Abstract
Purpose
Excellent results of anteromedialization of the tibial tuberosity for recurrent patellar dislocation have been reported; however, the contribution of the preoperative anatomic factors to postoperative patellar instability has not been well established. The purpose of this study was to investigate the mid-term results and the incidence of postoperative patellar instability after Fulkerson procedure for recurrent patella dislocation, and to determine the radiologic predictor of the postoperative patellar instability.
Methods
Sixty-two knees of 41 patients underwent Fulkerson procedure with or without lateral retinacular release for recurrent patellar dislocation and were followed-up for 85–155 months. Predisposing anatomic factors for recurrent patellar dislocation were evaluated preoperatively, including valgus knee alignment (femorotibial angle), patella alta (Insall–Salvati ratio), trochlear dysplasia (trochlear depth), lateral patellar displacement (congruence angle) and lateral malposition of the tibial tuberosity (tibial tuberosity-trochlear groove distance). The relationship between the measurements of anatomic factors and postoperative patellar instability, which was defined by the patellar re-dislocation or residual apprehension after surgery, was analyzed.
Results
The Fulkerson score and the Kujala score were significantly improved from the median of 65 (35–80) points and 68 (36–82) points preoperatively to 95 (60–100) points and 92 (57–100) points at the final follow-up, respectively. Three knees (4.8%) experienced postoperative patellar re-dislocation and 4 knees (6.5%) showed the positive apprehension sign at the final follow-up. The statistical analysis showed that the postoperative patellar instability correlated with only patella alta.
Conclusion
Patella alta was the only predictor of postoperative patellar instability after Fulkerson procedure. These results indicated that isolated Fulkerson procedure should not be indicated for recurrent patellar dislocation with severe patella alta.
Level of evidence
Case–control study, Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Transfer of the tibial tuberosity has a long history of being widely recommended as first choice for recurrent patellar dislocation, and it was supported by clinical investigations showing that the patellar instability was significantly associated with the tibial tuberosity-trochlear groove distance (TT-TG) [13, 31]. Hauser procedure [20], which is the medial and distal transfer of the tibial tuberosity, has an advantage of correcting patella height, while the high incidence of patellofemoral osteoarthritis caused by simultaneous posterior transfer has been reported [11, 19]. Excellent outcomes of Elmslie-Trillat procedure [5, 42, 45], which is the pure medial transfer, would be expected for patients without osteoarthritis [35]; however, patellofemoral arthritic change has developed during long-term follow-up [33]. Fulkerson procedure, which is the combination of medial and anterior transfer, has a biomechanical superiority of decreasing the patellofemoral contact pressure [6], and the satisfactory results were obtained for the patients with severe patellofemoral osteoarthritis [17] and the active older patients with patellofemoral osteoarthritis [9]. Another concern after tibial tuberosity transfer is recurrent patellar instability, which has been reported in the literature to have an incidence of approximately 10% [5, 31, 39, 42]. Since recurrent patellar dislocation is multifactorial [31, 37], tibial tuberosity transfer can directly correct only the lateral malposition of the tibial tuberosity, and other anatomical predisposing factors theoretically remain. It remains questionable whether these curable and incurable aspects of anatomical pathology affect the postoperative outcome of recurrent patellar dislocation. For success of the Fulkerson procedure, it is important to understand what particular predisposing anatomic factors have a deleterious impact on the clinical results.
The purpose of this study was to demonstrate the mid-term results of Fulkerson procedure for recurrent patellar dislocation with particular focus on: (1) clinical knee function and radiologic patellofemoral congruency, (2) the contribution of the patellofemoral cartilage lesion, (3) the incidence of postoperative patellar instability with postoperative re-dislocation or residual patellar apprehension, and (4) the contribution of predisposing anatomic factors such as valgus knee alignment, patella alta, trochlear dysplasia, lateral displacement of the patella and lateral malposition of the tibial tuberosity. It was hypothesized that successful clinical results could be achieved regardless of the severity of patellofemoral cartilage lesions, and patella alta and trochlear dysplasia that were incurable with Fulkerson procedure would be a radiologic predictor of postoperative patellar instability.
Materials and methods
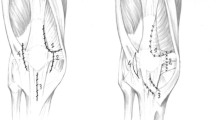
The indication for using Fulkerson procedure in our institute was a knee that fulfilled all the following criteria: (1) a history of patellar subluxation more than 2 times, which was defined as an episode of acute anterior knee pain with a feeling of lateral patellar slipping, or dislocation which was confirmed with direct or indirect findings in imaging examinations; (2) residual anterior knee pain or apprehension; (3) positive apprehension sign [15] and positive active patellar subluxation test [22]; (4) over two quadrants glide in the lateral patellar glide test [25]; (5) lateral shift and tilt of the patella demonstrated on Merchant axial radiographs [29]; (6) lateral malposition of the tibial tuberosity with more than 15 mm of the TT-TG in CT images; and (7) skeletal maturation with closed physis of the proximal tibia on MRI [41]. From 1996 to 2002, 90 knees of 57 patients were seen who matched the surgical indication of Fulkerson procedure (Fig. 1). The exclusion criteria from this study were (1) a surgical history of the involved knee, which was not related to the patellofemoral disorders; (2) concomitant cartilage lesion of the femorotibial joint, meniscus injury or ligament injury; (3) combined proximal realignment surgery except lateral retinacular release; and (4) less than 7 years of postoperative follow-up. Six patients who had femorotibial cartilage lesion, medial meniscus injury or anterior cruciate ligament tear were excluded, while 4 patients with prior MPFL repair and 1 patient with prior lateral retinacular release were involved in this study. In our institute at that time, Fulkerson procedure was the first choice surgery for recurrent patellar dislocation which fulfilled above-mentioned criteria, and therefore all 80 knees of 51 patients who matched the surgical criteria were treated with Fulkerson procedure with or without lateral retinacular release. The study design was approved by the ethics committee in our institution (registration number 20-11-013), and all 51 patients provided informed consent to participate in this prospective study.
Preoperative radiologic evaluation
The predisposing anatomic factors were quantitatively assessed by measuring the following radiologic indicators on anteroposterior, lateral and axial radiographs and CT images obtained preoperatively: (1) femorotibial angle consisting of the distal femoral axis and the proximal tibial axis for detecting valgus knee alignment; (2) Insall–Salvati ratio (ISR) for detecting patella alta [23]; (3) trochlear depth for detecting trochlear dysplasia [13] (Fig. 2); (4) congruence angle on the Merchant view for detecting lateral displacement of the patella [29] (Fig. 3); and (5) TT-TG on superimposed CT images for detecting lateral malposition of the tibial tuberosity [13] (Fig. 4). In addition, the minimum distance of patellofemoral joint space was measured on skyline view of axial radiographs for assessing the development of patellofemoral osteoarthritis [24]. The medialization distance to normalize the TT-TG to 10–15 mm was estimated from the CT measurements. All radiologic measurements were performed on a digital radiography system (FCR, Fujifilm Medical Co Ltd, Tokyo, Japan), and the intraclass correlation coefficient calculated for the reliability of measurement was between 0.84 and 0.96 for all radiologic indicators.
Measurement of the trochlear depth. The trochlea depth was the distance from the floor of trochlea (B) to the most anterior condylar contour line (A) along a line subtended 15 degrees distal from the perpendicular that intersected the tangent of the posterior femoral cortex and the most proximal portion of the posterior femoral condyles
Measurement of the tibial tuberosity-trochlear groove distance (TT-TG) using the superimposed femoral and tibial CT images. The TT-TG was the separate distance between 2 parallel lines, which were one line passing through the center of tibial tuberosity and another passing through line at the bottom of the trochlear groove perpendicular to the posterior condylar line
Surgery
After induction of general anesthesia, the lateral patellar glide test, the medial patellar glide test and the passive patellar tilt test were performed to examine the patellofemoral passive stabilizers [25]. Either a medial patella glide of one quadrant or less, or inability to lift the transverse axis of the patella beyond the horizontal required adding lateral retinacular release in 56 knees (90.3%) to treat the over-tightened lateral soft tissue. The cartilage lesion was arthroscopically classified using the International Cartilage Repair Society (ICRS) articular cartilage injury classification (http://www.cartilage.org). Fulkerson procedure was performed according to the techniques described by Fulkerson [16] with some modifications: (1) a transverse skin incision of approximately 5 cm was made on the distal edge of the tibial tuberosity to preserve the infrapatellar branch of the saphenous nerve [30]; (2) 2 Kirschner wires were used as the osteotomy guide to minimize a risk of injury to the anterior tibial vessels and the peroneal nerve; (3) the tibial tuberosity was anteromedially transferred so that the medialization estimated from the preoperative CT images was achieved; and (4) the cancellous bone harvested from the lateral tibial plateau was grafted beside the medial osteotomy site to promote earlier bone-to-bone healing. After fixation with 2 bicortical screws, the medialization distance of the lateral cortex of the tibial tuberosity was measured on the coronal plane the site of maximum distance, and the average and SD were 13.5 ± 3.2 (10–22) mm.
Rehabilitation
The range of motion exercise with a continuous passive motion machine and isometric quadriceps exercise was started from the day after surgery. Partial weight-bearing gait with a knee extension brace was allowed as the patient tolerated, and full weight-bearing gait was permitted after 2 weeks. Aggressive quadriceps and hamstrings muscle exercise was added after 8 weeks or more. Running and full sports activities were permitted after 3 and 6 months, respectively.
Outcome evaluation
Overall knee function was evaluated with the Fulkerson score [17] and the Kujala score [26]. The Knee Injury and Osteoarthritis Outcome Score (KOOS) was used for a patient-administered assessment [34]. Radiographic measurements of the congruence angle, the ISR and the minimum distance of patellofemoral joint space were followed postoperatively. Postoperative patellar instability, which was defined by the presence of patellar re-dislocation or positive apprehension sign during the follow-up period, was investigated. In knees which required revision surgery for recurrent patellar instability, the data obtained just before the revision surgery were used as the data at the final follow-up.
Statistical analysis
The Fulkerson score and the Kujala score were compared between preoperative and at the final follow-up using the Wilcoxon signed rank test. The change in the congruence angle, the ISR and the minimum patellofemoral joint space were analyzed using the repeated measure ANOVA. Based on the most advanced cartilage lesion, the patients were divided into the group with ICRS 0, 1 or 2 lesion (ICRS 0-1-2 group) and the group with ICRS 3 or 4 lesion (ICRS 3-4 group). The Fulkerson score, the Kujala score and the KOOS were compared between the 2 groups using the Mann–Whitney U test. Also, the patients were divided into the recurrent group and the non-recurrent group based on the presence of postoperative patellar instability. The Fulkerson score, the Kujala score, the KOOS and the preoperative radiologic indicators were compared between the 2 groups using the Mann–Whitney U test. Logistic regression analysis was performed with the presence of postoperative patellar instability as the dependent variable and the preoperative radiologic indicators as the independent variables. Our power analysis showed that the smallest study population in each group was 7 for more than 90% of statistical power if there was a difference of 2 mm with a SD of 1 mm in the TT-TG, or a difference of 0.10 with a SD of 0.05 in the ISR. All analyses were performed using SPSS version 16.0 software (SPSS Inc, Chicago, Illinois), with a significant level of 0.05.
Results
Two patients who underwent Avikainen adductor magnus tenodesis [4] combined with Fulkerson procedure were excluded from the study and another 8 patients were lost to follow-up. Consequently, 62 knees (77.5%) of 41 patients (80.3%) consisting of 33 females and 8 males were followed-up more than 7 years postoperatively and were involved in the data analysis. The average age at surgery was 20 ± 7 (12–42) years, and the average follow-up period was 115 ± 20 (85–155) months.
In the preoperative evaluation, the average value of each radiologic indicator was 176 ± 2 (172–181) degrees for the femorotibial angle (Fig. 5a), 1.23 ± 0.11 (0.93–1.47) for the ISR (Fig. 5b), 2 ± 2 (0–7) mm for the trochlear depth (Fig. 5c), 23 ± 13 (0–60) degrees for the congruence angle (Fig. 5d) and 23 ± 4 (15–33) mm for the TT-TG (Fig. 5e). All 62 knees showed the positive crossing sign, and there were 16 knees in type A, 34 knees in type B, 9 knees in type C and 3 knees in type D [12]. Under arthroscopic examination, cartilage lesions were observed in 44 knees (71.0%; Table 1), and 51 knees of 31 patients and 11 knees of 10 patients were assigned into the ICRS 0-1-2 group and the ICRS 3-4 group, respectively.
The histograms of the radiologic indicators for the predisposing anatomical factors: a femorotibial angle, b Insall–Salvati ratio, c trochlear depth, d congruence angle, and e tibial tuberosity-trochlear groove distance (TT-TG). The solid and dotted lines in the histograms indicate the values of average minus 1 SD and average plus 1 SD, respectively
The Fulkerson score and the Kujala score were significantly improved at the final follow-up compared to the preoperative value (Table 2). The excellent (100–95), very good (94–90), good (89–80), fair (79–70) and poor (less than 70) grade in the postoperative Fulkerson score accounted for 53.7, 26.8, 9.8, 2.4 and 7.3%, respectively. The KOOS at the final follow-up was 95 ± 9 points for pain, 94 ± 9 points for symptoms, 97 ± 6 points for activities of daily living, 91 ± 15 points for sport and recreation function, and 89 ± 15 points for knee-related quality of life. The congruence angle was significantly decreased from 23 ± 13 degrees preoperatively to 0 ± 13 degrees at the 1-year postoperative follow-up (P < 0.001) and 1 ± 13 degrees at the final follow-up (P < 0.001). The ISR was significantly decreased from 1.23 ± 0.11 preoperatively to 1.17 ± 0.13 at the 1-year postoperative follow-up (P < 0.001) and 1.17 ± 0.13 at the final follow-up (P < 0.001). The minimum distance of patellofemoral joint space was 5 ± 2 mm preoperatively, 5 ± 2 at the 1-year postoperative follow-up and 5 ± 2 at the final follow-up, representing no significant difference.
The Fulkerson score and the Kujala score at the final follow-up were not different between the ICRS 0-1-2 group and the ICRS 3-4 group (Table 2). In the KOOS, significant difference was detected only in knee-related quality of life between 93 ± 8 points for the ICRS 0-1-2 group and 78 ± 15 points for the ICRS 3-4 group (P = 0.014).
Three knees (4.8%) experienced postoperative patellar re-dislocation, which was diagnosed with direct or indirect findings in imaging examinations, 4 knees (6.5%) showed a positive apprehension sign during the follow-up, and they were assigned into the recurrent group. At the final follow-up, the Fulkerson score and the Kujala score for the recurrent group were significantly lower compared to those for the non-recurrent group, respectively (Table 2). In the KOOS, significant difference was detected in sport and recreation function (97 ± 4 points for the recurrent group vs. 73 ± 22 points for the non-recurrent group, P = 0.010) and in knee-related quality of life (94 ± 7 points for the recurrent group vs. 76 ± 14 points for the non-recurrent group, P = 0.003). In the comparison of predisposing anatomic factors between the recurrent and non-recurrent group, significant difference was detected in only the ISR (P = 0.002; Table 3). The logistic regression analysis also showed that only the ISR statistically correlated with the recurrence of the patellar instability after Fulkerson procedure (P = 0.009; Table 4). The increase by 0.1 in the ISR elevated the risk of the postoperative patellar instability by 6.8 times.
Two of 3 knees with postoperative patellar re-dislocation underwent MPFL reconstruction as revision surgery. One knee with nonunion of the osteotomy site received a revision surgery of the screw fixation with a cancellous bone graft. No patients had other surgical complications of superficial or deep infection, neurovascular injury, deep venous thrombosis or joint contracture.
Discussion
The most important findings of the present study were (1) good clinical results with the improved knee functional scores and the corrected patellofemoral congruency at the final follow-up, (2) no deteriorative effect of the advanced cartilage lesion in the preoperative patellofemoral joint on the knee functional scores, (3) the incidence of 11.3% for postoperative patellar instability, and (4) increased risk of the postoperative patellar instability in the knees with the larger ISR.
In this study, 90.3% of patients were rated as excellent to good in the Fulkerson score at the final follow-up, and it was close to previously reported results of 88.5 and 86.1%, which are results of studies using the same surgical techniques and evaluation scale [8, 17]. The radiologic evaluation showed that the corrected congruence angle was preserved in an equal range from 1 year postoperatively to the final follow-up. The Fulkerson score and the Kujala score in the ICRS 3-4 group were not significantly different from those in the ICRS 0-1-2 group, supporting the similar results in the previous reports [8, 17]. No significant change in the patellofemoral joint space could reflect the unloading effect of anteromedialization on the patellofemoral joint [6, 17].
There were 11.3% of knees associated with postoperative patellar instability during an average follow-up of 115 months. The result was comparable to the 8.6–15.2% recurrent instability rate after the modified Elmslie-Trillat procedure [5, 31, 39, 42] and the modified Fulkerson procedure [1], although the definitions of postoperatively recurrent instability varied. The statistical analysis partially supported our hypothesis; patella alta was the radiologic predictor of recurrent patellar instability after the Fulkerson procedure, while the trochlear dysplasia was not. All 7 knees that resulted in recurrent patellar instability showed a larger ISR than the average, and the ISR in 4 of 7 knees were over the average plus 1 SD. Marcacci et al. [28] reported a supplemental effect of the modified Elmslie-Trillat procedure on the decrease in patellar height. Also in this study, the ISR was decreased from 1.35 ± 0.07 preoperatively to 1.31 ± 0.09 at 1 year postoperative follow-up and 1.30 ± 0.07 at the final follow-up even in the recurrent group (Fig. 6). However, those were still statistically higher compared to 1.16 ± 0.12 at 1 year postoperative follow-up (P = 0.003) and 1.15 ± 0.12 at the final follow-up (P = 0.002) in the non-recurrent group, respectively (in 2-way ANOVA and Tukey’s post hoc test). The mismatch between the patellar joint surface and the trochlear joint surface in a sagittal plane causes lateral patellar instability [7, 31]. In the knee with patella alta, the patella glides a longer distance on the flat or convex surface of the supracondyle and upper trochlear, and it exposes the patella to a risk of dislocation or subluxation in a larger range of knee motion. Furthermore, the longer patellar tendon compromises the effect of the tibial tuberosity medialization on correcting the quadriceps angle. In contrast, no statistical correlation was detected between the trochlear depth and postoperative patellar instability. In this series, the trochlear depth in 89% of the knees was 4 mm or less, and this small range of variation might mask the effect of shallow trochlear grove and cause no statistical correlation with the postoperative patellar instability.
The question of what surgical procedure is best for the treatment of recurrent patellar dislocation with patella alta remains. MPFL reconstruction has an advantage of reproducing the primary restraint against lateral patellar displacement [14, 21, 32, 40], while the single application of MPFL reconstruction to the knee with patella alta is questionable. Nomura [36] reported that only 2 of 24 MPFL-reconstructed knees experienced postoperative re-dislocation or subluxation in the long-term follow-up; however, the series involved only 1 knee with the ISR more than 1.25. Arendt [3] specified the patellar height with the ISR less than 1.2 as one of the indication criteria for isolated MPFL reconstruction. Undesirable distribution of much more tension into the reconstructed MPFL than the patellar tendon increases a risk of postoperative extension lag and quadriceps weakness after MPFL reconstruction for patella alta [43]. MPFL reconstruction combined with distalization of the tibial tuberosity was recommended for the knee with the ISR more than 1.4 [2], whereas no clinical results have been demonstrated. Theoretically, distalization of the tibial tuberosity combined with Fulkerson procedure is available to normalize the patellar height and to correct the patellofemoral alignment and was recommended as a good long-lasting surgical solution with successful clinical results [10, 38, 44]. From the results of this study, it is suggested that isolated Fulkerson procedure should be avoided and combined distal transfer is recommended in cases of patella alta with ISR of 1.30 or more. Careful patient selection based on precise preoperative examinations could potentially improve the surgical outcomes by reducing the risk of postoperative patellar instability after Fulkerson procedure for recurrent patellar dislocation.
We note several limitations to our study. The muscular function to control the knee and hip joints plays an important role for stabilizing the patella [18, 27]; however, it was not examined. A lack of postoperative CT images made it difficult to analyze the effect of medialization distance on postoperative instability. The clinical evaluation at the final follow-up was performed by only 1 author, who did not have the detailed data of the preoperative radiologic measurements but could obtain the surgical information, and it potentially introduced a degree of bias.
Conclusion
In summary, the mid-term clinical study demonstrated that most patients with recurrent patellar dislocation gained successful knee function after Fulkerson procedure with or without lateral retinacular release. However, postoperative patellar instability was present in 11.3% of knees and statistically correlated with the magnitude of patella alta. The patient who is treated with Fulkerson procedure should be strictly selected based on the predisposing anatomic factors of patellar instability with a special focus on the patella height. Single application of Fulkerson procedure for recurrent patellar dislocation with severe patella alta increases the risk of postoperative patellar instability.
References
Akgün U, Nuran R, Karahan M (2010) Modified Fulkerson osteotomy in recurrent patellofemoral dislocations. Acta Orthop Traumatol Turc 44:27–35
Arendt EA (2009) MPFL reconstruction for PF instability: the soft (tissue) approach. Orthop Traumatol 95:S97–S100
Arendt EA (2010) MPFL reconstruction: the adductor sling approach. In: Zaffagnini S (ed) Patellofemoral pain, instability, and arthritis. Springer, Berlin, pp 175–179
Avikainen VJ, Nikku RK, Seppanen-Lehmonen TK (1993) Adductor magnus tenodesis for patellar dislocation: technique and preliminary results. Clin Orthop Relat Res 297:12–16
Barber FA, McGarry JE (2008) Elmslie-Trillat procedure for the treatment of recurrent patellar instability. Arthroscopy 24:77–81
Beck PR, Thomas AL, Farr J, Lewis PB, Cole BJ (2005) Trochlear contact pressures after anteromedialization of the tibial tubercle. Am J Sports Med 33:1710–1715
Biedert RM (2010) Trochlear lengthening osteotomy with or without elevation of the lateral trochlear facet. In: Zaffagnini S (ed) Patellofemoral pain, instability, and arthritis. Springer, Berlin, pp 209–215
Buuck DA, Fulkerson JP (2000) Anteromedialization of the tibial tubercle: a 4- to 12-year follow-up. Oper Tech Sports Med 8:131–137
Carofino BC, Fulkerson JP (2008) Anteromedialization of the tibial tubercle for patellofemoral arthritis in patients > 50 years. J Knee Surg 21:101–105
Caton JH, Dejour D (2010) Tibial tubercle osteotomy in patello-femoral instability and in patellar height abnormality. Int Orthop 34:305–309
Crosby EB, Insall J (1976) Recurrent dislocation of the patella: relation of treatment to osteoarthritis. J Bone Joint Surg Am 58:9–13
Dejour D, Le Coultre B (2007) Osteotomies in patello-femoral instabilities. Sports Med Arthrosc 15:39–46
Dejour H, Walch G, Nove-Josserand G, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2:19–26
Desio SM, Burks RT, Bachus KN (1998) Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med 26:59–65
Fairbank HA (1937) Internal derangement of the knee in children and adolescents. Proc R Soc Med 30:427–432
Fulkerson JP (1983) Anteromedialization of the tibial tuberosity for patellofemoral malalignment. Clin Orthop Relat Res 177:176–181
Fulkerson JP, Becker GJ, Meaney JA, Miranda M, Folcik MA (1990) Anteromedial tibial tubercle transfer without bone graft. Am J Sports Med 18:490–497
Goh JC, Lee PY, Bose K (1995) A cadaver study of the function of the oblique part of vastus medialis. J Bone Joint Surg Br 77:225–231
Hampson WGJ, Hill P (1975) Late results of transfer of the tibial tubercle for recurrent dislocation of the patella. J Bone Joint Surg Br 57:209–213
Hauser EDW (1983) Total tendon transplant for slipping patella: new operation for recurrent dislocation of the patella. Surg Gynecol Obstet 66:199–214
Hautamaa PV, Fithian DC, Kaufman KR, Daniel DM, Pohlmeyer AM (1998) Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res 349:174–182
Inoue M, Shino K, Nakata K, Maeda A, Nakagawa S, Toritsuka Y (1992) Analysis of initial onset of symptomatic patellar subluxation. Jpn J Orthop Sports Med 11:123–125
Insall J, Salvati E (1971) Patella position in the normal knee joint. Radiology 101:101–104
Iwano T, Kurosawa H, Tokuyama H, Hoshikawa Y (1990) Roentgenographic and clinical findings of patellofemoral osteoarthrosis: with special reference to its relationship to femorotibial osteoarthrosis and etiologic factors. Clin Orthop Relat Res 252:190–197
Kolowich PA, Paulos LE, Rosenberg TD, Farnsworth S (1990) Lateral release of the patella: indications and contraindications. Am J Sports Med 18:359–365
Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O (1993) Scoring of patellofemoral disorders. Arthroscopy 9:159–163
Lee TQ, Morris G, Csintalan RP (2003) The influence of tibial and femoral rotation on patellofemoral contact area and pressure. J Orthop Sports Phys Ther 33:686–693
Marcacci M, Zaffagnini S, Lo Presti M, Vascellari A, Iacono F, Russo A (2004) Treatment of chronic patellar dislocation with a modified Elmslie-Trillat procedure. Arch Orthop Trauma Surg 124:250–257
Merchant AC, Mercer RL, Jacobsen RH, Cool CR (1974) Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am 56:1391–1396
Mishra AK, Fanton GS, Dillingham MF, Carver TJ (1995) Patellar tendon graft harvesting using horizontal incisions for anterior cruciate ligament reconstruction. Arthroscopy 11:749–752
Monk AP, Beard DJ, Gill HS, Murray DW, Doll HA, Gibbons CL, Ostlere S (2011) The patho-anatomy of patellofemoral subluxation. J Bone Joint Surg Br 93:1341–1347
Mountney J, Senavongse W, Amis AA, Thomas NP (2005) Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg Br 87:36–40
Nakagawa K, Wada Y, Minamide M, Tsuchiya A, Moriya H (2002) Deterioration of long-term clinical results after the Elmslie-Trillat procedure for dislocation of the patella. J Bone Joint Surg Br 84:861–864
Nakamura N, Takeuchi R, Sawaguchi T, Ishikawa H, Saito T, Goldhahn S (2011) Cross-cultural adaptation and validation of the Japanese Knee Injury and Osteoarthritis Outcome Score (KOOS). J Orthop Sci 16:516–523
Naranja RJ Jr, Reilly PJ, Kuhlman JR, Haut E, Torg JS (1996) Long term evaluation of the Elmslie-Trillat-Maquet procedure for patellofemoral dysfunction. Am J Sports Med 24:779–784
Nomura E, Inoue M, Kobayashi S (2007) Long-term follow-up and knee osteoarthritis change after medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med 35:1851–1858
Panni AS, Cerciello S, Maffulli N, Di Cesare M, Servien E, Neyret P (2011) Patellar shape can be a predisposing factor in patellar instability. Knee Surg Sports Traumatol Arthrosc 19:663–670
Pritsch T, Haim A, Arbel R, Snir N, Shasha N, Dekel S (2007) Tailored tibial tubercle transfer for patellofemoral malalignment: analysis of clinical outcomes. Knee Surg Sports Traumatol Arthrosc 15:994–1002
Rillmann P, Dutly A, Kieser C, Berbig R (1998) Modified Elmslie-Trillat procedure for instability of the patella. Knee Surg Sports Traumatol Arthrosc 6:31–35
Sandmeier RH, Burks RT, Bachus KN, Billings A (2000) The effect of reconstruction of the medial patellofemoral ligament on patellar tracking. Am J Sports Med 28:345–349
Sasaki T, Ishibashi Y, Okamura Y, Toh S, Sasaki T (2002) MRI evaluation of growth plate closure rate and pattern in the normal knee joint. J Knee Surg 15:72–76
Tecklenburg K, Feller JA, Whitehead TS, Webster KE, Elzarka A (2010) Outcome of surgery for recurrent patellar dislocation based on the distance of the tibial tuberosity to the trochlear groove. J Bone Joint Surg Br 92:1376–1380
Thaunat M, Erasmus PJ (2007) The favorable anisometry: an original concept for medial patellofemoral ligament reconstruction. Knee 14:424–428
Tjoumakaris FP, Forsythe B, Bradley JP (2010) Patellofemoral instability in athletes: treatment via modified Fulkerson osteotomy and lateral release. Am J Sports Med 38:992–999
Trillat A, Dejour H, Couette A (1964) Diagnostic et traitement des subluxations r’ecidevantes de la rotule. Rev Chir Orthop 50:813–824
Acknowledgments
The authors thank Ryo Inoue, MD, Hirosaki University Graduate School of Medicine, for statistical analysis, and Yuka Kimura, MD, Hirosaki University Graduate School of Medicine, for data processing.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsuda, E., Ishibashi, Y., Yamamoto, Y. et al. Incidence and radiologic predictor of postoperative patellar instability after Fulkerson procedure of the tibial tuberosity for recurrent patellar dislocation. Knee Surg Sports Traumatol Arthrosc 20, 2062–2070 (2012). https://doi.org/10.1007/s00167-011-1832-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1832-2