Abstract
We hypothesized changes in rotations and translations after TKA with a fixed-bearing anterior cruciate ligament (ACL)-sacrificing but posterior cruciate ligament (PCL)-retaining design with equal-sized, circular femoral condyles would reflect the changes of articular geometry. Using 8 cadaveric knees, we compared the kinematics of normal knees and TKA in a standardized navigated position with defined loads. The quadriceps was tensed and moments and drawer forces applied during knee flexion-extension while recording the kinematics with the navigation system. TKA caused loss of the screw-home; the flexed tibia remained at the externally rotated position of normal full knee extension with considerably increased external rotation from 63° to 11° extension. The range of internal-external rotation was shifted externally from 30° to 20° extension. There was a small tibial posterior translation from 40° to 90° flexion. The varus-valgus alignment and laxity did not change after TKA. Thus, navigated TKA provided good coronal plane alignment but still lost some aspects of physiologic motion. The loss of tibial screw-home was related to the symmetric femoral condyles, but the posterior translation in flexion was opposite the expected change after TKA with the PCL intact and the ACL excised. Thus, the data confirmed our hypothesis for rotations but not for translations. It is not known whether the standard navigated position provides the best match to physiologic kinematics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The long-term results of TKA have been favorable in terms of implant survival; some studies [17, 43, 44] have reported greater than 90% survival at 10 to 15 years. However, this gives no indication of the patient’s subjective impression of function, and several studies have reported dissatisfaction rates of 20% to 40% [1, 15, 29]. Dissatisfaction may be explained partly by abnormal kinematics affecting muscle moment arms and sensations of instability. The advent of Roentgenstereophotogrammetric analysis and videofluoroscopy has enhanced our ability to describe these kinematics.
Uvehammer et al. used Roentgenstereophotogrammetric analysis in vivo to show cruciate-retaining and -sacrificing designs exhibited abnormal kinematics when compared with controls [40–42]. They reported all designs had increased femoral anterior translation with flexion when compared with the normal knee and that there was abnormal tibial anteroposterior (AP) motion with knee extension.
Single-plane fluoroscopy has further enhanced understanding and various studies have shown normal kinematics are lost after TKA [2, 4, 6, 25, 31, 38]. Banks and Hodge [3] found a closer reproduction of normal knee kinematics with posterior cruciate-sacrificing designs with an average medial center of axial rotation during knee extension from flexion. After cruciate-retaining TKA, the average center of rotation was displaced lateral to the center of the tibia; this was associated with paradoxic medial femoral condylar roll-forward with flexion for some designs. Wimmer and Andriacchi [46] noted abnormal tractive-rolling forces are generated at the articular interface after TKA because the coefficient of friction (μ) of artificial joints (μ = 0.03–0.10 [16]) is higher than in the natural joint (μ = 0.002–0.03 [14]). This phenomenon also may induce abnormal kinematics by altering the normal rolling/sliding behavior.
The properties of the implants and the nonanatomic shape of their articulations suggest normal knee kinematics are unlikely to be replicated. Erratic stick-slip behavior (the femoral component suddenly sliding forward over the tibia when the expected physiologic motion should be progressive roll-back) arising from the raised friction [46] may partly explain patient perceptions after TKA. However, the unpredictability of knee kinematics after TKA [39] may, at least partly, result from variability in component positioning and the resulting effects on soft tissue behavior [5, 7, 8]. Prior studies have been unable to account for that variability, because they did not document implant positions and measure the kinematics after surgery. The introduction of computer assistance to TKA allows more precise positioning relative to predefined axes that are based on current knowledge and guidelines, reducing variability from the desired alignment [11] and so reducing the shortcomings of earlier methods.
One would anticipate that even with carefully navigated component alignment, TKAs would still cause changes in the path of motion and joint laxity, particularly tibial internal-external and varus-valgus rotations, plus anterior-posterior translations, across the range of knee flexion-extension. For example, take a femoral component with equal medial and lateral fixed radii of curvature in the sagittal plane and a tibial bearing surface that is only partially conforming but with the same sagittal plane geometry medially and laterally. Given the putative accuracy of a navigation system balancing the ligaments, we presume the kinematic changes primarily would be attributable to the articular geometry and secondarily to the loss of the ACL.
We formulated three hypotheses: (1) The design features noted above would inhibit tibial internal-external rotation during knee flexion-extension motion, giving motion more compatible with a fixed axis; (2) Internal-external rotation and varus-valgus laxity would not be changed substantially across the arc of knee flexion-extension; and (3) The normal AP tibiofemoral relationship would not be maintained after TKA, specifically excision of the ACL would result in anterior subluxation under drawer testing and larger than normal AP laxity during flexion-extension motion.
Materials and Methods
We measured natural knee kinematics and laxity across the range of knee flexion-extension for several loading conditions: active knee extension, AP drawer, internal-external rotation, and varus-valgus moments. We then repeated the measurements after TKA so paired comparisons could be made to find changes.
We obtained 10 adult fresh-frozen disarticulated limbs in conformity with local legal requirements. We used two limbs in developing this method, leaving eight knees for analysis unless specified otherwise. A post hoc power analysis indicated that, with the standard deviations calculated, we could detect changes of 6 mm or 11° with 80% power at the 95% level. All were left-sided, had normal alignment, and no evidence of gross arthritic changes, ligamentous instability, or previous surgery. Navigation trackers (Stryker Knee Navigation System; Stryker Leibinger, Freiburg, Germany) were fixed securely to the outer cortices of the femora and tibiae 150 mm from the joint line. For each specimen, we recorded the position of standard navigation reference points at the center of the femoral head and ankle. The legs were divided 200 mm above and below the joint line and mounted in a dedicated loading rig with the transepicondylar axis aligned approximate to the flexion-extension axis of the rig [12] (Fig. 1). The rig allowed unconstrained tibial motion relative to the femur, apart from control of flexion-extension, so the knee did not need its axis of flexion aligned to that of the test rig; the axis alignment had no effect on the relative tibiofemoral motions that were calculated only between the two bone-mounted motion trackers. The tibia hung free, allowing flexion-extension of the knee (0°–120°) by moving the femur in an approximate vertical arc and applying displacing loads to the quasistatic tibia [18].
To obtain active knee extension, we applied a quadriceps tension of 200 N to the patella through a cable attached to a pneumatic cylinder acting parallel to the femoral axis. This tension was limited by the fragility of the specimens from elderly cadavers; it was sufficient to ensure tibiofemoral joint compression through the range of motion (ROM). Tibial internal-external rotation moments of 5 Nm could be applied by hanging weights on two cords that pulled in opposite directions and were attached at the opposite sides of a large pulley connected to an intramedullary rod in the distal tibia. This induced tibial rotation without causing a resultant translation force and has been used in similar work [18]. Similarly, we applied tibial varus-valgus moments of 3.5 Nm using a cord-pulley system pulling medially or laterally on the distal end of the intramedullary rod. Anteroposterior forces of 70 N were applied to the proximal tibia through a low-friction bearing on a hoop so the resultant force was always through the center of the tibial plateau and secondary rotations were not inhibited. The displacing forces and moments were chosen to reflect those imposed during clinical examination of joint laxity, again with limits imposed by the fragility of the specimens; clinical anterior drawer tests often use 89 N force [13]. We then extended and flexed the femur by hand, with and against the quadriceps action, with each motion cycle taking approximately 5 seconds. This rate of motion allowed collection of sufficient kinematic data points.
The navigation system recorded the movements of the femur and tibia of the intact knee during active knee extension motion from 90° to 0° for the following loading conditions: internal rotation moment (5 Nm), external rotation moment (5 Nm), anterior drawer (70 N), posterior drawer (70 N), varus moment (3.5 Nm), valgus moment (3.5 Nm), and neutral (no additional loading other than the simulated extensor load).
We then inserted a Scorpio CR (Stryker Orthopaedics, Mahwah, NJ) posterior cruciate-retaining prosthesis in a classic standardized alignment [21]. This implant was widely used and linked to a navigation system that would allow accurate implant positioning and measurement of kinematics. The implant had design features that were expected to affect the kinematics and laxity of the knee. The femoral component had equal-sized medial and lateral condyles that had a fixed radius of curvature in the sagittal plane; the tibial bearing surface was partially conforming and had the same sagittal plane geometry medially and laterally. The distal femur was cut perpendicular to the computer estimation of the mechanical axis in coronal and sagittal planes; the resection was 0 to 1 mm deeper than the thickness of the distal part of the femoral component. We determined the rotation of the femoral component according to Berger et al. [9]. The final cuts were made after ensuring accurate AP positioning with the navigation. We cut the tibia perpendicular to its mechanical axis. The resection level matched the thickness of the insert, and the rotational alignment was referenced using the PCL and medial one-third of the tibial tuberosity. We cemented the tibial component and the femoral component was press fit. The arthrotomy was closed in the same manner as in clinical practise with Number 1 Vicryl (Ethicon, Somerville, NJ) to fascial layers and 2–0 Vicryl to fat and skin. We repeated the kinematic measures for the same conditions as the intact knee.
Kinematics data were described with six degrees of freedom according to the Grood and Suntay joint coordinate system [19] without adjustment for clinical abduction-adduction. Flexion-extension was a tibial rotation about the digitized femoral epicondylar axis [9]; internal-external rotation was about the long axis of the tibia, the zero point of which was defined by the relative position of the malleolar mediolateral axis and the femoral epicondylar axis; and varus-valgus motion (change of alignment in the coronal plane is, mechanically, a rotation) was about a floating axis mutually perpendicular to the other two axes in the AP direction [19]. We measured translations along these axes; only AP translation is presented. Care was taken to define the centers of the hip, knee, and ankle to minimize crosstalk, which is an inaccuracy in the calculated kinematics arising from misalignment of coordinates [33]; the center of the femoral head was known; the center of the knee was defined as the highest point of the anterior-distal outlet of the intercondylar notch; and the center of the ankle was the midpoint of a line joining the malleoli. The average of three extension cycles over the range 90° to 0° was used for analysis.
We used paired two-way t-tests to compare the neutral paths of motion and the joint laxity with the knee in two states: without and with the TKA, and across the range of knee flexion-extension. The dependent variables were the primary motions of the knee, ie, tibial AP translation, tibial internal-external rotation, or tibial varus-valgus angulation. We did not analyze coupled motions. When describing the difference between intact and TKA implanted knees, the 95% confidence interval bands of this difference were calculated and plotted in the graphs of results. Data relating to each of the hypotheses (tibial internal-external rotation, varus-valgus rotation, and AP translation) were calculated for the neutral path of motion and the limits of laxity, across the range of knee flexion-extension, and at the forces or moments applied (sometimes known as the envelope of laxity [10]). The neutral path of motion was that followed by the tibia when the knee extended with only the specimen weight and quadriceps tension acting.
Results
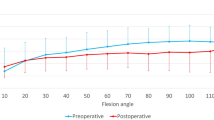
When the intact knee extended from 25° flexion to full extension, the tibia rotated externally by a mean of 8°; this was the screw-home mechanism. After TKA, there was almost no tibial rotation as the knee extended (Fig. 2). The tibia was in the same mean rotation after TKA as it had been when the intact knee was externally rotated after the screw-home in extension. After TKA, the tibia was rotated more externally (0.003 ≤ p < 0.05) than the intact knee had been over the extension range of 63° to 11°.
Comparison of the internal-external rotation pathways of the natural and prosthetic knees shows that the screw-home mechanism was abolished by the prosthesis. (A) The neutral pathway of tibial internal-external rotation for the intact knee (n = 8, ±standard deviation), and (B) the neutral pathway of tibial internal-external rotation after TKA implantation (n = 8, ±95% confidence interval of the difference between intact and TKA) are shown. Considerable differences are indicated with the bracket.
The tibial internal-external rotation laxity for the intact and post-TKA knees reduced progressively as the knee extended (Fig. 3). For the intact knee, both limits of the rotational laxity envelope moved into tibial external rotation in terminal knee extension, similar to the screw-home motion. Because the screw-home was lost after TKA, the limits of internal and external rotation laxity after TKA were more externally rotated than for the intact knee: for external rotation, 0.026 ≤ p < 0.05 from 32° to 14° knee extension, and for internal rotation, 0.007 ≤ p < 0.05 from 41° to 20° extension (Fig. 3).
Comparison of the ranges of internal-external rotation of the natural and prosthetic knees shows that, although the range of laxity was maintained, it was shifted by the loss of the screw-home mechanism after TKA, reflecting the loss of the screw-home. (A) Tibial internal-external rotation envelope of laxity for the intact knee (n = 8, ±standard deviation), and (B) tibial internal-external rotation envelope of laxity after TKA implantation (n = 8, ±95% confidence interval of the difference between intact and TKA) are shown. Differences are indicated with the brackets.
Neither the neutral pathway nor the limits of laxity of tibial varus-valgus motion was changed (p > 0.05) by TKA (Figs. 4, 5). On average, the neutral paths of the tibiae were aligned within 1° to the mechanical axis over the full ROM examined. However, the large confidence intervals of the difference between the normal and implanted knees show some had a large difference from average behavior. Data for one knee were lost in the varus-valgus loading condition, therefore, data for seven are presented here.
Implantation of the prosthesis did not affect the mean varus-valgus alignment of the knee; the large CI indicates that some knees had motion differing from the mean. (A) The neutral pathway of tibial varus-valgus angle for the intact knee (n = 7, ±standard deviation), and (B) the neutral pathway of tibial varus-valgus angle after TKA implantation (n = 7, ±95% confidence interval of the difference between intact and TKA) are shown.
The TKA did not affect the range of varus-valgus laxity as the knee flexed, but there was a tendency for the range of laxity to shift into varus. (A) Tibial varus-valgus angle envelope of laxity for the intact knee (n = 7, ±standard deviation), and (B) tibial varus-valgus angle envelope of laxity after TKA implantation (n = 7, ±95% confidence interval of the difference between intact and TKA) are shown.
The TKA did not have a large effect on either the neutral path of AP motion or the AP laxity when the knee was near extension (Figs. 6, 7). In the flexed knee, the tibial positions were shifted considerably posteriorly after TKA for the neutral path (0.024 ≤ p < 0.05 from 87° to 75° extension) and with a posterior drawer force (0.0002 ≤ p < 0.05 from 87° to 44° extension). The anterior laxity did not change very much (p > 0.05) at any angle of knee flexion examined.
After TKA, the tibial position moved progressively posteriorly with knee flexion compared with the natural position. (A) The neutral pathway of tibial AP translation for the intact knee (n = 8, ±standard deviation), and (B) the neutral pathway of tibial AP translation after TKA implantation (n = 8, ±95% confidence interval of the difference between intact and TKA). Considerable differences are indicated with the bracket.
Although the range of AP laxity was maintained after TKA, it shifted progressively posteriorly as the knee flexed compared with the natural range of tibial positions. (A) Tibial AP translation envelope of laxity for the intact knee (n = 8, ±standard deviation), and (B) tibial AP translation envelope of laxity after TKA implantation (n = 8, ±95% confidence interval of the difference between intact and TKA). Considerable differences are indicated with the bracket.
Discussion
It has been difficult to relate knee kinematics to specific details of a surgical procedure or implant design, partly because of the inherent lack of precision in surgery. That has been overcome to a large extent by the introduction of optical navigation systems that typically can measure to ±0.5 mm or ±0.5°, thus allowing consistent TKA positioning in relation to anatomic features. Improving kinematics should improve the function of patients after TKA, particularly with increasing use in younger patients. We report data arising from placing one type of prosthesis at a position to which the surgeon was guided by navigation software; the resulting construct led to some deviations from the natural path of motion and laxity limits. Analysis of the design of the chosen prosthesis, along with a review of the literature, led to several hypotheses relating to alterations from the natural motion and laxity of the knee caused by the TKA. The chosen implant design had equal-sized femoral condyles, of constant radius, that articulated with partly conforming fixed tibial bearing surfaces that also were the same size. We hypothesized these features would lead to motion compatible with that of a fixed axis, losing rotational components of motion about other axes. Because of the constant-radius femoral condyles and accuracy of the navigation system when setting up the collateral ligaments, it was hypothesized that internal-external rotation and varus-valgus laxity would remain within normal limits across the arc of knee flexion-extension. Published data regarding loss of roll-back led to the hypothesis that the normal AP tibiofemoral roll-back relationship would not be maintained after TKA. Excision of the ACL led to the hypothesis that the tibia would subluxate anteriorly under drawer testing and have larger than normal AP laxity.
These findings must be interpreted in light of the specific limitations of these experiments in vitro: the use of TKA with a fixed bearing and equal-sized medial and lateral femoral condyles with one radius of curvature in the sagittal plane; loading imposed only by a quadriceps tension; and analysis only of knee extension motion. Although the specimens did reflect the ages of patients undergoing TKA, these specimens were more normal than those to be replaced; however, we believe it is important to know how well a TKA restores normal function. We also imposed only a quadriceps load to the knees to provide an extension moment; simulation with other muscles could alter the kinematics and numerous combinations are possible. We chose not to add muscle cocontractions because that would have added to the complexity of an already complex experiment. The important point is the geometry and loading were well-defined; we believe differences between kinematics studies may result from lack of control of the forces across the knee, especially in vivo. The quadriceps tension was limited to 200 N because we found in an earlier pilot experiment that we sometimes damaged frail cadaveric knees when applying 400 N. However, this force was sufficient to ensure that the articular surfaces were compressed together during the tests, so the knee motion was controlled by the implant geometry. We postulate that a larger compressive force would have reduced the limits of laxity for the natural and artificial joints. The validity of the data resulting from this work in vitro may be judged by reference to data obtained in vivo. Our experiments differed from those of Stiehl et al. [39] in that we did not observe the erratic AP motion they reported. However, loss of screw-home rotation was reported in a fluoroscopic study of the same prosthesis in vivo [26].
We confirmed the hypothesis that symmetric and conforming condyles of the TKA components would inhibit the natural screw-home rotation kinematics. The prosthesis maintained a constant rotation that matched the natural knee in full extension. That stable position reflected the close-packing of the articular surfaces with simultaneous tightening of the soft tissues around the knee. The natural screw-home motion in the intact knees was in accordance with previous studies [10, 20, 24, 27], although variations have been reported and Lafortune et al. [28] did not find screw-home motion. These variations might reflect differences in loading conditions and definition of axes of motion [33]. Screw-home sometimes is lost after TKA [30, 31, 42], although that is not inevitable [23, 37]. Differences in behavior may reflect the use of symmetric versus asymmetric condyles, inherent constraint between the components, or differing alteration of the soft tissues during implantation. In particular, tightening of the ACL as the natural knee reaches extension imposes an external rotation torque on the tibia [20], which was lost by ACL excision during TKA.
We also confirmed the hypothesis that the limits of tibial rotation laxity after TKA would remain similar to those of intact knees. The pattern of reducing laxity as the natural knee extended, from 27° to 6° internal-external rotation, was matched closely by the prosthetic knee. This suggests progressive tightening of the soft tissues as the natural knee extended was preserved after TKA and constraint in the articulation was not excessive. However, the limits of rotational laxity after TKA also reflected the loss of the screw-home and so were considerably externally rotated compared with normal, from approximately 40° to 10° knee extension. Whiteside et al. [45] suggested rotational constraint is not necessary in a TKA to maintain normal rotational laxity as long as the soft tissues are tensed correctly.
The data confirmed the hypothesis that after TKA, varus-valgus laxity would not be altered substantially across the arc of knee flexion-extension. Varus-valgus alignment was aided by accuracy of the navigation system when cutting the femoral condyles and setting up the collateral ligaments to have constant tension when moving around the constant-radius prosthetic condyles. It was expected that knee varus-valgus alignment would be maintained because of the accuracy of the navigation system. The tendency to move into varus in flexion after TKA reflected the femoral component rotation, that followed from the surgeon’s judgement when digitizing the transepicondylar axis, which deviates from the posterior condylar line [36]. However, the extra bone resected from the posterior medial condyle was matched at the tibia, maintaining a parallel space for the implant.
Finally, the data do not support the hypothesis that excision of the ACL and preservation of the PCL during TKA would lead to the tibia moving in a relatively anteriorly translated position. After TKA, the AP position of the tibia was normal when the knee was in extension, but it shifted considerably posteriorly in flexion, the opposite tendency to what was expected. This indicates a loss of femoral roll-back in flexion and loss of normal restraint by the PCL. We confirmed, by reopening the knees, that the PCL always remained intact. This implies the size, position, and shape of the femoral component, which acts like a cam against the tibial component concavity, had effectively allowed the PCL to slacken as the knee flexed. The abnormal posterior translation of the tibia did not imply stretching of the PCL if the implant geometry had allowed the tibia to move proximally to maintain contact, as has been reported [22]. The kinematic data showed that there had been a mean proximal translation of 1.8 mm at 70° flexion. Conversely, the tibia tended not to be drawn forward to its physiologic anterior laxity limit in the flexed knee, despite the ACL having been excised. These observations suggest the prosthetic articulation forced the tibia posteriorly in the flexed knee. In addition, the quadriceps tension would have acted to prevent tibiofemoral distraction, which would result from the femoral component sliding up the slope of the posterior part of the tibial articular surface during anterior drawer testing. Thus, the mechanics of the loaded articulation prevented femoral roll-back (the posterior movement of the tibiofemoral contact points [35]) seen in the natural knee [34]. This has been reported with other implants [32] and causes posterior impingement and loss of knee flexion [6].
The clinical relevance of this in vitro study relates to the desire to improve function of patients after TKA, particularly with younger patients undergoing TKAs. In the past, it has been difficult to relate knee kinematics to specific details of surgical procedure or implant design, partly because of the inherent lack of precision in surgery. That has been overcome to a large extent by the introduction of optical navigation systems that can measure typically to ±0.5 mm or ±0.5°, thus allowing consistent prosthesis positioning in relation to anatomic features. We report data arising from placing one type of prosthesis at a position to which the surgeon has been guided by navigation software; the resulting construct led to some deviations from the natural path of motion and laxity limits. Much of that deviation is now explainable by reference to the prosthetic articular geometry, as discussed previously. It is not known whether the datum position in the software will give the best restoration of physiologic kinematics, but the technology now can be applied to study this question. Such a study carries the inherent assumption that a search for restoration of normal kinematics is desirable for optimizing patient function, and that also is not yet known but does appear a reasonable assumption.
Our data suggest the kinematics of the natural knee were not maintained in all respects after arthroplasty with an implant that had equal-sized circular femoral condyles, when loaded and moved in vitro. Use of a navigation system enabled accurate maintenance of tibiofemoral coronal alignment and varus-valgus limits of laxity, across the range of knee flexion-extension. However, the conforming cylindrical articular geometry led to loss of the natural pattern of tibial rotation, the screw-home mechanism, whereas the range of internal-external rotation laxity was maintained. Contrary to the initial hypothesis, excision of the ACL during arthroplasty did not lead to abnormal tibial anterior translation. On the contrary, there was lack of physiologic femoral roll-back on the tibial plateau when the knee was flexed after arthroplasty, in line with published studies using video fluoroscopy in vivo. Although these findings are implant-specific, the differences between the kinematics of natural and artificial knees suggest that an adjustment of the guidance given by the navigation system might lead to an implant position that provides better maintenance of physiologic motion.
References
Aglietti P, Buzzi R, Gaudenzi A. Patellofemoral functional results and complications with posterior stabilized total knee prosthesis. J Arthroplasty. 1988;3:17–25.
Banks SA, Hodge WA. Accurate measurement of three-dimensional knee replacement kinematics using single-plane fluoroscopy. IEEE Trans Biomed Eng. 1996;43:638–649.
Banks SA, Hodge WA. Implant design affects knee arthroplasty kinematics during stair-stepping. Clin Orthop Relat Res. 2004;426:187–193.
Banks SA, Markovich GD, Hodge WA. In-vivo kinematics of cruciate-retaining and substituting knee arthroplasties. J Arthroplasty. 1997;12:297–304.
Barrack RL, Schrader T, Bertot AJ, Wolfe MW, Myers L. Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop Relat Res. 2001;392:46–55.
Bellemans J, Banks S, Victor J, Vandenneucker H, Moemans A. Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty: influence of posterior condylar offset. J Bone Joint Surg Br. 2002;84:50–53.
Berger RA, Crossett LS, Jacobs JJ, Rubash HE. Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res. 1998;356:144–153.
Berger RA, Lyon JH, Jacobs JJ, Barden RM, Berkson EM, Sheinkop MB, Rosenberg AG, Galante JO. Problems with cementless total knee arthroplasty at 11 years followup. Clin Orthop Relat Res. 2001;392:196–207.
Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res. 1993;286:40–47.
Blankevoort L, Huiskes R, de Lange A. The envelope of passive knee joint motion. J Biomech. 1988;21:705–720.
Chauhan SK, Scott RG, Breidahl W, Beaver RJ. Computer-assisted knee arthroplasty versus a conventional jig-based technique: a randomized, prospective trial. J Bone Joint Surg Br. 2004;86:372–377.
Churchill DL, Incavo SJ, Johnson CC, Beynnon BD. The transepicondylar axis approximates the optimal flexion axis of the knee. Clin Orthop Relat Res. 1998;356:111–118.
Daniel DM, Malcom LL, Losse G, Stone ML, Sachs R, Burks R. Instrumented measurement of anterior laxity of the knee. J Bone Joint Surg Am. 1985;67:720–726.
Dowson D. Biotribology of natural and replacement synovial joints. In: Mow VC, Ratcliffe A, Woo SLY, eds. Biomechanics of Diarthrodial Joints. New York, NY: Springer-Verlag; 1990:305–345.
Figgie HE 3rd, Goldberg VM, Hieple KG, Moller HS 3rd, Gordon NH. The influence of tibial-patellofemoral location on the function of the knee in patients with posterior stabilized condylar knee prosthesis. J Bone Joint Surg Am. 1986;68:1035–1040.
Fisher J, Dowson D (1991). Tribology of total artificial joints. Proc Inst Mech Eng [H] 205:73–79.
Fort-Rodriguez DE, Scuderi GR, Insall JN. Survivorship of cemented total knee arthroplasty. Clin Orthop Relat Res. 1997;345:79–86.
Grood ES, Stowers SF, Noyes FR. Limits of movement in the human knee: effect of sectioning the posterior cruciate ligament and posterolateral structures. J Bone Joint Surg Am. 1988;70:88–97.
Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng. 1983;105:133–144.
Hallen LG, Lindahl O. The “screw-home” movement in the knee joint. Acta Orthop Scand. 1966;37:97–106.
Hsu HP, Garg A, Walker PS, Spector M, Ewald FC. Effect of knee component alignment on tibial load distribution with clinical correlation. Clin Orthop Relat Res. 1989;248:135–144.
Incavo SJ, Beynnon BD, Johnson CC, Churchill DL. Knee kinematics in genesis total knee arthroplasty: a comparison of different tibial designs with and without posterior cruciate ligament substitution in cadaveric specimens. Am J Knee Surg. 1997;10:209–215.
Ishii Y, Terajima K, Koga Y, Bechtold JE. Screw home motion after total knee replacement. Clin Orthop Relat Res. 1999;358:181–187.
Ishii Y, Terajima K, Terashima S, Koga Y. Three-dimensional kinematics of the human knee with intracortical pin fixation. Clin Orthop Relat Res. 1997;343:144–150.
Karrholm J, Jonsson H, Nilsson KG, Soderqvist I. Kinematics of successful knee prostheses during weight-bearing: three dimensional movements and positions of screw axes in Tricon-M and Miller-Galante designs. Knee Surg Sports Traumatol Arthrosc. 1994;2:50–59.
Kessler O, Durselen L, Banks S, Mannel H, Marin F. Sagittal curvature of total knee replacements predicts in vivo kinematics. Clin Biomech (Bristol, Avon). 2007;22:52–58
Kettelkamp DB, Johnson RJ, Smidt GL, Chao EY, Walker M. An electrogoniometric study of knee motion in normal gait. J Bone Joint Surg Am. 1970;52:775–790.
Lafortune MA, Cavanagh PR, Sommer HJ 3rd, Kalenak A. Three-dimensional kinematics of the human knee during walking. J Biomech. 1992;25:347–357.
Merkow RL, Soudry M, Insall JN. Patellar dislocation following total knee replacement. J Bone Joint Surg Am. 1985;67:1321–1327.
Most E, Li G, Schule S, Sultan P, Park SE, Zayontz S, Rubash HE. The kinematics of fixed- and mobile-bearing total knee arthroplasty. Clin Orthop Relat Res. 2003;416:197–207.
Nilsson KG, Karrholm J, Gadegaard P. Abnormal kinematics of the artificial knee: roentgen stereophotogrammetric analysis of 10 Miller-Galante and five New Jersey LCS knees. Acta Orthop Scand. 1991;62:440–446.
Pandit H, Ward T, Hollinghurst D, Beard J, Gill HS, Thomas NP, Murray DW. Influence of surface geometry and cam-post mechanism on the kinematics of total knee replacement. J Bone Joint Surg Br. 2005;87:940–945.
Piazza SJ, Cavanagh PR. Measurement of the screw-home motion of the knee is sensitive to errors in axis alignment. J Biomech. 2000;33:1029–1034.
Pinskerova V, Johal P, Nakagawa S, Sosna A, Williams A, Gedroyc W, Freeman MA. Does the femur roll-back with flexion? J Bone Joint Surg Br. 2004;86:925–931.
Scarvell JM, Smith PN, Refshauge KM, Galloway HR, Woods KR. Comparison of kinematic analysis by mapping tibiofemoral contact with movement of the femoral condylar centres in healthy and anterior cruciate ligament injured knees. J Orthop Res. 2004;22:955–962.
Shih YF, Bull AM, Amis AA. The cartilaginous and osseous geometry of the femoral trochlear groove. Knee Surg Sports Traumatol Arthrosc. 2004;12:300–306.
Stein A, Fleming B, Pope MH, Howe JG. Total knee arthroplasty kinematics: an in vivo evaluation of four different designs. J Arthroplasty. 1988;3(suppl):S31–36.
Stiehl JB, Dennis DA, Komistek RD, Crane HS. In vivo determination of condylar lift-off and screw-home in a mobile bearing total knee arthroplasty. J Arthroplasty. 1999;14:293–299.
Stiehl JB, Komistek RD, Dennis DA, Paxson RD, Hoff WA. Fluoroscopic analysis of kinematics after posterior-cruciate-retaining knee arthroplasty. J Bone Joint Surg Br. 1995;77:884–889.
Uvehammer J. Knee joint kinematics, fixation and function related to joint area design in total knee arthroplasty. Acta Orthop Scand Suppl. 2001;72:1–52.
Uvehammer J, Kärrholm J, Brandsson S. In vivo kinematics of total knee arthroplasty: concave versus posterior-stabilised tibial joint surface. J Bone Joint Surg Br. 2000;82:499–505.
Uvehammer J, Kärrholm J, Brandsson S, Herberts P, Carlsson L, Karlsson J, Regnér L. In vivo kinematics of total knee arthroplasty: flat compared with concave tibial joint surface. J Orthop Res. 2000;18:856–864.
Vince KG, Insall JN, Kelly MA. The total condylar prosthesis: 10- to 12-year results of a cemented knee replacement. J Bone Joint Surg Br. 1989;71:793–797.
Weir DJ, Moran CG, Pinder IM. Kinematic condylar total knee arthroplasty: 14-year survivorship analysis of 208 consecutive cases. J Bone Joint Surg Br. 1996;78:907–911.
Whiteside LA, Kasselt MR, Haynes DW. Varus-valgus and rotational stability in rotationally unconstrained total knee arthroplasty. Clin Orthop Relat Res. 1987;219:47–157.
Wimmer MA, Andriacchi TP. Tractive forces during rolling motion of the knee: implications for wear in total knee replacement. J Biomech. 1997;30:131–137.
Acknowledgments
We thank D. Lucas, who performed much of the experimental work; however, the analysis, discussion, and conclusions are those of the authors alone. We thank J. L. Moctezuma, H. Boschert, and P. Zimmerman of Stryker (Leibinger) for their support with data recording using the Stryker Navigation System; and P. Wilson of the Mechanical Engineering Department for technical support. We also thank Prof P. Aichroth for advice.
Author information
Authors and Affiliations
Corresponding author
Additional information
One or more of the authors (AAA, AMJB) have received funding by Stryker (Europe).
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that tissue specimens were obtained in accordance with the laws of France.
About this article
Cite this article
Bull, A.M.J., Kessler, O., Alam, M. et al. Changes in Knee Kinematics Reflect the Articular Geometry after Arthroplasty. Clin Orthop Relat Res 466, 2491–2499 (2008). https://doi.org/10.1007/s11999-008-0440-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-008-0440-z