Abstract
Purpose
The purpose of the present study was to compare the clinical and radiographic results after TKA using two prostheses with different sagittal patellofemoral design features, including outcomes related to compatibility of the patellofemoral joint.
Methods
The clinical and radiographic results of 81 patients (100 knees) who underwent TKA using the specific prosthesis (group A) were compared with those in a control group who underwent TKA using the other prosthesis (group B). The presence of anterior knee joint pain, patellar crepitation, and patellar clunk syndrome was also checked.
Results
The function score and maximum flexion angle at the last follow-up were slightly better in group A than those in group B (92.0 ± 2.3 vs. 90.6 ± 4.2) (133.6° ± 8.4° vs. 129.6° ± 11.4°). Anterior knee pain was observed in 6 knees and patellar crepitation in four knees in group A. In group B, these symptoms were observed in 22 knees and 18 knees, respectively. There was no patellar clunk syndrome in either group. The alignment was corrected with satisfactory positioning of components. The patellar height remained unchanged after TKA in the two groups. The differences between preoperative and postoperative patellar tilt angle and patellar translation were small.
Conclusion
When comparing the clinical and radiographic results after TKA using two prostheses with different sagittal patellofemoral design features, TKA using the specific prosthesis provided satisfactory results with less clinical symptoms related to the patellofemoral kinematics with TKA using the other prosthesis.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patellofemoral joint compatibility has important effects on clinical outcome and patient satisfaction after total knee arthroplasty (TKA) [31]. Incompatibility and instability of the patellofemoral joint cause various patellofemoral complications, including anterior knee joint pain, subluxation, dislocation, patellar crepitation, and patellar clunk syndrome [4]. The compatibility of the patellofemoral joint is influenced not only by factors related to the surgical technique, such as the position of the components, patellar height (Insall–Salvati ratio), and patellar tilt angle, but also by prosthesis factors, such as the geometry of the femoral component and the kinematic pattern of the prosthesis (femoral rollback) [9, 10, 30, 33].
The specific prosthesis (Vanguard, Biomet, Warsaw, IN) has newly modified design features incorporated into the sagittal profile of the femoral component. It is characterized by increased contact surface conformity of the femoral and patellar components. Major design features of the femoral component include a rounded sagittal profile and a deep, long, and wide trochlear groove [20, 21, 25]. This component design places the site of transition to intercondylar notch more posteriorly than previous designs, thus avoiding soft tissue impingement in deep knee flexion [34]. It is a relatively new TKA prosthesis introduced in 2003. Some studies have reported clinical and survival analyses of TKA with this prosthesis [20, 34, 35, 37], but only one study has reported the clinical and radiographic results related to compatibility of the patellofemoral joint [23]. We thought that there was rare previous report to compare the outcomes related to the compatibility of the patellofemoral joint after TKA using various prostheses with different sagittal patellofemoral design features with the same surgical technique.
Another prosthesis [Press Fit Condylar (PFC) Sigma, Johnson and Johnson Professional Inc., Raynham, MA] has an anatomical sagittal profile of the femoral component. It was designed with a deepened trochlear groove and an asymmetric epicondylar ridge, which allows the patellar component to have a maximized area of contact with the trochlear groove and therefore have reduced shear forces [3]. These characteristics contribute to improve patellar tracking. However, the incidence of anterior knee pain and patellar crepitation has been reported to be relatively higher than that of other prostheses [7, 18, 28]. Its distal aspect of the anterior flange is located at a more proximal position than recently designed TKA prostheses, which may be one of the reasons of its relatively higher incidence of patellofemoral complications [14, 17].
This study compared the clinical and radiographic results after a minimum 2-year follow-up after TKA using two prostheses with different sagittal patellofemoral design features, including outcomes related to the compatibility of the patellofemoral joint. It was hypothesized that the clinical and radiographic results of the one prosthesis would be comparable to or better than the other prosthesis, especially in regard of uncomfortable symptoms related to patellofemoral kinematics.
Materials and methods
All consecutive patients who had TKAs using the specific prosthesis (Vanguard) between 2006 and 2011 were included in the study group (group A) and were retrospectively reviewed. During this period, 112 arthroplasties in 93 patients were performed using this prosthesis. Five patients were lost to follow-up before 2 years, and 7 patients refused to participate in the present study, leaving 100 TKAs in 81 patients. For each patient reviewed, we matched a control patient from our patient database who had undergone primary TKA with the other prosthesis (PFC Sigma; group B) because we regarded its sagittal patellofemoral design features as less patellofemoral compatible than the former prosthesis [7, 28]. The senior surgeon has performed TKA with various designs of prostheses, and other prostheses had been used more frequently than the former prosthesis. The senior surgeon’s selection of specific type of implants was based on various considerations, including anatomical geometry and aspect ratio (ML/AP distance) of the distal femur. However, there was no selection bias in clinically important preoperative variables, such as severity of deformity or soft tissue imbalance. The matches were made according to age, gender, body mass index (BMI), diagnosis, preoperative range of motion (ROM), severity of preoperative deformity, and operation time. No significant difference was found in the demographics and preoperative clinical status between the two groups, except for patellar tilt angle (Table 1).
Surgical technique and rehabilitation
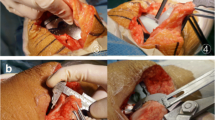
Medial parapatellar approach was used with a midline skin incision. Bone cuts were made with a measured resection, and a carefully planned soft tissue technique was used. Intramedullary guide was used for femoral resection, and the transepicondylar axis was used to position the anteroposterior femoral cutting guide system for femoral component rotation. Extramedullary guide was used for tibial resection. The reference line for tibia rotation was accurately aimed at a line passing through the medial third of the tibial tubercle and the second metatarsal or the middle of talus, which is practically 3–5 mm medial to the centre of the ankle. Any contracted medial or lateral soft tissue was carefully evaluated and selectively released where required as much as necessary. All patellae were resurfaced. Peripatellar denervation with electrocautery was performed. All implants were cemented onto cleaned, dried surfaces. The patellofemoral articulation was carefully evaluated with the no thumb technique. No lateral retinacular release was performed. There was no knee in which postoperative patellar subluxation occurred. Isometric exercises using the extensor and flexor muscles were initiated shortly after the operation. A Hemovac drain was inserted during surgery and was removed on the second postoperative day, followed by the initiation of active and assisted ROM exercise. Full weight-bearing ambulation was started at 4 days to the extent that the patient’s condition permitted.
Clinical and radiographic evaluation
The clinical scores had been recorded prospectively in our database and medical records, and they were collected by detailed retrospective reviews of database and medical records. The clinical and radiographic evaluations, except that for the signs of patellofemoral complications, were performed by independent orthopaedic surgeons. For clinical evaluation, the Knee Society knee score and function score were used to access pain and function, including ROM, at the preoperative and latest follow-up periods [19]. ROM was measured using a long-armed goniometer. The presence of anterior knee joint pain, patellar crepitation, patellar clunk syndrome, and any surgery-related complications was checked. Mobility of patella, patellofemoral instability, or patellar dislocation was also evaluated. The patients had been carefully evaluated by the senior author for signs of patellofemoral complications at every follow-up visit. The regular follow-up periods were postoperative 3 months, 6 months, 1 year, and annually thereafter.
Pre- and postoperative anteroposterior (AP), lateral, axial radiographs, and orthoroentgenograms (full-length standing AP radiographs) were obtained to assess limb alignment and component positioning. Measurements from these images were taken using a picture archiving and communication system (PACS). Pre- and postoperative mechanical axes were defined as the angle between femoral and tibial mechanical axes on orthoroentgenograms. Detailed analyses of the AP and lateral radiographs were conducted to determine α, β, γ, and δ angles, using the Knee Society radiological evaluation method [12]. Posterior femoral offset was measured on lateral radiographs as the perpendicular distance between the line extended from the posterior femoral cortex and the most posterior aspect of the femoral condyle (Fig. 1) [5]. Preoperative and postoperative patellar height was measured on lateral radiograph with Insall–Salvati ratio [36]. Joint line height was defined as the shortest distance between the fibular head and lateral femoral condyle on AP radiograph (Fig. 2) [1]. Preoperative and postoperative patellar tilt angles were measured in Merchant’s view, taken with the knee joint flexed at 45° (Fig. 3). A positive value indicated opening towards the medial side of patella. Preoperative and postoperative patellar translations were also measured in Merchant’s view (Fig. 3). A positive value indicated lateral translation of patella, compared to the femoral trochlea or sulcus of the femoral component. Incompatibility of the patellofemoral joint was defined as a malposition of the patella when the patellar tilt angle was more than ±10° or the patellar translation was more than ±5 mm. Because there has been no definition of radiographic incompatibility of the patellofemoral joint after TKA, the cut-off value of ±10° and ±5 mm was theoretically selected, with consideration on the measurement accuracy on axial view radiographs.
Measuring methods of patellar tilt angle (°) and translation (mm). a The preoperative patellar tilt angle is defined as the angle subtended by the equatorial line of the patella and the line connecting the anterior limits of the femoral condyles on Merchant’s view. The preoperative patellar translation is defined as the distance (c) to the median ridge of the patella, which is the deepest point of the patella in relation to the equatorial line of the patella, from the femoral trochlea. b The postoperative patellar tilt angle is defined as the angle subtended by the equatorial line of the patella and the line connecting the anterior limits of the femoral component. The postoperative patellar translation is defined as the distance (c) between the centre of the patella prosthesis and a line drawn through the central intercondylar sulcus of the femoral component
The study was approved by the institutional review board of Kyung Hee University Medical Center (KHUHMDIRB 0901-01). Informed consents of all patients were obtained before the review.
Statistical analysis
To minimize any observation bias, two independent investigators repetitively performed all radiographic measurements with an interval of 2 weeks, and average values were used for analysis. The intra- and interobserver reliabilities of all measurements were assessed using the intraclass correlation coefficient. In this study, intraclass correlation coefficient values of all measurements were greater than 0.8 for both intra- and interobserver reliabilities.
Clinical and radiographic results before operation and at the last follow-up visit were compared between the two groups (student’s t test). Preoperative clinical and radiographic results were compared to postoperative results (paired t test). The patellofemoral complication rate was compared between the two groups (Chi-square test). Statistical analyses were performed using SPSS version 18.0 (Chicago, IL), and p values <0.05 were considered statistically significant.
Results
Most postoperative clinical scores did not differ between the two groups. However, postoperative function score at last follow-up was slightly better in group A than that in group B (Table 2). Postoperative maximum flexion angle at last follow-up in group A was greater than that in group B (Table 2). Anterior knee pain was observed in six knees in group A and 22 knees in group B (p = 0.001; Table 2). Patellar crepitation was observed in four knees in group A and 18 knees in group B (p = 0.002; Table 2). However, there was no patellar clunk syndrome in either group. There was no patellofemoral instability or dislocation. There was one complication in group A, in which the polyethylene insert locking bar had been disengaged and required re-fixation of the polyethylene insert.
Regarding radiographic results, the postoperative mechanical axis did not differ significantly between the two groups (Table 3). The mean α, β, and γ angle did not differ between the two groups at the last follow-up. However, the δ angle was significantly larger in group B (Table 3). The joint line height and patellar height of Insall–Salvati ratio remained unchanged after TKA in the two groups. The preoperative and postoperative patellar tilt angles were significantly different between the two groups (Table 3). The change from baseline of the patellar tilt angle was 3.8° ± 4.9° in group A and −3.0° ± 5.2° in group B. There was no incompatibility of the patellofemoral joint in group A, in which the patellar tilt angle would be more than ±10° or the patellar translation more than ± 5 mm. In group B, there was no knee with patellar tilt angle more than ±10°. There were seven knees in which the patellar translation was more than ± 5 mm.
Discussion
The most notable finding of the present study was that the incidence of patellofemoral complications was significantly lower in patients with the one prosthesis (Vanguard) compared to patients with the other (PFC Sigma) prosthesis. Patellofemoral complications after TKA are well known, with a reported incidence of 0–25 % with a variety of TKA designs [16, 31, 32]. Several old prostheses were thought to have increased patellofemoral complications, and those design characteristics included femoral box designs with larger intercondylar box ratio, proximally positioned or wide notch box, and sharp transition into the intercondylar notch box [26, 27, 39]. The evolution of prosthesis design and surgical technique has been decreasing its incidence after TKA. However, patellar crepitus or clunk is still being reported with a few recently developed prostheses, ranging from 10 to 17 % [7, 13, 14]. To our knowledge, no report has focused on patellofemoral complications after TKA using the Vanguard® Complete Knee System, although it was innovated to be a patella-friendly design. It has a femoral component with a rounded sagittal profile and a lower anterior flange to improve the compatibility of the patellofemoral joint [24]. It may be more forgiving to the retinaculum due to the absence of over-tensioning of soft tissues. Its trochlear groove is also longer and deeper to better guide the patella and the quadriceps tendon during deep flexion.
Appropriate patellofemoral tracking is important in order to decrease anterior knee joint pain. Patellofemoral tracking after TKA and the incidence of anterior knee pain may be influenced not only by factors related to the surgical technique, but also by factors related to prosthesis designs [9, 11]. In the present study, pain was observed only in six knees among patients of group A and the incidence was quite low when it was compared to that of 22 knees among patients of group B or to previous studies (Table 4) [2, 6, 28, 38, 40]. It is ascribed to the use of the prosthesis with good patellofemoral joint compatibility and optimal positioning of the prosthesis.
Patellar crepitation is another patellofemoral complication with a wide range of incidence [7, 11, 32]. The major reason behind the wide range is thought to be the variety in the severity of symptom that counts into incidence. Several studies included only disabled patients with patellar crepitus painful enough to require surgical intervention [7, 11]. In the present study, we had four patients with patellar crepitus among patients of group A, which were not symptomatic enough to require arthroscopic debridement. Therefore, we thought that the rate of 4 % of patellar crepitation was low compared to previous studies [7, 11, 14, 28]. Peralta–Molero et al. [32] demonstrated that patients with a higher postoperative flexion angle are at increased risk of developing patellofemoral complications. They postulated that the patella articulates with the femur in a more distal and posterior position at higher flexion angles, which allows the soft tissues at the proximal patellar pole to engage the intercondylar notch, contributing to formation of inflammatory, hypertrophic tissue, and development of patellar crepitation. In the present study, the incidence of patellar crepitation in patients of group A was lower despite the higher postoperative flexion angle of 133.6° ± 8.4° compared to patients of group B, who had 18 % of patellar crepitation with postoperative flexion angle of 129.6° ± 11.4°.
It has been suggested that patella baja, excessive patellar tilt, and anterior placement of the tibial component contribute to patellar crepitation [4, 16, 39]. The risk of patellar crepitation increased when the joint height increased by more than 8 mm [16, 39]. In the present study, the patellar height of Insall–Salvati ratio remained unchanged after TKA. No knee had patellofemoral joint incompatibility, in which the patellar tilt angle would be more than ±10° or the patellar translation more than ±5 mm. It is believed that the newly modified design features in Vanguard® prosthesis help to minimize patellar crepitation with meticulous clearing of the soft tissue around the patella and careful restoration of the compatibility of the patellofemoral articulation, patellar position, and patellar thickness.
Patellar clunk syndrome is a rare complication with currently used prostheses. It was related to the sharp structure of the femoral groove and the relatively high femoral intercondylar AP length of the old prostheses [14–16, 26, 39]. Recently, it was reported that patellar clunk syndrome occurred in 13.3 % of 93 patients who received the PFC® Sigma RP prosthesis (DePuy, Johnson and Johnson, Professional, MA) [14]. They regarded the prosthesis design as a major aetiologic factor causing patellar clunk and suggested that the larger intercondylar box ratio of the PFC RP may be one of the reasons for the higher incidence of patellar clunk. Schroer et al. [34]. reported 0.4 % of patellar clunk syndrome when the Vanguard® prosthesis was used with the mini-subvastus approach. No patellar clunk syndrome was seen in our series when TKA was performed using the same prosthesis with conventional medial parapatellar approach. The low incidence of patellar clunk syndrome did not seem to be the result of surgical approach when using this prosthesis.
Patellofemoral complications can cause poor clinical outcomes and may result in revision surgery. It is highly dependent on the design and the position of the femoral component [13, 18]. There is a wide variation in the design features of current TKA prostheses, in such aspects as rotation alignment, trochlear geometry, intercondylar box ratio, sagittal radius of the femoral component, and tibiofemoral kinematic pattern [10, 29]. In particular, surgeons should make efforts to minimize patellofemoral complications in patients who have preoperative risk factors for patellofemoral complications, such as poor preoperative patellar tracking, dysplastic trochlea, or malrotation of the distal femur [8, 17]. The prosthesis with patellofemoral compatible design features, which was used in the present study, can provide an optimal option for the surgeon’s prosthesis selection.
This study has limitations in its retrospective design and the relatively short follow-up. Prospective studies will be necessary to justify the advantages of the prosthesis with patellofemoral compatible design features. We think that a longer-term follow-up evaluation, including survivorship analysis related to patellofemoral complications, is necessary. Another limitation was the difference in preoperative patellar tilt angle between the two groups. Although patellar tilt angle alone may not directly influence the incidence of patellofemoral complication, demographics with similar patellar tilt angle will be necessary for a prospective comparative study. The last limitation was that most patients in the present study were females with low BMI. Such gender distribution of osteoarthritis and low BMI are common findings in the Korean ethnic group [22]. The differences need to be considered to extrapolate our findings to other populations.
However, the strengths of this study include prospective collection of data and accurate radiographic measurement. All data were collected prospectively in a clinical database, although the data review was done retrospectively. The radiographic measurements from high-quality images using a PACS could qualify the evaluation of patellofemoral articulation such as the patellar height, patellar tilt angle, and patellar translation.
Conclusion
TKA using the Vanguard® prosthesis provided satisfactory results with less clinical symptoms related to the compatibility of the patellofemoral joint, compared to TKA using the PFC sigma® prosthesis. The theoretical advantages of patellofemoral compatible design features incorporated into the sagittal profile of the femoral component were demonstrated clinically.
References
Bae DK, Song SJ, Yoon KH (2010) Total knee arthroplasty following closed wedge high tibial osteotomy. Int Orthop 34:283–287
Baliga S, McNair CJ, Barnett KJ, MacLeod J, Humphry RW, Finlayson D (2012) Does circumpatellar electrocautery improve the outcome after total knee replacement? A prospective, randomised, blinded controlled trial. J Bone Joint Surg Br 94:1228–1233
Ballantyne A, McKinley J, Brenkel I (2003) Comparison of the lateral release rates in the press fit condylar prosthesis and the PFC Sigma prosthesis. Knee 10:193–198
Beight JL, Yao B, Hozack WJ, Hearn SL, Booth RE Jr (1994) The patellar “clunk” syndrome after posterior stabilized total knee arthroplasty. Clin Orthop Relat Res 299:139–142
Bellemans J, Banks S, Victor J, Vandenneucker H, Moemans A (2002) Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty. Influence of posterior condylar offset. J Bone Joint Surg Br 84:50–53
Breugem SJ, van Ooij B, Haverkamp D, Sierevelt IN, van Dijk CN (2014) No difference in anterior knee pain between a fixed and a mobile posterior stabilized total knee arthroplasty after 7.9 years. Knee Surg Sports Traumatol Arthrosc 22:509–516
Choi WC, Ryu KJ, Lee S, Seong SC, Lee MC (2013) Painful patellar clunk or crepitation of contemporary knee prostheses. Clin Orthop Relat Res 471:1512–1522
Conrad DN, Dennis DA (2014) Patellofemoral crepitus after total knee arthroplasty: etiology and preventive measures. Clin Orthop Surg 6:9–19
D’Lima DD, Chen PC, Kester MA, Colwell CW (2003) Impact of patellofemoral design on patellofemoral forces and polyethylene stresses. J Bone Joint Surg Am 85-A(Suppl 4):85–93
Dejour D, Ntagiopoulos PG, Saffarini M (2014) Evidence of trochlear dysplasia in femoral component designs. Knee Surg Sports Traumatol Arthrosc 22:2599–2607
Dennis DA, Kim RH, Johnson DR, Springer BD, Fehring TK, Sharma A (2011) The John Insall Award: control-matched evaluation of painful patellar Crepitus after total knee arthroplasty. Clin Orthop Relat Res 469:10–17
Ewald FC (1989) The knee society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 248:9–12
Frye BM, Floyd MW, Pham DC, Feldman JJ, Hamlin BR (2012) Effect of femoral component design on patellofemoral crepitance and patella clunk syndrome after posterior-stabilized total knee arthroplasty. J Arthroplasty 27:1166–1170
Fukunaga K, Kobayashi A, Minoda Y, Iwaki H, Hashimoto Y, Takaoka K (2009) The incidence of the patellar clunk syndrome in a recently designed mobile-bearing posteriorly stabilised total knee replacement. J Bone Joint Surg Br 91:463–468
Heyse TJ, le Chong R, Davis J, Haas SB, Figgie MP, Potter HG (2012) MRI diagnosis of patellar clunk syndrome following total knee arthroplasty. HSS J 8:92–95
Hozack WJ, Rothman RH, Booth RE Jr, Balderston RA (1989) The patellar clunk syndrome. A complication of posterior stabilized total knee arthroplasty. Clin Orthop Relat Res 241:203–208
Indelli PF, Marcucci M, Cariello D, Poli P, Innocenti M (2012) Contemporary femoral designs in total knee arthroplasty: effects on the patello-femoral congruence. Int Orthop 36:1167–1173
Indelli PF, Marcucci M, Pipino G, Charlton S, Carulli C, Innocenti M (2014) The effects of femoral component design on the patello-femoral joint in a PS total knee arthroplasty. Arch Orthop Trauma Surg 134:59–64
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Kievit AJ, Schafroth MU, Blankevoort L, Sierevelt IN, van Dijk CN, van Geenen RC (2014) Early experience with the vanguard complete total knee system: 2–7 years of follow-up and risk factors for revision. J Arthroplasty 29:348–354
Kim JH, Lee S, Ko DO, Yoo CW, Chun TH, Lee JS (2011) The analysis of risk factors in no thumb test in total knee arthroplasty. Clin Orthop Surg 3:274–278
Koh IJ, Kim TK, Chang CB, Cho HJ, In Y (2013) Trends in use of total knee arthroplasty in Korea from 2001 to 2010. Clin Orthop Relat Res 471:1441–1450
Kong CG, Park SW, Yang H, In Y (2014) The effect of femoral component design on patellar tracking in total knee arthroplasty: genesis II prosthesis versus vanguard prosthesis. Arch Orthop Trauma Surg 134:571–576
Koninckx A, Deltour A, Thienpont E (2014) Femoral sizing in total knee arthroplasty is rotation dependant. Knee Surg Sports Traumatol Arthrosc 22:2941–2946
Lombardi AV Jr, Ellison BS, Berend KR (2008) Polyethylene wear is influenced by manufacturing technique in modular TKA. Clin Orthop Relat Res 466:2798–2805
Lonner JH, Jasko JG, Bezwada HP, Nazarian DG, Booth RE Jr (2007) Incidence of patellar clunk with a modern posterior-stabilized knee design. Am J Orthop (Belle Mead NJ) 36:550–553
Maloney WJ, Schmidt R, Sculco TP (2003) Femoral component design and patellar clunk syndrome. Clin Orthop Relat Res 410:199–202
Meftah M, Jhurani A, Bhat JA, Ranawat AS, Ranawat CS (2012) The effect of patellar replacement technique on patellofemoral complications and anterior knee pain. J Arthroplasty 27:1075–1080
Mugnai R, Digennaro V, Ensini A, Leardini A, Catani F (2014) Can TKA design affect the clinical outcome? Comparison between two guided-motion systems. Knee Surg Sports Traumatol Arthrosc 22:581–589
Ogawa H, Matsumoto K, Akiyama H (2016) Effect of patellar resurfacing on patellofemoral crepitus in posterior-stabilized total knee arthroplasty. J Arthroplasty. doi:10.1016/j.arth.2016.01.023
Parker DA, Dunbar MJ, Rorabeck CH (2003) Extensor mechanism failure associated with total knee arthroplasty: prevention and management. J Am Acad Orthop Surg 11:238–247
Peralta-Molero JV, Gladnick BP, Lee YY, Ferrer AV, Lyman S, Gonzalez Della Valle A (2014) Patellofemoral crepitation and clunk following modern, fixed-bearing total knee arthroplasty. J Arthroplasty 29:535–540
Saffarini M, Demey G, Nover L, Dejour D (2016) Evolution of trochlear compartment geometry in total knee arthroplasty. Ann Transl Med 4:7
Schroer WC, Diesfeld PJ, Reedy ME, LeMarr A (2009) Association of increased knee flexion and patella clunk syndrome after mini-subvastus total knee arthroplasty. J Arthroplasty 24:281–287
Schroer WC, Stormont DM, Pietrzak WS (2014) Seven-year survivorship and functional outcomes of the high-flexion vanguard complete knee system. J Arthroplasty 29:61–65
Scuderi GR, Windsor RE, Insall JN (1989) Observations on patellar height after proximal tibial osteotomy. J Bone Joint Surg Am 71:245–248
Tsukamoto R, Williams PA, Shoji H, Hirakawa K, Yamamoto K, Tsukamoto M, Clarke IC (2008) Wear in molded tibial inserts: knee simulator study of H1900 and GUR1050 polyethylenes. J Biomed Mater Res B Appl Biomater 85:314–319
van Jonbergen HP, Scholtes VA, van Kampen A, Poolman RW (2011) A randomised, controlled trial of circumpatellar electrocautery in total knee replacement without patellar resurfacing. J Bone Joint Surg Br 93(8):1054–1059. doi:10.1302/0301-620X.93B8.26560
Yau WP, Wong JW, Chiu KY, Ng TP, Tang WM (2003) Patellar clunk syndrome after posterior stabilized total knee arthroplasty. J Arthroplasty 18:1023–1028
Zha GC, Sun JY, Dong SJ (2014) Less anterior knee pain with a routine lateral release in total knee arthroplasty without patellar resurfacing: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc 22:517–525
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bae, D.K., Baek, J.H., Yoon, K.T. et al. Comparison of patellofemoral outcomes after TKA using two prostheses with different patellofemoral design features. Knee Surg Sports Traumatol Arthrosc 25, 3747–3754 (2017). https://doi.org/10.1007/s00167-016-4264-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4264-1