Abstract
Purpose
The purpose of our study was to investigate whether advanced, 3D computed tomographic (CT)-generated hip models improves inter-and intra-observer agreement when compared to plain radiographs in identifying femoroacetabular impingement (FAI) morphology.
Methods
Eight consecutive patients who underwent surgery for FAI pathology were selected for this study. Preoperative CT scan image data were used to create high resolution, 3D hip reconstruction models. Four observers (two attending hip surgeons and radiologists) performed a blinded review of preselected radiographs and 3D CT hip models. Alpha and lateral center-edge angle measurements, location of cam lesion and the presence of a “crossover sign” were assessed. Inter- and intra-observer agreement was determined by calculating the intra-class correlation coefficients (ICC) or kappa coefficients to evaluate agreement for categorical variables.
Results
The parameter that demonstrated the highest and poorest inter-observer agreement was the presence of a “crossover sign” using 3D CT-generated high resolution hip models (ICC = 0.76, p = 0.00) and anteroposterior pelvis radiography, respectively (ICC = 0.20, p = 0.02). Alpha angle values were significantly higher using plain radiographs when compared to 3D hip reconstruction models (61.1° ± 10.4° versus 55.4° ± 14.4°, p = 0.003). Furthermore, when compared to radiographs, 3D hip reconstruction models demonstrated significantly higher intra-observer agreement (ICC = 0.856 versus 0.405, p = 0.005) when determining the presence of a “crossover sign”.
Conclusions
Our findings were suggestive that for most commonly used FAI morphology parameters, CT-generated hip models demonstrated little benefit over plain radiographs in improving inter-observer agreement among providers.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Femoroacetabular impingement (FAI) is a frequent source of hip pain in the young athletic population [1, 5]. Many radiographic parameters have been established to identify FAI in symptomatic and asymptomatic patients [7, 9, 10, 14]. Because the complex anatomy of the hip and the characteristics of FAI are considered to be three-dimensional entities, computed tomographic (CT) imaging has been used as an adjunct to plain radiographs to further identify and characterize FAI morphology [8, 16]. With the advent of newer methods to create greater detailed 3D CT-generated hip models, such advances can manipulate images to better improve identification of subtle morphologic signs of FAI. Specifically, the use of Materialise’s Interactive Medical image Control System (Mimics) software (Ann Arbor, MI) has been previously demonstrated to be effective in generating sophisticated models to improve precision for mapping anatomy, for preoperative planning and biomedical research [4, 18]. Such software use has been documented in shoulder research [11], but to the authors’ knowledge has had limited use in hip preservation imaging and research. It is thought that such advances can improve preoperative templates to better guide surgical planning, and ultimately lead to improve patient satisfaction and surgical results. However, the potential risk of increased radiation exposure contributing to the rise of malignant neoplasm, particularly in the pediatric population [3], and challenges faced with increasing health care costs raises the question on whether advanced CT imaging is necessary to improve identification of FAI morphology and consensus among musculoskeletal experts.
Although several reports exist in the literature comparing radiographs and CT imaging for selected parameters of FAI [15, 19], to the author’s knowledge, there are few studies that investigate the inter- and intra-observer reliability of several radiographic parameters of cam and pincer impingement when compared to modern, 3D CT-generated CT hip models that can manipulate images in a way to accentuate FAI morphology in a surgical patient cohort for symptomatic FAI. Thus, the purpose of our study was to compare the inter- and intra-observer reliability of FAI morphology parameters between modern, 3D CT-generated hip models (Mimics) and plain radiographs in a surgical cohort for symptomatic FAI. The null hypothesis for this study is that there is no difference seen in inter-or intra-observer agreement in identifying common FAI parameters between plain radiographs and advanced, 3D CT-generated hip models. The objective of this study was to determine whether advanced, 3D CT-generated images are a necessary component in the diagnostic algorithm of FAI diagnosis.
Materials and methods
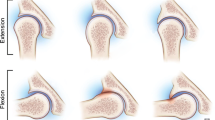
From the period of September 2009 and June 2011, eight consecutive patients who had previously undergone surgery for FAI pathology and agreed to preoperative CT scans for surgical planning purposes were selected for this study. All radiographs were taken at our institution using a standardized protocol for obtaining appropriate anteroposterior (AP) pelvis and frog lateral hip radiographic view as described by Clohisy et al. [6] (Fig. 1). CT scan images with 3D reconstructions were obtained with standard institutional protocols for the hip. CT scan image data were then imported into Mimics software for creation of high resolution, 3D reconstructions. Mimics software has the capacity to manipulate 3D CT-generated hip models to accentuate selected areas of the hip anatomy that need to be studied (Figs. 2, 3, 4). The 3D Mimics views that were created and used for analysis included the following: (1): anterior view of the affected hemipelvis; (2) anterior view of the affected hemipelvis with the femur subtracted from the image; (3), coronal anterior view of isolated femur; (4) coronal posterior view of isolated femur; (5) lateral view of isolated femur; and (6) superolateral view of isolated femur (Figs. 2, 3, 4). The anterior wall of the acetabulum was made relatively transparent so that the posterior wall of the acetabulum could be highlighted (Fig. 3). This was done to accentuate the presence of a true “crossover sign” [9]. All identifying information was removed from images and patients were randomly assigned a number so that the observers were blinded to diagnosis, clinical history and surgical procedure performed prior to the radiographic analysis.
Preoperative 3D Mimics, CT-generated hip model of same patient described in Fig. 1, demonstrating an AP pelvis view with the femur positioned in the acetabulum
AP pelvis view and with the femur subtracted from the acetabulum with a transparent anterior (a) and posterior wall (b) of the pelvis. Note the presence of a crossover sign (a and b; red arrow) demonstrating regional acetabular retroversion that was absent on the AP pelvis radiograph view (Fig. 1a)
Preoperative 3D Mimics, 3D CT-generated hip model of same patient described in patient 1 with rotated lateral (a, b) and coronal views of the femur subtracted from the acetabulum. The rotated 3D Mimics views demonstrate an anterior (black arrow) and posterior (dotted arrow). The posterior cam lesion is not well visualized on either the AP or frog lateral plain radiograph views of the same patient (Fig. 1a and b, respectively)
Two attending musculoskeletal radiologists and attending orthopedic surgeons, respectively, with special expertise in FAI surgery performed a blinded review of the preselected radiographs 3D CT-generated images created by Mimics software. The images were prepared in a presentation format and sent electronically. FAI parameters for radiographs and 3D CT analysis that were used included: (1) alpha angle; (2) lateral center-edge angle; (3) location of CAM lesion; e.g., anterior, posterior or both; and (4) the presence of a crossover sign [11, 13].
Alpha angle measurement was determined by the method previously describe by Clohisy et al. and Notzli et al. [6, 17]. Briefly, alpha angles were calculated by measuring the angle between two lines: (1) a line from the center of the femoral head to the point on the anterolateral aspect of the head-neck junction where the radius of the femoral head is discontinued (e.g., where the “bump” is located) and (2) a line drawn through the center of the femoral neck, connecting to the center of the femoral head. The lateral center-edge angle was measured by the method previously described by Clohisy et al. [6]. Briefly, a line is drawn through the center of the femoral head, perpendicular to the transverse axis of the pelvis. A second line is drawn through the center of the femoral head, passing through the most superolateral point of the sclerotic weight-bearing zone of the acetabulum. The angle created by the intersection of these two lines was determined to be the lateral center-edge angle. A positive “crossover sign” was determined whether a line drawn from the anterior acetabular rim bisected the line formed by the posterior acetabular rim [9].
Measurements were taken over the course of an eight-week period. The first and third distributions of images included a presentation of the selected radiographic images, only. Observers were asked to report their findings of the preselected FAI parameters. Radiographic review was separated over the course of a minimum of 2 weeks, and the order of the patients within the presentation was changed randomly with each distribution. The second and fourth distribution of images included the 3D CT-generated Mimics hip models, only. The order of images was again changed at random with each wave and each reading was separated by a minimum of 2 weeks. The data collected for radiographic and 3D CT-generated Mimics hip models for each subject were matched to one another analyzed. The study was approved by the Columbia University Medical Center Institutional Review Board (Protocol IRB-AAAF4010).
Statistical analysis
Inter- and intra-observer agreement was determined with the calculation of either first, the intra-class correlation coefficients (ICC) to evaluate the agreement between continuous variables or, second, kappa coefficients [12] to evaluate agreement for categorical variables. The inter- and intra-observer reliability was evaluated for each parameter between all raters. A test of equality of two correlation coefficients based Fisher z-transformation was performed to compare the reliability between radiographs and 3D CT-generated Mimics hip models. Differences in magnitude of alpha angle and lateral center-edge angle measurements between plain radiographs and CT-generated Mimics hip models were determined using a Student’s t test. A statistical significant difference was determined with an alpha error <0.05. As this was a preliminary investigation of this imaging modality, a feasibility sample of 8 patients corresponding to a review of 128 radiographic images per assessor during the study was completed.
Results
The mean age of the patients was 29.0 ± 11.9 years (range 17–48 years of age). There was an equal distribution of male and female patients (n = 4, each). Seven of eight patients demonstrated Tönnis grade 0, or no radiographic evidence of osteoarthrosis. One patient (17-year-old male) demonstrated Tönnis grade 1 radiographic evidence of osteoarthrosis on plain radiographs (e.g., increased sclerosis and slight joint space narrowing). Cam and pincer type impingement was arthroscopically confirmed in all patients.
Inter-observer reliability of FAI parameters using plain radiographs
The radiographic parameter that demonstrated the highest inter-observer reliability was alpha angle measurement (ICC = 0.75); however, this value did not reach statistical significant value (n.s., Table 1). Measurement of the lateral center-edge angle demonstrated a significant, moderate inter-observer reliability among all readers (ICC = 0.64, p = 0.00). Furthermore, determining the presence of a “crossover sign” on plain radiographs demonstrated a significantly poor inter-observer reliability among all readers (ICC = 0.20, p = 0.02; Table 1).
Inter-observer reliability of FAI parameters using 3D CT-generated Mimics hip models
The parameter that demonstrated the highest inter-observer reliability using 3D CT-generated Mimics modeling was determining whether a “crossover sign” was present (ICC = 0.76); this value was found to be statistical significant (p = 0.00) and was the parameter that had the highest ICC value between reviewers (Table 1). Measurement of the lateral center-edge angle also demonstrated a statistically significant and moderate inter-observer reliability among all readers (ICC = 0.50, p = 0.00, Table 1).
Intra-observer reliability of FAI parameters using plain radiographs
The presence of a “crossover” sign and measurement of the alpha angle demonstrated significant poor-to-moderate intra-observer reliability (ICC = 0.41, p = 0.01 and ICC = 0.34, p = 0.03, respectively, Table 2). The radiographic parameter that demonstrated the highest intra-observer reliability was the measurement of the lateral center-edge angle (ICC = 0.69); this value was found to be statistically significant (p = 0.00, Table 2).
Intra-observer reliability of FAI parameters using 3D CT-generated Mimics hip models
The measurements of the alpha angle on lateral projections (ICC = 0.58), lateral center-edge angle (ICC = 0.62) and determination of the presence of a “crossover” sign (ICC = 0.86) demonstrated statistically significant moderate-to-strong intra-observer reliability (p = 0.00 for all parameters).
Comparison of inter-observer reliability of radiographs and 3D CT-generated hip models
There was no significant difference when comparing inter-observer ICC values between plain radiographs and 3D CT-generated hip models for (1) lateral center-edge angle measurements, (2) alpha angle when measuring on a lateral projection, (3) determining the location of the cam lesion or (4) determining the presence of a “crossover” sign (Table 3).
Comparison of intra-observer reliability of radiographs and 3D CT-generated Mimics hip models
When compared to plain radiographs, 3D Mimics hip models significantly improved intra-observer reliability when determining the presence of a “crossover sign” (ICC = 0.86 versus 0.41, p = 0.01, Table 4).
Comparison of magnitude of alpha and lateral center-edge angle measurements on radiographs and 3D CT-generated Mimics hip models
Mean alpha angles measured on frog lateral radiographs were significantly higher than comparable measurements on lateral, 3D Mimics hip models (61° vs. 55°, radiographs vs. CT model, p = 0.00). Conversely, there was no significant difference in lateral center-edge angle measurements between radiographs and 3D CT-generated Mimics hip models (35° vs. 36°, radiographs vs. CT model, n.s., Table 5).
Discussion
The most important finding of this study is that, CT-generated hip models demonstrated little benefit over plain radiographs in improving inter-observer agreement among providers. The decision on whether to use 3D CT imaging in defining FAI morphology is often a difficult one that many practitioners encounter in daily clinical practice. This finding may help to limit the overuse of generating expensive, and more importantly, high radiation exposure CT images for FAI diagnosis and morphology identification.
Currently, there are few studies that look at the strength of inter- and intra-observer agreement of commonly used FAI radiographic parameters using plain radiographs and advanced, 3D CT-generated hip models. Furthermore, there are limited studies that investigate the relationship between inter- and intra-observer agreement when comparing equivalent FAI parameters on radiographs and advanced, 3D CT-generated hip models in a surgical patient cohort [15]. In the present study, the parameter that reached the highest, significant inter-observer agreement was determining the presence of a “crossover sign” using anatomy-accentuating 3D CT-generated hip models. Conversely, the determination of the presence of a “crossover sign” on plain radiographs demonstrated the poorest, significant inter-observer agreement. However, this was the only parameter that 3D CT-generated hip models that demonstrated an advantage over plain radiographs.
There are several studies that investigate specific parameters of FAI and inter- and intra-observer reliability [2]. The most inclusive study of these studies was the one performed by Mast et al. [14]. The authors identified twenty plain radiographic parameters of FAI and examined the agreement among observers by calculating the intra-class coefficient (ICC). The observers consisted of a third-year resident surgeon and second-year hip fellow who were given radiographic interpretation instructions. The authors concluded that “measurements that could be measured directly” (e.g., femoral head diameter) were more reliable that measurements that required estimation on the part of the observer (e.g., Tönnis angle or neck shaft angle). Although the authors were rather inclusive with regard to number of radiographic parameters studied, the authors did not include advanced, 3D CT imaging in their analysis to determine whether CT could improve inter- and/or intra-observer reliability. Furthermore, one could consider the observers as having limited experience in identifying FAI pathology when compared to attending hip surgeons.
With regard to radiographic parameters of cam impingement, Nepple et al. [15] investigated the correlation of alpha angle radiographic measurements using the method described by Notzli et al. [17], of plain radiographs when compared with CT-reformatted images in a series of forty-one surgical patients. The authors noted that observers assigned larger alpha angles on plain radiographs in over 60 % of cases when compared to CT-reformatted images. These findings support this result as observers in this study also reported higher alpha angles on radiographs when compared to similar projections using 3D CT-generated hip models. However, Nepple et al. [15] reported moderate intra-class correlation of alpha angle measurements (ICC between 0.64 and 0.75) between radiographs and CT radiographs. This is contrary to findings in this study where inter-observer reliability was moderate for alpha angle using plain radiographs, but much lower when using 3D CT-generated Mimics models, and no significant differences were observed between radiograph and CT imaging with regards to inter- or intra-observer ICC for alpha angle measurement. To explain the differences seen in the two reports, it should be noted that in the study by Nepple et al. [15], utilized the CT images were two-dimensional in nature. It is possible that using 2D, CT-reformatted images may underestimate the subtle FAI morphology captured with 3D CT imaging. The findings of the present study suggest that the addition of increased complexity to the CT-generated models do not appear to increase inter-observer agreement over plain radiographs for the identification of most FAI morphology.
Furthermore, with regard to radiographic parameters of pincer impingement, Zaltz et al. [20] demonstrated that radiographic the presence of a “crossover sign” can overestimate acetabular retroversion even among experienced hip surgeons when examining plain radiographs and comparing 3D CT acetabular version analysis. The authors identify “down-sloping” or “hooked” anterior inferior iliac spine (AIIS) morphology as a causative factor for falsely overestimating acetabular retroversion using plain radiographs. The present study differs from the report of Zaltz et al. [20], with the ability of using Mimics 3D CT-generated hip models to highlight pertinent acetabular morphology (e.g., posterior wall) while simultaneously creating a “transparent” anterior wall to better aide in identifying a true “crossover sign” and AIIS morphology. Furthermore, by using Mimics 3D CT-generated hip models, we were able to control for proper pelvic tilt and rotation with image manipulation and standardize image creation when compared to the variability in technique commonly seen with standard hip radiographs.
There are several limitations in this study. First, the authors recognize that the cohort investigated in this study was small and the findings reported in this study should be considered preliminary. The small sample number was due to the limited availability of preoperative CT scans needed to generated 3D Mimics hip models, as preoperative CT imaging is not routinely ordered in our institution for FAI surgery. However, despite the small study numbers, significant intra-class correlations were seen for both imaging modalities. Second, generating Mimics, 3D hip models are time-consuming and costly and thus may not be cost-effective in routine clinical practice and cases. Thus, the investigators currently support advanced 3D hip models for research and for potential use in difficult cases, such as revision FAI surgery or cases with abnormal pelvic tilt. Future studies will need to be performed to determine whether adding advanced 3D hip models in the clinical algorithm for FAI can improve surgical outcomes when compared to using plain radiographs for preoperative planning. Third, we recognize that many other parameters of FAI do exist and were not studied and may have significant inter- and intra-observer agreement between radiographs and advanced CT imaging. Furthermore, this study is unique compared to previously mentioned studies in that the observers consisted of two experienced hip surgeons familiar with FAI surgery and two experienced radiologists. Although sub-analysis of differences between hip surgeons and radiologist were not highlighted in this report, the authors recognize that future studies are needed to determine whether differences exist between these important groups of musculoskeletal providers that treat FAI [2].
Conclusion
In conclusion, for determining the presence of a “crossover sign”, advanced, 3D CT-generated hip models improve inter- and intra-observer agreement. However, for the majority of the other common parameters for FAI identification, our findings suggest that there appears to be no significant advantage in improving inter-observer agreement using advanced, 3D CT-generated hip model when compared to plain radiographs.
References
Ayeni OR, Banga K, Bhandari M, Maizlin Z, de Sa D, Golev D, Harish S, Farrokhyar F (2014) Femoroacetabular impingement in elite ice hockey players. Knee Surg Sports Traumatol Arthrosc 22(4):920–925
Ayeni OR, Chan K, Whelan DB, Gandhi R, Williams D, Harish S, Choudur H, Chiavaras M, Karlsson J, Bhandari M (2014) Diagnosing femoroacetabular impingement from plain radiographs: do radiologists and orthopaedic surgeons differ? Orthop J Sports Med 2(7):1–7
Brenner DJ, Elliston CD, Hall EJ, Berdon WE (2001) Estimates of the cancer risks from pediatric CT radiation are not merely theoretical: comment on “point/counterpoint: in X-ray computed tomography, technique factors should be selected appropriate to patient size against the proposition”. Med Phys 28(11):2387–2388
Bryce CD, Pennypacker JL, Kulkarni N, Paul EM, Hollenbeak CS, Mosher TJ, Armstrong AD (2008) Validation of three-dimensional models of in situ scapulae. J Shoulder Elbow Surg 17(5):825–832
Chaudhry H, Ayeni OR (2014) The etiology of femoroacetabular impingement: what we know and what we don’t. Sports Health 6(2):157–161
Clohisy JC, Carlisle JC, Beaule PE, Kim YJ, Trousdale RT, Sierra RJ, Leunig M, Schoenecker PL, Millis MB (2008) A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am 90(Suppl 4):47–66
Gosvig KK, Jacobsen S, Sonne-Holm S, Gebuhr P (2008) The prevalence of cam-type deformity of the hip joint: a survey of 4151 subjects of the Copenhagen Osteoarthritis Study. Acta Radiol 49(4):436–441
Grabinski R, Ou D, Saunder K, Rotstein A, Singh P, Pritchard M, O’Donnell J (2014) Protocol for CT in the position of discomfort: preoperative assessment of femoroacetabular impingement—how we do it and what the surgeon wants to know. J Med Imaging Radiat Oncol. doi:10.1111/1754-9485.12201
Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, Leunig M (2007) Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign”. J Orthop Res 25(6):758–765
Kalberer F, Sierra RJ, Madan SS, Ganz R, Leunig M (2008) Ischial spine projection into the pelvis: a new sign for acetabular retroversion. Clin Orthop Relat Res 466(3):677–683
Khan M, Ranawat A, Williams D, Gandhi R, Choudur H, Parasu N, Simunovic N, Ayeni OR (2014) Relationship between the alpha and beta angles in diagnosing CAM-type femoroacetabular impingement on frog-leg lateral radiographs. Knee Surg Sports Traumatol Arthrosc [Epub ahead of print]
Kraemer HC, Periyakoil VS, Noda A (2002) Kappa coefficients in medical research. Stat Med 21(14):2109–2129
Mariconda M, Cozzolino A, Di Pietto F, Ribas M, Bellotti V, Soldati A (2014) Radiographic findings of femoroacetabular impingement in capoeira players. Knee Surg Sports Traumatol Arthrosc 22(4):874–881
Mast NH, Impellizzeri F, Keller S, Leunig M (2011) Reliability and agreement of measures used in radiographic evaluation of the adult hip. Clin Orthop Relat Res 469(1):188–199
Nepple JJ, Martel JM, Kim YJ, Zaltz I, Clohisy JC (2012) Do plain radiographs correlate with CT for imaging of cam-type femoroacetabular impingement? Clin Orthop Relat Res 470(12):3313–3320
Nepple JJ, Prather H, Trousdale RT, Clohisy JC, Beaulé PE, Glyn-Jones S, Rakhra K, Kim YJ (2013) Diagnostic imaging of femoroacetabular impingement. J Am Acad Orthop Surg 21(Suppl 1):S20–S26
Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J (2002) The contour of the femoral head–neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br 84(4):556–560
Nowak DD, Bahu MJ, Gardner TR, Dyrszka MD, Levine WN, Bigliani LU, Ahmad CS (2009) Simulation of surgical glenoid resurfacing using three-dimensional computed tomography of the arthritic glenohumeral joint: the amount of glenoid retroversion that can be corrected. J Shoulder Elbow Surg 18(5):680–688
Tannast M, Mistry S, Steppacher SD, Reichenbach S, Langlotz F, Siebenrock KA, Zheng G (2008) Radiographic analysis of femoroacetabular impingement with Hip2Norm—reliable and validated. J Orthop Res 26(9):1199–1205
Zaltz I, Kelly BT, Hetsroni I, Bedi A (2012) The crossover sign overestimates acetabular retroversion. Clin Orthop Relat Res 471(8):2463–2470
Acknowledgments
We would like to thank Dr. Darren de SA, Orthopaedic Resident at McMaster University, for his contributions toward preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cadet, E.R., Babatunde, O.M., Gorroochurn, P. et al. Inter- and intra-observer agreement of femoroacetabular impingement (FAI) parameters comparing plain radiographs and advanced, 3D computed tomographic (CT)-generated hip models in a surgical patient cohort. Knee Surg Sports Traumatol Arthrosc 24, 2324–2331 (2016). https://doi.org/10.1007/s00167-014-3315-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3315-8