Abstract
Purpose
The purpose of this study was to evaluate the outcomes of arthroscopy-guided direct suprascapular nerve block performed after arthroscopic rotator cuff repair.
Methods
In the present prospective, randomized, double-blinded clinical study, 30 patients were divided into two groups: 15 patients (group I) were treated with arthroscopy-guided suprascapular nerve block using 10 mL 0.5 % ropivacaine with 1:200,000 epinephrine, and 15 patients (group II) were treated with placebo using 10 mL 0.9 % saline after arthroscopic rotator cuff repair. Patient pain levels were measured using the visual analog scale (VAS) at 1, 3, 6, 12, 18, and 24 h post-operatively. Additionally, the number of boluses and total amount of fentanyl dispensed by patient-controlled analgesia administration during the 24-h post-operative period were evaluated.
Results
VAS scores did not differ significantly between groups I and II during the 24-h post-operative period, but mean fentanyl bolus consumption was significantly less in group I compared with group II (p = 0.015).
Conclusion
Arthroscopy-guided suprascapular nerve block at the end of a rotator cuff repair was safe and less time-consuming than expected. Although this procedure did not significantly reduce the post-operative pain, the post-operative need for fentanyl boluses as analgesia was reduced significantly, and it would be beneficial if this procedure involved a sensory branch of axillary nerve block or was performed at the beginning of the arthroscopic procedure.
Level of evidence
Prospective, randomized, double-blinded clinical trial, Level I.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although most shoulder surgeries are now performed in a minimally invasive way with arthroscopy, the severity of post-operative pain is often sufficient to negatively impact recovery and rehabilitation [16]. Thus, reducing immediately post-operative pain is very important in increasing patients’ satisfaction rates and subjective and objective results.
Many post-operative pain management modalities have been introduced, and such modalities are often used in combination to provide the most effective pain control. Methods of providing pain relief include the periarticular injection of morphine or a local anaesthetic [5], interscalene nerve block [1], suprascapular nerve block (SSNB) [11], oral analgesics, patient-controlled analgesia (PCA) with intravenous opioids, and the subacromial local anaesthetic infusion pump [4]. One of these options, SSNB, provides excellent pain relief in shoulder disorders because the suprascapular nerve is the main contributor to pain from acute or chronic injury to the shoulder joint [6, 23]. Furthermore, use of the SSNB for post-operative pain relief is effective, helping to reduce the post-operative morphine requirement and shorten the recovery process after arthroscopic shoulder surgery [19]. However, no data about the effectiveness of intraoperative arthroscopic-guided direct SSNB as a post-operative pain management method in rotator cuff repair are currently available, and no comparative study has assessed the procedure.
The purpose of this study was to evaluate the outcomes of intraoperative arthroscopy-guided direct SSNB as a post-operative pain management option in arthroscopic rotator cuff repair under general anaesthesia. Our null hypothesis was that intraoperative arthroscopy-guided direct SSNB would not significantly reduce post-operative pain after rotator cuff repair, but that the pain might be influenced by the severity of rotator cuff repair.
Materials and methods
Thirty patients (11 females, 19 males) with a mean age of 50 years with a rotator cuff tear were included in the study. The diagnoses of a rotator cuff tear were made according to detailed physical and radiological examinations. The exclusion criteria were the presence of (1) stiffness, (2) glenohumeral arthritis, or (3) pre-existing suprascapular dysfunction in addition to the rotator cuff tear. Patients with a history of allergy to local analgesic agents were also excluded.
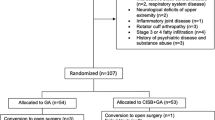
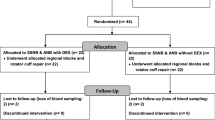
The study was conducted at the Department of Orthopedic Surgery of Hallym University. The trial was approved by the local ethics committee and was performed in accord with the Declaration of Helsinki. After institutional review board approval had been given and all patients had provided informed consent, patients scheduled for arthroscopic rotator cuff shoulder surgery were enrolled in this prospective, randomized, double-blinded, placebo-controlled trial between February and September 2012. Randomization to the SSNB or placebo group was performed using a numbered, sealed envelope method with random permuted blocks to guarantee balance. Group allocation was revealed only to the study coordinator. Pre-operatively, patients were educated in the use of the visual analog scale (VAS) for pain and the PCA system.
For double blinding, the surgeon, patient, and data collector were blinded to the contents of syringes used to administer the SSNB. A research assistant prepared the syringes and delivered them to a scrub nurse who was not involved in this study during the rotator cuff repair procedure.
All patients were randomized to treatment with arthroscopy-guided SSNB using 10 mL 0.5 % ropivacaine with 1:200,000 epinephrine (group I) or arthroscopy-guided SSNB using 10 mL 0.9 % saline solution (group II) at the end of the arthroscopic rotator cuff repair procedure.
Perioperative treatment
For the arthroscopic rotator cuff repair, general anaesthesia was induced with an intravenous injection of propofol (2 mg/kg). Rocuronium (0.7 mg/kg) was administered for muscle relaxation and tracheal intubation, and the lungs were mechanically ventilated. Anaesthesia was maintained with 50 % nitrous oxide in oxygen and 2–2.5 % sevoflurane in a semi-closed circle system.
Patients received a placebo block or an SSNB at the end of the main rotator cuff procedure. The suprascapular ligament and adjacent suprascapular nerve were exposed using electrocautery introduced through the anterior portal. An 18-gauge spinal needle was inserted perpendicularly 7 cm medial to the lateral margin of the acromion and just above the previously isolated transverse suprascapular ligament. Under direct visualization of the suprascapular nerve, an 18-gauge needle was introduced and the drug was infused around the nerve running medial to the transverse suprascapular ligament. After suctioning the saline from the portal and closing the wound, the randomly assigned injection was administrated. The injection material was 10 mL 0.5 % ropivacaine or saline.
Post-operative treatment
Post-operative analgesia was provided by a PCA intravenous pump that was programmed to deliver a 1-μg kg−1 bolus of fentanyl as rescue analgesia. The lockout time was 1 h, and the maximum dose was 700 μg.
Outcome assessment
The primary outcome measure (post-operative pain) was assessed using the 10-point modified VAS. Pain scores were obtained 1, 3, 6, 12, 18, and 24 h after surgery. The number of boluses and total amount of fentanyl dispensed by PCA during the 24-h post-operative period were also evaluated. During the first 24 h post-operatively, we checked for adverse events, including the incidence of post-operative nausea and vomiting, and the need for a rescue drug.
Statistical analysis
An a priori power analysis was performed. A minimum of 15 patients in each treatment group were anticipated to provide approximately 80 % power for detecting a difference of 20 % in the proportion of patients who underwent arthroscopy-guided direct SSNB using 10 mL 0.5 % ropivacaine with 1:200,000 epinephrine versus 10 mL saline at a significance level of 0.05. Normally distributed data were analysed using the t test for independent samples; the incidence of nausea and vomiting was analysed using Fisher’s exact test; all other data were analysed using the nonparametric Mann–Whitney U test. Our null hypothesis was that post-operative pain scores and the need for opioid analgesia would not differ between the two groups. Statistical significance was defined as p < 0.05. All analyses were conducted using SPSS software (version 16.0 for Windows; SPSS, Chicago, IL, USA).
Results
No significant differences in age, sex, height, weight, rotator cuff tear size, or hospital stay between the two groups were found (Table 1).
Post-operative VAS scores
VAS scores at 1, 3, 6, 12, 18, and 24 h post-operatively did not differ significantly between patients treated with arthroscopy-guided SSNB using 10 mL 0.5 % ropivacaine with 1:200,000 epinephrine (group I) and those treated with SSNB using 10 mL 0.9 % saline (group II), but average pain scores were slightly lower in group I (Table 2).
Number of boluses and total amount of fentanyl dispensed by PCA
In group I, five patients (33 %) used the PCA for post-operative analgesia, and the overall group I mean number of boluses used was 2.1. In group II, all patients (100 %) used the PCA, and the overall group II mean number of boluses used was 4.9. The mean consumption of fentanyl during the 24-h post-operative period differed significantly between groups I (137.8 ± 212.4 μg) and II (315.1 ± 110.4 μg; p = 0.015; Table 3).
The incidence of nausea and vomiting
Two patients (13 %) in group I and six patients (40 %) in group II felt nausea within 24 h after surgery; however, the incidence of nausea did not differ significantly between the groups. There was no significant difference in the incidence of vomiting between groups I (one patient; 7 %) and II (one patient; 7 %). Rescue drugs were given to one patient in each group who vomited, and there was no significant difference between the groups (Table 4).
Discussion
The most important finding of this study was that single SSNB might not be sufficient for controlling post-operative pain after a rotator cuff repair, despite using the most accurate approach for needle placement for the suprascapular nerve. Factors contributing negative effects included central sensitization, anatomical variant of articular sensory branch of suprascapular nerve, and none of its sensory innervation to the inferior and anterior shoulder region.
Arthroscopic shoulder surgery is often associated with severe post-operative pain [16]. To improve post-operative analgesic treatment and reduce the need for systemic analgesic medications, including opioids, a regional anaesthetic regime can be helpful [2, 8, 19]. The interscalene brachial plexus block is the most frequently used pain relief technique in arthroscopic shoulder surgery [1, 14, 17, 21]. Singelyn et al. [21] reported that this block was the most efficient analgesic technique after arthroscopic acromioplasty. However, this method is associated with potentially serious complications, such as central nervous system, respiratory, or cardiovascular complications [15]; moreover, it is contraindicated in some patient categories (e.g. patients with severe chronic obstructive pulmonary disease) [9].
Suprascapular nerve block offers a safe alternative to an interscalene nerve block [21]; consequently, many studies have evaluated its use [11, 12, 19]. This method blocks sensory innervation to the posterior shoulder joint and surrounding tissues. However, the suprascapular nerve supplies only 70 % of the sensory fibres to the joint and capsule. In other words, patients might suffer from shoulder pain caused by the remaining 30 % of sensory fibres innervating the shoulder, such as the lateral pectoral nerve and axillary nerve, despite SSNB administration. Furthermore, the SSNB does not provide cutaneous analgesia, and patients might also suffer from incisional wound pain. Thus, the singular use of the SSNB might not provide sufficient post-operative pain relief.
The majority of studies reporting nerve block injections into the shoulder were carried out in a blind fashion with the clinician using anatomical landmarks to guide the injection. Of course, a landmark-guided SSNB might be completely sufficient, and this has been shown in some studies [11, 12]. Nevertheless, some authors have suggested that inaccurate placement of the needle tip might be the cause of the variable effectiveness of this technique [7, 22]. Reported demonstrated accuracy rates have ranged from 10 to 50 % [13, 24]. Thus, despite the high cost and skill required, many studies have reported the use of image-guided intervention to improve accuracy and reduce adverse effects [10, 20].
In this study, we performed SSNB for post-operative pain relief under direct arthroscopic visualization following arthroscopic rotator cuff repair, and average time for the procedure was 3 min. Our study results showed no significant improvement in post-operative pain scores following surgery compared with the placebo group; however, average pain scores were slightly lower in the treatment group (group I). In contrast to our findings, some studies showed that pre-emptive SSNB significantly reduced VAS scores and post-operative opioid requirements [12, 19]. This contradictory result might be caused by the problem of central sensitization or the severity of the main surgery. In this study, we did not perform SSNB before the rotator cuff repair because we were concerned about the early occurrence of extravasation in which oedematous soft tissue can encroach on the operative field. The severity of arthroscopic procedure is another variable. We enrolled only patients who underwent reconstructive procedures that consisted of subacromial bursectomy, acromioplasty, and biceps tenotomy (or tenodesis) and rotator cuff repair. The previous reports that showed a positive effect of SSNB enrolled patients who underwent only acromioplasty, bursectomy, or arthroscopic capsular release [3, 11, 12].
Patients’ needs for bolus doses of intravenous opioids by PCA were significantly reduced. Although opioid analgesics effectively relieve post-operative pain, they also cause well-known adverse effects, such as nausea, vomiting, dizziness, pruritus, respiratory depression, constipation, and prolonged hospital stays [18]. In this study, two patients (13 %) in group I and six patients (40 %) in group II experienced nausea within 24 h after surgery. Therefore, an opioid-sparing analgesic technique after shoulder surgery is desirable, and our SSNB might be useful in this regard for post-operative analgesia and nausea.
This study design had some limitations. All patients were offered a PCA system that intravenously administered fentanyl and were able to decide the amount they used within the limit of 700 μg. Patients in group II used much more fentanyl, which made it difficult to evaluate the efficacy of our SSNB using the VAS. Furthermore, the timing of PCA use was not evaluated, only the total number of boluses and amount of fentanyl dispensed during the 24-h post-operative period. Additionally, the initial study design did not take into consideration the potential for central sensitization; the performance of arthroscopy-guided direct SSNB immediately after arthroscope insertion may yield better results.
Arthroscopy-guided SSNB at the end of rotator cuff repair was safe and less time-consuming than expected. Although this procedure did not significantly reduce post-operative pain, it would be beneficial if this procedure involved a sensory branch of the axillary nerve or was performed at the beginning of the arthroscopic procedure.
Conclusion
Patients treated with arthroscopy-guided direct SSNB after arthroscopic rotator cuff repair showed no significant improvement in post-operative VAS scores in comparison with the placebo group. However, the post-operative need for fentanyl analgesia was reduced significantly.
References
Al-Kaisy A, McGuire G, Chan VW et al (1998) Analgesic effect of interscalene block using low-dose bupivacaine for outpatient arthroscopic shoulder surgery. Reg Anesth Pain Med 23:469–473
Capdevila X, Dadure C, Bringuier S et al (2006) Effect of patient-controlled perineural analgesia on rehabilitation and pain after ambulatory orthopedic surgery: a multicenter randomized trial. Anesthesiology 105:566–573
Checcucci G, Allegra A, Bigazzi P, Gianesello L, Ceruso M, Gritti G (2008) A new technique for regional anesthesia for arthroscopic shoulder surgery based on a suprascapular nerve block and an axillary nerve block: an evaluation of the first results. Arthroscopy 24:689–696
Coghlan JA, Forbes A, McKenzie D, Bell SN, Buchbinder R (2009) Efficacy of subacromial ropivacaine infusion for rotator cuff surgery. A randomized trial. J Bone Joint Surg Am 91:1558–1567
Doss NW, Splain SH, Crimi T, Michael R, Abadir AR, Gintautas J (2001) Intra-articular morphine, ropivacaine, and morphine/ropivacaine for pain control after arthroscopy: preliminary observation. Proc West Pharmacol Soc 44:195–196
Emery P (1989) Suprascapular nerve block for chronic shoulder pain in rheumatoid arthritis. Br Med J 299:1079–1080
Eustace JA, Brophy DP, Gibney RP, Bresnihan B, FitzGerald O (1997) Comparison of the accuracy of steroid placement with clinical outcome in patients with shoulder symptoms. Ann Rueum Dis 56:59–63
Fontana C, Di Donato A, Giacoma G et al (2009) Postoperative analgesia for arthroscopic shoulder surgery: a prospective randomized controlled study of intraarticular, subacromial injection, interscalene brachial plexus block and intraarticular plus subacromial injection efficacy. Eur J Anaesthesiol 26:689–693
Fujimuta N, Namba H, Tsunoda K et al (1995) Effects of hemidiaphragmatic paresis caused by interscalene plexus block on breathing pattern, chest wall mechanics, and arterial blood gases. Anesth Analg 81:962–966
Harmon D, Hearty C (2007) Ultrasound-guided suprascapular nerve block technique. Pain Physician 10:743–746
Jerosch J, Saad M, Greig M, Filler T (2008) Suprascapular nerve block as a method of preemptive pain control in shoulder surgery. Knee Surg Sports Traumatol Arthrosc 16:602–607
Jeske HC, Kralinger F, Wambacher M et al (2011) A randomized study of the effectiveness of suprascapular nerve block in patient satisfaction and outcome after arthroscopic subacromial decompression. Arthroscopy 27:1323–1328
Jones A, Regan M, Hedingham J, Pattrick M, Manhire A, Doherty M (1993) Importance of placement of intra-articular injections. BMJ 307:1329–1330
Laurila PA, Lopponen A, Kangas-Saarela T, Flinkkila T, Salomaki TE (2002) Interscalene brachial plexus block is superior to subacromial bursa block after arthroscopic shoulder surgery. Acta Anaesth Scand 46:1031–1036
Lenters TR, Davies J, Matsen FA 3rd (2007) The types and severity of complications associated with interscalene brachial plexus block anesthesia: local and national evidence. J Shoulder Elbow Surg 16:379–387
Moote C (1994) Random double-blind comparison of intra-articular bupivacaine and placebo for analgesia after outpatient shoulder arthroscopy. Anesthesiology 81:A49 (abstract)
Pippa P, Cominelli E, Marinelli C, Aito S (1990) Brachial plexus block using the posterior approach. Eur J Anaesthesiol 7:411–420
Pizzi LT, Toner R, Foley K, Thomson E, Chow W, Kim M, Couto J, Royo M, Viscusi E (2012) Relationship between potential opioid-related adverse effects and hospital length of stay in patients receiving opioids after orthopedic surgery. Pharmacotherapy 32:502–514
Ritchie ED, Tong D, Chung F, Norris M, Miniaci A, Vairavanathan SD (1997) Suprascapular nerve block for postoperative pain relief in arthroscopic shoulder surgery: a new modality? Anesth Analg 84:1306–1312
Schneider-Kolsky ME, Pike J, Connell DA (2004) CT-guided suprascapular nerve blocks: a pilot study. Skeletal Radiol 33:277–282
Singelyn FJ, Lhotel L, Fabre B (2004) Pain relief after arthroscopic shoulder surgery: a comparison of intraarticular analgesia, suprascapular nerve block, and interscalene brachial plexus block. Anesth Analg 99:589–592
Stoker DJ (1991) Intra-articular injections in capsulitis (letter). BMJ 303:123
Wassef MR (1992) Suprascapular nerve block: a new approach for the management of frozen shoulder. Anaesthesia 47:120–124
White AET, Tuite JD (1996) The accuracy and efficacy of shoulder injections in restrictive capsulitis. J Orthop Rheumatol 9:37–40
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, J.J., Yoo, YS., Hwang, JT. et al. Efficacy of direct arthroscopy-guided suprascapular nerve block after arthroscopic rotator cuff repair: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc 23, 562–566 (2015). https://doi.org/10.1007/s00167-013-2451-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-013-2451-x