Abstract
Purpose
Detailed biomechanical analysis including isokinetic muscle strength measurements after autologous chondrocyte implantation (ACI) are still rare, but might be of crucial importance for long-term outcomes. The present prospective study was performed to evaluate whether defect location had any influence on clinical and biomechanical outcomes 4 years after ACI.
Methods
Forty-four patients with full-thickness cartilage defects ICRS grade III B and C underwent ACI and were assigned to two groups, the femoral condyle group or the patellofemoral joint group. Clinical scores were gathered preoperatively and 6, 12 and 48 months after implantation using the International Knee Documentation Committee (IKDC) score and the International Cartilage Repair Society (ICRS) form. Isokinetic strength measurements were performed 48 months postoperatively comparing healthy and operated knee joint of each patient.
Results
Clinical scores (ICRS, IKDC) showed continuous significant (p < 0.05) improvement over the study period for both groups. Isokinetic muscle strength measurements showed significantly reduced maximum strength capacities for the operated knee joint compared to the healthy knee in both groups (p < 0.05). Hamstring–quadriceps ratios of the operated extremity revealed a significant change in physiological muscle balancing (ratios >1.0) based on significantly impaired extensor muscle strength in the patellofemoral joint group.
Conclusion
All patients showed significant strength deficits on the operated extremity 4 years after ACI. Furthermore, the patellofemoral compartment in particular showed significantly worse hamstring–quadriceps ratios compared to condylar defects. Consequently, more efforts should be made to restore muscular strength especially of the quadriceps and the rehabilitation protocol should be adjusted accordingly.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Articular cartilage defects appear frequently in all age groups and may cause severe limitations in activities of daily living due to symptoms such as pain and joint stiffness. With the introduction of autologous chondrocyte implantation (ACI) in 1994 [8] and the developments of this technique, it now appears that a promising treatment option may have been found. Many studies have been published, indicating that, if current indications and contraindications are respected [5], patients benefit significantly from this procedure even over the long term [7, 36, 40]. Furthermore, the second-generation ACI is also a suitable treatment option for the repair of focal degenerative defects of the knee [26].
To date, there has been no general agreement on the postoperative treatment and rehabilitation after ACI. There have been continuous surgical advances in the treatment of articular cartilage lesions, yet few detailed biomechanical evaluations after ACI exist. Previously published biomechanical studies analysing muscle strength after anterior cruciate ligament reconstruction have revealed significant strength deficits that persist at long-term follow-up [3, 4, 18, 23, 30]. Quadriceps weakness in particular, which may result from activation failure as well as muscle atrophy [39], has been shown to have a long-term negative impact on knee function and may also be a predictor of early onset of osteoarthritis [38, 44].
This is corroborated by Mikkelsen et al. [34] who showed that patients with good quadriceps torque after ACL reconstruction returned to their previous activity level significantly earlier.
To date, only five studies have been published dealing with muscle strength measurements after autologous chondrocyte implantation [13, 27–29, 31]. However, this is the first study to evaluate the particular influence of defect location on biomechanical strength outcomes and the balancing of different muscle groups.
The aim of this prospective study was to evaluate whether defect location had an impact on clinical outcome and isokinetic muscle strength performance 4 years after autologous chondrocyte implantation by comparing the operated leg with the healthy, non-treated extremity. Correlation between clinical and isokinetic outcome was done.
The results of this study may contribute to develop specific rehabilitation protocols optimized for different implantation locations to improve clinical and functional outcomes after autologous chondrocyte implantation.
Materials and methods
Between December 2001 and April 2004, 79 patients with focal posttraumatic or degenerative symptomatic cartilage defects were treated with matrix-associated autologous chondrocyte implantation (BioSeed®-C, BioTissue Technologies GmbH, Freiburg, Germany).
In total, there were 44 patients, who fulfilled the inclusion criteria (below) and were enrolled in this prospective trial for a period of 48 months.
Inclusion criteria
Patients had to be between 18 and 55 years of age. Chondral defects had to be full-thickness defects grade III B, C according to the ICRS classification system [19]. The lesions were sized ≥2 cm2 and had to be localized in only one of the 3 knee compartments.
Exclusion criteria
Patients with acute trauma, limits in knee extension or flexion less than 130°, varus or valgus deformities of more than 5°, patella malalignment with medial or lateral shift of more than 0.5 cm, instabilities of the collateral or cruciate ligaments, meniscal tears, status after total or partial meniscectomy, osteochondral defects, drug treatment for osteoarthritis or intra-articular corticosteroid injections within the previous month were excluded.
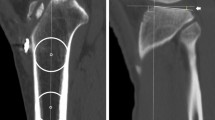
Table 1 shows the baseline characteristics of the included patients. The patient collective was divided into two major groups according to the defect location: the femoral condyle group (medial and lateral femoral condyles) (n = 28) and the patellofemoral joint group (Trochlea (n = 5) and retropatellar (n = 11)) (n = 16). There were no significant differences between both groups concerning patients’ characteristics.
Surgical procedure
Implantation of matrix-associated autologous chondrocytes was done in a two-step procedure: in a first arthroscopy, approximately 250 mg of healthy cartilage tissue was harvested from a less weight bearing area of the knee joint. After in vitro expansion, approximately 20 million chondrocytes were rearranged in a three-dimensional polymer-based scaffold (3 × 2 × 0.2 cm). The second step consisted in a mini-open implantation of the graft into the defect area by the previously described anchor-knot technique [15, 26, 27].
Rehabilitation protocol
Patients’ mobilization on crutches with a maximal loading of 15 % body weight and continuous passive motion and range of motion (ROM) exercises started the day after surgery. Patients with femoral condyle implants were not limited in their ROM in contrast to patients treated with patellofemoral joint implants. These patients were limited to 40° ROM for the first 2 weeks, 60° ROM in the following 2 weeks and 90° ROM in weeks 5–6 postoperatively. Patients then gradually increased loading and performed active physiotherapy and gentle ergometric training for the next 6 weeks. Full weight bearing was anticipated after 10–12 weeks in combination with increased strength training and coordination exercises. After 4 months, low-impact activities such as cycling or jogging were allowed, while more strenuous activities and contact sports were not recommended before 9–12 months after implantation. Patients’ compliance with rehabilitation was not monitored.
Clinical evaluation and isokinetic muscle strength measurements
Clinical outcome of 44 patients was evaluated using the International Cartilage Repair Society (ICRS) and the International Knee Documentation Committee (IKDC) forms [2]. Data were documented preoperatively and at 6, 12 and 48 months after implantation.
Strength measurements were performed after 48 months by a single examiner using an isokinetic dynamometer (CON-TREX MJ Multi-joint Module, CMV AG, Dübendorf, Switzerland). Isokinetic strength measurements performed on this dynamometer have been proven objective, reliable, valid and reproducible [9, 32].
On physical examination before isokinetic testing, none of our patients had significant effusion, swelling or pain on exertion, thus allowing us to perform strength measurements on all of them. Before testing, patients warmed up on a treadmill for 10 min. Patients were then seated in the assessment chair with trunk and thighs stabilized with belts to avoid additional body movement during isokinetic testing. The test protocol consisted of 5 reciprocal flexion and extension movements with maximal strength effort to evaluate hamstring and quadriceps strength. After gravity correction of the tested limb, each measurement was performed in three different test modes with the healthy, then the operated knee joint. Two concentric modes had an angular velocity of 60°/s and 180°/s and an eccentric mode 60°/s. Range of motion (ROM) was defined 0/10/90° (extension/flexion) at all test modes. A rest period of at least 60 s followed each set. In every mode, 5 maximum peak torque values were recorded in Newtonmeters (Nm).
To achieve the highest possible accuracy of our measurements, the parameter used for analysis of maximum strength was the mean value calculated from the best 3 of 5 maximum peak torque values as described in previous studies [21, 33, 35]. Furthermore, mean values were used to calculate the hamstring–quadriceps (H–Q) ratio of the operated leg in comparison with the healthy leg.
Statistical analysis
For statistical analysis, comparison of clinical and isokinetic outcomes between subgroups was performed using the Mann–Whitney U test for nonparametric data and considered significant at p < 0.05. Improvement or decline of clinical scores over the follow-up period was compared using the Wilcoxon test for parametric data. Differences were considered significant at p < 0.05. The Wilcoxon test was further used to analyse parametric biomechanical data at 4-year follow-up, performed on the healthy and operated knee of each patient. Differences were considered significant at p < 0.05. We also correlated clinical scores and isokinetic outcome at 48 months after implantation using the Pearson’s coefficient of correlation that was considered significant at p < 0.05.
Results
Clinical evaluation 4 years after implantation of autologous chondrocytes
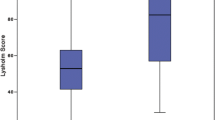
The ICRS score (Table 2a) showed a constant improvement in both the femoral condyle and the patellofemoral joint group. Statistical comparison between both defect groups revealed no significant differences over the entire follow-up period.
With a single exception (patellofemoral group 6–12 months), improvements were significant (p < 0.05) over the entire study period. Compared to the preoperative baseline, both groups achieved highly significant improvements (p < 0.001) 4 years after treatment. Mean findings in the ICRS score improved in both groups to now “nearly normal” clinical findings compared to “severe abnormal” before ACI (Table 2a).
The IKDC knee evaluation score (Table 2b) also improved continuously over the entire study period in both groups. Again no significant differences were found between both groups. The Wilcoxon test showed significant improvement for every tested adjacent follow-up period with highly significant improvement after 4 years compared to baseline results (p < 0.001).
Biomechanical strength evaluation 4 years after implantation of autologous chondrocytes
As Table 3 shows, the operated knee joint revealed significantly (p < 0.05) weaker quadriceps and hamstring peak torques compared to the corresponding healthy muscle group in all test modes and all groups. The patellofemoral joint group in particular showed severely reduced quadriceps strength compared to the femoral condyle group. However, even if the mean values of the patellofemoral joint group were noticeably worse, statistical comparison of single muscle groups did not show significant differences between both groups yet (p > 0.05). The hamstring–quadriceps ratio is often used in international literature to determine muscular balance. The physiological range is between 0.5 and 0.75 depending on age and angular velocity [1, 17, 20, 46], indicating that the quadriceps muscle normally is up to twice as strong as the hamstring group. Four years after implantation of autologous chondrocytes both groups revealed considerably altered hamstring–quadriceps ratios particularly on the operated extremity (Table 4). Furthermore, resulting from the aforementioned severe reduction in quadriceps strength, the operated leg of patients treated at the patellofemoral compartment experienced a change in strength with ratios above 1.0 in concentric and eccentric test modes. Statistical comparison of hamstring–quadriceps ratios now revealed significantly worse results in the patellofemoral joint group compared to the femoral condyle group (p < 0.05, concentric 60°/s operated and healthy, eccentric operated).
Correlation of clinical and isokinetic scores 48 months after implantation of Bioseed-C
Correlation between clinical scores and isokinetic values were performed for all patients together using the Pearson’s coefficient of correlation (PC). Objective ICRS score showed positive correlation (p < 0.05) with all collected peak torque mean values with a single exception (Table 5). The subjective IKDC score showed positive correlations (p < 0.05) with the operated extensor and flexor muscles in the concentric test modes.
Discussion
The most important finding of the present study was the persisting significant strength deficit at the operated extremity even 48 months after ACI and furthermore the location-specific significant differences in hamstring–quadriceps ratios.
Supporting previously published positive mid- to long-term results after the second-generation ACI [6, 12, 24], the included patients showed good to excellent clinical outcomes with highly significant improvement 4 years postoperatively compared to the preoperative baseline. Furthermore, the patellofemoral joint group, for which worse clinical outcomes had been previously reported [7, 37, 40], showed comparable results to the femoral condyle group with no statistically significant differences. However, despite the good clinical outcome, the patellofemoral joint group in particular showed the greatest strength deficits, predominantly affecting the quadriceps muscle.
The biomechanical data presented in this study confirm the results of two other studies including strength measurements after autologous chondrocyte implantation published by Loken et al. [31] and Ebert et al. [13]. In Lokens et al. study, 21 patients were evaluated clinically and isokinetically 1, 2 and 7.4 years after the first-generation ACI. While clinical scores improved constantly, they found highly significant side-to-side differences for knee flexion and extension workload even 7.4 years after ACI [31]. Supporting the findings of the present study, strength deficits of the operated knee in their patient population were greater in knee extension than in flexion. The authors did not distinguish between different defect locations.
In Ebert’s et al. [13] published study, isokinetic strength values of 60 patients 5 years after the second-generation ACI were assessed. While there were no significant differences in hamstring strength between operated and non-operated side, they found a significantly impaired quadriceps strength at a defined flexion angle of 45° on the operated leg.
While the statistical comparison of hamstring and quadriceps muscles individually did not show significant differences between both defect groups, the particular impact of the defect location could be revealed by analysing the muscle balancing. Resulting from the severely impaired extensor muscles, the patellofemoral group showed significantly worse hamstring–quadriceps ratios compared to condylar defects in all test modes (p < 0.05).
Ebert et al. [13] also reported elevated H–Q ratios varying from 0.81 to 0.93 on the healthy extremity and from 0.86 to 0.97 on the operated side. Bilaterally elevated H–Q ratios are suggestive of a general bilateral postoperative weakness in quadriceps strength that result from the prolonged period of relative inactivity after ACI surgery [13]. Ebert et al. did not provide information about their patients’ clinical outcome, and they only treated patients with femoral and not with patellar defects, what aggravates a comparison with our results.
A possible explanation for the significantly reduced quadriceps strength of the patellofemoral group might be the more invasive arthrotomy with elevation of the patella compared to defects on the femoral condyles. For the articulation of the patella, muscle balancing and proprioception in the patellofemoral joint are more important than in the femorotibial compartment. With the more invasive approach in the patellofemoral compartment, both the extensor muscles, and the joint capsule and ligaments were affected, leading to a pronounced strength deficit of the extensor muscles. Development of more soft-tissue sparing surgical approaches in this specific compartment might therefore reduce damage to these structures and may result in improved postoperative muscle strength and balancing.
Likewise, the delayed postoperative exercise regimen of this group (weeks 1–2 flexion limit 40°, weeks 3–4 flexion limit 60°, weeks 5–6 flexion limit 90°) may as well result in more muscle atrophy and functional limitation of the knee joint, than generally anticipated.
Strengths of our study are the detailed bilateral biomechanical evaluations 4 years after ACI and well-defined inclusion and exclusion criteria. In this context, patients with pre-existing patellofemoral or femorotibial malalignment, which have been shown to influence clinical and functional outcome [45], were previously excluded, thus raising the quality of the presented results.
A limitation of the present study is a follow-up intermission between the results after 1 year and the midterm re-evaluation 48 months after ACI. However, based on previous studies after ACI, which showed greatest improvement in clinical outcome predominantly in the first 12 months and only few changes afterwards [12, 16, 42], we decided to re-evaluate the patient collective with special focus on midterm results at 48 months.
Furthermore, we did not differentiate if the operated knee joint was in the dominant or non-dominant leg, based on previously published studies, that showed no significant differences between dominant and non-dominant leg [11, 13].
Strength measurements were not compared with a non-operated control group. As an alternative, the patients’ contralateral extremity was used as a control, assuming that the non-treated side would correspond to a healthy normal value for each patient [13, 22, 31]. It cannot be conclusively determined if patients with retropatellar or trochlear defects had greater pre-existing strength deficits before implantation of autologous chondrocytes, since biomechanical tests on this isokinetic dynamometer were unfortunately not available earlier than 48 months after ACI. However, preoperative assessment of maximum strength scores tend to be unreliable because of pain, swelling and other functional limitations [13]. For this reason, both other available isokinetic studies after ACI by Ebert et al. and Loken et al. [13, 31] purposely abstained from performing preoperative muscle strength measurements similar to the present study, where the focus of the biomechanical tests was placed on the 48-month midterm outcomes.
Besides the good clinical midterm results of the included patients, the distinct impairment of quadriceps strength in the patellofemoral compartment with resultant muscular imbalance in the H–Q ratio is concerning. As reported in other studies, quadriceps strength deficit is a strong negative predictor for long-term clinical outcome, since it leads to early onset of osteoarthritis [41, 43]. For this reason, all efforts must be made to restore muscle strength, particularly of the quadriceps to secure normal muscle balancing. Additionally, the rehabilitation process should be appropriately modified to include early patella mobilization as well as postoperative strength and neuromuscular coordination exercises.
Affirming this aspect, Della Villa et al. [10] reported that early postoperative quadriceps training after ACI had positive effects on clinical outcome and resulted in an earlier return to preoperative activity levels. Furthermore, intensified physical training after ACI led to significantly better long-term outcomes compared to patients with a lower activity level [25].
The preoperative quadriceps strength is also an important factor for postoperative outcome: Eitzen et al. [14] showed in their study that patients with preoperative quadriceps strength approaching normal values had significantly better results 2 years after anterior cruciate ligament reconstruction. Therefore, we recommend quadriceps training in the preoperative period, e.g. between arthroscopical cartilage biopsy and implantation of the loaded scaffold 6 weeks later. The location-specific biomechanical strength measurements after ACI in the present study help to improve treatment and postoperative rehabilitation protocols of patients with patellofemoral defects. However, further studies examining the influence of such modified pre- and postoperative rehabilitation protocols on clinical and biomechanical outcomes after ACI are recommended.
Conclusion
The promising clinical results of our patients are negatively affected by a marked persisting strength deficit especially affecting the quadriceps muscle of patients treated in the patellofemoral compartment. Therefore, muscle strength must be restored as soon as possible in order to prevent clinical worsening. A pain adapted bilateral preoperative strength training and a defect location-specific postoperative treatment regimen under physiotherapeutic guidance with close clinical observations for the first two postoperative years would be desirable.
References
Aagaard P, Simonsen EB, Trolle M, Bangsbo J, Klausen K (1995) Isokinetic hamstring/quadriceps strength ratio: influence from joint angular velocity, gravity correction and contraction mode. Acta Physiol Scand 154(4):421–427
Aglietti A, Gambardella R, Hangody L et al (2000) ICRS Cartilage injury evaluation package. http://www.cartilage.org/_files/contentmanagement/ICRS_evaluation.pdf
Anderson AF, Snyder RB, Lipscomb AB (2001) Anterior cruciate ligament reconstruction. A prospective randomized study of three surgical methods. Am J Sports Med 29(3):272–279
Beard DJ, Anderson JL, Davies S, Price AJ, Dodd CA (2001) Hamstrings vs. patella tendon for anterior cruciate ligament reconstruction: a randomized controlled trial. Knee 8(1):45–50
Behrens P, Bosch U, Bruns J et al (2004) Indications and implementation of recommendations of the working group “Tissue Regeneration and Tissue Substitutes” for autologous chondrocyte transplantation (ACT). Z Orthop Ihre Grenzgeb 142(5):529–539
Behrens P, Bitter T, Kurz B, Russlies M (2006) Matrix-associated autologous chondrocyte transplantation/implantation (MACT/MACI)–5-year follow-up. Knee 13(3):194–202
Brittberg M (2008) Autologous chondrocyte implantation-technique and long-term follow-up. Injury 39(Suppl 1):40–49
Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L (1994) Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med 331(14):889–895
Carpenter MR, Carpenter RL, Peel J, Zukley LM, Angelopoulou KM, Fischer I, Angelopoulos TJ, Rippe JM (2006) The reliability of isokinetic and isometric leg strength measures among individuals with symptoms of mild osteoarthritis. J Sports Med Phys Fitness 46(4):585–589
Della Villa S, Kon E, Filardo G, Ricci M, Vincentelli F, Delcogliano M, Marcacci M (2010) Does intensive rehabilitation permit early return to sport without compromising the clinical outcome after arthroscopic autologous chondrocyte implantation in highly competitive athletes? Am J Sports Med 38(1):68–77
Demura S, Yamaji S, Goshi F, Nagasawa Y (2001) Lateral dominance of legs in maximal muscle power, muscular endurance, and grading ability. Percept Mot Skills 93(1):11–23
Ebert JR, Robertson WB, Woodhouse J, Fallon M, Zheng MH, Ackland T, Wood DJ (2011) Clinical and magnetic resonance imaging-based outcomes to 5 years after matrix-induced autologous chondrocyte implantation to address articular cartilage defects in the knee. Am J Sports Med 39(4):753–763
Ebert JR, Lloyd DG, Wood DJ, Ackland TR (2012) Isokinetic knee extensor strength deficit following matrix-induced autologous chondrocyte implantation. Clin Biomech (Bristol, Avon) 27(6):588–594
Eitzen I, Holm I, Risberg MA (2009) Preoperative quadriceps strength is a significant predictor of knee function two years after anterior cruciate ligament reconstruction. Br J Sports Med 43(5):371–376
Erggelet C, Sittinger M, Lahm A (2003) The arthroscopic implantation of autologous chondrocytes for the treatment of full-thickness cartilage defects of the knee joint. Arthroscopy 19(1):108–110
Henderson I, Francisco R, Oakes B, Cameron J (2005) Autologous chondrocyte implantation for treatment of focal chondral defects of the knee- a clinical, arthroscopic, MRI and histologic evaluation at 2 years. Knee 12(3):209–216
Hewett TE, Myer GD, Zazulak BT (2008) Hamstrings to quadriceps peak torque ratios diverge between sexes with increasing isokinetic angular velocity. J Sci Med Sport 11(5):452–459
Hiemstra LA, Webber S, MacDonald PB, Kriellaars DJ (2000) Knee strength deficits after hamstring tendon and patellar tendon anterior cruciate ligament reconstruction. Med Sci Sports Exerc 32(8):1472–1479
Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, Richmond JC, Shelbourne KD (2001) Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med 29(5):600–613
Kannus P (1988) Ratio of hamstring to quadriceps femoris muscles’ strength in the anterior cruciate ligament insufficient knee. Relationship to long-term recovery. Phys Ther 68(6):961–965
Kannus P (1994) Isokinetic evaluation of muscular performance: implications for muscle testing and rehabilitation. Int J Sports Med 15. Suppl 1:S11–S18
Kannus P, Yasuda K (1992) Value of isokinetic angle-specific torque measurements in normal and injured knees. Med Sci Sports Exerc 24(3):292–297
Keays SL, Bullock-Saxton J, Keays AC, Newcombe P (2001) Muscle strength and function before and after anterior cruciate ligament reconstruction using semitendinosus and gracilis. Knee 8(3):229–234
Kon E, Gobbi A, Filardo G, Delcogliano M, Zaffagnini S, Marcacci M (2009) Arthroscopic second-generation autologous chondrocyte implantation compared with microfracture for chondral lesions of the knee: prospective nonrandomized study at 5 years. Am J Sports Med 37(1):33–41
Kreuz PC, Steinwachs M, Erggelet C, Lahm A, Ghanem N, Uhl M (2007) Importance of sports in cartilage regeneration after autologous chondrocyte implantation: a prospective study with a 3-year follow-up. Am J Sports Med 35(8):1261–1268
Kreuz PC, Müller S, Ossendorf C, Kaps C, Erggelet C (2009) Treatment of focal degenerative cartilage defects with polymer-based autologous chondrocyte grafts: four-year clinical results. Arthritis Res Ther 11(2):R33
Kreuz PC, Müller S, Freymann U, Erggelet C, Niemeyer P, Kaps C, Hirschmüller A (2011) Repair of focal cartilage defects with scaffold-assisted autologous chondrocyte grafts: clinical and biomechanical results 48 months after transplantation. Am J Sports Med 39(8):1697–1705 Epub 2011 May 3
Kreuz PC, Müller S, Erggelet C, von Keudell A, Tischer T, Kaps C, Niemeyer P, Hirschmüller A (2012) Is gender influencing the biomechanical results after autologous chondrocyte implantation? Knee Surg Sports Traumatol Arthrosc 22(1):72–79
Kreuz PC, Müller S, von Keudell A, Tischer T, Kaps C, Niemeyer P, Erggelet C (2013) Influence of sex on the outcome of autologous chondrocyte implantation in chondral defects of the knee. Am J Sports Med 41(7):1541–1548
Lautamies R, Harilainen A, Kettunen J, Sandelin J, Kujala UM (2008) Isokinetic quadriceps and hamstring muscle strength and knee function 5 years after anterior cruciate ligament reconstruction: comparison between bone-patellar tendon- bone and hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc 16(11):1009–1016
Loken S, Ludvigsen TC, Hoysveen T, Holm I, Engebretsen L, Reinholt FP (2009) Autologous chondrocyte implantation to repair knee cartilage injury: ultrastructural evaluation at 2 years and long-term follow-up including muscle strength measurements. Knee Surg Sports Traumatol Arthrosc 17(11):1278–1288
Maffiuletti N, Bizzini M, Desbrosses K, Babault N, Munzinger U (2007) Reliability of knee extension and flexion measurements using the Con-Trex isokinetic dynamometer. Clin Physiol Funct Imaging 27(6):346–353
Mayer F, Horstmann T, Baurle W, Grau S, Hande M, Dickhuth HH (2001) Diagnostics with isokinetic devices in shoulder measurements—potentials and limits. Isokinet Exerc Sci 9:19–25
Mikkelsen C, Werner S, Eriksson E (2000) Closed kinetic chain alone compared to combined open and closed kinetic chain exercises for quadriceps strengthening after anterior cruciate ligament reconstruction with respect to return to sports: a prospective matched follow-up study. Knee Surg Sports Traumatol Arthrosc 8(6):337–342
Mueller S, Baur H, Konig T, Hirschmuller A, Mayer F (2007) Reproducibility of isokinetic single- and multi-joint strength measurements in healthy and injured athletes. Isokinet Exerc Sci 15:295–302
Nehrer S, Dorotka R, Domayer S, Stelzeneder D, Kotz R (2009) Treatment of full thickness chondral defects with hyalograft C in the knee: a prospective clinical case series with 2 to 7 years’ follow-up. Am J Sports Med 37(Suppl 1):81–87
Niemeyer P, Steinwachs M, Erggelet C, Kreuz PC, Kraft N, Köstler W, Mehlhorn A, Südkamp NP (2008) Autologous chondrocyte implantation for the treatment of retropatellar cartilage defects: clinical results referred to defect localisation. Arch Orthop Trauma Surg 128(11):1223–1231
Palmieri-Smith RM, Thomas AC (2009) A neuromuscular mechanism of posttraumatic osteoarthritis associated with ACL injury. Exerc Sport Sci Rev 37(3):147–153
Palmieri-Smith RM, Thomas AC, Wojtys EM (2008) Maximizing quadriceps strength after ACL reconstruction. Clin Sports Med 27(3):405–424
Peterson L, Vasiliadis HS, Brittberg M, Lindahl A (2010) Autologous chondrocyte implantation: a long-term follow-up. Am J Sports Med 38(6):1117–1124
Rehan Youssef A, Longino D, Seerattan R, Leonard T, Herzog W (2009) Muscle weakness causes joint degeneration in rabbits. Osteoarthr Cartil 17(9):1228–1235
Robertson WB, Fick D, Wood DJ, Linklater JM, Zheng MH, Ackland TR (2007) MRI and clinical evaluation of collagen-covered autologous chondrocyte Implantation (CACI) at two years. Knee 14(2):117–127
Slemenda C, Brandt KD, Heilman DK et al (1997) Quadriceps weakness and osteoarthritis of the knee. Ann Intern Med 127(2):97–104
Slemenda C, Heilman DK, Brandt KD, Katz BP, Mazzuca SA, Braunstein EM, Byrd D (1998) Reduced quadriceps strength relative to body weight: a risk factor for knee osteoarthritis in women? Arthritis Rheum 41(11):1951–1959
Trinh TQ, Harris JD, Siston RA, Flanigan DC (2013) Improved outcomes with combined autologous chondrocyte implantation and patellofemoral osteotomy versus isolated autologous chondrocyte implantation. Arthroscopy 29(3):566–574
Yoon TS, Park DS, Kang SW, Chun SI, Shin JS (1991) Isometric and isokinetic torque curves at the knee joint. Yonsei Med J 32(1):33–43
Acknowledgments
None of the authors received funding for this study, for the study design, for the collection, analysis and interpretation of data or for preparing the manuscript. The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Sebastian Müller and Peter C. Kreuz have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Müller, S., Hirschmüller, A., Erggelet, C. et al. Significantly worse isokinetic hamstring–quadriceps ratio in patellofemoral compared to condylar defects 4 years after autologous chondrocyte implantation. Knee Surg Sports Traumatol Arthrosc 23, 2151–2158 (2015). https://doi.org/10.1007/s00167-014-2964-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-2964-y