Abstract
Purpose
Anterior knee pain is a major cause of complaint in total knee arthroplasty (TKA) without patellar resurfacing. The concept of improved patellar tracking and decreased retropatellar contact pressure for lateral retinacular release theoretically suggests that patients with lateral retinacular release in TKA would achieve a lower incidence of anterior knee pain when compared without lateral retinacular release. We sought to determine (1) whether those patients who received a routine lateral retinacular release in TKA would attain lower incidence of anterior knee pain as compared to patients who received TKA without lateral retinacular release and (2) whether lateral retinacular release would increase the lateral retinacular release-related complications.
Methods
A total of 148 patients who underwent TKA with the use of the Gemini MK II mobile bearing were randomized to receive either routine lateral retinacular release (intervention group) or not (control group). Patients were assessed by the visual analogue scale for anterior knee pain, the Knee Society clinical scoring system of knee score and function score, and patellar score for clinical function. Patients’ satisfaction and lateral retinacular release-related complications were also evaluated.
Results
The overall incidence of anterior knee pain in the intervention group at 18 months follow-up was 5.6 %, while that of the control group was 20.6 % (p = 0.009). No statistical difference was detected between the two groups in terms of lateral retinacular release-related complications (n.s.), patients’ satisfaction (n.s.), knee score (n.s.), function score (n.s.), and patellar score (n.s.) at 18 months follow-up.
Conclusion
The present study suggests that routine lateral retinacular release can reduce anterior knee pain and does not increase lateral retinacular release-related complications, in TKA with the use of the Gemini MK II mobile bearing without patellar resurfacing.
Level of evidence
Therapeutic, Level I.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior knee pain has been documented to be reduced with the improved surgical technique and the prosthesis design in contemporary total knee arthroplasties, no matter whether the patella is resurfaced or not [15]. The option of patellar non-resurfacing is advantageous in reducing patellar-related complications (such as loosening and fracture) and in preserving bone stocks for future revision surgeries. However, the high incidence of anterior knee pain, which is reported to be 6.1–38 % for the patients having underwent the primary total knee arthroplasty (TKA) [2, 13, 17, 35], has been a hassling problem in TKA without patellar resurfacing.
Lateral retinacular release can succeed in improving patellar tracking and in decreasing the retropatellar contact pressure [16, 20, 27, 30, 40]. Therefore, in theory, lateral retinacular release could reduce postoperative anterior knee pain because the two factors of patellar maltracking and increased patellofemoral contact pressure have been reported to be related with anterior knee pain [22, 38]. However, there is a lack of study to probe into whether routine performance of intraoperative lateral retinacular release is beneficial for the patients with TKA, because some authors believe that lateral retinacular release is associated with increased lateral retinacular release-related complications (haematoma, wound complications, lateral knee pain, patellar fracture, and patellar osteonecrosis) [5, 34].
Accordingly, the present prospective randomized controlled double-blind (both patient and clinical evaluator blinded) study aims at exploring: (1) whether the patients who received routine lateral retinacular release in TKA without patellar resurfacing would attain lower incidence of anterior knee pain as compared with patients who received TKA without lateral retinacular release and (2) whether lateral retinacular release would increase the lateral retinacular release-related complications. We hypothesized that lateral retinacular release may be a safe, simple, and efficient surgical procedure to reduce the incidence of anterior knee pain in TKA without patellar resurfacing.
Materials and methods
The criteria for inclusion included: (1) a diagnosis of primary degenerative osteoarthritis and (2) surgery on just one side; the criteria for exclusion included: (1) patients with mental disorder or mental illness, (2) severe contralateral knee osteoarthritis, (3) total hip arthroplasty (THA), contralateral TKA, or periprosthetic fractures in the period of study, (4) patients with symptomatic arthritis in back, hip, contralateral knee, and feet, (5) a history of patella fracture, high tibial or distal femoral osteotomy, THA and TKA, and (6) fixed varus, or valgus deformity of >15°.
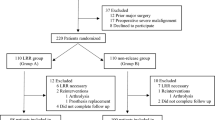
This trial began recruiting participants in January 2010 and closed enrolment in January 2012. During this period, 201 patients were eligible for assessment, and 53 were excluded before randomization. There remained 148 (54 males and 94 females) patients with a mean age of 68.5 ± 7.8 years (range, 51–85 years) and a mean weight of 62.7 ± 4.3 kg (range, 53–76 kg).
Method of randomization
In the operating room, all of the 148 patients with general anaesthesia were assigned to receive routine lateral retinacular release (intervention group) or non-lateral retinacular release (control group) in the computer-generated randomization sequence, which were placed in an opaque envelope; in order to protect the integrity of the randomization scheme, an independent biostatistician ensured that the block sizes were confidential. But some patients would be excluded from the control group when a lateral retinacular release must be performed by virtue of intraoperative patellar maltracking (Fig. 1).
Surgical procedure
All surgeries were performed by the senior surgeon (JYS) with the use of the Gemini MK II (Link, Germany) mobile-bearing TKA without patellar resurfacing. The patients were operated on under general anaesthesia and with tourniquet control. A midline skin incision and a medial arthrotomy were used to expose the knee, with resection of the infrapatellar fat pad. The distal femoral and the proximal tibial resection was performed, under the intramedullary and extramedullary alignment guidance, respectively. Careful attention was given to the 6° distal femoral valgus and 3° external rotation relative to the posterior condyles to establish the appropriate femoral rotation. Proximal tibial preparation was performed using the anatomical AP axis of the tibia to establish the tibial rotation [1]. When symmetric balance of the flexion–extension gaps is obtained, both the tibial and femoral components are cemented. All patients underwent circumpatellar electrocautery and patelloplasty. If osteotomy surfaces were not covered by the prosthesis, they were sealed with bone wax to control the bleeding. We did not use a wound drain following surgery. The tourniquet was released when the wound was closed and bandaged.
Regardless of the patellofemoral tracking in the intervention group, a lateral retinacular release at least 2 cm lateral to the border of the patella was routinely performed with using the inside-out technique while preserving the superior lateral geniculate artery. The lateral retinacular release extended from the inferior third of the tendon of vastus lateralis to the level of the distal pole of the patella. In contrast, an intraoperative assessment of patellar tracking was performed in the control group, according to ‘no thumb’ test [10]. If tracking was inadequate (appropriate patellar tracking which was defined as a patella that remained full contact with the femoral component trochlear groove medially and laterally through 90° of flexion with no tendency of tilt or subluxation), a lateral retinacular release was performed with the same technique. Four knees (5.4 %) in the control group required lateral retinacular release and were excluded in this study.
Perioperative regimen
All patients were managed with the same perioperative regimen. Antibiotic prophylaxis with a first-generation cephalosporin was used preoperatively and during the first 24 h postoperatively. Intraarticular multimodal analgesic injection [7] was used for the control over postoperative pain. Low molecular weight heparin was administered routinely for the thromboembolic prophylaxis. The day after the surgery, patients were encouraged to begin progressive weight bearing and active knee range of motion, quadriceps and hamstrings strengthening. Patients could discharge after 5 days if the wound was dry, and they were able to walk with a walker, ascend several stairs, and actively flex the affected knee to 90°. After discharge, patients were traced by telephone, letter, or e-mail and were asked to return for completing the clinical and radiological postoperative evaluation at 6 weeks, 6 months, 1 year, and annually thereafter.
Clinical evaluation
Intraoperative degree of chondromalacia of the patella was assessed by the senior author (JYS), according to the Outerbridge grading system [28]. Preoperative and postoperative clinical data were evaluated by the independent surgeon (JXT) who was blind to the patient’s randomization.
Preoperative and postoperative clinical outcome was assessed with the Knee Society clinical scoring system of knee score (0–100 points) and function score (0–100 points) [18], and the patellar score [12]. And the assessment of anterior knee pain was implemented with visual analogue scale (VAS) with a range of 0–10 points. The cutoff value for the presence of anterior knee pain was >0 points. The VAS was graded into none (0 points), mild (0–2 points), moderate (3–4 points), and severe (5–10 points). Patients were also asked whether they were satisfied with the outcomes achieved after TKA, with the following answers to choose: ‘very satisfied’, ‘satisfied’, ‘unsure’, or ‘dissatisfied’. These data were also evaluated, including lateral retinacular release-related complications, operating time, and the length of hospital stay.
Radiographic evaluation
Radiographic evaluation was carried out by another blinded, independent surgeon (SKZ). Preoperative and postoperative radiographs of the knee were assessed with standing anteroposterior, lateral, Merchant views. Radiographic evaluation was performed according to the Knee Society Radiological Evaluation System [11]. Patellar positions (including neutral tracking, tilt and displacement) were measured from Merchant views, according to the technique of Gomes et al. [14]. Patellar maltracking was defined as patellar tilt of >5° or displacement >5 mm [3]. The shape of the patella [37], the degree of the patellofemoral osteoarthritis [19], the sulcus angle, and the congruence angle were also evaluated.
Follow-up
In order to compare the results in the two groups, all patients were assessed at the same time point that was set 18 months after surgery. At the 18 months follow-up, three patients (two in the intervention group and one in the control group) had been dead for reasons irrelevant to the surgery; one patient in the intervention group was lost in the follow-up period and one patient in the control group sustained a trauma result in periprosthetic fracture at the distal femur and was treated by open reduction and internal fixation. These five patients were excluded. And there remained 139 patients (seventy-one in the intervention group and sixty-eight in the control group) available for analysis (Fig. 1). Detailed distribution of the 139 patients’ demographics and characteristics is shown in Table 1. The study was approved by the Ethics Committee of the First Affiliated Hospital of Soochow University (ID number 09-498), and informed consent was obtained from all patients.
Statistical analysis
STATA version 11.0 for Windows (StataCorp LP, College Station TX) was used for statistical analysis. Randomization sequence was generated by STATA. The clinical outcomes (anterior knee pain, knee score, patellar score, and patients’ satisfaction) and patellar position at postoperative 18 months were analysed for this study. All analysis was based on intention of treatment, that is, all patients were analysed according to their allocation at randomization. The continuous data of the two groups of patients were analysed with a two-tailed, unpaired t test. If continuous data were unable to meet the assumption of normal distribution, Mann–Whitney U test was selected. Chi-square analysis was used to test for statistically significant differences in the frequencies of findings between two groups. Fischer’s exact test was performed for the comparison of categorical data when the expected theoretical figures were lower than 5. Two-sided p value <0.05 was considered to be significant.
Results
The preoperative clinical data and intraoperative degree of chondromalacia of patella, mean operating time, and the length of hospital stay were not significantly different between the two groups (Tables 1, 2). All patients in both groups did not receive a transfusion. No revisions or re-operations were performed.
Anterior knee pain
Less anterior knee pain in patients with lateral retinacular release (4 of 71, 5.6 %) than without lateral retinacular release (14 of 68, 20.6 %) (p = 0.009) at follow-up at 18 months (Table 3).
Knee Society clinical scoring system and patellar score
The mean postoperative knee score, function score, and patellar score improved significantly (p < 0.05) in both groups (Table 4). There was no significant statistical difference in mean postoperative knee score (n.s.), function score (n.s.), or patellar score (n.s.) between the both groups at follow-up at 18 months (Table 4).
Patients’ satisfaction
Patients were questioned whether they were satisfied with the outcomes, which were achieved after TKA at follow-up at 18 months. On the whole, 82.0 % (114 of 139) of patients were very satisfied or satisfied with their TKA. There existed no difference in the patients’ satisfaction between the two groups (n.s.) (Table 3). However, patients with anterior knee pain often were dissatisfied. For example, 4 of 4 (100 %) patients with anterior knee pain in intervention group were dissatisfied and 10 of 14 (71.4 %) in control group were dissatisfied; these patients with anterior knee pain expressed a significantly higher dissatisfaction with the outcomes of TKA when compared to patients without anterior knee pain [2.5 % (3 out of 121) vs. 77.8 % (14 out of 18)] (p = 0.000).
Radiographic examination
Knee Society Radiological Evaluation System
Proper implant alignment was observed in both groups at 18 months follow-up (Table 3). No radiolucent lines at the bone–implant interface were seen around the tibial components and femoral components in both groups. Osteolysis around the tibial components and femoral components was also not observed.
Patellar position
Preoperative 35 patients with patellae tracked centrally in the intervention group, and no patellar malposition was observed in patients at follow-up at 18 months. Among preoperative 36 patients with patellar malposition in the intervention group, 22 patellae were corrected and 14 maintained. Among preoperative 39 patellae tracked centrally in the control group, 7 patients were observed patellar malposition at follow-up at 18 months. Among preoperative 29 patients with patellar malposition in the control group, 11 patellae were corrected and 18 maintained. The incidence of patellar malposition in the patients with routine lateral retinacular release was lower than those without lateral retinacular release [19.7 % (14 of 71) vs. 36.8 % (25 of 68), p = 0.025] (Table 3). However, no statistical difference was detected between the two groups in terms of patellar maltracking (3 out of 71 vs. 5 out of 68) (n.s.) (Table 3). In addition, there was a significant difference in incidence of anterior knee pain of patients with patellar malposition between two groups [14.3 % (2 out of 14 patients) vs. 48.0 % (12 out of 25 patients)] (p = 0.044). Medial subluxation or tilt of the patella was not observed in both groups.
Lateral retinacular release-related complications
Five knees showed signs of haematoma in 3 days of TKA, but these haematomas were small and could be resorbed without a surgical evacuation. Wound complications occurred on six patients (Table 2), and only those required to limit early range of motion or walking, local wound care, and/or oral antibiotics. No patients experienced lateral knee pain in both groups. Patellar fracture and patellar osteonecrosis were not observed in any of the patients. We did not find the difference in incidence of lateral retinacular release-related complications (n.s.) (Table 2).
Discussion
The most important finding of the present study was that (1) routine lateral retinacular release gives a significantly lower incidence of anterior knee pain at 18 months postoperatively compared with no lateral retinacular release (p = 0.009); (2) patients with routine lateral retinacular release can achieve a lower incidence of patellar malposition when compared to those without lateral retinacular release (p = 0.025); (3) patients with routine lateral retinacular release do not have increased lateral retinacular release-related complications compared to those without lateral retinacular release (n.s.); (4) the majority of patients (77.8 %) with anterior knee pain who expressed their dissatisfaction with the outcomes after TKA. Currently, with the improvement in surgical technique and prosthesis design, the incidence of anterior knee pain was still high. A recent meta-analysis of 7 studies showed that a total of 26.8 % of patients who underwent TKA without patellar resurfacing experienced postoperative anterior knee pain [13]. The causes of anterior knee pain remain unclear, a secondary patellar resurfacing in the treatment for the pain, only 44–62 % of patients referring subjective improvement [25]. Therefore, for patients who did not undergo lateral retinacular release during the previous TKA, an arthroscopy-guided lateral retinacular release may be a good choice in relieving the anterior knee pain, according to this study. In addition, in recent years, emphasis on minimal invasive TKA may increase the incidence of component malpositioning which is likely to result in high rate of postoperative anterior knee pain. In such situations, routine lateral retinacular release may be considered to decrease anterior knee pain and may be beneficial for patients. Therefore, the investigation of the influence of lateral retinacular release on clinical results is currently pertinent.
In this study, the incidence of anterior knee pain at 18 months postoperatively in the patients with routine lateral retinacular release was significantly lower than those without lateral retinacular release (5.6 vs. 20.6 %, p = 0.009); as well as when patients with patellar malposition, patients with routine lateral retinacular release can achieve a lower incidence of anterior knee pain compared with those without lateral retinacular release (14.4 vs. 48.0 %). It may be attributed to the two important factors of the improved patellar tracking and decreased patellofemoral contact pressure in patients with lateral retinacular release [16, 20, 27, 30, 40], both of which has been reported to be closely related with anterior knee pain [22, 32, 38]. Wilson et al. [38] found differences in the patellar kinematics between patients with and those without anterior knee pain, as well as an abnormal patellar tracking in patients with anterior knee pain. In Lee et al. [22] in a prospective cohort study of 271 patients, it was found that patients with patellar decompression can reduce anterior knee pain following TKA without patellar resurfacing when compared to those without patellar decompression. In addition, Leichtle et al. [23] reported a significant increase in patellofemoral contact pressure after TKA even without a patellar maltracking. Therefore, a routine lateral retinacular release may create the potential ability to offset the pressure change following TKA and, as a result, to achieve a low incidence of anterior knee pain.
In this study, patients with routine lateral retinacular release can achieve a lower incidence of patellar malposition at follow-up at 18 months compared with those without lateral retinacular release (19.7 vs. 36.8 %). Several literature reported that lateral retinacular release should be selectively performed according to the ‘no thumb’ or towel clip test [4, 8]. But the present study has shown that if the performance of lateral retinacular release according to the above-mentioned tests (‘no thumb’ test) could not always prevent the patellar malposition effectively, the test was not under muscle tone and postoperative function was dynamic. The findings echo those of Yang et al. [39] and Engh et al. [9] wherein the patients without lateral retinacular release had a higher patellar tilt than those with lateral retinacular release.
No statistical difference was detected between the patients with a routine lateral retinacular release and those without lateral retinacular release in terms of lateral retinacular release-related complications (n.s.), and these complications were usually mild and did not require reoperation. In support to the findings, a retrospective study by Kusuma et al. [21] on 1,108 patients with or without lateral retinacular release found no significant difference in lateral retinacular release-related complications between the two groups at an average follow-up of 4.7 years. Weber et al. [36] did a retrospective study of 1,071 patients with a follow-up of 5–11 years and suggested that the complications of lateral retinacular release are minimal. Though some authors reported that the lateral retinacular release could increase some complications, including patellar osteonecrosis, patella fracture, and wound-healing difficulties [5, 34], these complications often occur in patients with resurfacing of the patella and these literatures concerned are relatively old.
In this study, the length of hospital stay was similar in both groups (6.2 vs. 6.4 days), and none of patients in both groups needed a transfusion. Conversely, Molyneux and Brenkel [24] reported that the patients with lateral retinacular release stayed longer in hospital (10.8 vs. 8.6 days) and had higher transfusion rates (20.3 vs. 10.1 %) than those without lateral retinacular release. As to those patients discharged, this may use different criteria. In their study, it was routine that lots of their patients need stay in hospital longer, instead of postoperative complications. Molyneux and Brenkel [24] reported that the increased intraoperative blood loss led to a higher transfusion rates in patients with lateral retinacular release than those without lateral retinacular release. However, in the present study, the tourniquet was released when the limb was bandaged, and the bone wax was used to seal the osteotomy surfaces that were not covered by the prosthesis, which controlled the bleeding. Hence, our patients did not need a transfusion.
No statistical difference was detected between patients with a routine lateral retinacular release and those without lateral retinacular release in terms of postoperative patients’ satisfaction rates (83.1 vs. 80.9 %) at follow-up at 18 months. However, there are 77.8 % (14 out of 18) of patients with anterior knee pain who expressed their dissatisfaction with the outcomes of TKA. This suggests that anterior knee pain might be related to the patients’ dissatisfaction. Patients’ satisfaction following TKA is multifactorial and may be related to the patient expectation, pain relief, and the functional outcome, but a painful TKA was significantly associated with patients’ dissatisfaction [33].
The present study has several limitations. First, the outcomes were assessed at follow-up of 18 months, which may be too short, particularly for the evaluation of patellar fracture and osteonecrosis. However, the incidence of anterior knee pain and lateral retinacular release-related complications (such as haematoma, wound complications, and lateral knee pain) following TKA majorly occurred in short term [6]; in addition, it was actually reported that if the superior lateral geniculate artery was saved, lateral retinacular release had no effect on the incidence of patellar fracture and osteonecrosis [31]. Even though lateral retinacular release affects the blood supply of patella, it is transient that the blood supply to patella can be recovered to a near normal at 8 weeks [29]. Nevertheless, further follow-up is reasonable to determine whether routine performance of lateral retinacular release in TKA is similar for long-term rates of postoperative complications. Second, we did not compare differences in the rotation angle of components between the both groups. Postoperative component rotation alignment was not recommended as a routine examination, and many patients refuse to examine the rotation angle of components because the price of CT is expensive. And all the surgeries were performed by the same senior surgeon using the same surgical technique. Theoretically, the rotation angle of components was similar in the both groups. Third, the incidences of anterior knee pain in two groups were not stratified based on the degree of chondromalacia of the patellar cartilage. Many studies have suggested that the incidence of anterior knee pain did not associate with the chondromalacia [26, 35].
Conclusion
The results of this study show that a routine lateral retinacular release can reduce anterior knee pain and does not increase lateral retinacular release-related complications, in TKA with the use of the Gemini MK II mobile bearing without patellar resurfacing.
References
Akagi M, Oh M, Nonaka T et al (2004) An anteroposterior axis of the tibia for total knee arthroplasty. Clin Orthop Relat Res 420:213–219
Baliga S, McNair CJ, Barnett KJ et al (2012) Does circumpatellar electrocautery improve the outcome after total knee replacement? A prospective, randomised, blinded controlled trial. J Bone Joint Surg Br 94:1228–1233
Bindelglass DF, Cohen JL, Dorr LD (1993) Patellar tilt and subluxation in total knee arthroplasty. Relationship to pain, fixation, and design. Clin Orthop Relat Res 286:103–109
Bindelglass DF, Vince KG (1996) Patellar tilt and subluxation following subvastus and parapatellar approach in total knee arthroplasty. Implication for surgical technique. J Arthroplasty 11:507–511
Boyd AD Jr, Ewald FC, Thomas WH et al (1993) Long-term complications after total knee arthroplasty with or without resurfacing of the patella. J Bone Joint Surg Am 75:674–681
Breugem SJ, Sierevelt IN, Schafroth MU et al (2008) Less anterior knee pain with a mobile-bearing prosthesis compared with a fixed-bearing prosthesis. Clin Orthop Relat Res 466:1959–1965
Busch CA, Shore BJ, Bhandari R et al (2006) Efficacy of periarticular multimodal drug injection in total knee arthroplasty. A randomized trial. J Bone Joint Surg Am 88:959–963
Cho WS, Woo JH, Park HY et al (2011) Should the ‘no thumb technique’ be the golden standard for evaluating patellar tracking in total knee arthroplasty? Knee 18:177–179
Engh GA, Parks NL, Ammeen DJ (1998) Influence of surgical approach on lateral retinacular releases in total knee arthroplasty. Clin Orthop Relat Res 331:56–63
Ewald FC (1991) Leg lift technique for simultaneous femoral, tibial and patella prosthetic cementing, rule of “no thumb” for patella tracking and “steel rod rule” for ligament tension. Tech Orthop 6:44–46
Ewald FC (1989) The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 248:9–12
Feller JA, Baartllet RJ, Lang DM (1996) Patellar resurfacing versus retention in total knee arthroplasty. J Bone Joint Surg Br 78:226–228
Fu Y, Wang G, Fu Q (2011) Patellar resurfacing in total knee arthroplasty for osteoarthritis: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 19:1460–1466
Gomes LS, Bechtold JE, Gustilo RB (1988) Patellar prosthesis positioning in total knee arthroplasty. A roentgenographic study. Clin Orthop Relat Res 236:72–81
Holt GE, Dennis DA (2003) The role of patellar resurfacing in total knee arthroplasty. Clin Orthop Relat Res 416:76–83
Hsu HC, Luo ZP, Rand JA et al (1997) Influence of lateral release on patellar tracking and patellofemoral contact characteristics after total knee arthroplasty. J Arthroplasty 12:74–83
Hwang BH, Yang IH, Han CD (2012) Comparison of patellar retention versus resurfacing in LCS mobile-bearing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20:524–531
Insall JN, Dorr LD, Scott RD et al (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Jones AC, Ledingham J, McAlindon T et al (1994) Radiographic assessment of patellofemoral osteoarthritis. Ann Rheum Dis 52:655–658
King JJ III, Chakravarty R, Cerynik DL et al (2012) Decreased ratios of lateral to medial patellofemoral forces and pressures after lateral retinacular release and gender knees in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-012-2200-6
Kusuma SK, Puri N, Lotke PA (2009) Lateral retinacular release during primary total knee arthroplasty: effect on outcomes and complications. J Arthroplasty 24:383–390
Lee GW, Lee SM, Jang SJ et al (2013) The efficacy of patellar decompression for improving anterior knee pain following total knee arthroplasty without patellar resurfacing. Arch Orthop Trauma Surg 133:561–567
Leichtle UG, Wünschel M, Leichtle CI et al (2013) Increased patellofemoral pressure after TKA: an in vitro study. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-013-2372-8
Molyneux S, Brenkel I (2012) Predictors and outcomes of lateral release in total knee arthroplasty: a cohort study of 1859 knees. Knee 19:688–691
Muñoz-Mahamud E, Popescu D, Nuñez E, Lozano LM et al (2011) Secondary patellar resurfacing in the treatment of patellofemoral pain after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19:1467–1472
Oh IS, Kim MK, You DS et al (2006) Total knee arthroplasty without patellar resurfacing. Int Orthop 30:415–419
Ostermeier S, Holst M, Hurschler C et al (2007) Dynamic measurement of patellofemoral kinematics and contact pressure after lateral retinacular release: an in vitro study. Knee Surg Sports Traumatol Arthrosc 15:547–554
Outerbridge RE (1961) The etiology of chondromalacia patellae. J Bone Joint Surg Br 43:752–757
Pawar U, Rao KN, Sundaram PS et al (2009) Scintigraphic assessment of patellar viability in total knee arthroplasty after lateral release. J Arthroplasty 24:636–640
Peretz JI, Driftmier KR, Cerynik DL et al (2012) Does lateral release change patellofemoral forces and pressures? A pilot study. Clin Orthop Relat Res 470:903–909
Ritter MA, Pierce MJ, Zhou H et al (1999) Patellar complications (total knee arthroplasty). Effect of lateral release and thickness. Clin Orthop Relat Res 367:149–157
Sala D, Silvestre A, Gomar-Sancho F (1999) Intraosseous hyperpressure of the patella as a cause of anterior knee pain. Medscape Orthop Sports Med 3:1–8
Scott CE, Howie CR, MacDonald D et al (2010) Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Joint Surg Br 92:1253–1258
Scuderi G, Scharf SC, Meltzer LP et al (1987) The relationship of lateral releases to patella viability in total knee arthroplasty. J Arthroplasty 2:209–214
van Jonbergen HP, Scholtes VA, van Kampen A et al (2011) A randomised, controlled trial of circumpatellar electrocautery in total knee replacement without patellar resurfacing. J Bone Joint Surg Br 9:1054–1059
Weber AB, Worland RL, Jessup DE et al (2003) The consequences of lateral release in total knee replacement: a review of over 1000 knees with follow up between 5 and 11 years. Knee 10:187–191
Wiberg G (1941) Roentgenographic and anatomic studies on the patellofemoral joint with special reference to chondromalacia patellae. Acta Orthop Scand 12:319–410
Wilson NA, Press JM, Koh JL et al (2009) In vivo noninvasive evaluation of abnormal patellar tracking during squatting in patients with patellofemoral pain. J Bone Joint Surg Am 91:558–566
Yang CC, McFadden LA, Dennis DA et al (2008) Lateral retinacular release rates in mobile- versus fixed-bearing TKA. Clin Orthop Relat Res 466:2656–2661
Zhang DH, Wu ZQ, Zuo XC et al (2011) Diagnosis and treatment of excessive lateral pressure syndrome of the patellofemoral joint caused by military training. Orthop Surg 3:35–39
Acknowledgments
We are grateful for all patients who agreed to participate in this study. We thank Dr. Jia-Xiang Tian and Shi-Kai Zhang who evaluated the clinical data of patients.
Conflict of interest
This research was supported by the Postgraduate Innovation Project of Jiangsu Province of China (CXLX13_830). None of the authors has received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zha, GC., Sun, JY. & Dong, SJ. Less anterior knee pain with a routine lateral release in total knee arthroplasty without patellar resurfacing: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc 22, 517–525 (2014). https://doi.org/10.1007/s00167-013-2789-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-013-2789-0