wright RW (2011) Intra-articular findings in primary and revision anterior cruciate ligament reconstruction surgery: a comparison of the MOON and MARS study groups. Am J Sports Med 39:1889–1893
Carson E, Anisko E, Restrepo C, Panariello RA, O’Brien SJ, Warren RF (2004) Revision anterior cruciate ligament reconstruction: etiology of failures and clinical results. J Knee Surg 17:127–132
Cheatham SA, Johnson DL (2010) Anatomic revision ACL reconstruction. Sports Med Arthrosc 18:33–39
Colombet PH, Neyret PH, Trojani C, Sbihi A, Djian P, Potel JF, Hulet C, Jouve F, Bussière C, Ehkirch P, Burdin G, Dubrana F, Beaufils P, Franceschi JP, Chassaing V (2007) Revision ACL surgery. Rev Chir Orthop 93(Suppl 8):5S54–5S67
Colombet P (2011) Navigated intra-articular ACL reconstruction with additional extra-articular tenodesis using the same hamstring graft. Knee Surg Sports Traumatol Arthrosc 19:384–389
Colombet P (2011) Knee laxity control in revision anterior cruciate ligament reconstruction versus anterior cruciate ligament reconstruction and lateral tenodesis. Am J Sports Med 39:1248–1254
Colosimo AJ, Heidt RS, Traub JA, Calonas RL (2001) Revision anterior cruciate ligament reconstruction with a reharvested ipsilateral patellar tendon. Am J Sports Med 29:746–750
Denti M, Lo Vetere D, Bait C, Schönhuber H, Melegati G, Volpi P (2008) Revision anterior cruciate ligament reconstruction: causes of failure, surgical technique, and clinical results. Am J Sports Med 36:1896–1902
Eberhardt C, Kurth AH, Hailer N, Jäger A (2000) Revision ACL reconstruction using autogenous patellar tendon graft. Knee Surg Sports Traumatol Arthrosc 8:290–295
Feretti A, Conteduca F, Monaco E, De Carli A, D’arrigo C (2006) Revision anterior cruciate ligament reconstruction with doubled semitendinosus and gracilis tendons and lateral extra-articular reconstruction. J Bone Joint Surg 88-A:2373–2379
Fox J, Pierce M, Bojchuk J, Hayden J, Bush-Joseph CA, Bach BR Jr (2004) Revision anterior cruciate ligament reconstruction with nonirradiated fresh-frozen patellar tendon allograft. Arthroscopy 20:787–794
Fules PJ, Madhav RT, Goddard RK, Mowbray MA (2003) Revision anterior cruciate ligament reconstruction using autografts with a polyester fixation device. Knee 10:335–340
Galway R, Beaupre A, Mc Intosh D (1972) Pivot shift: a clinical sign of anterior cruciate ligament insufficiency. J Bone Joint Surg Br 71:763–764
Grossman MG, ElAttrache NS, Shields CL, Glousman RE (2005) Revision anterior cruciate ligament reconstruction: three to nine year follow-up. Arthroscopy 21:418–423
Harilainen A, Sandelin J (2001) Revision anterior cruciate ligament surgery: a review of the literature and resultst of our own revisions. Scand J Med Sci Sports 11:163–169
Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, Richmond JC, Shelbourne KD (2001) Development and validation of the International Knee Documentation Committee subjective knee form. Am J Sports Med 29:600–613
Johnson DL, Swenson TM, Irrgang JJ, Fu FH, Harner CD (1996) Revision anterior cruciate ligament surgery: experience from Pittsburgh. Clin Orthop Relat Res 325:100–109
Kamath GV, Redfern JC, Greis PE, Burks RT (2011) Revision anterior cruciate ligament reconstruction. Am J Sports Med 39:199–217
Kartus J, Stener S, Lindahl S, Eriksson BI, Karlsson J (1998) Ipsi or contra-lateral patellar tendon graft in anterior cruciate ligament revision surgery: a comparison of two methods. Am J Sports Med 26:499–504
Lemaire M (1967) Ruptures anciennes du ligament croisé antérieur. Fréquence-Clinique-traitement. J Chir 93:311–320
MacIntosh DL, Darby JA (1976) Lateral substitution reconstruction. J Bone Joint Surg Br 58:142
Marcacci M, Zaffagnini S, Giordano G, Iacono F, Preti ML (2009) Anterior cruciate ligament reconstruction associated with extra-articular tenodesis: a prospective clinical and radiographic evaluation with 10- to 13- year follow-up. Am J Sports Med 37:707–714
Muneta T, Hara K, Ju YJ, Mochizuki T, Morito T, Yagishita K, Sekiya I (2010) Revision anterior cruciate ligament reconstruction by double-bundle technique using multi-strand semitendinosus tendon. Arthroscopy 26:769–781
Noyes F, Barber-Westin SD (1996) Revision anterior cruciate ligament surgery: experience from Cincinati. Clin Orthop Relat Res 325:116–129
Noyes F, Barber-Westin SD (2001) Revision ACL surgery with the use of bone patellar tendon bone autogenous grafts. J Bone Joint Surg Am 83:1131–1143
Pernin J, Verdonk P, Si Selmi TA, Massin P, Neyret P (2010) Long-term follow-up of 24.5 years after intra-articular anterior cruciate ligament reconstruction with lateral extra-articular augmentation. Am J Sports Med 38:1094–1102
O’Neil D (2004) Revision arthroscopically assisted anterior cruciate ligament with previously unharvested ipsilateral autografts. Am J Sports Med 32:1833–1841
Rollier JC, Besse JL, Lerat JL, Moyen B (2007) Anterior cruciate ligament revision: analysis and results from a series of 74 cases. Rev Chir Orthop 93:344–350
Salmon LJ, Pinczewski LA, Russell VJ, Refshauge K (2006) Revision anterior cruciate ligament reconstruction with hamstring tendon autograft. 5- to 9- year follow-up. Am J Sports Med 34:1604–1614
Taggart T, Kumar A, Bickerstaff D (2004) Revision anterior cruciate ligament reconstruction: a midterm patient assessment. Knee 11:29–36
Texier A, Hulet C, Acquitter Y (2001) Reconstruction itérative du ligament croisé antérieur sous arthroscopie. A propos de 32 cas. Rev Chir Orthop 87:653–660
Torg J, Conrad W, Kalen V (1976) Clinical diagnosis of anterior cruciate ligament instability in the athlete. Am J Sports Med 4:84–93
Trojani C, Sbihi A, Djian P, Potel JF, Hulet C, Jouve F, Bussière C, Ehkirch FP, Burdin G, Dubrana F, Beaufils P, Franceschi JP, Chassaing V, Colombet P, Neyret P (2011) Causes for failure of ACL reconstruction and influence of meniscectomies after revision. Knee Surg Sports Traumatol Arthrosc 19:196–201
Uribe JW, Hetchtman Zvijac JE (1996) Revision ACL surgery: experience from Miami. Clin Orthop Relat Res 325:91–99
Van Eck CF, Kropf EJ, Romanowski JR, Lesniak BP, Tranovich MJ, van Dijk CN, Fu FH (2011) Factors that influence the intra-articular rupture pattern of the ACL graft following single bundle reconstruction. Knee Surg Sports Traumatol Arthrosc 19:1243–1248
Van Eck CF, Kropf EJ, Romanowski JR, Lesniak BP, Tranovich MJ, van Dijk CN, Fu FH (2011) ACL graft re-rupture after double-bundle reconstruction: factors that influence the intra-articular pattern of injury. Knee Surg Sports Traumatol Arthrosc 19:340–346
Wegrzyn J, Chouteau J, Philippot R, Fessy MH, Moyen B (2009) Repeat revision of anterior cruciate ligament reconstruction: a retrospective review of management and outcome of 10 patients with an average 3-year follow-up. Am J Sports Med 37:776–785
Woods GW, Fincher AL, O’Connor DP, Bacon SA (2001) Revision anterior cruciate ligament reconstruction using the lateral third of the ipsilateral patellar tendon after failure of the central-third graft: a preliminary report on 10 patients. Am J Knee Surg 14:23–31
Wright RW, Huston LJ, Spindler KP, Dunn WR, Haas AK, Allen CR, Cooper DE, DeBerardino TM, Lantz BB, Mann BJ, Stuart MJ (2010) Descriptive epidemiology of the multicenter ACL revision study (MARS) cohort. Am J Sports Med 38:1979–1986
Zaffagnini S, Signorelli C, Lopomo N, Bonanzinga T, Marcheggiani Muccioli GM, Bignozzi S, Visani A, Marcacci M (2011) Anatomic double-bundle and over the top with additional extra-articular tenodesis : an in vivo quantitative assessment of knee laxity in two different ACL reconstructions. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-011-1589-7
Acknowledgments
The authors wish to thank Agnès Uranovicz for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Trojani, C., Beaufils, P., Burdin, G. et al. Revision ACL reconstruction: influence of a lateral tenodesis. Knee Surg Sports Traumatol Arthrosc 20, 1565–1570 (2012). https://doi.org/10.1007/s00167-011-1765-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1765-9