Abstract
Purpose
The aim of this systematic review is to compare the clinical outcomes of patients treated with different trochleoplasty procedures, the rate of complications and recurrence of patellar dislocation.
Methods
A systematic review of the literature was performed, in accord with the PRISMA guidelines. PubMed, MEDLINE, CINAHL, Cochrane, EMBASE and Google Scholar databases were comprehensively searched using the keyword combinations, “Dejour trochleoplasty”, “Bereiter Trochleoplasty”, “Albee Trochleoplasty”, “Recession Trochleoplasty”, “Trochlear Dysplasia”, “Instability”, “Adult”, “Clinical Outcome” and “Surgery”.
Results
Three-hundred and ninety-two knees in 371 patients were included. Bereiter U-shaped deepening trochleoplasty was the most commonly used technique for the treatment of trochlear dysplasia in the included studies with the lowest rate of recurrence and post-operative ROM deficiency. On the other hand, Dejour V-shaped deepening trochleoplasty showed the highest mean post-operative value of Kujala score with 79.3 (SD 8.4) points. Statistical differences were found in terms of redislocation rate between Goutallier procedure and Bereiter trochleoplasty (p < 0.05) and in terms of post-operative osteoarthritis between Bereiter and Dejour procedures (p < 0.05).
Conclusion
Bereiter trochleoplasty seems to be the most efficiency procedure in terms of post-operative patellar redislocation, post-operative osteoarthritis and ROM, but the highest mean post-operative Kujala score is obtained by Dejour procedure. Therefore, none of the surgical techniques analysed highlighted a real superiority. Randomised clinical trials are needed to establish whether of available surgical technique is the best to treat patient with trochlear dysplasia. The clinical relevance of this paper is that the three most popular trochleoplasty techniques are associated with significantly improved stability and function, showing a relatively low rate of osteoarthritis and pain, and a moderate rate of complications.
Level of evidence
Systematic review, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
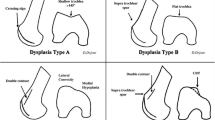
Trochlear dysplasia is a condition in which the femoral trochlea has an abnormal shape and function. This condition occurs in <2% of the population; however, up to 85% of patients with recurrent patellar instability have trochlear dysplasia [13, 19]. Dejour et al. [12] proposed a classification of trochlear dysplasia based on the combined evaluation of axial and lateral radiographs, distinguishing four types of dysplasia. Type A is characterized by the presence of crossing sign in the lateral view, a shallow trochlea and a sulcus angle >145° on the axial view. Type B is characterized by a crossing sign and trochlear spur on lateral radiographs. Type C is characterized by a crossing sign and a double-contour sign (representing the medial hypoplastic facet) on the lateral view. Type D is characterized by crossing sign, supratrochlear spur and double-contour sign with asymmetry of the facet’s height.
Trochleoplasty aims to change the shape of the trochlea in order to stabilize an unstable patella. Several trochleoplasty procedures have been proposed. Firstly, Albee [1] pioneered a procedure to elevate the lateral facet of the trochlea, to increase its obliquity and to restore the normal anatomy by an osteotomy and interposition of a tibial graft. This procedure may induce an increased pressure across the lateral facet of the patella-femoral articulation generating patellofemoral pain and subsequently patellofemoral osteoarthritis.
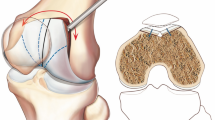
Secondly, the procedure proposed by Masse [25], later modified by Dejour and Saggin [11] and Dejour et al. [12], tried to decrease the prominence of the trochlea and create a new “V-shaped” groove with a normal depth using a straight midline skin incision carried out from the superior patellar margin to the tibiofemoral articulation (Fig. 1a: sulcus deepening trochleoplasty according to Dejour has the main goal to decrease the prominence of the trochlea and to create a new groove with normal depth, thus optimizing patellar tracking). Thirdly, Bereiter [5] described a “U-shaped” deepening trochleoplasty with a lateral parapatellar approach (Fig. 1b: Bereiter U-shaped” deepening trochleoplasty: a thin osteochondral flake with 2 mm of subchondral bone is elevated from the trochlea extending until the intercondylar notch; the distal femoral subchondral bone is deepened and refashioned with osteotomes and a high-speed burr. Next, the osteochondral flap is seated in the refashioned bed and fixed with 3-mm-wide vicryl bands, passing through the centre of the groove and exiting in the lateral femoral condyle. The periosteum is reattached to the edge of the cartilage and closure of the wound is performed). Finally, Goutallier proposed a “recession trochleoplasty” to eliminate the supratrochlear spur (Fig. 1c: Goutallier “recession trochleoplasty” aims to decrease patellofemoral compression by increasing the angle between the quadriceps muscle force and the patellar tendon force).
Trochleoplasty has been also combined with other surgical procedures to correct the associated factors of patellar instability in addition to severe trochlea dysplasia, such as tibial tuberosity medialization osteotomy, vastus medialis obliquus (VMO) plasty, reconstruction of the medial patellofemoral ligament (MPFL) or medial reefing [3, 10, 13, 32, 33].
The aim of this systematic review was to compare clinical outcomes and post-operative complication rates in patients who underwent different surgical trochleoplasties. No differences in terms of clinical outcomes and post-operative complication rate were expected amongst the analysed procedures.
Materials and methods
A systematic review of the literature was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines with a PRISMA checklist and algorithm. The search algorithm according to the PRISMA guidelines is shown in Fig. 2. A comprehensive search of PubMed, MEDLINE, CINAHL, Cochrane, EMBASE and Google Scholar data bases using various combinations of the keywords “Dejour trochleoplasty”, “Bereiter trochleoplasty”, “Albee trochleoplasty”, “recession trochleoplasty”, “trochlear dysplasia”, “instability”, “adult” and “clinical outcome” since the inception of the databases until 2016 was performed.
Three independent reviewers (U.G.L., V.C. and N.M.) conducted the search separately. All journals were considered, and all relevant studies were analysed. To qualify for the study, an article had to be published in a peer-reviewed journal. All articles were initially screened for relevance. The three investigators separately reviewed the abstract of each publication and then performed a close reading of all articles and extracted data to minimize selection bias and errors. The last search was performed on 25 September 2016. According to the Oxford Centre of Evidence-Based Medicine, Level I to Level IV articles were found in the literature and included in our study. Articles only in English were included.
Articles that reported clinical outcome or rate of recurrence were included, or both, after a trochleoplasty procedure for the management of patients with trochlear dysplasia. Missing data pertinent to these parameters warranted exclusion from this systematic review. Literature reviews; case reports; studies on animals; on cadavers, or in vitro; biomechanical reports; technical notes; letters to editors; and instructional courses were excluded. Finally, to avoid bias, the selected articles, the relative list of references and the articles excluded from the study were reviewed, assessed and discussed by all the authors. All investigators independently extracted the following data: demographics, type of trochlear dysplasia, type of surgery for the treatment of trochlear dysplasia, additional procedures complications, previous surgery, clinical assessment, months of follow-up, complications and outcome scores.
Quality assessment
To assess the quality of the studies, we used the Coleman Methodology Score (CMS), which assesses methodology with the use of ten criteria, giving a total, score ranging between 0 and 100 points. A score of 100 indicates that the study largely avoids chance, various biases and confounding factors. The final score can be defined as excellent (85–100 points), good (70–84 points), fair (50–69 points) and poor (<50 points). The subsections that make up the CMS are based on the subsections of the CONSORT statement (for randomized controlled trials) and are modified to allow for other trial designs [2]. Coleman criteria were modified to make them reproducible and relevant for the systematic review on trochleoplasty techniques in patients with trochlear dysplasia. Each study was scored by three reviewers (U.G.L., M.C. and V.C.) independently and in triplicate for each of the criteria adopted to give a total CMS between 0 and 100. Each author performed this procedure twice.
Statistical analysis
Statistical analysis with Fisher’s exact test was performed to establish whether the difference of percentage in terms of post-operative pain, patellar redislocation and osteoarthritis was statistical relevant. A p value <0.05 was considered significant.
Results
The literature search and cross-referencing resulted in a total of 75 articles. Finally 14 articles on the treatment of trochlear instability with Dejour V-shaped deepening trochleoplasty [9, 14, 30, 35, 42, 45], Bereiter U-shaped deepening trochleoplasty [4, 6, 15, 28, 37, 41, 43] and Goutallier recession trochleoplasty [39] were included in the final review (Fig. 2).
Demographics (Table 1)
A total of 392 knees in 371 patients were included, with a median age at surgery of 22.5 years ranging from 16 years [35] to 49 years [35]. Patients were assessed at follow-up for an average of 56.6 months (SD 44), ranging from 18 months [42] to 183.6 months [35].
Trochlear dysplasia (Table 1)
Only few authors reported the rate of trochlear dysplasia. Particularly, authors reported that 355 knees from 392 (90.6%) had trochlear dysplasia: 16 (4.5%) knees type A dysplasia according to Dejour’s classification system [15, 35, 39]; 120 (33.8%) type B dysplasia [6, 9, 15, 30, 35, 37, 39, 43]; 34 (9.6%) type C dysplasia [6, 15, 35, 39]; 185 (52.1%) type D dysplasia [6, 9, 14, 15, 28, 30, 35, 39, 41].
Surgical procedures (Tables 1, 2)
The most common procedure used for the treatment of trochlear instability was Bereiter U-shaped deepening trochleoplasty. It was used in 248 knees (63.3% of the procedures). The Dejour V-shaped deepening trochleoplasty, instead, was used in 125 knees (31.9% of the procedures), and the Goutallier recession trochleoplasty was used in 19 knees (4.8% of the procedures) (Table 1).
Other procedures were also performed, in addition to trochleoplasty, including lateral retinaculum release in 191 cases (48.7% of the knees) [9, 14, 15, 30, 37, 39, 41, 45], vastus medialis plasty in 158 cases (40.3% of the knees) [9, 15, 30, 35, 37, 41, 45], medial patellofemoral ligament reconstruction (MPFLR) in 112 cases (28.6% of the knees) [4, 6, 9, 28, 30, 39, 41], tibial tuberosity transfer in 85 cases (21.7% of the knees) [9, 14, 30, 35, 39, 41] and medial reefing in 81 cases (20.7% of the knees) [14, 41, 43, 45] (Table 1).
Outcome measurements and radiological assessment (Table 5)
Several outcome measures were reported in the included studies. The most frequently reported score was the Kujala score, used in 13 (92.9%) of 14 studies [4, 6, 9, 14, 15, 28, 30, 35, 37, 39, 41, 43, 45].
The overall mean value of preoperative and post-operative Kujala score was 53.8 (SD 22.2) and 74 (SD 6.3) points, respectively. Dejour V-shaped trochleoplasty procedure showed a mean preoperative Kujala score of 54 (SD 5.6) and a mean post-operative Kujala score of 79.3 (SD 8.4).The Bereiter U-shaped deepening trochleoplasty had a mean preoperative and post-operative value of 53.8 (SD 29.1) and 64.5 (SD 4.9) points, respectively. Finally in patients who underwent Goutallier recession trochleoplasty, the preoperative Kujala score was not available and the post-operative score was 80.
Four (28.6%) authors used in their studies only radiographs for radiological assessment [35, 42, 43, 45], 5 (35.7%) radiographs and computer tomography [9, 14, 30, 37, 39] and 5 (35.7%) radiographs and MRI [4, 6, 15, 28, 41] (Table 3).
Complications (Tables 3, 4)
The overall rate of complications was 157 (40% of the treated knees). The most common complication was increased pain. It was found in 43 patients (11% of knees) [6, 9, 15, 30, 35, 37, 42, 43]. Similar rate of pain was found between Bereiter U-shaped deepening trochleoplasty (10.8%, 25/248 knees) [6, 15, 37, 43] and Dejour V-shaped deepening trochleoplasty [9, 29, 35, 42] (14.4%, 18/125 knees). No statistical difference was found between the two groups (n.s.). On the contrary, Goutallier procedure did not show an increment of post-operative pain (0%, 0/19 knees).
The second most common complication was the deficit of range of motion (ROM) with an overall rate of 6.7%. In particular, the Bereiter trochleoplasty showed a rate of 2% [4, 14, 28, 39, 41, 42], Dejour procedure a rate of 16% [4, 14, 28, 35, 39, 41, 42] and Goutallier recession trochleoplasty [39] a rate of 5%.
Osteoarthritis occurred in 47 patients [35, 39, 43, 45] with a rate of 4.4% for Bereiter trochleoplasty [43, 45], 16% for Goutallier recession trochleoplasty [35, 39] and 26.5% for Dejour procedure [45]. Statistical differences were highlighted between Bereiter and Dejour procedures (p < 0.05). On the contrary, the different rate between Bereiter and Goutallier and between Dejour and Goutallier recession trochleoplasty showed no statistical difference (n.s.).
The overall rate of patella redislocation was 2%. In particular, the procedure that showed the highest rate was the Goutallier trochleoplasty with a rate of 10.5% [39], followed by Dejour [45] and Bereiter [15, 41] trochleoplasty with a rate of 3.2 and 0.8%, respectively. No statistical differences were found between Bereiter trochleoplasty and the Dejour procedure (n.s.); on the contrary between the first one and Goutallier trochleoplasty, statistical difference was found (n.s.).
Other less frequent complications reported in the included studies were: 5 arthrofibrosis (1.2% of the knees) [42]; 1 tibial tuberosity non-union (0.3% of the knees) [39]; 1 superficial wound infection (0.3% of the knees) [41]; 1 transient post-operative femoral nerve palsy after peripheral anaesthesia (0.3% of the knees) [15]; 1 wound-healing problem (0.3% of the knees) [15]; 1 complex regional pain syndrome (0.3% of the knees) [15]; 1 residual patella baja (0.3% of the knees) [43]; 1 residual oedema (0.3% of the knees) [42]; and 1 deep venous thrombosis (0.3% of the knees) [30].
Quality assessment
The mean value of the CMS score was 76 points, with a range from 84 to 71, showing that the mean quality of included study was good. No statistically significant difference was found between mean values of CMS calculated by the three examiners.
Discussion
The most important findings of this systematic review were that the Bereiter U-shaped deepening trochleoplasty was the most commonly used technique for the treatment of trochlear dysplasia in the included studies with the lowest rate of recurrence and post-operative ROM deficiency. On the other hand, Dejour V-shaped deepening trochleoplasty showed the highest mean post-operative value of Kujala score with 79.3 points. Statistical differences were found in terms of redislocation rate between Goutallier procedure and Bereiter trochleoplasty (p < 0.05) and in terms of post-operative osteoarthritis between Goutallier procedure and Dejour V-shaped deepening trochleoplasty (p < 0.05).
The three major types of trochleoplasty were associated with significantly improved stability, function and Kujala scores and a relatively low rate of osteoarthritis and pain. Nevertheless, the risks of osteoarthritis from trochleoplasty procedures are unclear. Degenerative changes of patellofemoral joint can be found in most of the cases at the time of surgery [43], and a conservative management could lead to a high degree of osteoarthritis. The currently available evidence is not sufficient to prove that trochleoplasty procedures lead to patellofemoral osteoarthritis. Rouanet et al. [35] evaluated a series of sulcus deepening trochleoplasties with a mean post-operative follow-up of 15 years. Given the long follow-up period, this study is of course the right to consider the long-term effects of sulcus deepening trochleoplasty. Particularly, this study shows that sulcus deepening trochleoplasty leads to osteoarthritis: ten cases of preoperative patellofemoral osteoarthritis were identified, but none with >Iwano 2, whilst osteoarthritis was present in 33 of 34 cases at the final follow-up with 20 cases >Iwano 2 (65%). The limitation of this study is that trochleoplasty was never performed alone, so is difficult to evaluate exactly effect of this procedure.
Of the 392 knees treated, type D dysplasia was found to be the most common (47.1%).
There is not a consensus on the correct management of patellar instability: it is a multifactorial condition and non-trochleoplasty procedures could have acceptable clinical outcomes and provide adequate stability [40]. On the other hand, recent studies reported negative clinical outcome after isolated MPFLR in treating patellar instability [44] with a high rate of recurrent instability [38], especially in patients with severely dysplastic trochleas. Other procedures, such as isolated tibial tubercle transfer, could leave recurrent instability in patients with dysplastic trochleas [24, 26]. The aim of transfer of the tibial tuberosity is to restore the tibial tuberosity–trochlear groove distance (TT–TG) and Q-angle and manage patellofemoral instability, lateral patellar overload, tilt, compression, and to unload lateral or distal patellar cartilage lesions [19]. Several procedures have been described. Roux firstly performed tibial tubercle medialization for instability of the patella [36]; Hauser, subsequently, reported a posterior and medial shift of the patella [36]. Maquet described an anteriorization of the tubercle. Later Elmslie–Trillat reported a technique for reduction in contact pressures, later modified by Fulkerson [19].
Elmslie–Trillat procedure (the pure medial transfer of the tibial tuberosity) is indicated for patients without osteoarthritis and has excellent outcomes [27]. However, it seems to lead to patella-femoral osteoarthritis during long-term follow-up [26]. On the other hand, Fulkerson procedure is the combination of medial and anterior transfer. This procedure provides excellent outcomes also in patients with severe patellofemoral osteoarthritis [7]. However, single application of Fulkerson procedure for recurrent patellar dislocation with severe patella alta increases the risk of post-operative patellar instability [40].
It has been well documented that to leave the dysplastic trochlea surface leads to unfavourable results [29]. Satisfactory clinical outcomes were reported after a trochleoplasty in patients with previous failed non-trochleoplasty management for patellar instability in whom dysplastic trochlea was left untreated [11].
Conversely, the main trochleoplasty procedures have been documented to be safe and successful in terms of post-operatively improvement in outcome scores [29, 37, 42, 45]. The purpose of these procedures is to improve patellofemoral congruency taking into consideration the abnormal shape of the opposing patella.
The Bereiter U-shaped deepening trochleoplasty was first described in 1994, whereby a lateral parapatellar approach is used to deepen the distal femoral subchondral bone (used in 248 knees, 63.3% of all procedures). Also used in the most studies (7 of 14), and with the lowest percentage of ROM deficiency (2%), it has been shown to be a safe technique with good outcomes [15, 25, 29].
However, this technique had many post-operative pain reports (10.08%). This is particularly important since pain was the most commonly reported complication post-operatively, found in 43 patients (11% of the knees). This shows that whilst a given trochleoplasty technique may perform well post-operatively in one area, it may disappoint in others.
Patellofemoral pain, presenting before trochleoplasty, may in part be explained by osteoarthritic changes of the patellofemoral joint in the long term, and the technique itself may represent a predisposing factor for osteoarthritis [20,21,22,23]. On the other side, the damage to the articular cartilage and the patellofemoral osteoarthritis may be caused by recurrent patellar dislocations without surgical intervention [18, 31, 34].
The Dejour V-shaped deepening trochleoplasty was used in 125 knees (31.9% of the procedures). In this procedure, the flap created by resection of cancellous bone forms the new trochlea and is fixed with two staples, restoring the normal trochlear groove proximally. Whilst the Dejour V-shaped deepening trochleoplasty had a rate of post-operative pain similar to Bereiter trochleoplasty, it had a low rate of patellar redislocations (3.2%) and the highest rate of patients with ROM deficiency (16%). The differences observed in post-operative stiffness and pain may be attributed to different surgical techniques amongst authors, different rehabilitation protocols after trochleoplasty, and different indications for trochleoplasty. This further substantiates the notion that different trochleoplasty techniques have their advantages and disadvantages and that there may not be one technique that stands out as superior.
The mean preoperative Kujala score in patients who underwent Dejour V-shaped deepening trochleoplasty score had increased 25.3 points post-operatively (54 points preoperatively to 79.3 points post-operatively). This was compared to a mean increase in Kujala score of 10.7 for patients who underwent Bereiter U-shaped deepening trochleoplasty (53.8 points preoperatively to 64.5 points post-operatively). This demonstrates the clinical outcomes of the trochleoplasty procedures were significantly improved at the final follow-up in most of the studies (Table 5). In patients who underwent Goutallier recession trochleoplasty, the preoperative Kujala score was not available and the post-operative score was 80.
However, it cannot be said that the Dejour V-shaped deepening trochleoplasty is superior to the Bereiter U-shaped deepening trochleoplasty, based on the Kujala score alone. Firstly, as noted, the Kujala is a subjective scoring system and as such is liable to selection bias. Secondly, because there is a discrepancy in the number of procedures performed, with Dejour trochleoplasty being used in only 31.9% of knees, compared to the Bereiter trochleoplasty in 63.3% of knees, it is difficult to conclude that this is an accurate representation of the total population of patients undergoing these procedures [17].
The Goutallier recession trochleoplasty is performed by removing a supratrochlear spur alone, whilst preserving the shape of the trochlea [16]. Since this procedure was used in only 19 knees (4.8% of procedures), it is difficult to draw an accurate conclusion on the outcome scores and complication rates. This procedure was introduced in 2002, and uptake of the procedure amongst patella-femoral surgeons may be slow. None of the patients who underwent this procedure had pain post-operatively, but it had a high rate of patellar redislocations (10.5%).
The difference in numbers of surgical techniques warrants further investigation as to why this is the case. This may be purely as a result of surgeon preference. It is interesting to note that most authors agree that trochleoplasty is an extremely successful treatment for patellar dislocation in the setting of trochlea dysplasia, regardless of the type of technique [29]. Despite this, trochleoplasty has been described as a technically challenging and demanding procedure, and adaptations will continually be made wherever it is deemed beneficial. With such precise indications, trochleoplasty may not be a procedure that orthopaedic surgeons are greatly familiar with.
There are some limitations inherent within this study. These mainly include the lack of reporting in some of the studies that we have analysed and some concern regarding the methods used within those studies. First, it is difficult to evaluate the efficacy of trochleoplasty as a single procedure because most of the patients present concomitant anomalies that need associated correction.
Ideally, all of the studies should report the same standardized scoring systems, to make analysis more homogenous. However, the Tegner score, the International Knee Documentation Committee (IKDC) score, the Knee Injury and Osteoarthritis Outcome Score (KOOS) and the WOMAC, Western Ontario McMasters Osteoarthritis Index, was used in only 4 (28.6%), 7 (50%), 2 (14.3%) and 2 (14.3%) studies, respectively. Also, the Oxford Knee Score, the activity rating scale (ARS), the Larsen–Lauridsen score and the Lysholm and Gillquist scores were only used in one study each. Furthermore, radiographic analysis, computer tomography and MRI, more objective outcome measures, were only used in 4 (28.6%), 5 (35.7%) and 5 (35.7%) studies, respectively. This makes comparing the different studies difficult, as each scoring system assesses a different aspect of post-operative performance.
The variability of different procedures previously undertaken may be a source of confounding. In order to truly characterize the differences between the main trochleoplasty procedures described earlier, all other variables in the studies analysed would ideally be the same. However, this level of control is impossible; large sample sizes should be analysed; therefore, a compromise must be made. Not only will the presence of previous surgery impact on the outcomes, but trochleoplasty is, out of necessity, combined with various other soft tissue procedures [8, 29].
Finally, the limitations of our review are similar to those of the articles that we assessed. Most of the studies we analysed were of Level IV evidence, consigning our systematic review to the same limitations inherent within this level of evidence. Also, since the method of data collection was mostly retrospective, this method is subject to limitations such as selection and information bias. Finally, retrospective analyses are not able to accurately determine the temporal relationship between procedural technique and outcomes post-operatively, compared to a prospective study.
The results of this study are useful for clinicians to compare clinical outcomes of patients treated with different trochleoplasty procedures, the rate of complications and recurrence of patellar dislocation.
Conclusion
Bereiter trochleoplasty is the most efficient procedure in terms of post-operative patellar redislocation, post-operative osteoarthritis and ROM, but the highest mean post-operative Kujala score is obtained by Dejour procedure. Therefore, none of the surgical techniques analysed have shown a real supremacy. This finding is probably due to the poor quality of studies available in the current literature resulting in the inability to perform a meta-analysis.
Change history
22 November 2019
A Correction to this paper has been published: https://doi.org/10.1007/s00167-019-05784-w
References
Albee F (1915) Bone graft wedge in the treatment of habitual dislocation of the patella. Med Rec 88:257–259
Altman DG, Schulz KF, Moher D, Egger M, Davidoff F, Elbourne D et al (2001) The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Ann Intern Med 134:663–694
Arendt E (2009) MPFL reconstruction for PF instability: the soft (tissue) approach. Orthop Traumatol Surg Res 95:S97–S100
Banke IJ, Kohn LM, Meidinger G, Otto A, Hensler D, Beitzel K, Imhoff AB, Schöttle PB (2014) Combined trochleoplasty and MPFL reconstruction for treatment of chronic patellofemoral instability: a prospective minimum 2-year follow-up study. Knee Surg Sports Traumatol Arthrosc 22:2591–2598
Bereiter H, Gautier E (1994) Die trochleaplastik als chirurgische Therapie der rezidivierenden Patellaluxation bei Trochleadysplasie des Femurs. Arthroskopie 7:281–286
Blønd L, Haugegaard M (2014) Combined arthroscopic deepening trochleoplasty and reconstruction of the medial patellofemoral ligament for patients with recurrent patella dislocation and trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc 22:2484–2490
Carofino BC, Fulkerson JP (2008) Anteromedialization of the tibial tubercle for patellofemoral arthritis in patients > 50 years. J Knee Surg 21:101–105
Crossley KM, Bennell KL, Cowan SM, Green S (2004) Analysis of outcome measures for persons with patellofemoral pain: which are reliable and valid? Arch Phys Med Rehabil 85:815–822
Dejour D, Byn P, Ntagiopoulos PG (2013) The Lyon’s sulcus-deepening trochleoplasty in previous unsuccessful patellofemoral surgery. Int Orthop 37:433–439
Dejour D, Le Coultre B (2007) Osteotomies in patello-femoral instabilities. Sports Med Arthrosc 15:39–46
Dejour D, Saggin P (2010) The sulcus deepening trochleoplasty: the Lyon’s procedure. Int Orthop 34:311–316
Dejour H, Walch G, Neyret P, Adeleine P (1990) Dysplasia of the femoral trochlea. Rev Chir Orthop Reparatrice Appar Mot 76:45–54 (in French)
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2:19–26
Donell ST, Joseph G, Hing CB, Marshall TJ (2006) Modified Dejour trochleoplasty for severe dysplasia: operative technique and early clinical results. Knee 13:266–273
Fucentese SF, Zingg PO, Schmitt J, Pfirrmann CW, Meyer DC, Koch PP (2011) Classification of trochlear dysplasia as predictor of clinical outcome after trochleoplasty. Knee Surg Sports Traumatol Arthrosc 19:1655–1661
Goutallier D, Raou D, Van-Driessche S (2002) Retro-trochlear wedge reduction trochleoplasty for the treatment of painful patella syndrome with protruding trochleae. Technical note and early results. Rev Chir Orthop Reparatrice Appar Mot 88:678–685
Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O (1993) Scoring of patellofemoral disorders. Arthroscopy 9:159–163
Longo UG, Loppini M, Berton A, Marinozzi A, Maffulli N, Denaro V (2012) The FIFA 11 + program is effective in preventing injuries in elite male basketball players: a cluster randomized controlled trial. Am J Sports Med 40:996–1005
Longo UG, Rizzello G, Ciuffreda M, Loppini M, Baldari A, Maffulli N et al (2016) Elmslie–Trillat, Maquet, Fulkerson, Roux Goldthwait, and Other Distal Realignment Procedures for the Management of Patellar Dislocation: systematic review and quantitative synthesis of the literature. Arthroscopy 32:929–943. doi:10.1016/j.arthro.2015.10.019
Maffulli N, Longo UG, Gougoulias N, Caine D, Denaro V (2011) Sport injuries: a review of outcomes. Br Med Bull 97:47–80
Maffulli N, Longo UG, Gougoulias N, Loppini M, Denaro V (2010) Long-term health outcomes of youth sports injuries. Br J Sports Med 44:21–25
Maffulli N, Longo UG, Spiezia F, Denaro V (2011) Aetiology and prevention of injuries in elite young athletes. Med Sport Sci 56:187–200
Maffulli N, Longo UG, Spiezia F, Denaro V (2010) Sports injuries in young athletes: long-term outcome and prevention strategies. Phys Sportsmed 38:29–34
Marcacci M, Zaffagnini S, Lo Presti M, Vascellari A, Iacono F, Russo A (2004) Treatment of chronic patellar dislocation with a modified Elmslie–Trillat procedure. Arch Orthop Trauma Surg 124:250–257
Masse Y (1978) Trochleoplasty. Restoration of the intercondylar groove in subluxations and dislocations of the patella. Rev Chir Orthop Reparatrice Appar Mot 64:3–17
Nakagawa K, Wada Y, Minamide M, Tsuchiya A, Moriya H (2002) Deterioration of long-term clinical results after the Elmslie–Trillat procedure for dislocation of the patella. J Bone Joint Surg Br 84:861–864
Naranja RJ Jr, Reilly PJ, Kuhlman JR, Haut E, Torg JS (1996) Long-term evaluation of the Elmslie–Trillat–Maquet procedure for patellofemoral dysfunction. Am J Sports Med 24:779–784
Nelitz M, Dreyhaupt J, Lippacher S (2013) Combined trochleoplasty and medial patellofemoral ligament reconstruction for recurrent patellar dislocations in severe trochlear dysplasia: a minimum 2-year follow-up study. Am J Sports Med 41:1005–1012
Ntagiopolous PG, Dejour D (2014) Current concepts on trochleopalasty procedures for the surgical treatment of trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc 22:2531–2539
Ntagiopoulos PG, Byn P, Dejour D (2013) Midterm results of comprehensive surgical reconstruction including sulcus-deepening trochleoplasty in recurrent patellar dislocations with high-grade trochlear dysplasia. Am J Sports Med 41:998–1004
Oliva F, Ronga M, Longo UG, Testa V, Capasso G, Maffulli N (2009) The 3-in-1 procedure for recurrent dislocation of the patella in skeletally immature children and adolescents. Am J Sports Med 37:1814–1820
Placella G, Speziali A, Sebastiani E, Morello S, Tei MM, Cerulli G (2016) Biomechanical evaluation of medial patello-femoral ligament reconstruction: comparison between a double-bundle converging tunnels technique versus a single-bundle technique. Musculoskelet Surg 100(2):103–107
Placella G, Tei M, Sebastiani E, Speziali A, Antinolfi P, Delcogliano M et al (2015) Anatomy of the Medial Patello–Femoral Ligament: a systematic review of the last 20 years literature. Musculoskelet Surg 99:93–103
Ronga M, Oliva F, Longo UG, Testa V, Capasso G, Maffulli N (2009) Isolated medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med 37:1735–1742
Rouanet T, Gougeon F, Fayard JM, Remy F, Migaud H, Pasquier G (2015) Sulcus deepening trochleoplasty for patellofemoral instability: a series of 34 cases after 15 years postoperative follow-up. Orthop Traumatol Surg Res 101:443–447
Roux C (1979) The classic. Recurrent dislocation of the patella: operative treatment. Clin Orthop Relat Res 144:4–8
Schöttle PBFS, Pfirrmann C, Bereiter H, Romero J (2005) Trochleaplasty for patellar instability due to trochlear dysplasia: a minimum 2-year clinical and radiological follow-up of 19 knees. Acta Orthop 76(5):693–698
Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C (2012) A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med 40:1916–1923
Thaunat M, Bessiere C, Pujol N, Boisrenoult P, Beaufils P (2011) Recession wedge trochleoplasty as an additional procedure in the surgical treatment of patellar instability with major trochlear dysplasia: early results. Orthop Traumatol Surg Res 97:833–845
Tsuda E, Ishibashi Y, Yamamoto Y, Maeda S (2012) Incidence and radiologic predictor of postoperative patellar instability after Fulkerson procedure of the tibial tuberosity for recurrent patellar dislocation. Knee Surg Sports Traumatol Arthrosc 20:2062–2070
Utting MR, Mulford JS, Eldridge JD (2008) A prospective evaluation of trochleoplasty for the treatment of patellofemoral dislocation and instability. J Bone Joint Surg Br 90:180–185
Verdonk R, Jansegers E, Stuyts B (2005) Trochleoplasty in dysplastic knee trochlea. Knee Surg Sports Traumatol Arthrosc 13:529–533
von Knoch F, Böhm T, Bürgi ML, von Knoch M, Bereiter H (2006) Trochleaplasty for recurrent patellar dislocation in association with trochlear dysplasia; a 4- to 14- year follow up-study. J Bone Joint Surg Br 88:1331–1335
Wagner D, Pfalzer F, Hingelbaum S, Huth J, Mauch F, Bauer G (2013) The influence of risk factors on clinical outcomes following anatomical medial patellofemoral ligament (MPFL) reconstruction using the gracilis tendon. Knee Surg Sports Traumatol Arthrosc 21:318–324
Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, Luetzow WF, Vaccari V, Benzi A, Marcacci M (2014) Medial patellotibial ligament (MPTL) reconstruction for patellar instability. Knee Surg Sports Traumatol Arthrosc 22:2491–2498
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Funding
No external source of funding was used.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
No informed consent was necessary for this study.
Rights and permissions
About this article
Cite this article
Longo, U.G., Vincenzo, C., Mannering, N. et al. Trochleoplasty techniques provide good clinical results in patients with trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc 26, 2640–2658 (2018). https://doi.org/10.1007/s00167-017-4584-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4584-9