Abstract
Purpose
The influence of gender on the biomechanical outcome after autologous chondrocyte implantation (ACI) including isokinetic muscle strength measurements has not been investigated. The present prospective study was performed to evaluate gender-specific differences in the biomechanical function 48 months after ACI.
Methods
Fifty-two patients (mean age 35.6 ± 8.5 years) that met our inclusion criteria, underwent ACI with Bioseed C® and were evaluated with the KOOS score preoperatively, 6, 12 and 48 months after surgery. At final follow-up, 44 out of the 52 patients underwent biomechanical evaluation with isokinetic strength measurements of both knees. All data were evaluated separately for men and women and compared for each time interval using the Mann–Whitney U test.
Results
Clinical scores improved significantly over the whole study period (p < 0.05). Male patients demonstrated significantly better scores during the follow-up in the KOOS score (p < 0.05). Isokinetic strength measurements after 48 months revealed a significant strength deficit of the treated knee in all test modes compared to the healthy extremity (p < 0.05). Furthermore, male patients achieved significantly higher strength values compared to female patients (p < 0.05).
Conclusions
ACI is a viable treatment option for full-thickness chondral defects in the knee of both genders. Isokinetic muscle strength measures are significantly worse in women (p < 0.05), but physiological and may play a role for the explanation of gender-specific results after ACI.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Focal cartilage lesions of the knee are common and may increase the risk of progressive osteoarthritis [31]. The process includes the loss of proteoglycans and water in the extracellular matrix and the disruption of the collagenous fibrillar network therein, followed by cell metaplasia and cell loss [8, 14, 33]. Surgical treatment algorithms include marrow stimulation techniques such as microfracture or osteochondral autograft transplantation for small lesions [11, 20, 35]. Patients with large defects often fail these modalities and therefore should undergo autologous chondrocyte implantation (ACI) of the chondral defect [18, 19, 30, 37]. The presence of autogenous chondrocytes within the prepared defect area improves the formation of hyaline-like cartilage with a superior biomechanical quality and durability compared to the fibrocartilaginous fill of microfracture [18].
ACI has emerged as an effective and durable solution for the treatment of large full-thickness chondral lesions of the knee joint. Good clinical and functional outcomes remain stable even 10–20 years after the implantation [2, 27, 28].
Today, advanced techniques of ACI with scaffolds may avoid typical problems including periosteal hypertrophy, insufficient bonding and delamination, seen with the first classical technique using a periosteal membrane [22]. The cell carriers are composed of different biodegradable materials such as collagen gels or membranes, copolymers of polyglycolic/polylactic acid and polydioxanone, and hyaluronic acid [19, 21, 32, 36]. Biomechanical evaluations by isokinetic strength measurements have shown improvement in the postoperative follow-up; however, the surgically treated leg often remains significantly weaker [24]. The influence of gender on the biomechanical outcome after ACI has not been investigated. The present prospective study was performed to evaluate gender-specific differences in the biomechanical function 48 months after ACI with a cell-based fibrin polymer graft. The results of this study may help to develop gender-specific rehabilitation protocols after autologous chondrocyte implantation for a better clinical and functional outcome.
Materials and methods
Between 2001 and 2004, we enrolled 52 patients (27 male, 25 females) with full-thickness chondral defects in the knee in a prospective study. All subjects were treated with Bioseed C, a second-generation ACI tissue engineering cartilage graft that is based on autologous chondrocytes embedded in a three-dimensional bioresorbable two-component gel-polymer scaffold. Inclusion criteria were age between 18 and 55 years with single isolated symptomatic full-thickness chondral defects grade III B, C according to the ICRS-classification system [1]. We included lesions extending down to the calcified layer (IIIB) but not through the subchondral bone plate (IIIC). Minimum size defect was 2 cm2 and had to be localized in only one of the 3 knee compartments (medial femoro-tibial joint, lateral femoro-tibial joint or femoro-patellar joint). Varus or valgus deformities >5° were addressed with additional osteotomy, and ligament instabilities were reconstructed. Exclusion criteria consisted of the presence of chronic inflammatory arthritis, osteochondral defects, limits in knee extension or flexion less 130°, prior or planned meniscectomy (>30 % of meniscus), BMI > 30 kg/m2, osteochondral defects, drug treatment for osteoarthritis, intra-articular corticosteroid injections within the previous month or knee arthroscopy within the previous 6 months, osteoarthritis and chondrocalcinosis.
This prospective study investigated gender-dependent differences in the clinical and biomechanical results after ACI. Furthermore, correlation between clinical and biomechanical data should give information about the importance of muscle strength as potential prognostic parameter after ACI in men and women.
Each patient was evaluated with the Knee Injury and Osteoarthritis Outcome Score [29] at 6, 12 and 48 months after surgery by an orthopaedic surgeon. Varus or valgus deformities were detected by long leg X-ray, and correct patella position was evaluated by a routine medio-lateral, femoro-patellar and axial joints radiograph.
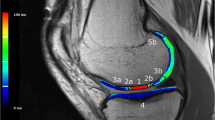
Forty-four (25 males, 19 females) out of the 52 patients gave consent for additional biomechanical evaluation of the treated knee 48 months after surgery. The details of both genders appear in Table 1. Isokinetic testing of maximum strength was conducted in concentric and eccentric test modes (60°/s) with an isokinetic dynamometer (Con-Trex MJ Multi-joint Module, CMV AG, Dübendorf, Switzerland). After a 5-min bicycle warm-up period, quadriceps and hamstring strength capacities were measured in Newton-metres during reciprocal knee flexion and extension of both knees [21]. The level of pain during isokinetic strength measurement was detected for all patients on a numeric scale (no pain: 0 points; maximum pain: 10 points).
Surgical technique
After evaluation of the chondral defect, 250 mg of the patient’s healthy cartilage was harvested arthroscopically from a less weight-bearing area of the knee. The cells were cultivated for 6 weeks, seeded on a scaffold and subsequently implanted in the cartilage defect during a second procedure. Depending on the lesion location, a medial or lateral mini-open parapatellar skin incision was made. The lesion was exposed and debrided carefully to normal surrounding articular cartilage. The defect size was measured and the chondrocyte-containing fleece tailored correspondingly. Fixation of the scaffold was performed in each corner with Vicryl sutures with attached knots, pulled into predrilled bone channels with a Kirschner wire. The knots serve as bone anchors and fix the graft within the prepared defect area [6]. Before wound closure, a drain was placed into the joint.
Rehabilitation
The patients were hospitalized for an average of 5 days. On the first postoperative day, the knee joints were subjected to cold therapy and continuous passive motion (CPM) for 6–8 h per day. For femoral defects, range of motion was limited to 90° for 6 weeks. For chondral lesions in the femoro-patellar compartment, flexion was limited with a brace for 2 weeks to 30°, for another 2 weeks to 60° and until the 6th week after surgery to 90°. For 6 weeks, only crutch-assisted touchdown weight-bearing was allowed. At 7–12 weeks after surgery, patients gradually increased the loading and performed specific strengthening exercises, active physiotherapy. Full weight-bearing was allowed after 3 months, low impact sports after 6 months and contact sports (such as tennis or football) after 9–12 months.
Statistical analysis
Descriptive statistics during follow-up (arithmetic mean, standard deviation, range) were calculated using standard formulas. The clinical results were evaluated during the follow-up period by paired Wilcoxon-tests and Friedman-tests for the KOOS score. The Mann–Whitney U test for non-parametric data was used to compare gender-specific clinical results at each time interval and to compare the four-year postoperative isokinetic strength measurements of the concentric and eccentric test modes between men and women. Pearson’s correlation coefficients were calculated to analyse the association between biomechanical data and clinical scores. All statistics were performed with SPSS 18 (Chicago, Illinois) and reviewed by an independent statistician. A p value <0.05 was considered significant.
Results
Preoperative patient evaluation revealed lower values in the KOOS score in women compared to men (p < 0.05). The differences were not significant in the KOOS subgroup symptoms (Fig. 1). The period of preoperative symptoms, the average age, the BMI and the number of patients did not differ significantly between both genders (Table 1). There was a significant improvement in clinical outcome scores pre- and postoperatively at the final follow-up for both genders (p < 0.05) (Fig. 1). Male patients achieved better clinical results at every time of follow-up than female patients except in the KOOS subgroup “Quality of Life” (QoL): women had higher outcome scores after 48 months, however, without any significant difference to males.
Gender-specific results in the KOOS score preoperative, 6, 12 and 48 months after implantation of Bioseed C. An asterisk/rhomb (*for men, # for women) shows significant improvement (p < 0.05) compared to the last time-interval. Furthermore, significant differences (p < 0.05) between males and females are shown for all KOOS subgroups with a bar at each follow-up period. Overall, male patients achieved in all groups better clinical results at every time of follow-up. The gender-specific differences were significant (p < 0.05) in the KOOS subgroups pain and symptoms 6 months after surgery and in the subgroups ADL, sports and QoL at 12 months postoperative
The gender-specific differences were significant in the KOOS subgroups “pain” and “symptoms” 6 months after surgery and in the subgroups “ADL” and “QoL” at 12 months postoperative (Fig. 1).
Isokinetic strength measurements after 48 months revealed for both genders a persisting significant strength deficit of the operated extensor and flexor muscles in all test modes compared to the healthy extremity (p < 0.05) (Table 2a, b). Gender-dependent data evaluation revealed significantly higher strength values in the male group 48 months after surgery (p < 0.05). Single exception was the concentric mode of the extensors of the treated knee, where no gender-dependent differences could be found (n.s.). Almost no patient reported having pain during isokinetic strength measurement. Numerical pain scaling revealed 0.8 points (range 0–2) for men and 0.4 points (range 0–2) for women (n.s.).
There was no significant correlation between clinical scores and isokinetic measurements in all eccentric test modes (Table 3). In contrast, significant correlation could be found between the KOOS subgroup “sports” and the operated knee in the concentric test mode for flexors and extensors (p < 0.05). The other KOOS subgroups showed no significant correlation with the isokinetic values. The strength values of the healthy knee showed no significant correlation with the clinical scores.
Discussion
The most important finding of the present study was the gender-specific clinical and biomechanical differences even 48 months after ACI. Twenty-five male and 19 female patients were investigated clinically and biomechanically by isokinetic measurement of the maximum strength of the knee flexors and extensors at 48-month follow-up using the Contrex multi-joint dynamometer. Clinical evaluation revealed that 6 and 12 months postoperatively men had significantly better clinical outcome scores than women (p < 0.05). During the postoperative follow-up period, both genders improved in the time intervals between preoperative to 6 months, 6–12 months and 12–48 months after surgery (p < 0.05). However, women never reached the same amount of clinical outcome scores, but men did up to 4 years after index surgery.
A randomized controlled trial comparing microfracture and ACI has shown that female patients had more failures irrespective of the treatment and that ACI resulted in better outcome in participants with time since symptom onset less than 3 years, which was statistically significant and clinically relevant [30, 37]. In our patient group, preoperative duration of symptoms was on average 13 months longer in women compared to men, but in both genders, endured symptoms for more than 4 years before undergoing ACI surgery. Therefore, we do not believe that the gender-dependent differences in the duration of preoperative symptoms may influence the clinical results and the muscle strength before ACI procedures. Furthermore, we have a long study period of 4 years for comparable clinical recovery, muscle adaptation and graft hyalinization in both groups. Moreover, the defect size was significantly larger in men compared to women (p < 0.05) which would suggest worse results in final outcome.
Biomechanical evaluation comparing the healthy knee with the treated knee of each patient revealed significantly (p < 0.05) higher maximum strength values of the healthy knee in all test modes. Significant correlation (p < 0.05) between the concentric strength values and the KOOS subgroup sports was detected only in the treated, but not in the healthy knee. Possibly, the questionnaires were biased due to the fact of asking specifically for symptoms or limitations with the treated extremity and therefore excluding the contralateral side.
Men reached significantly higher peak torques in both knees (p < 0.05) compared to women. However, the significant differences between both genders in the operated as well as in the healthy knee indicate that the muscle force differences are physiological between men and women. Gender differences in absolute muscle strength are well documented. Studies have shown that men generally have larger and stronger muscles than women, who reach about 70 % of the force compared to their male counterparts [26]. Women reach the maximum strength between 14 and 18 years, men with 20 years. After 30 years, the muscle strength declines gradually [26]. Active musculoskeletal stiffness is an important factor in joint stability and protection of cartilage during regeneration and in preventing further injury. Biomechanical studies on cadaver limbs with dynamic measurements simulating knee flexion and rotation have shown that loading of the knee with balanced hamstrings and quadriceps reduces tibial rotation and translation compared to the passive condition [38]. In a spring-mass oscillating model, leg-stiffness values were significantly greater (p < 0.01) in men compared to women at different hopping frequencies [9]. The data are supported by the study by Wojtys et al. who tested the hypothesis that women are able to volitionally increase the apparent torsional stiffness of the knee, by maximally activating the knee muscles, significantly less than are men participating in the same type of sport. For this purpose, a medially directed 80N-impulse force was applied to the lateral aspect of the forefoot. They found that maximal rotations of the leg were greater in women than in men (p < 0.05) and that female athletes exhibited less muscular protection of the knee during external loading (p < 0.05) [39]. These results demonstrate less leg-stiffness and knee joint stabilization with a higher risk of musculoskeletal knee injury in women. However, knee stability is crucial for the maturation of the soft newly formed tissue after ACI. Overloading of the graft is detrimental; since hyaline-like cartilage does not reach the composition of intact hyaline cartilage [27], it is thought to take years to reach full maturation. Brun et al. reported in second- and third-look biopsies taken at 18 months postoperatively a continuous maturation process of the newly formed tissue [3]. Gikas et al. demonstrated that with doubling of the time after implantation, the histological outcome was increased by more than fourfold (p < 0.001) [7].
A further gender-specific problem after ACI may lie in the postoperative recovery. The preoperative period of constricted use of the lower extremity due to pain in addition to the postoperative period of limb immobilization and partial weight-bearing may contribute to overall deconditioning. Studies have shown that a reduction in muscle usage can evoke marked adaptations in the neuromuscular system. However, it has been reported that recovery is impeded, especially in women [34]. This could cause an overloading of the newly formed cartilage during the maturation process. To our knowledge, no study has investigated gender-specific histological results after ACI. Incidental reports from basic science research have pointed towards the influence of estrogens on chondral differentiation and matrix production. In this context, experiments with cell cultures have shown a suppression of chondrogenesis by estradiol via membrane-associated E2 receptors with smaller aggregates and significantly lower type II collagen and sGAG content after treatment with E2 in a dose-dependent manner [15]. Further studies have shown that estrogens are able to directly affect the cell population kinetics as well as proliferation and differentiation of growth plate cells and cause apoptosis in male and female resting zone and growth zone chondrocytes in a dose-dependent manner, based on elevated DNA fragmentation [40]. Estrogens appear to have the ability to reduce the longitudinal bone growth and the final height of an individual and aromatase inhibitors, which blocks the conversion of androgens to estrogens, are used in the treatment of children with familial/genetic short stature, constitutional growth delay or idiopathic short stature [5, 17]. All these results support the hypothesis that estrogens could impede cartilage maturation and matrix production after ACI.
A few reports described significant gender-dependent differences in the outcome after different techniques for cartilage repair. A recently published cohort study with 413 patients following first, second and third generation ACI revealed the female gender as one of the prognostic factors associated with a significantly higher risk for reintervention (p = 0.033) [16]. Similar results were detected in a randomized controlled trial 5 years after ACI with characterized chondrocytes with a higher failure rate in female compared to male patients (p = 0.007) [37].
In conclusion, gender-dependent differences in hormones, neuromuscular coordination and muscle strength could explain better clinical results after ACI in men compared to women. Imbalances of muscle groups and neuromuscular factors appear to be also the most important reason for the higher risk of anterior cruciate ligament (ACL) injuries in women that exceeds their male counterparts by 2–8 times [12]. Studies have shown that neuromuscular control and valgus loading of the knee predicts the ACL injury risk in female athletes [10, 13]. In consequence, the Prevent Injury and Enhance Performance (PEP) programme with comprehensive and proprioceptive training was introduced and could significantly reduce the incidence of ACL tears in female athletes [25]. It remains unclear whether gender-specific programmes could improve the clinical results after ACI in women studies on male athletes have shown that intensive ACI rehabilitation including neuromuscular training allows a faster return to competition and also influences positively the clinical outcome at medium-term follow-up [4].
Furthermore, continuous physical training improves long-term results after ACI of the knee and should be carried out for at least 2 years after surgery [23]. Limitations of our clinical and biomechanical study include the lack of neuromuscular examinations pre- and postoperatively and serial biomechanical data over the whole study period. Biomechanical evaluation was performed 4 years after the surgery. However, given the amount of follow-up, all patients should have enough time for a comparable recovery, training and muscle adaptation. Furthermore, pain evaluation on a numerical scale during the biomechanical investigations showed negligible values under 1 without any significant difference between men and women. Therefore, we conclude that muscle strength measurement was not influenced by clinical symptoms. In summary, we were able to demonstrate that there is a significant gender-specific clinical and biomechanical difference up to 48 months after ACI surgery. Our clinical results support the theory that especially female patients could profit from a special postoperative rehabilitation programme. This programme should focus on strengthening the quadriceps and on balancing the extensor and flexor forces of the upper thigh.
Conclusion
ACI is a viable treatment option for full-thickness chondral defects in the knee of men and women. Isokinetic muscle strength measures are significantly worse in women (p < 0.05) and may play a role for the explanation of gender-specific results after ACI. Our data support the development of rehabilitation protocols with special focus on balancing the forces of the extensor and flexor muscles of the knee. Further clinical studies are necessary to investigate the potential improvements of special intensive muscular and proprioceptive training in clinical outcome after ACI in the female knee.
References
Aglietti A, Gambardella R, Hangody L et al (2000) http://www.cartilage.org/_files/contentmanagement/ICRS_evaluation.pdf
Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L (1994) Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med 331(14):889–895
Brun P, Dickinson SC, Zavan B, Cortivo R, Hollander AP, Abatangelo G (2008) Characteristics of repair tissue in second-look and third-look biopsies from patients treated with engineered cartilage: relationship to symptomatology and time after implantation. Arthrits Res Ther 10(6):R132
Della Villa S, Kon E, Filardo G, Ricci M, Vincentelli F, Delcogliano M, Marcacci M (2010) Does intensive rehabilitation permit early return to sport without compromising the clinical outcome after arthroscopic autologous chondrocyte implantation in highly competitive athletes? Am J Sports Med 38(1):68–77
Dunkel L (2006) Use of aromatase inhibitors to increase final height. Mol Cell Endocrinol 25:207–216
Erggelet C, Kreuz PC, Mrosek EH, Schagemann JC, Lahm A, Ducommun PP, Ossendorf C (2010) Autologous chondrocyte implantation versus ACI using 3D-bioresorbable graft for the treatment of large full-thickness cartilage lesions in the knee. Arch Orthop Trauma Surg 130(8):957–964
Gikas PD, Morris T, Carrington R, Skinner J, Bentley G, Briggs T (2009) A correlation between the timing of biopsy after autologous chondrocyte implantation and the histological appearance. J Bone Joint Surg 91-B:1172–1177
Goldring MB, Goldring SR (2007) J Cell Physiol. Osteoarthritis 213(3):626–634
Granata KP, Padua DA, Wilson SE (2002) Gender differences in active musculoskeletal stiffness. Part II. Quantification of leg stiffness during functional hopping tasks. J Electromoyogr Kinesiol 12(2):127–135
Griffin LY, Albohm MJ, Arendt EA et al (2006) Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt valley II meeting, January 2005. Am J Sports Med 34(9):1512–1532
Gudas R, Kalesinskas RJ, Kimtys V, Stankevicius E, Toliusis V, Bernotavicius G, Smailys A (2005) A prospective randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint in young athletes. Arthroscopy 21(9):1066–1075
Harmon KG, Ireland ML (2000) Gender differences in noncontact anterior cruciate ligament injuries. Clin Sports Med 19:287–302
Hewett TE, Myer GD, Ford KR, Heidt RS Jr, Colosimo AJ, McLean SG, van den Bogert AJ, Paterno MV, Succop P (2005) Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med 33:492–501
Hunziker EB (2002) Articular cartilage repair: basic science and clinical progress. A review of the current status and prospects. Osteoarthritis Cartilage 10:432–463
Jenei-Lanzl Z, Straub RH, Dienstknecht T, Huber M, Hager M, Grässel S, Kujat R, Angele MK, Nerlich M, Angele P (2010) Estradiol inhibits chondrogenic differentiation of mesenchymal stem cells via nonclassic signaling. Arthritis Rheum 62(4):1088–1096
Jungmann PM, Salzmann GM, Schmal H, Pestka JM, Südkamp NP, Niemeyer P (2012) Autologous chondrocyte implantation for treatment of cartilage defects of the knee: what predicts the need for reintervention? Am J Sports Med 40(1):58–67
Karimian E, Sävendahl L (2011) Estrogen signaling in growth plate cartilage. Endocr Dev 21:42–51
Knutsen G, Drogset JO, Engebretsen L, Grontvedt T, Isaksen V, Ludvigsen TC, Roberts S, Solheim E, Strand T, Johansen O (2007) A randomized trial comparing autologous chondrocyte implantation with microfracture. Findings at five years. J Bone Joint Surg Am 89(10):2105–2112
Kon E, Filardo G, Berruto M, Benazzo F, Zanon G, Della Villa S, Marcacci M (2011) Articular cartilage treatment in high-level male soccer players: a prospective comparative study of arthroscopic second-generation autologous chondrocyte implantation versus microfracture. Am J Sports Med 39(12):2549–2557
Kreuz PC, Erggelet C, Steinwachs MR, Krause SJ, Lahm A, Niemeyer P, Ghanem N, Uhl M, Südkamp N (2006) Is microfracture of chondral defects in the knee associated with different results in patients aged 40 years or younger? Arthroscopy 22(11):1180–1186
Kreuz PC, Müller S, Freymann U, Erggelet C, Niemeyer P, Kaps C, Hirschmüller A (2011) Repair of focal cartilage defects with scaffold-assisted autologous chondrocyte grafts: clinical and biomechanical results 48 months after transplantation. Am J Sports Med 39(8):1697–1705
Kreuz PC, Steinwachs M, Erggelet C, Krause SJ, Ossendorf C, Maier D, Ghanem N, Uhl M, Haag M (2007) Classification of graft hypertrophy after autologous chondrocyte implantation of full-thickness chondral defects in the knee. Osteoarthritis Cartilage 15(12):1339–1347
Kreuz PC, Steinwachs M, Erggelet C, Lahm A, Krause S, Ossendorf C, Meier D, Ghanem N, Uhl M (2007) Importance of sports in cartilage regeneration after autologous chondrocyte implantation: a prospective study with a 3-year follow-up. Am J Sports Med 35(8):1261–1268
Loken S, Ludvigsen T, Hoysveen T, Holm I, Engebretsen L, Reinholt FP (2009) Autologous chondrocyte implantation to repair knee cartilage injury: ultrastructural evaluation at 2 years and long-term follow-up including muscle strength measurements. Knee Surg Sports Traumatol Arthrosc 17:1278–1288
Mandelbaum BR, Silvers HJ, Watanabe DS, Knarr JF, Thomas SD, Griffin LY, Kirkendall DT, Garrett W (2005) Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med 33(7):1003–1010
Miller AEJ, MacDougall JD, Tarnopolsky MA, Sale DG (1993) Gender differences in strength and muscle fiber characteristics. Eur J Appl Physiol 66:254–262
Peterson L, Brittberg M, Kiviranta I, Akerlund EL, Lindahl A (2002) Autologous chondrocyte transplantation: biomechanics and long-term durability. Am J Sports Med 30(1):2–12
Peterson L, Vasiliadis HS, Brittberg M, Lindahl A (2010) Autologous chondrocyte implantation: a long-term follow-up. Am J Sports Med 38(6):1117–1124
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD (1998) Knee Injury and Osteoarthritis Outcome Score (KOOS)-development of a self-administered outcome measure. J Orthop Sports Phys Ther 28(2):411–418
Saris D, Vanlauwe J, Victor J, Almqvist KF, Verdonk R, Bellemans J, Luyten FP, TIG/ACT/01/2000&EXT study group (2009) Treatment of symptomatic cartilage defects of the knee: characterized chondrocyte implantation results in better clinical outcome at 36 months in a randomized trial compared to microfracture. Am J Sports Med 37(Suppl 1):10S–19S
Schinhan M, Gruber M, Vavken P, Dorotka R, Samouh L, Chiari C, Gruebl-Barabas R, Nehrer S (2012) Critical-size defect induces unicompartmental osteoarthritis in a stable ovine knee. J Orthop Res 30(2):214–220
Schneider U, Rackwitz L, Andereya S, Siebenlist S, Fensky F, Reichert J, Läer I, Barthel T, Rudert M, Nöth U (2011) A prospective multicenter study on the outcome of type I collagen hydrogel-based autologous chondrocyte implantation (CaReS) for the repair of articular cartilage defects in the knee. Am J Sports Med 39(12):2558–2565
Schroeppel JP, Crist JD, Anderson HC, Wang J (2011) Molecular regulation of articular chondrocyte function and its significance in osteoarthritis. Histol Histopathol 26(3):377–394
Semmler JG, Kutzscher DV, Enoka RM (1999) Gender differences in the fatigability of human skeletal muscle. J Neurophysiol 82:3590–3593
Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ, Rodkey WG (2003) Outcomes of microfracture for traumatic chondral defects of the knee: average 11-year follow-up. Arthroscopy 19:477–484
Steinwachs M, Kreuz PC (2007) Autologous chondrocyte implantation in chondral defects of the knee with a type I/III collagen membrane: a prospective study with a 3-year follow-up. Arthroscopy 23(4):381–387
Vanlauwe J, Saris DB, Victor J, Almqvist KF, Bellemans J, Luyten FP, TIG/ACT/01/2000&EXT study group (2011) Five-year outcome of characterized chondrocyte implantation versus microfracture for symptomatic cartilage defects of the knee: early treatment matters. Am J Sports Med 39(12):2566–2574
Victor J, Labey L, Wong P, Innocenti B, Bellemans J (2010) The influence of muscle load on tibiofemoral knee kinematics. J Orthop Res 28(4):419–428
Wojtys EM, Huston LJ, Schock HJ, Boylan JP, Ashton-Miller JA (2003) Gender differences in muscular protection of the knee in torsion in size-matched athletes. J Bone Joint Surg 85(5):782–789
Zhong M, Carney DH, Boyan BD, Schwartz Z (2011) 17ß-estradiol regulates rat growth plate chondrocyte apoptosis through a mitochondrial pathway not involving nitric oxide or MAPKs. Endocrinology 152(1):82–92
Acknowledgments
No financial support of this project has occurred. The authors have received nothing of value. This manuscript does not contain information about medical devices.
Author information
Authors and Affiliations
Corresponding author
Additional information
Peter C. Kreuz and Sebastian Müller contributed equally to the work.
Rights and permissions
About this article
Cite this article
Kreuz, P.C., Müller, S., Erggelet, C. et al. Is gender influencing the biomechanical results after autologous chondrocyte implantation?. Knee Surg Sports Traumatol Arthrosc 22, 72–79 (2014). https://doi.org/10.1007/s00167-012-2280-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-2280-3